Difference between revisions of "Kidney tumours"
m (→Oncocytoma: format) |
|||
| (402 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
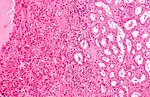
'''Kidney tumours''' - includes '''malignant kidney tumours''' and '''benign kidney tumours'''. Medical renal diseases are dealt with in the [[medical renal diseases]] article. | [[Image:Renal oncocytoma.jpg|thumb|250px|A kidney tumour ([[renal oncocytoma]]). (WC/Emmanuelm)]] | ||
'''[[Kidney]] tumours''' - includes '''malignant kidney tumours''' ('''kidney cancer''') and '''benign kidney tumours'''. Medical renal diseases are dealt with in the [[medical renal diseases]] article. | |||
Pediatric kidney tumours are dealt with in the ''[[pediatric kidney tumours]]'' article. | |||
=Renal specimens= | |||
*[[Renal biopsy]] - usually for [[renal oncocytoma]] vs. renal cell carcinoma (RCC) ''or'' medical diseases - see ''[[medical kidney]]''. | |||
*[[Partial nephrectomy]]. | |||
*[[Nephrectomy]]. | |||
*[[Nephroureterectomy]] (includes [[ureter]]) - done for [[urothelial cell carcinoma]] (UCC) of the renal pelvis and ureteric UCC. | |||
*[[Radical nephrectomy]] - includes Gerota's fascia. | |||
**May include the [[adrenal gland]].<ref name=Ref_WMSP|288>{{Ref WMSP|288}}</ref> | |||
In excisions done for tumours, a comment should be made about kidney distant from the tumour. People with less renal mass, i.e. less kidney, are predisposed to focal segmental glomerulosclerosis (FSGS). | |||
=== | ==Anatomy== | ||
Layers (superficial to deep): | |||
#Renal fascia (Gerota's fascia). | |||
#Perinephric fat. | |||
#Renal capsule. | |||
#Renal parenchyma (cortex). | |||
===Sign out=== | |||
====Missed renal biopsy==== | |||
{{Main|Missed renal biopsy}} | |||
=Tabular comparison (selected tumours)= | |||
Selected common tumours of the kidney:<ref>GUP | Selected common tumours of the kidney:<ref name=Ref_GUP281>{{Ref GUP|281-304}}</ref><ref name=pmid19494850>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 }}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| | | | ||
| '''Clear cell RCC''' | |||
| '''Papillary RCC<br>type 1''' | |||
| '''Papillary RCC<br>type 2''' | |||
| '''Chromophobe RCC<br>classic variant''' | |||
| '''Chromophobe RCC<br>eosinophilic variant''' | |||
| '''Oncocytoma''' | |||
|- | |- | ||
|Gross | |Gross | ||
| Golden yellow, solid | |||
| friable | |||
| friable | |||
| light brown | |||
| light brown | |||
| mahogany/brown, +/-central scar | |||
|- | |- | ||
|Architecture | |Architecture | ||
| nests, sheets | |||
| papillary, simple | |||
| papillary,<br>pseudostratified | |||
| nests, sheets | |||
| nests, sheets | |||
| nests, sheets | |||
|- | |- | ||
|Nuclear atypia | |Nuclear atypia | ||
| low-high<br>typically medium-high | |||
| low-medium | |||
| medium-high | |||
| low-high, "raisinoid" <br>nuc. membrane | |||
| low-high, "raisinoid" <br>nuc. membrane | |||
| low-medium, round nuclei | |||
|- | |- | ||
|Cytoplasm | |Cytoplasm | ||
| clear | |||
| eosinophilic | |||
| eosinophilic | |||
| cobwebs/clear | |||
| eosinophilic/cobwebs | |||
| eosinophilic/<br>granular & abundant | |||
|- | |- | ||
|Other | |Other | ||
| delicate vessels,<br>[[necrosis]] common | |||
| histiocytes<br> in fibrovascular cores, >0.5 cm | |||
| histiocytes<br> in fibrovascular cores, >0.5 cm | |||
| perinuclear clearing, thick vessels | |||
| perinuclear clearing, thick vessels | |||
| in loose fibrous/hyaline stroma | |||
|- | |- | ||
|IHC | | |IHC | ||
| [[CK7]]-, EMA+ | |||
| AMACR+, EMA+, CK7+ | |||
| AMACR+, E-cadherin+, CK7- | |||
| CD117+, CK7+ (membrane) | |||
| CD117+, CK7+ (membrane) | |||
| Vimentin-, EMA+ | |||
|- | |- | ||
|Main DDx | |Main DDx | ||
| chromophobe<br>classic variant | |||
| PaRCC type 2, mets | |||
| PaRCC type 1, mets | |||
| clear cell RCC | |||
| oncocytoma | |||
| chromophobe<br>eosinophilic variant | |||
|- | |- | ||
|Key features | |Key features | ||
| clear cells, vascular | |||
| papillae, histiocytes<br>simple epithelium | |||
| papillae, histiocytes,<br>stratified | |||
| perinuc. clearing,<br>wispy cytoplasm | |||
| perinuc. clearing,<br>wispy eosinophilic<br>cytoplasm | |||
| eosinophilic, granular cytoplasm | |||
|- | |||
|Image(s) | |||
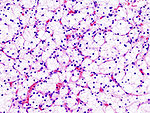
| [[Image:Renal_clear_cell_ca_%281%29_Nephrectomy.jpg|thumb|150px| CCRCC (WC)]] | |||
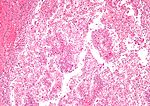
| [[Image:Papillary_renal_cell_carcinoma_intermed_mag.jpg|thumb|150px| PaRCC - intermed. (WC)]], [[Image:Papillary_renal_cell_carcinoma_very_high_mag.jpg | thumb|150px| PaRCC - high (WC)]] | |||
| | |||
| | |||
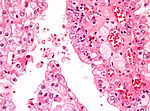
| [[Image:Oncocytic_chromophobe_rcc_high_mag.jpg|thumb|150px| ChRCC (WC)]] | |||
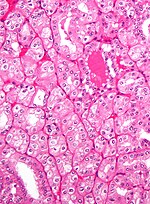
| [[Image:Renal_oncocytoma2.jpg|thumb|150px| Oncocytoma (WC)]] | |||
|} | |} | ||
Notes: | Notes: | ||
*Cell shape: all have epithelioid morphology. | *Cell shape: all have epithelioid morphology. | ||
== | ===Tabular comparison of oncocytoma and chromophobe RCC=== | ||
Histomorphologic features useful to distinguish chromophobe RCC (eosinophilic variant) and oncocytoma:<ref name=pmid9844591>{{Cite journal | last1 = Tickoo | first1 = SK. | last2 = Amin | first2 = MB. | title = Discriminant nuclear features of renal oncocytoma and chromophobe renal cell carcinoma. Analysis of their potential utility in the differential diagnosis. | journal = Am J Clin Pathol | volume = 110 | issue = 6 | pages = 782-7 | month = Dec | year = 1998 | doi = | PMID = 9844591 }}</ref> | |||
{| class="wikitable sortable" | |||
