|
|
| (126 intermediate revisions by the same user not shown) |
| Line 1: |
Line 1: |
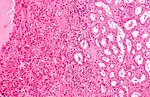
| '''[[Kidney]] tumours''' - includes '''malignant kidney tumours''' and '''benign kidney tumours'''. Medical renal diseases are dealt with in the [[medical renal diseases]] article. | | [[Image:Renal oncocytoma.jpg|thumb|250px|A kidney tumour ([[renal oncocytoma]]). (WC/Emmanuelm)]] |
| | '''[[Kidney]] tumours''' - includes '''malignant kidney tumours''' ('''kidney cancer''') and '''benign kidney tumours'''. Medical renal diseases are dealt with in the [[medical renal diseases]] article. |
|
| |
|
| Pediatric kidney tumours are dealt with in the ''[[pediatric kidney tumours]]'' article. | | Pediatric kidney tumours are dealt with in the ''[[pediatric kidney tumours]]'' article. |
|
| |
|
| =Renal specimens= | | =Renal specimens= |
| *Renal biopsy - usually for renal onocytoma vs. renal cell carcinoma (RCC) ''or'' medical diseases - see ''[[medical kidney]]''. | | *[[Renal biopsy]] - usually for [[renal oncocytoma]] vs. renal cell carcinoma (RCC) ''or'' medical diseases - see ''[[medical kidney]]''. |
| *Partial nephrectomy. | | *[[Partial nephrectomy]]. |
| *Nephrectomy. | | *[[Nephrectomy]]. |
| *Nephroureterectomy (includes ureter) - done for [[urothelial cell carcinoma]] (UCC) of the renal pelvis and ureteric UCC. | | *[[Nephroureterectomy]] (includes [[ureter]]) - done for [[urothelial cell carcinoma]] (UCC) of the renal pelvis and ureteric UCC. |
| *Radical nephrectomy - includes Gerota's fascia. | | *[[Radical nephrectomy]] - includes Gerota's fascia. |
| **May include the [[adrenal gland]].<ref name=Ref_WMSP|288>{{Ref WMSP|288}}</ref> | | **May include the [[adrenal gland]].<ref name=Ref_WMSP|288>{{Ref WMSP|288}}</ref> |
|
| |
|
| Line 14: |
Line 15: |
|
| |
|
| ==Anatomy== | | ==Anatomy== |
| The anatomy is important for properly staging renal neoplasms.
| |
|
| |
| Layers (superficial to deep): | | Layers (superficial to deep): |
| #Renal fascia (Gerota's fascia). | | #Renal fascia (Gerota's fascia). |
| Line 24: |
Line 23: |
| ===Sign out=== | | ===Sign out=== |
| ====Missed renal biopsy==== | | ====Missed renal biopsy==== |
| <pre>
| | {{Main|Missed renal biopsy}} |
| KIDNEY (LESION), LEFT, CORE BIOPSY:
| |
| - RENAL PARENCHYMA.
| |
| - NEGATIVE FOR MASS LESION, SEE COMMENT.
| |
| | |
| COMMENT:
| |
| No mass lesion is apparent in the tissue sampled. A re-biopsy should be considered.
| |
| | |
| Renal parenchyma:
| |
| - Glomeruli: seven glomeruli sampled, no apparent glomerular pathology on the H&E sections.
| |
| - Interstitium: interstitial fibrosis is not identified.
| |
| - Tubules: no pathology is apparent.
| |
| - Vessels: mild atherosclerosis, no hyalinization of arterioles apparent.