! Morphologic feature | |||
! [[ChRCC]] (eosinophilic<br> variant) | |||
! [[Renal oncocytoma]] | |||
|- | |||
| Nuclear morphology | |||
| "raisinoid"/wrinkled appearance | |||
| round with small nucleolus, <br>usu. little size variation | |||
|- | |||
| Multinucleation | |||
| common - binucleation | |||
| uncommon | |||
|- | |||
| Chromatin | |||
| coarse | |||
| fine | |||
|- | |||
| Architecture | |||
| solid, crowded nests | |||
| spaced nests / <br>archipelago-like, solid | |||
|- | |||
| Cytoplasm | |||
| perinuclear halo, may be focal | |||
| no perinuclear halo | |||
|- | |||
| Degenerative foci<br>(focal atypia & pleomorphism) | |||
| absent | |||
| present in ~20% of cases | |||
|- | |||
| Image | |||
| [[Image:Oncocytic_chromophobe_rcc_high_mag.jpg |thumb|150px|ChRCC (WC/Nephron)]] | |||
| [[Image:Renal_oncocytoma2.jpg |thumb|150px|Oncocytoma (WC/Nephron)]] | |||
|} | |||
===Common DDx=== | |||
====Spindle cell tumours==== | |||
Malignant spindle cell tumours of the kidney: | |||
*[[Renal cell carcinoma with sarcomatoid differentiation]]. | |||
*[[Renal mucinous tubular and spindle cell carcinoma]]. | |||
*[[Wilms tumour]]. | |||
*[[Renal cell carcinoma, unclassified]]. | |||
Benign spindle cell tumours of the kidney: | |||
*[[Angiomyolipoma]]. | |||
* | *[[Cystic nephroma]]. | ||
* | |||
=== | ====Renal tumours with eosinophilic cytoplasm==== | ||
{{Main|Renal tumours with eosinophilic cytoplasm}} | |||
=== | =WHO classification of renal neoplasia= | ||
* | *Based on 2004 iteration - as per WMSP, slightly modified.<ref>{{Ref WMSP|291}}</ref> Online, the classification can [http://www.urosource.com/fileadmin/user_upload/european_urology/PIIS0302283805008316.pdf found here]. | ||
* | ===Renal cell tumours=== | ||
* | Common: | ||
*[[Clear cell renal cell carcinoma]]. | |||
*[[Papillary renal cell carcinoma]]. | |||
*[[Renal papillary adenoma|Papillary adenoma]]. | |||
*[[Chromophobe renal cell carcinoma]]. | |||
*[[Renal oncocytoma|Oncocytoma]]. | |||
Less common: | |||
*[[Multilocular clear cell renal cell carcinoma]]. | |||
* | *[[Carcinoma of the collecting ducts of Bellini]]. | ||
* | *[[Renal cell carcinoma, unclassified]]. | ||
* | *[[Renal medullary carcinoma]]. | ||
*[[Renal tumour with Xp11.2 translocation|Xp11 translocation carcinoma]]. | |||
*[[Mucinous tubular and spindle cell carcinoma]]. | |||
*Carcinoma associated with neuroblastoma. | |||
=== | ===Metanephric tumours=== | ||
* | *[[Metanephric adenoma]]. | ||
* | *[[Metanephric stromal tumour]]. | ||
* | *[[Metanephric adenofibroma]]. | ||
* | ===Nephroblastic tumours=== | ||
* | *Nephrogenic rests. | ||
*[[Nephroblastoma]]. | |||
=== | ===Mesenchymal tumours=== | ||
Childhood: | |||
* | *[[Clear cell sarcoma of the kidney]]. | ||
* | *[[Rhabdoid tumour]]. | ||
* | *[[Mesoblastic nephroma|Congenital mesoblastic nephroma]]. | ||
Adults: | |||
*Unique to kidney: | |||
**[[Juxtaglomerular cell tumour]]. | |||
**[[Renomedullary interstitial cell tumour]]. | |||
Other: | |||
*[[Angiomyolipoma]]. | |||
*[[Epithelioid angiomyolipoma]]. | |||
*[[Leiomyosarcoma]]. | |||
*[[Angiosarcoma]]. | |||
*[[Pleomorphic undifferentiated sarcoma]]. | |||
*[[Hemangiopericytoma]]. | |||
*[[Solitary fibrous tumour]]. | |||
*[[Osteosarcoma]]. | |||
*[[Schwannoma]]. | |||
===Mixed mesenchymal and epithelial tumours=== | |||
* | *[[Cystic nephroma]]. | ||
*[[Mixed epithelial and stromal tumour]]. | |||
*[[Synovial sarcoma]]. | |||
===Others=== | |||
* | *[[Neuroendocrine tumours]]. | ||
*Hematologic tumours. | |||
*[[Germ cell tumour]]s. | |||
*[[Metastases]]. | |||
== | ==Vancouver modification of WHO classification== | ||
=== | In 2012/2013, several additions were made:<ref name=pmid24025519>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | last3 = Eble | first3 = JN. | last4 = Egevad | first4 = L. | last5 = Epstein | first5 = JI. | last6 = Grignon | first6 = D. | last7 = Hes | first7 = O. | last8 = Moch | first8 = H. | last9 = Montironi | first9 = R. | title = The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia. | journal = Am J Surg Pathol | volume = 37 | issue = 10 | pages = 1469-89 | month = Oct | year = 2013 | doi = 10.1097/PAS.0b013e318299f2d1 | PMID = 24025519 }}</ref> | ||
*[[Tubulocystic renal cell carcinoma]]. | |||
* | *[[Acquired cystic disease associated renal cell carcinoma]]. | ||
*[[Clear cell papillary renal cell carcinoma]] (clear cell tubulopapillary renal cell carcinoma). | |||
*[[Hereditary leiomyomatosis renal cell carcinoma syndrome associated renal cell carcinoma]]. | |||
*MiT family translocation renal cell carcinoma - includes: | |||
**[[t(6;11) renal cell carcinoma]]. | |||
"Emerging" entities (as per Vancouver) are: | |||
* | *[[Thyroid-like follicular renal cell carcinoma]]. | ||
*[[Succinate dehydrogenase-deficient renal cell carcinoma]]. | |||
*[[ALK translocation renal cell carcinoma]]. | |||
== | ==Entities proposed after Vancouver== | ||
*[[Eosinophilic, solid and cystic renal cell carcinoma]] - part of 2022 WHO Classification. | |||
* | *[[Biphasic hyalinizing psammomatous renal cell carcinoma]]. | ||
*[[Papillary renal neoplasm with reverse polarity]]. | |||
* | *[[Low-grade oncocytic renal tumour]]. | ||
* | |||
=Renal cell carcinoma= | |||
*'' | ==Overview== | ||
* | ===General=== | ||
* | *Relatively common form of cancer. | ||
* | *Often abbreviated '''RCC'''. | ||
*[[AKA]] ''hypernephroma''.<ref>URL:[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001544/ http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001544/]. Accessed on: 14 July 2011.</ref> | |||
*RCC represents approx. 90% of malignancies in kidneys of adults.<ref name=Ref_WMSP289>{{Ref WMSP|289}}</ref> | |||
===Origin=== | |||
*Proximal renal tubule. | |||
===Clinical=== | |||
* | *Classically described as a triad:<ref name=schmid>{{cite journal |author=Schmid HP, Szabo J |title=[Renal cell carcinoma--a current review] |language=German |journal=Praxis (Bern 1994) |volume=86 |issue=20 |pages=837?3 |year=1997 |month=May |pmid=9312811 |doi= |url=}}</ref> | ||
**Hematuria (most common symptom). | |||
**Abdominal mass. | |||
**Flank pain. | |||
*Frequently picked-up on imaging (incidentaloma) ~ 1/3 of cases. | |||
===Risk factors=== | |||
*[ | *[[Smoking]] - most important.<ref name=Ref_WMSP289>{{Ref WMSP|289}}</ref> | ||
*Chemical exposures (arsenic, asbestos, cadmium, organic solvents, pesticides, fungal toxins).<ref name=Ref_WMSP289>{{Ref WMSP|289}}</ref> | |||
*Chronic renal failure. | |||
**[[Acquired cystic renal disease]]. | |||
*Male>female (~2:1). | |||
*Hereditary - familial syndromes (see [[Hereditary RCC]]). | |||
*[[Obesity]].<ref name=pmid8770461>{{Cite journal | last1 = Chow | first1 = WH. | last2 = McLaughlin | first2 = JK. | last3 = Mandel | first3 = JS. | last4 = Wacholder | first4 = S. | last5 = Niwa | first5 = S. | last6 = Fraumeni | first6 = JF. | title = Obesity and risk of renal cell cancer. | journal = Cancer Epidemiol Biomarkers Prev | volume = 5 | issue = 1 | pages = 17-21 | month = Jan | year = 1996 | doi = | PMID = 8770461 }}</ref> | |||
===Clear cell | ===Subtypes of RCC=== | ||
*Papillary | RCC (renal cell carcinoma) comes in different subtypes:<ref name=Ref_PBoD1016>{{Ref PBoD|1016}}</ref> | ||
*Clear cell carcinoma (70-80% of RCC) -- abbrev. CCRCC. | |||
*Papillary renal cell carcinoma (10-15% of RCC) -- abbrev. PRCC. | |||
*Chromophobe renal carcinoma (5% of RCC) -- abbrev. ChRCC. | |||
*Collecting duct (Bellini duct) carcinoma (1% of RCC). | |||
== | Notes: | ||
=== | *Subtype is an independent predictor of mortality - but adds very little to multivariate models with staging information.<ref name=pmid19076149>{{Cite journal | last1 = Capitanio | first1 = U. | last2 = Cloutier | first2 = V. | last3 = Zini | first3 = L. | last4 = Isbarn | first4 = H. | last5 = Jeldres | first5 = C. | last6 = Shariat | first6 = SF. | last7 = Perrotte | first7 = P. | last8 = Antebi | first8 = E. | last9 = Patard | first9 = JJ. | title = A critical assessment of the prognostic value of clear cell, papillary and chromophobe histological subtypes in renal cell carcinoma: a population-based study. | journal = BJU Int | volume = 103 | issue = 11 | pages = 1496-500 | month = Jun | year = 2009 | doi = 10.1111/j.1464-410X.2008.08259.x | PMID = 19076149 }}</ref> | ||
* | *CCRCC tends to be worse than ChRCC and PRCC, probably due to higher incidence of mets.<ref name=pmid17886093>{{Cite journal | last1 = Delahunt | first1 = B. | last2 = Bethwaite | first2 = PB. | last3 = Nacey | first3 = JN. | title = Outcome prediction for renal cell carcinoma: evaluation of prognostic factors for tumours divided according to histological subtype. | journal = Pathology | volume = 39 | issue = 5 | pages = 459-65 | month = Oct | year = 2007 | doi = 10.1080/00313020701570061 | PMID = 17886093 }}</ref> | ||
*The exam answer (worst to best): clear cell RCC, papillary RCC, chromophobe RCC. | |||
===IHC - is it RCC?=== | |||
*RCC Ma (+), CD10 (+) -- specific for RCC<ref>{{cite journal |author=Zhou M, Roma A, Magi-Galluzzi C |title=The usefulness of immunohistochemical markers in the differential diagnosis of renal neoplasms |journal=Clin. Lab. Med. |volume=25 |issue=2 |pages=247?7 |year=2005 |month=June |pmid=15848735 |doi=10.1016/j.cll.2005.01.004 |url=}}</ref> | |||
=== | ===IHC - differentiation of types=== | ||
* | *Clear cell RCC vs. papillary RCC: | ||
* | ** CK7 (-ve CCRCC), AMACR (+ve in PRCC).<ref name=pmid15848735>{{cite journal |author=Zhou M, Roma A, Magi-Galluzzi C |title=The usefulness of immunohistochemical markers in the differential diagnosis of renal neoplasms |journal=Clin. Lab. Med. |volume=25 |issue=2 |pages=247?7 |year=2005 |month=June |pmid=15848735 |doi=10.1016/j.cll.2005.01.004 |url=}}</ref> | ||
* | *Papillary RCC type 1 vs. papillary RCC type 2: | ||
** E-cadherin +ve in PRCC type 2.<ref name=pmid14657952>{{cite journal |author=Langner C, Ratschek M, Rehak P, Schips L, Zigeuner R |title=Expression of MUC1 (EMA) and E-cadherin in renal cell carcinoma: a systematic immunohistochemical analysis of 188 cases |journal=Mod. Pathol. |volume=17 |issue=2 |pages=180? |year=2004 |month=February |pmid=14657952 |doi=10.1038/modpathol.3800032 |url=}}</ref> | |||
**[[EMA]] (MUC1) +ve in PRCC type 1.<ref name=pmid14657952/> | |||
=== | *ChRCC vs. oncocytoma (ONC): | ||
** CK7 (ChRCC +ve membrane), CK20, CD15.<ref name=pmid15848735/> | |||
** CK7 -- ChRCC 86% +ve vs. ONC 0% +ve.<ref name=pmid17683191>{{cite journal |author=Liu L, Qian J, Singh H, Meiers I, Zhou X, Bostwick DG |title=Immunohistochemical analysis of chromophobe renal cell carcinoma, renal oncocytoma, and clear cell carcinoma: an optimal and practical panel for differential diagnosis |journal=Arch. Pathol. Lab. Med. |volume=131 |issue=8 |pages=1290? |year=2007 |month=August |pmid=17683191 |doi= |url=http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=131&page=1290 }}</ref> | |||
* | ** CD15 -- ChRCC 11% +ve vs. ONC 57% +ve.<ref name=pmid15500648>{{cite journal |author=Pan CC, Chen PC, Ho DM |title=The diagnostic utility of MOC31, BerEP4, RCC marker and CD10 in the classification of renal cell carcinoma and renal oncocytoma: an immunohistochemical analysis of 328 cases |journal=Histopathology |volume=45 |issue=5 |pages=452? |year=2004 |month=November |pmid=15500648 |doi=10.1111/j.1365-2559.2004.01962.x |url=}}</ref> | ||