| |
| </pre>
| |
|
| |
|
| =Tabular comparison (selected tumours)= | | =Tabular comparison (selected tumours)= |
|
| |
|
| Selected common tumours of the kidney:<ref>{{Ref GUP|281-304}}</ref><ref name=pmid19494850>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 }}</ref> | | Selected common tumours of the kidney:<ref name=Ref_GUP281>{{Ref GUP|281-304}}</ref><ref name=pmid19494850>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 }}</ref> |
| {| class="wikitable" | | {| class="wikitable" |
| | | | | |
| Line 92: |
Line 78: |
| |- | | |- |
| |IHC | | |IHC |
| | CK7-, EMA+ | | | [[CK7]]-, EMA+ |
| | AMACR+, EMA+, CK7+ | | | AMACR+, EMA+, CK7+ |
| | AMACR+, E-cadherin+, CK7- | | | AMACR+, E-cadherin+, CK7- |
| Line 116: |
Line 102: |
| |- | | |- |
| |Image(s) | | |Image(s) |
| | [http://commons.wikimedia.org/wiki/File:Renal_clear_cell_ca_%281%29_Nephrectomy.jpg CCRCC (WC)] | | | [[Image:Renal_clear_cell_ca_%281%29_Nephrectomy.jpg|thumb|150px| CCRCC (WC)]] |
| | [http://commons.wikimedia.org/wiki/File:Papillary_renal_cell_carcinoma_intermed_mag.jpg PaRCC - intermed. (WC)], [http://commons.wikimedia.org/wiki/File:Papillary_renal_cell_carcinoma_very_high_mag.jpg PaRCC - high (WC)] | | | [[Image:Papillary_renal_cell_carcinoma_intermed_mag.jpg|thumb|150px| PaRCC - intermed. (WC)]], [[Image:Papillary_renal_cell_carcinoma_very_high_mag.jpg | thumb|150px| PaRCC - high (WC)]] |
| | | | | |
| | | | | |
| | [http://commons.wikimedia.org/wiki/File:Oncocytic_chromophobe_rcc_high_mag.jpg ChRCC (WC)] | | | [[Image:Oncocytic_chromophobe_rcc_high_mag.jpg|thumb|150px| ChRCC (WC)]] |
| | [http://commons.wikimedia.org/wiki/File:Renal_oncocytoma2.jpg Oncocytoma (WC)] | | | [[Image:Renal_oncocytoma2.jpg|thumb|150px| Oncocytoma (WC)]] |
| |} | | |} |
| Notes: | | Notes: |
| Line 127: |
Line 113: |
|
| |
|
| ===Tabular comparison of oncocytoma and chromophobe RCC=== | | ===Tabular comparison of oncocytoma and chromophobe RCC=== |
| Histomorphologic features useful to distinguish chromophobe RCC (eosinophilic variant) and oncocytoma:<ref name=pmid9844591>{{Cite journal | last1 = Tickoo | first1 = SK. | last2 = Amin | first2 = MB. | title = Discriminant nuclear features of renal oncocytoma and chromophobe renal cell carcinoma. Analysis of their potential utility in the differential diagnosis. | journal = Am J Clin Pathol | volume = 110 | issue = 6 | pages = 782-7 | month = Dec | year = 1998 | doi = | PMID = 9844591 }} | | Histomorphologic features useful to distinguish chromophobe RCC (eosinophilic variant) and oncocytoma:<ref name=pmid9844591>{{Cite journal | last1 = Tickoo | first1 = SK. | last2 = Amin | first2 = MB. | title = Discriminant nuclear features of renal oncocytoma and chromophobe renal cell carcinoma. Analysis of their potential utility in the differential diagnosis. | journal = Am J Clin Pathol | volume = 110 | issue = 6 | pages = 782-7 | month = Dec | year = 1998 | doi = | PMID = 9844591 }}</ref> |
| </ref> | |
| {| class="wikitable sortable" | | {| class="wikitable sortable" |
| ! Morphologic feature | | ! Morphologic feature |
| Line 159: |
Line 144: |
| |- | | |- |
| | Image | | | Image |
| | [http://commons.wikimedia.org/wiki/File:Oncocytic_chromophobe_rcc_high_mag.jpg ChRCC (WC)] | | | [[Image:Oncocytic_chromophobe_rcc_high_mag.jpg |thumb|150px|ChRCC (WC/Nephron)]] |
| | [http://commons.wikimedia.org/wiki/File:Renal_oncocytoma2.jpg Oncocytoma (WC)] | | | [[Image:Renal_oncocytoma2.jpg |thumb|150px|Oncocytoma (WC/Nephron)]] |
| |} | | |} |
|
| |
|
| ===Common DDx=== | | ===Common DDx=== |
| Spindle cell tumours: | | ====Spindle cell tumours==== |
| *Malignant:
| | Malignant spindle cell tumours of the kidney: |
| **[[Renal cell carcinoma with sarcomatoid differentiation]].