** Hale's colloidal iron +ve in ChRCC, usually neg. in ONC.<ref name=pmid18603673>{{cite journal |author=Geramizadeh B, Ravanshad M, Rahsaz M |title=Useful markers for differential diagnosis of oncocytoma, chromophobe renal cell carcinoma and conventional renal cell carcinoma |journal=Indian J Pathol Microbiol |volume=51 |issue=2 |pages=167?1 |year=2008 |pmid=18603673 |doi= |url=http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2008;volume=51;issue=2;spage=167;epage=171;aulast=Geramizadeh }}</ref> | |||
** PAX2 -- ChRCC (1/11) +ve vs. ONC (20/23) +ve.<ref name=pmid17210525>{{cite journal |author=Memeo L, Jhang J, Assaad AM, ''et al.'' |title=Immunohistochemical analysis for cytokeratin 7, KIT, and PAX2: value in the differential diagnosis of chromophobe cell carcinoma |journal=Am. J. Clin. Pathol. |volume=127 |issue=2 |pages=225–9 |year=2007 |month=February |pmid=17210525 |doi=10.1309/9KWEA4W9Y94D1AEE |url=http://ajcp.ascpjournals.org/cgi/pmidlookup?view=long&pmid=17210525}}</ref> | |||
**Kidney-specific cadherin (Ksp-cadherin) -- ChRCC 97% +ve (distinctive membrane pattern) vs. ONC only 3% +ve.<ref name=pmid15712178>{{cite journal |author=Mazal PR, Exner M, Haitel A, ''et al.'' |title=Expression of kidney-specific cadherin distinguishes chromophobe renal cell carcinoma from renal oncocytoma |journal=Hum. Pathol. |volume=36 |issue=1 |pages=22–8 |year=2005 |month=January |pmid=15712178 |doi=10.1016/j.humpath.2004.09.011 |url=}}</ref> | |||
*ChRCC & renal oncocytoma vs. others: | |||
* | ** CD117 (ckit) +ve (100% membrane, ~75% cytoplasmic).<ref>{{cite journal |author=Krueger S, Sotlar K, Kausch I, Horny HP |title=Expression of KIT (CD117) in renal cell carcinoma and renal oncocytoma |journal=Oncology |volume=68 |issue=2-3 |pages=269-75 |year=2005 |pmid=16015044 |doi=10.1159/000086783 |url=}}</ref> | ||
* | *Clear cell RCC vs. chromophobe RCC: | ||
* | **Hale's colloidal iron (+ve in ChRCC).<ref name=pmid18603673/> | ||
**CK7 (cell membrane +ve in ChRCC). | |||
Notes: | |||
=== | *One paper<ref>{{cite journal |author=Martignoni G, Brunelli M, Gobbo S, ''et al'' |title=Role of molecular markers in diagnosis and prognosis of renal cell carcinoma |journal=Anal. Quant. Cytol. Histol. |volume=29 |issue=1 |pages=41? |year=2007 |month=February |pmid=17375873 |doi= |url=}}</ref> describes CD10, parvalbumin, AMACR, CK7 and S100A1 as being useful. | ||
* | *Another paper I came across:<ref>{{cite journal |author=Avery AK, Beckstead J, Renshaw AA, Corless CL |title=Use of antibodies to RCC and CD10 in the differential diagnosis of renal neoplasms |journal=Am. J. Surg. Pathol. |volume=24 |issue=2 |pages=203?0 |year=2000 |month=February |pmid=10680888 |doi= |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0147-5185&volume=24&issue=2&spage=203}}</ref> | ||
*c-kit (CD117) not useful for differentiating ONC and ChRCC.<ref name=pmid17210525>{{cite journal |author=Memeo L, Jhang J, Assaad AM, ''et al.'' |title=Immunohistochemical analysis for cytokeratin 7, KIT, and PAX2: value in the differential diagnosis of chromophobe cell carcinoma |journal=Am. J. Clin. Pathol. |volume=127 |issue=2 |pages=225–9 |year=2007 |month=February |pmid=17210525 |doi=10.1309/9KWEA4W9Y94D1AEE |url=http://ajcp.ascpjournals.org/cgi/pmidlookup?view=long&pmid=17210525}}</ref> | |||
*E-cadherin ''not'' useful for differentiating ChRCC and ONC.<ref name=pmid12613443>{{cite journal |author=Kim MK, Kim S |title=Immunohistochemical profile of common epithelial neoplasms arising in the kidney |journal=Appl. Immunohistochem. Mol. Morphol. |volume=10 |issue=4 |pages=332–8 |year=2002 |month=December |pmid=12613443 |doi= |url=}}</ref> | |||
===RCC vs. Urothelial cell carcinoma=== | |||
{{main|Urothelium}} | |||
*Clinically/radiologically, it may not be possible to differentiate renal pelvis UCC and RCC if the tumour is large. | |||
* | *Pathologically, this is not very difficult. | ||
** | *On gross specimens, it is almost always obvious what one is dealing with: | ||
** | **[[UCC]] = ''[[nephroureterectomy]]''. | ||
**[[RCC]] = ''[[partial nephrectomy]]'', ''nephrectomy'' or ''[[radical nephrectomy]]''. | |||
== | ===Renal cell carcinoma with sarcomatoid differentiation=== | ||
*[[AKA]] ''sarcomatoid renal cell carcinoma''. | |||
* | {{Main|Renal cell carcinoma with sarcomatoid differentiation}} | ||
=== | ===Renal cell carcinoma with rhabdoid morphology=== | ||
*[[AKA]] ''renal cell carcinoma with rhabdoid change''. | |||
{{Main|Renal cell carcinoma with rhabdoid morphology}} | |||
*[[ | |||
==Hereditary renal cell carcinoma== | |||
{{Main|Hereditary renal cell carcinoma}} | |||
== | ==Renal cell carcinoma grading== | ||
{{Main|Renal cell carcinoma grading}} | |||
= | ==Renal cell carcinoma staging== | ||
{{Main|Kidney cancer staging}} | |||
== | ===Renal sinus invasion=== | ||
=== | {{Main|Kidney cancer staging}} | ||
=== | ==Clear cell renal cell carcinoma== | ||
{{Main|Clear cell renal cell carcinoma}} | |||
==Multilocular cystic renal cell carcinoma== | |||
{{Main|Multilocular cystic renal cell carcinoma}} | |||
=== | ==Papillary renal cell carcinoma== | ||
{{Main|Papillary renal cell carcinoma}} | |||
==Chromophobe renal cell carcinoma== | |||
{{Main|Chromophobe renal cell carcinoma}} | |||
==Clear cell papillary renal cell tumour== | |||
In the past, it was known as ''clear cell papillary renal cell carcinoma''. | |||
{{Main|Clear cell papillary renal cell tumour}} | |||
== | ==Unclassified renal cell carcinoma== | ||
*Abbreviated ''URCC''. | |||
{{Main|Unclassified renal cell carcinoma}} | |||
* | |||
=== | =Renal translocation carcinomas= | ||
==Renal tumour with Xp11.2 translocation== | |||
{{Main|Renal tumour with Xp11.2 translocation}} | |||
=== | ==Renal tumour with t(6;11) translocation== | ||
*[[AKA]] ''t(6;11) renal cell carcinoma''. | |||
* | {{main|Renal tumour with t(6;11) translocation}} | ||
==== | =Benign tumours= | ||
* | ==Papillary adenoma of the kidney== | ||
*[[AKA]] ''renal papillary adenoma''. | |||
{{Main|Papillary adenoma of the kidney}} | |||
=== | ==Renal oncocytoma== | ||
{{Main|Renal oncocytoma}} | |||
==Angiomyolipoma== | |||
* | *Abbreviated ''AML''. | ||
{{Main|Angiomyolipoma}} | |||
=Mimics= | |||
==Xanthogranulomatous pyelonephritis== | ==Xanthogranulomatous pyelonephritis== | ||
*Abbreviated ''XGP''. | |||
* | {{Main|Xanthogranulomatous pyelonephritis}} | ||
=== | ==Malakoplakia== | ||
{{main|Malakoplakia}} | |||
=Rare stuffs= | |||
*[ | ==Juxtaglomerular cell tumour== | ||
*[[AKA]] juxtaglomerular tumour, reninoma.<ref name=pmid18192852>{{Cite journal | last1 = Wong | first1 = L. | last2 = Hsu | first2 = TH. | last3 = Perlroth | first3 = MG. | last4 = Hofmann | first4 = LV. | last5 = Haynes | first5 = CM. | last6 = Katznelson | first6 = L. | title = Reninoma: case report and literature review. | journal = J Hypertens | volume = 26 | issue = 2 | pages = 368-73 | month = Feb | year = 2008 | doi = 10.1097/HJH.0b013e3282f283f3 | PMID = 18192852 }}</ref> | |||
{{Main|Juxtaglomerular cell tumour}} | |||
=== | ==Renomedullary interstitial cell tumour== | ||
*[[AKA]] ''medullary fibroma''.<ref name=pmid11054036 >{{Cite journal | last1 = Bircan | first1 = S. | last2 = Orhan | first2 = D. | last3 = Tulunay | first3 = O. | last4 = Safak | first4 = M. | title = Renomedullary interstitial cell tumor. | journal = Urol Int | volume = 65 | issue = 3 | pages = 163-6 | month = | year = 2000 | doi = | PMID = 11054036 }}</ref> | |||
{{Main|Renomedullary interstitial cell tumour}} | |||
==Metanephric adenoma== | |||
*[[ | *Should '''not''' be confused ''[[mesonephric adenoma]]'', another term for ''nephrogenic adenoma''. | ||
** | **Memory device: me'''t'''anephric adenoma is a '''t'''umour. | ||
{{Main|Metanephric adenoma}} | |||
== | ==Renal epithelial and stromal tumour== | ||
{{ | :Abbreviated ''REST''. | ||
The lumping term for both:<ref name=pmid17414095>{{Cite journal | last1 = Turbiner | first1 = J. | last2 = Amin | first2 = MB. | last3 = Humphrey | first3 = PA. | last4 = Srigley | first4 = JR. | last5 = De Leval | first5 = L. | last6 = Radhakrishnan | first6 = A. | last7 = Oliva | first7 = E. | title = Cystic nephroma and mixed epithelial and stromal tumor of kidney: a detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumor (REST) as a unifying term. | journal = Am J Surg Pathol | volume = 31 | issue = 4 | pages = 489-500 | month = Apr | year = 2007 | doi = 10.1097/PAS.0b013e31802bdd56 | PMID = 17414095 }}</ref> | |||
#[[Mixed epithelial and stromal tumour]]. | |||
#[[Cystic nephroma]]. | |||
== | ==Mixed epithelial and stromal tumour== | ||
*Abbreviated ''MEST''. | |||
* | {{Main|Mixed epithelial and stromal tumour of the kidney}} | ||
== | ==Cystic nephroma== | ||
{{Main|Cystic nephroma}} | |||
=== | ==Renal mucinous tubular and spindle cell carcinoma== | ||
*[[AKA]] ''renal mucinous tubular spindle cell carcinoma''. | |||
*[[AKA]] ''mucinous tubular and spindle cell carcinoma of the kidney''.<ref name=pmid16258504>{{Cite journal | last1 = Brandal | first1 = P. | last2 = Lie | first2 = AK. | last3 = Bassarova | first3 = A. | last4 = Svindland | first4 = A. | last5 = Risberg | first5 = B. | last6 = Danielsen | first6 = H. | last7 = Heim | first7 = S. | title = Genomic aberrations in mucinous tubular and spindle cell renal cell carcinomas. | journal = Mod Pathol | volume = 19 | issue = 2 | pages = 186-94 | month = Feb | year = 2006 | doi = 10.1038/modpathol.3800499 | PMID = 16258504 }}</ref> | |||
{{Main|Renal mucinous tubular and spindle cell carcinoma}} | |||
== | ==Collecting duct carcinoma== | ||
{{Main|Collecting duct carcinoma}} | |||
= | ==Renal medullary carcinoma== | ||
{{Main|Renal medullary carcinoma}} | |||
== | ==Tubulocystic carcinoma of the kidney== | ||
{{Main|Tubulocystic carcinoma of the kidney}} | |||
== | ==Acquired cystic disease-associated renal cell carcinoma== | ||
{{Main|Acquired cystic disease-associated renal cell carcinoma}} | |||
== | ==Kidney metastasis== | ||
* | *[[AKA]] ''renal metastasis'', ''metastatic kidney disease''. | ||
{{Main|Kidney metastasis}} | |||
=Pediatric= | |||
== | {{Main|Pediatric kidney tumours}} | ||
The most common is [[nephroblastoma]] (Wilms tumour). | |||
Others include: | |||
* | *[[Metanephric stromal tumour]]. | ||
*[[Metanephric adenofibroma]] | |||
*[[Metanephric adenoma]]. | |||
*[[Clear cell sarcoma of the kidney]]. | |||
== | =See also= | ||
* | *[[Urinary bladder]]. | ||
* | *[[Medical kidney]]. | ||
*[[Malakoplakia]] - yellow lesion on gross; may mimic RCC. | |||
== | =References= | ||
{{reflist|2}} | |||
= | =External links= | ||
*[http://www.uscap.org/site~/99th/pdf/companion13h03.pdf Renal tumours with eosinophilic cytoplasm (uscap.org)]. | |||
[[Category: Genitourinary pathology]] | [[Category: Genitourinary pathology]] | ||
Latest revision as of 20:49, 29 November 2024

Kidney tumours - includes malignant kidney tumours (kidney cancer) and benign kidney tumours. Medical renal diseases are dealt with in the medical renal diseases article.