| | *[[Renal cell carcinoma with sarcomatoid differentiation]]. |
| **[[Renal mucinous tubular and spindle cell carcinoma]].
| | *[[Renal mucinous tubular and spindle cell carcinoma]]. |
| **[[Wilms tumour]].
| | *[[Wilms tumour]]. |
| *Benign:
| | *[[Renal cell carcinoma, unclassified]]. |
| **[[Angiomyolipoma]].
| |
| **[[Cystic nephroma]].
| |
|
| |
|
| =WHO classification= | | Benign spindle cell tumours of the kidney: |
| *Based on 2004 iteration - as per WMSP, slightly modified.<ref>{{Ref WMSP|291}}</ref> | | *[[Angiomyolipoma]]. |
| ==Renal cell tumours== | | *[[Cystic nephroma]]. |
| | |
| | ====Renal tumours with eosinophilic cytoplasm==== |
| | {{Main|Renal tumours with eosinophilic cytoplasm}} |
| | |
| | =WHO classification of renal neoplasia= |
| | *Based on 2004 iteration - as per WMSP, slightly modified.<ref>{{Ref WMSP|291}}</ref> Online, the classification can [http://www.urosource.com/fileadmin/user_upload/european_urology/PIIS0302283805008316.pdf found here]. |
| | ===Renal cell tumours=== |
| Common: | | Common: |
| *[[Clear cell renal cell carcinoma]]. | | *[[Clear cell renal cell carcinoma]]. |
| *[[Multilocular clear cell renal cell carcinoma]].
| |
| *[[Papillary renal cell carcinoma]]. | | *[[Papillary renal cell carcinoma]]. |
| *[[Renal papillary adenoma|Papillary adenoma]]. | | *[[Renal papillary adenoma|Papillary adenoma]]. |
| *[[Chromophobe renal cell carinoma]]. | | *[[Chromophobe renal cell carcinoma]]. |
| *[[Renal oncocytoma|Oncocytoma]]. | | *[[Renal oncocytoma|Oncocytoma]]. |
|
| |
|
| Less common: | | Less common: |
| | *[[Multilocular clear cell renal cell carcinoma]]. |
| *[[Carcinoma of the collecting ducts of Bellini]]. | | *[[Carcinoma of the collecting ducts of Bellini]]. |
| *[[Renal cell carcinoma, unclassified]]. | | *[[Renal cell carcinoma, unclassified]]. |
| Line 192: |
Line 182: |
| *Carcinoma associated with neuroblastoma. | | *Carcinoma associated with neuroblastoma. |
|
| |
|
| ==Metanephric tumours== | | ===Metanephric tumours=== |
| *[[Metanephric adenoma]]. | | *[[Metanephric adenoma]]. |
| *[[Metanephric stromal tumour]]. | | *[[Metanephric stromal tumour]]. |
| *[[Metanephric adenofibroma]]. | | *[[Metanephric adenofibroma]]. |
|
| |
|
| ==Nephroblastic tumours== | | ===Nephroblastic tumours=== |
| *Nephrogenic rests. | | *Nephrogenic rests. |
| *[[Nephroblastoma]]. | | *[[Nephroblastoma]]. |
|
| |
|
| ==Mesenchymal tumours== | | ===Mesenchymal tumours=== |
| Childhood: | | Childhood: |
| *[[Clear cell sarcoma of the kidney]]. | | *[[Clear cell sarcoma of the kidney]]. |
| *[[Rhabdoid tumour]]. | | *[[Rhabdoid tumour]]. |
| *[[Mesoblastic nephroma|Congenital mesoblastic nephroma]] | | *[[Mesoblastic nephroma|Congenital mesoblastic nephroma]]. |
|
| |
|
| Adults: | | Adults: |
| Line 222: |
Line 212: |
| *[[Schwannoma]]. | | *[[Schwannoma]]. |
|
| |
|
| ==Mixed mesenchymal and epithelial tumours== | | ===Mixed mesenchymal and epithelial tumours=== |
| *[[Cystic nephroma]]. | | *[[Cystic nephroma]]. |
| *[[Mixed epithelial and stromal tumour]]. | | *[[Mixed epithelial and stromal tumour]]. |
| *[[Synovial sarcoma]]. | | *[[Synovial sarcoma]]. |
|
| |
|
| ==Others== | | ===Others=== |
| *[[Neuroendocrine tumours]]. | | *[[Neuroendocrine tumours]]. |
| *Hematologic tumours. | | *Hematologic tumours. |
| *[[Germ cell tumour]]s. | | *[[Germ cell tumour]]s. |
| *[[Metastases]]. | | *[[Metastases]]. |
| | |
| | ==Vancouver modification of WHO classification== |
| | In 2012/2013, several additions were made:<ref name=pmid24025519>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | last3 = Eble | first3 = JN. | last4 = Egevad | first4 = L. | last5 = Epstein | first5 = JI. | last6 = Grignon | first6 = D. | last7 = Hes | first7 = O. | last8 = Moch | first8 = H. | last9 = Montironi | first9 = R. | title = The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia. | journal = Am J Surg Pathol | volume = 37 | issue = 10 | pages = 1469-89 | month = Oct | year = 2013 | doi = 10.1097/PAS.0b013e318299f2d1 | PMID = 24025519 }}</ref> |
| | *[[Tubulocystic renal cell carcinoma]]. |
| | *[[Acquired cystic disease associated renal cell carcinoma]]. |
| | *[[Clear cell papillary renal cell carcinoma]] (clear cell tubulopapillary renal cell carcinoma). |
| | *[[Hereditary leiomyomatosis renal cell carcinoma syndrome associated renal cell carcinoma]]. |
| | *MiT family translocation renal cell carcinoma - includes: |
| | **[[t(6;11) renal cell carcinoma]]. |
| | |
| | "Emerging" entities (as per Vancouver) are: |
| | *[[Thyroid-like follicular renal cell carcinoma]]. |
| | *[[Succinate dehydrogenase-deficient renal cell carcinoma]]. |
| | *[[ALK translocation renal cell carcinoma]]. |
| | |
| | ==An entity proposed after Vancouver== |
| | *[[Eosinophilic, solid and cystic renal cell carcinoma]]. |
| | *[[Biphasic hyalinizing psammomatous renal cell carcinoma]]. |
| | *[[Papillary renal neoplasm with reverse polarity]]. |
| | *[[Low-grade oncocytic renal tumour]]. |
|
| |
|
| =Renal cell carcinoma= | | =Renal cell carcinoma= |
| Line 257: |
Line 267: |
| *Male>female (~2:1). | | *Male>female (~2:1). |
| *Hereditary - familial syndromes (see [[Hereditary RCC]]). | | *Hereditary - familial syndromes (see [[Hereditary RCC]]). |
| | *[[Obesity]].<ref name=pmid8770461>{{Cite journal | last1 = Chow | first1 = WH. | last2 = McLaughlin | first2 = JK. | last3 = Mandel | first3 = JS. | last4 = Wacholder | first4 = S. | last5 = Niwa | first5 = S. | last6 = Fraumeni | first6 = JF. | title = Obesity and risk of renal cell cancer. | journal = Cancer Epidemiol Biomarkers Prev | volume = 5 | issue = 1 | pages = 17-21 | month = Jan | year = 1996 | doi = | PMID = 8770461 }}</ref> |
|
| |
|
| ===Subtypes of RCC=== | | ===Subtypes of RCC=== |
| RCC (renal cell carcinoma) comes in different subtypes:<ref name=Ref_PBoD1016>{{Ref PBoD|1016}}</ref> | | RCC (renal cell carcinoma) comes in different subtypes:<ref name=Ref_PBoD1016>{{Ref PBoD|1016}}</ref> |
| *Clear cell carcinoma (70-80% of RCC) -- abbrev. CCRCC, | | *Clear cell carcinoma (70-80% of RCC) -- abbrev. CCRCC. |
| *Papillary renal cell carcinoma (10-15% of RCC) -- abbrev. PRCC, | | *Papillary renal cell carcinoma (10-15% of RCC) -- abbrev. PRCC. |
| *Chromophobe renal carcinoma (5% of RCC) -- abbrev. ChRCC, | | *Chromophobe renal carcinoma (5% of RCC) -- abbrev. ChRCC. |