Pediatric kidney tumours are dealt with in the pediatric kidney tumours article.
Renal specimens
- Renal biopsy - usually for renal oncocytoma vs. renal cell carcinoma (RCC) or medical diseases - see medical kidney.
- Partial nephrectomy.
- Nephrectomy.
- Nephroureterectomy (includes ureter) - done for urothelial cell carcinoma (UCC) of the renal pelvis and ureteric UCC.
- Radical nephrectomy - includes Gerota's fascia.
- May include the adrenal gland.[1]
In excisions done for tumours, a comment should be made about kidney distant from the tumour. People with less renal mass, i.e. less kidney, are predisposed to focal segmental glomerulosclerosis (FSGS).
Anatomy
Layers (superficial to deep):
- Renal fascia (Gerota's fascia).
- Perinephric fat.
- Renal capsule.
- Renal parenchyma (cortex).
Sign out
Missed renal biopsy
Tabular comparison (selected tumours)
Selected common tumours of the kidney:[2][3]
| Clear cell RCC | Papillary RCC type 1 |
Papillary RCC type 2 |
Chromophobe RCC classic variant |
Chromophobe RCC eosinophilic variant |
Oncocytoma | |
| Gross | Golden yellow, solid | friable | friable | light brown | light brown | mahogany/brown, +/-central scar |
| Architecture | nests, sheets | papillary, simple | papillary, pseudostratified |
nests, sheets | nests, sheets | nests, sheets |
| Nuclear atypia | low-high typically medium-high |
low-medium | medium-high | low-high, "raisinoid" nuc. membrane |
low-high, "raisinoid" nuc. membrane |
low-medium, round nuclei |
| Cytoplasm | clear | eosinophilic | eosinophilic | cobwebs/clear | eosinophilic/cobwebs | eosinophilic/ granular & abundant |
| Other | delicate vessels, necrosis common |
histiocytes in fibrovascular cores, >0.5 cm |
histiocytes in fibrovascular cores, >0.5 cm |
perinuclear clearing, thick vessels | perinuclear clearing, thick vessels | in loose fibrous/hyaline stroma |
| IHC | CK7-, EMA+ | AMACR+, EMA+, CK7+ | AMACR+, E-cadherin+, CK7- | CD117+, CK7+ (membrane) | CD117+, CK7+ (membrane) | Vimentin-, EMA+ |
| Main DDx | chromophobe classic variant |
PaRCC type 2, mets | PaRCC type 1, mets | clear cell RCC | oncocytoma | chromophobe eosinophilic variant |
| Key features | clear cells, vascular | papillae, histiocytes simple epithelium |
papillae, histiocytes, stratified |
perinuc. clearing, wispy cytoplasm |
perinuc. clearing, wispy eosinophilic cytoplasm |
eosinophilic, granular cytoplasm |
| Image(s) | , |
Notes:
- Cell shape: all have epithelioid morphology.
Tabular comparison of oncocytoma and chromophobe RCC
Histomorphologic features useful to distinguish chromophobe RCC (eosinophilic variant) and oncocytoma:[4]
| Morphologic feature | ChRCC (eosinophilic variant) |
Renal oncocytoma |
|---|---|---|
| Nuclear morphology | "raisinoid"/wrinkled appearance | round with small nucleolus, usu. little size variation |
| Multinucleation | common - binucleation | uncommon |
| Chromatin | coarse | fine |
| Architecture | solid, crowded nests | spaced nests / archipelago-like, solid |
| Cytoplasm | perinuclear halo, may be focal | no perinuclear halo |
| Degenerative foci (focal atypia & pleomorphism) |
absent | present in ~20% of cases |
| Image |
Common DDx
Spindle cell tumours
Malignant spindle cell tumours of the kidney:
- Renal cell carcinoma with sarcomatoid differentiation.
- Renal mucinous tubular and spindle cell carcinoma.
- Wilms tumour.
- Renal cell carcinoma, unclassified.
Benign spindle cell tumours of the kidney:
Renal tumours with eosinophilic cytoplasm
WHO classification of renal neoplasia
- Based on 2004 iteration - as per WMSP, slightly modified.[5] Online, the classification can found here.
Renal cell tumours
Common:
- Clear cell renal cell carcinoma.
- Papillary renal cell carcinoma.
- Papillary adenoma.
- Chromophobe renal cell carcinoma.
- Oncocytoma.
Less common:
- Multilocular clear cell renal cell carcinoma.
- Carcinoma of the collecting ducts of Bellini.
- Renal cell carcinoma, unclassified.
- Renal medullary carcinoma.
- Xp11 translocation carcinoma.
- Mucinous tubular and spindle cell carcinoma.
- Carcinoma associated with neuroblastoma.
Metanephric tumours
Nephroblastic tumours
- Nephrogenic rests.
- Nephroblastoma.
Mesenchymal tumours
Childhood:
Adults:
- Unique to kidney:
Other:
- Angiomyolipoma.
- Epithelioid angiomyolipoma.
- Leiomyosarcoma.
- Angiosarcoma.
- Pleomorphic undifferentiated sarcoma.
- Hemangiopericytoma.
- Solitary fibrous tumour.
- Osteosarcoma.
- Schwannoma.
Mixed mesenchymal and epithelial tumours
Others
- Neuroendocrine tumours.
- Hematologic tumours.
- Germ cell tumours.
- Metastases.
Vancouver modification of WHO classification
In 2012/2013, several additions were made:[6]
- Tubulocystic renal cell carcinoma.
- Acquired cystic disease associated renal cell carcinoma.
- Clear cell papillary renal cell carcinoma (clear cell tubulopapillary renal cell carcinoma).
- Hereditary leiomyomatosis renal cell carcinoma syndrome associated renal cell carcinoma.
- MiT family translocation renal cell carcinoma - includes:
"Emerging" entities (as per Vancouver) are:
- Thyroid-like follicular renal cell carcinoma.
- Succinate dehydrogenase-deficient renal cell carcinoma.
- ALK translocation renal cell carcinoma.
Entities proposed after Vancouver
- Eosinophilic, solid and cystic renal cell carcinoma - part of 2022 WHO Classification.
- Biphasic hyalinizing psammomatous renal cell carcinoma.
- Papillary renal neoplasm with reverse polarity.
- Low-grade oncocytic renal tumour.
Renal cell carcinoma
Overview
General
- Relatively common form of cancer.
- Often abbreviated RCC.
- AKA hypernephroma.[7]
- RCC represents approx. 90% of malignancies in kidneys of adults.[8]
Origin
- Proximal renal tubule.
Clinical
- Classically described as a triad:[9]
- Hematuria (most common symptom).
- Abdominal mass.
- Flank pain.
- Frequently picked-up on imaging (incidentaloma) ~ 1/3 of cases.
Risk factors
- Smoking - most important.[8]
- Chemical exposures (arsenic, asbestos, cadmium, organic solvents, pesticides, fungal toxins).[8]
- Chronic renal failure.
- Male>female (~2:1).
- Hereditary - familial syndromes (see Hereditary RCC).
- Obesity.[10]
Subtypes of RCC
RCC (renal cell carcinoma) comes in different subtypes:[11]
- Clear cell carcinoma (70-80% of RCC) -- abbrev. CCRCC.
- Papillary renal cell carcinoma (10-15% of RCC) -- abbrev. PRCC.
- Chromophobe renal carcinoma (5% of RCC) -- abbrev. ChRCC.
- Collecting duct (Bellini duct) carcinoma (1% of RCC).
Notes:
- Subtype is an independent predictor of mortality - but adds very little to multivariate models with staging information.[12]
- CCRCC tends to be worse than ChRCC and PRCC, probably due to higher incidence of mets.[13]
- The exam answer (worst to best): clear cell RCC, papillary RCC, chromophobe RCC.
IHC - is it RCC?
- RCC Ma (+), CD10 (+) -- specific for RCC[14]
IHC - differentiation of types
- Clear cell RCC vs. papillary RCC:
- CK7 (-ve CCRCC), AMACR (+ve in PRCC).[15]
- Papillary RCC type 1 vs. papillary RCC type 2:
- ChRCC vs. oncocytoma (ONC):
- CK7 (ChRCC +ve membrane), CK20, CD15.[15]
- CK7 -- ChRCC 86% +ve vs. ONC 0% +ve.[17]
- CD15 -- ChRCC 11% +ve vs. ONC 57% +ve.[18]
- Hale's colloidal iron +ve in ChRCC, usually neg. in ONC.[19]
- PAX2 -- ChRCC (1/11) +ve vs. ONC (20/23) +ve.[20]
- Kidney-specific cadherin (Ksp-cadherin) -- ChRCC 97% +ve (distinctive membrane pattern) vs. ONC only 3% +ve.[21]
- ChRCC & renal oncocytoma vs. others:
- CD117 (ckit) +ve (100% membrane, ~75% cytoplasmic).[22]
- Clear cell RCC vs. chromophobe RCC:
- Hale's colloidal iron (+ve in ChRCC).[19]
- CK7 (cell membrane +ve in ChRCC).
Notes:
- One paper[23] describes CD10, parvalbumin, AMACR, CK7 and S100A1 as being useful.
- Another paper I came across:[24]
- c-kit (CD117) not useful for differentiating ONC and ChRCC.[20]
- E-cadherin not useful for differentiating ChRCC and ONC.[25]
RCC vs. Urothelial cell carcinoma
- Clinically/radiologically, it may not be possible to differentiate renal pelvis UCC and RCC if the tumour is large.
- Pathologically, this is not very difficult.
- On gross specimens, it is almost always obvious what one is dealing with:
- UCC = nephroureterectomy.
- RCC = partial nephrectomy, nephrectomy or radical nephrectomy.
Renal cell carcinoma with sarcomatoid differentiation
- AKA sarcomatoid renal cell carcinoma.
Renal cell carcinoma with rhabdoid morphology
- AKA renal cell carcinoma with rhabdoid change.
Hereditary renal cell carcinoma
Renal cell carcinoma grading
Renal cell carcinoma staging
Renal sinus invasion
Clear cell renal cell carcinoma
Multilocular cystic renal cell carcinoma
Papillary renal cell carcinoma
Chromophobe renal cell carcinoma
Clear cell papillary renal cell tumour
In the past, it was known as clear cell papillary renal cell carcinoma.
Unclassified renal cell carcinoma
- Abbreviated URCC.
Renal translocation carcinomas
Renal tumour with Xp11.2 translocation
Renal tumour with t(6;11) translocation
- AKA t(6;11) renal cell carcinoma.
Benign tumours
Papillary adenoma of the kidney
- AKA renal papillary adenoma.
Renal oncocytoma
Angiomyolipoma
- Abbreviated AML.
Mimics
Xanthogranulomatous pyelonephritis
- Abbreviated XGP.
Malakoplakia
Rare stuffs
Juxtaglomerular cell tumour
Renomedullary interstitial cell tumour
Metanephric adenoma
- Should not be confused mesonephric adenoma, another term for nephrogenic adenoma.
- Memory device: metanephric adenoma is a tumour.
Renal epithelial and stromal tumour
- Abbreviated REST.
The lumping term for both:[28]
Mixed epithelial and stromal tumour
- Abbreviated MEST.
Cystic nephroma
Renal mucinous tubular and spindle cell carcinoma
- AKA renal mucinous tubular spindle cell carcinoma.
- AKA mucinous tubular and spindle cell carcinoma of the kidney.[29]
Collecting duct carcinoma
Renal medullary carcinoma
Tubulocystic carcinoma of the kidney
Acquired cystic disease-associated renal cell carcinoma
Kidney metastasis
- AKA renal metastasis, metastatic kidney disease.
Pediatric
The most common is nephroblastoma (Wilms tumour).
Others include:
- Metanephric stromal tumour.
- Metanephric adenofibroma
- Metanephric adenoma.
- Clear cell sarcoma of the kidney.
See also
- Urinary bladder.
- Medical kidney.
- Malakoplakia - yellow lesion on gross; may mimic RCC.
References
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 288. ISBN 978-0781765275.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 281-304. ISBN 978-0443066771.
- ↑ Srigley, JR.; Delahunt, B. (Jun 2009). "Uncommon and recently described renal carcinomas.". Mod Pathol 22 Suppl 2: S2-S23. doi:10.1038/modpathol.2009.70. PMID 19494850.
- ↑ Tickoo, SK.; Amin, MB. (Dec 1998). "Discriminant nuclear features of renal oncocytoma and chromophobe renal cell carcinoma. Analysis of their potential utility in the differential diagnosis.". Am J Clin Pathol 110 (6): 782-7. PMID 9844591.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 291. ISBN 978-0781765275.
- ↑ Srigley, JR.; Delahunt, B.; Eble, JN.; Egevad, L.; Epstein, JI.; Grignon, D.; Hes, O.; Moch, H. et al. (Oct 2013). "The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia.". Am J Surg Pathol 37 (10): 1469-89. doi:10.1097/PAS.0b013e318299f2d1. PMID 24025519.