| *Collecting duct (Bellini duct) carcinoma (1% of RCC). | | *Collecting duct (Bellini duct) carcinoma (1% of RCC). |
|
| |
|
| Line 278: |
Line 289: |
| *Papillary RCC type 1 vs. papillary RCC type 2: | | *Papillary RCC type 1 vs. papillary RCC type 2: |
| ** E-cadherin +ve in PRCC type 2.<ref name=pmid14657952>{{cite journal |author=Langner C, Ratschek M, Rehak P, Schips L, Zigeuner R |title=Expression of MUC1 (EMA) and E-cadherin in renal cell carcinoma: a systematic immunohistochemical analysis of 188 cases |journal=Mod. Pathol. |volume=17 |issue=2 |pages=180? |year=2004 |month=February |pmid=14657952 |doi=10.1038/modpathol.3800032 |url=}}</ref> | | ** E-cadherin +ve in PRCC type 2.<ref name=pmid14657952>{{cite journal |author=Langner C, Ratschek M, Rehak P, Schips L, Zigeuner R |title=Expression of MUC1 (EMA) and E-cadherin in renal cell carcinoma: a systematic immunohistochemical analysis of 188 cases |journal=Mod. Pathol. |volume=17 |issue=2 |pages=180? |year=2004 |month=February |pmid=14657952 |doi=10.1038/modpathol.3800032 |url=}}</ref> |
| **EMA (MUC1) +ve in PRCC type 1.<ref name=pmid14657952/> | | **[[EMA]] (MUC1) +ve in PRCC type 1.<ref name=pmid14657952/> |
|
| |
|
| *ChRCC vs. oncocytoma (ONC): | | *ChRCC vs. oncocytoma (ONC): |
| Line 305: |
Line 316: |
| *Pathologically, this is not very difficult. | | *Pathologically, this is not very difficult. |
| *On gross specimens, it is almost always obvious what one is dealing with: | | *On gross specimens, it is almost always obvious what one is dealing with: |
| **[[UCC]] = ''nephroureterectomy''. | | **[[UCC]] = ''[[nephroureterectomy]]''. |
| **[[RCC]] = ''partial nephrectomy'', ''nephrectomy'' or ''radical nephrectomy''. | | **[[RCC]] = ''[[partial nephrectomy]]'', ''nephrectomy'' or ''[[radical nephrectomy]]''. |
|
| |
|
| ===Renal cell carcinoma with sarcomatoid differentiation=== | | ===Renal cell carcinoma with sarcomatoid differentiation=== |
| *[[AKA]] ''sarcomatoid renal cell carcinoma''. | | *[[AKA]] ''sarcomatoid renal cell carcinoma''. |
| ====General====
| | {{Main|Renal cell carcinoma with sarcomatoid differentiation}} |
| Features:<ref name=pmid11224597>{{Cite journal | last1 = de Peralta-Venturina | first1 = M. | last2 = Moch | first2 = H. | last3 = Amin | first3 = M. | last4 = Tamboli | first4 = P. | last5 = Hailemariam | first5 = S. | last6 = Mihatsch | first6 = M. | last7 = Javidan | first7 = J. | last8 = Stricker | first8 = H. | last9 = Ro | first9 = JY. | title = Sarcomatoid differentiation in renal cell carcinoma: a study of 101 cases. | journal = Am J Surg Pathol | volume = 25 | issue = 3 | pages = 275-84 | month = Mar | year = 2001 | doi = | PMID = 11224597 }}</ref>
| |
| *Not recognized as a distinct entity in 2004 WHO classification.<ref name=pmid16442207>{{Cite journal | last1 = Lopez-Beltran | first1 = A. | last2 = Scarpelli | first2 = M. | last3 = Montironi | first3 = R. | last4 = Kirkali | first4 = Z. | title = 2004 WHO classification of the renal tumors of the adults. | journal = Eur Urol | volume = 49 | issue = 5 | pages = 798-805 | month = May | year = 2006 | doi = 10.1016/j.eururo.2005.11.035 | PMID = 16442207 }}</ref>
| |
| **It is considered an indicator of progression.
| |
| **Previously considered a distinct entity.<ref name=pmid16442207/><ref name=pmid10080595>{{Cite journal | last1 = Cangiano | first1 = T. | last2 = Liao | first2 = J. | last3 = Naitoh | first3 = J. | last4 = Dorey | first4 = F. | last5 = Figlin | first5 = R. | last6 = Belldegrun | first6 = A. | title = Sarcomatoid renal cell carcinoma: biologic behavior, prognosis, and response to combined surgical resection and immunotherapy. | journal = J Clin Oncol | volume = 17 | issue = 2 | pages = 523-8 | month = Feb | year = 1999 | doi = | PMID = 10080595 | URL = http://jco.ascopubs.org/content/17/2/523.full }}</ref>
| |
| *Tend to present at higher stage.
| |
| *Worse prognosis when adjusted for stage.
| |
|
| |
|
| ====Microscopic==== | | ===Renal cell carcinoma with rhabdoid morphology=== |
| Features:<ref name=pmid11224597/>
| | *[[AKA]] ''renal cell carcinoma with rhabdoid change''. |
| #Renal cell carcinoma.
| | {{Main|Renal cell carcinoma with rhabdoid morphology}} |
| #Sarcomatoid component:
| |
| #*[[Fibrosarcoma]] - most common.
| |
| #*[[Pleomorphic undifferentiated sarcoma|Undifferentiated]] - common.
| |
| #*[[Rhabdomyosarcoma]] - very rare.
| |
|
| |
|
| ==Hereditary renal cell carcinoma== | | ==Hereditary renal cell carcinoma== |
| The classics - which are ''all'' autosomal dominant:<ref name=Ref_PBoD1016>{{Ref PBoD|1016}}</ref>
| | {{Main|Hereditary renal cell carcinoma}} |
| # [[Von Hippel-Lindau syndrome]].
| |
| #* VHL gene mutation.
| |
| #* Clear cell RCC.
| |
| # Hereditary [[clear cell renal cell carcinoma]].
| |
| #* VHL gene mutation.
| |
| # Hereditary [[papillary renal cell carcinoma]].
| |
| #* MET proto-oncogene mutation.
| |
| #* PaRCC type 1.<ref name=Ref_WMSP290>{{Ref WMSP|290}}</ref>
| |
| # Hereditary leiomyomatosis and renal cell cancer:<ref name=Ref_WMSP290>{{Ref WMSP|290}}</ref>
| |
| #* FH (fumarate hydratase) gene mutation.<ref name=omim136850>{{OMIM|136850}}</ref>
| |
| #* PaRCC type 2.
| |
| #* Benign [[leiomyoma]]s skin/[[uterine leiomyoma|uterus]].
| |
| #* Uterine [[leiomyosarcoma]].
| |
| # [[Birt–Hogg–Dubé syndrome]]:<ref name=Ref_WMSP290>{{Ref WMSP|290}}</ref>
| |
| #* FLCN (folliculin) gene mutation.<ref name=omim135150>{{OMIM|135150}}</ref>
| |
| #* Skin lesions (fibrofolliculoma, trichodiscoma, [[acrochordon]]).
| |
| #* ChRCC most common, other types seen (e.g. [[renal oncocytoma|oncocytoma]]).