- ↑ URL:http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001544/. Accessed on: 14 July 2011.
- ↑ 8.0 8.1 8.2 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 289. ISBN 978-0781765275.
- ↑ Schmid HP, Szabo J (May 1997). "[Renal cell carcinoma--a current review]" (in German). Praxis (Bern 1994) 86 (20): 837?3. PMID 9312811.
- ↑ Chow, WH.; McLaughlin, JK.; Mandel, JS.; Wacholder, S.; Niwa, S.; Fraumeni, JF. (Jan 1996). "Obesity and risk of renal cell cancer.". Cancer Epidemiol Biomarkers Prev 5 (1): 17-21. PMID 8770461.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1016. ISBN 0-7216-0187-1.
- ↑ Capitanio, U.; Cloutier, V.; Zini, L.; Isbarn, H.; Jeldres, C.; Shariat, SF.; Perrotte, P.; Antebi, E. et al. (Jun 2009). "A critical assessment of the prognostic value of clear cell, papillary and chromophobe histological subtypes in renal cell carcinoma: a population-based study.". BJU Int 103 (11): 1496-500. doi:10.1111/j.1464-410X.2008.08259.x. PMID 19076149.
- ↑ Delahunt, B.; Bethwaite, PB.; Nacey, JN. (Oct 2007). "Outcome prediction for renal cell carcinoma: evaluation of prognostic factors for tumours divided according to histological subtype.". Pathology 39 (5): 459-65. doi:10.1080/00313020701570061. PMID 17886093.
- ↑ Zhou M, Roma A, Magi-Galluzzi C (June 2005). "The usefulness of immunohistochemical markers in the differential diagnosis of renal neoplasms". Clin. Lab. Med. 25 (2): 247?7. doi:10.1016/j.cll.2005.01.004. PMID 15848735.
- ↑ 15.0 15.1 Zhou M, Roma A, Magi-Galluzzi C (June 2005). "The usefulness of immunohistochemical markers in the differential diagnosis of renal neoplasms". Clin. Lab. Med. 25 (2): 247?7. doi:10.1016/j.cll.2005.01.004. PMID 15848735.
- ↑ 16.0 16.1 Langner C, Ratschek M, Rehak P, Schips L, Zigeuner R (February 2004). "Expression of MUC1 (EMA) and E-cadherin in renal cell carcinoma: a systematic immunohistochemical analysis of 188 cases". Mod. Pathol. 17 (2): 180?. doi:10.1038/modpathol.3800032. PMID 14657952.
- ↑ Liu L, Qian J, Singh H, Meiers I, Zhou X, Bostwick DG (August 2007). "Immunohistochemical analysis of chromophobe renal cell carcinoma, renal oncocytoma, and clear cell carcinoma: an optimal and practical panel for differential diagnosis". Arch. Pathol. Lab. Med. 131 (8): 1290?. PMID 17683191. http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=131&page=1290.
- ↑ Pan CC, Chen PC, Ho DM (November 2004). "The diagnostic utility of MOC31, BerEP4, RCC marker and CD10 in the classification of renal cell carcinoma and renal oncocytoma: an immunohistochemical analysis of 328 cases". Histopathology 45 (5): 452?. doi:10.1111/j.1365-2559.2004.01962.x. PMID 15500648.
- ↑ 19.0 19.1 Geramizadeh B, Ravanshad M, Rahsaz M (2008). "Useful markers for differential diagnosis of oncocytoma, chromophobe renal cell carcinoma and conventional renal cell carcinoma". Indian J Pathol Microbiol 51 (2): 167?1. PMID 18603673. http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2008;volume=51;issue=2;spage=167;epage=171;aulast=Geramizadeh.
- ↑ 20.0 20.1 Memeo L, Jhang J, Assaad AM, et al. (February 2007). "Immunohistochemical analysis for cytokeratin 7, KIT, and PAX2: value in the differential diagnosis of chromophobe cell carcinoma". Am. J. Clin. Pathol. 127 (2): 225–9. doi:10.1309/9KWEA4W9Y94D1AEE. PMID 17210525. http://ajcp.ascpjournals.org/cgi/pmidlookup?view=long&pmid=17210525.
- ↑ Mazal PR, Exner M, Haitel A, et al. (January 2005). "Expression of kidney-specific cadherin distinguishes chromophobe renal cell carcinoma from renal oncocytoma". Hum. Pathol. 36 (1): 22–8. doi:10.1016/j.humpath.2004.09.011. PMID 15712178.
- ↑ Krueger S, Sotlar K, Kausch I, Horny HP (2005). "Expression of KIT (CD117) in renal cell carcinoma and renal oncocytoma". Oncology 68 (2-3): 269-75. doi:10.1159/000086783. PMID 16015044.
- ↑ Martignoni G, Brunelli M, Gobbo S, et al (February 2007). "Role of molecular markers in diagnosis and prognosis of renal cell carcinoma". Anal. Quant. Cytol. Histol. 29 (1): 41?. PMID 17375873.
- ↑ Avery AK, Beckstead J, Renshaw AA, Corless CL (February 2000). "Use of antibodies to RCC and CD10 in the differential diagnosis of renal neoplasms". Am. J. Surg. Pathol. 24 (2): 203?0. PMID 10680888. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0147-5185&volume=24&issue=2&spage=203.
- ↑ Kim MK, Kim S (December 2002). "Immunohistochemical profile of common epithelial neoplasms arising in the kidney". Appl. Immunohistochem. Mol. Morphol. 10 (4): 332–8. PMID 12613443.
- ↑ Wong, L.; Hsu, TH.; Perlroth, MG.; Hofmann, LV.; Haynes, CM.; Katznelson, L. (Feb 2008). "Reninoma: case report and literature review.". J Hypertens 26 (2): 368-73. doi:10.1097/HJH.0b013e3282f283f3. PMID 18192852.
- ↑ Bircan, S.; Orhan, D.; Tulunay, O.; Safak, M. (2000). "Renomedullary interstitial cell tumor.". Urol Int 65 (3): 163-6. PMID 11054036.
- ↑ Turbiner, J.; Amin, MB.; Humphrey, PA.; Srigley, JR.; De Leval, L.; Radhakrishnan, A.; Oliva, E. (Apr 2007). "Cystic nephroma and mixed epithelial and stromal tumor of kidney: a detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumor (REST) as a unifying term.". Am J Surg Pathol 31 (4): 489-500. doi:10.1097/PAS.0b013e31802bdd56. PMID 17414095.
- ↑ Brandal, P.; Lie, AK.; Bassarova, A.; Svindland, A.; Risberg, B.; Danielsen, H.; Heim, S. (Feb 2006). "Genomic aberrations in mucinous tubular and spindle cell renal cell carcinomas.". Mod Pathol 19 (2): 186-94. doi:10.1038/modpathol.3800499. PMID 16258504.