| |
| #* Variable penetrance (autosomal dominant).
| |
| | |
| Others:
| |
| * Hereditary papillary carcinoma (TFE3 related translocations).<ref name=omim314310>{{OMIM|314310}}</ref>
| |
| | |
| Notes:<br>
| |
| *A total of ten hereditary renal cancer syndromes have been described. In eight of the ten the gene is known.<ref name=pmid20817385>{{Cite journal | last1 = Verine | first1 = J. | last2 = Pluvinage | first2 = A. | last3 = Bousquet | first3 = G. | last4 = Lehmann-Che | first4 = J. | last5 = de Bazelaire | first5 = C. | last6 = Soufir | first6 = N. | last7 = Mongiat-Artus | first7 = P. | title = Hereditary renal cancer syndromes: an update of a systematic review. | journal = Eur Urol | volume = 58 | issue = 5 | pages = 701-10 | month = Nov | year = 2010 | doi = 10.1016/j.eururo.2010.08.031 | PMID = 20817385 }}</ref>
| |
| | |
| ===Molecular===
| |
| Recurrent molecular changes in RCC:
| |
| *Clear cell RCC:
| |
| **Loss of 3p - contains the VHL gene.
| |
| *Papillary RCC:
| |
| **Sporadic:
| |
| ***Trisomy 7, 16, 17.
| |
| ***Loss of Y.
| |
| **Familial:
| |
| ***Trisomy 7 - contains MET gene.<ref>{{OMIM|164860}}</ref>
| |
| | |
| ==Grading RCC==
| |
| ===General===
| |
| Some subtypes are graded based on the '''Fuhrman system''' which considers:<ref name=Ref_GUP282>{{Ref GUP|282}}</ref>
| |
| *Nuclear pleomorphism (size, shape).
| |
| *Chromatin pattern.
| |
| *Nucleoli prominence.
| |
|
| |
|
| Notes:
| | ==Renal cell carcinoma grading== |
| *The system was validated for clear cell RCC.
| | {{Main|Renal cell carcinoma grading}} |
| *Fuhrman nuclear grade is '''not''' prognostic in ''chromophobe RCC'' and should not be used in that context.<ref name=pmid17527087>{{Cite journal | last1 = Delahunt | first1 = B. | last2 = Sika-Paotonu | first2 = D. | last3 = Bethwaite | first3 = PB. | last4 = McCredie | first4 = MR. | last5 = Martignoni | first5 = G. | last6 = Eble | first6 = JN. | last7 = Jordan | first7 = TW. | title = Fuhrman grading is not appropriate for chromophobe renal cell carcinoma. | journal = Am J Surg Pathol | volume = 31 | issue = 6 | pages = 957-60 | month = Jun | year = 2007 | doi = 10.1097/01.pas.0000249446.28713.53 | PMID = 17527087 }}</ref>
| |
|
| |
|
| ===Criteria & grades=== | | ==Renal cell carcinoma staging== |
| *Grade 1: no nucleoli, near 'normal' appearance.
| | {{Main|Kidney cancer staging}} |
| *Grade 2: finely granular chromatin (key feature), no nuclei visible with 10x objective lens.
| |
| *Grade 3: [[nucleoli]] seen easily (key feature).
| |
| *Grade 4: prominent pleomorphism (key feature), hyperchromasia, [[macronucleoli]].
| |
| Note: Most tumours are grade 2 & 3.
| |
|
| |
|
| ===Fuhrman grading in short=== | | ===Renal sinus invasion=== |
| *1 vs. 2: grade 2 has granular chromatin, grade 2 has nucleoli visible @ 20x objective.<ref>AE. June 2010.</ref>
| | {{Main|Kidney cancer staging}} |
| *2 vs. 3: grade 3 has nucleoli @ 10x objective.
| |
| *3 vs. 4: grade 4 has pleomorphism/hyperchromasia.
| |
|
| |
|
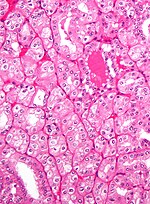
| ==Clear cell renal cell carcinoma== | | ==Clear cell renal cell carcinoma== |
| *Abbreviated ''CRCC'' or ''CCRCC''.
| | {{Main|Clear cell renal cell carcinoma}} |
| | |
| ===General===
| |
| *Most common subtype of RCC.
| |
| *May be associated with [[Von Hippel-Lindau syndrome]].
| |
| | |
| ===Gross===
| |
| *Gold/yellow.
| |
| *+/-Haemorrhage (common).
| |
| *+/-Necrosis (common in large tumours).
| |
| *+/-Calcification.
| |
| *+/-Cysts.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_PBoD1017-8>{{Ref PBoD|1017-8}}</ref>
| |
| *Solid or [[trabecular]] pattern.
| |
| *Polygonal cells.
| |
| *Clear cytoplasm.
| |
| *Central nucleus.
| |
| *Delicate branching vasculature.
| |
| **Often called "chicken wire-like" vasculature.
| |
| *+/-Rhabdoid cells:
| |
| **Eccentric nucleus.
| |
| **Abundant eosinophilic cytoplasma.
| |
| | |
| Notes:
| |
| *Cytoplasm may be eosinophilic.<ref name=Ref_WMSP291>{{Ref WMSP|291}}</ref>
| |
| **This change is typically focal - other areas have a classic appearance.
| |
| **Chicken wire-like vasculature present - helps distinguish from other tumours.
| |
| *[[Hyaline bodies]] common.<ref>AFIP Renal Tumours Book.</ref>
| |
| **Not common in papillary RCC.
| |
| *Clear cytoplasm - due to lipid content.
| |
| | |
| DDx:
| |
| *[[Chromophobe renal cell carcinoma]].
| |
| *[[Clear cell papillary renal cell carcinoma]].
| |
| *[[Xp11.2 translocation carcinoma]].
| |
| *[[Adrenocortical carcinoma]] (ACC)
| |
| **EMA -ve, CKs mostly -ve, inhibin +ve (neg. in RCC).<ref name=Ref_GUP285>{{Ref GUP|285}}</ref>
| |
| *[[Alveolar soft part sarcoma]].
| |
| *[[Adrenal gland]], normal.
| |
| | |
| Images:
| |
| *[http://commons.wikimedia.org/wiki/File:Clear_cell_renal_cell_carcinoma_intermed_mag.jpg CRCC - intermed. mag. (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Clear_cell_renal_cell_carcinoma_high_mag.jpg CRCC - high mag. (WC)].
| |
| | |
| ===IHC===
| |
| *CK7 -ve.
| |
| *CK20 -ve.
| |
| *Hale's colloidal iron -ve.
| |
| **+ve in [[chromophobe RCC]].
| |
| | |
| Note: ''[[Hale's colloidal iron]]'' does not stain iron... it stains hemosiderin.<ref>Latta. 27 January 2009.</ref>
| |
| Clear cell vs. chromophobe:
| |
| *Chromophobe: "translucent" (NOT quite clear), reticulated, Hale's colloidal iron stain+, CK7+ (cell membrane).
| |
| | |
| ===Sign out===
| |
| <pre>
| |
| KIDNEY, LEFT, NEPHRECTOMY:
| |
| - CLEAR CELL RENAL CELL CARCINOMA, pT1a, MARGINS NEGATIVE FOR MALIGNANCY.
| |
| - PLEASE SEE TUMOUR SUMMARY.
| |
| </pre>
| |
| | |
| Note:
| |
| *The surgeon wants the diagnosis and margin status; thus, these are included in the diagnosis line with the tumour stage.
| |
| | |
| ====Micro====
| |
| The sections show a tumour with a chicken wire-like vasculature composed of clear cells with basally stratified nuclei. Hemosiderin-laden macrophages are present. Necrosis is present. Abundant hyaline globules are present.
| |
| | |
| There is no perinuclear clearing. The cytoplasm is not whispy. Collections of macrophages are not identified within the stroma of the tumour. Papillae are not evident.
| |
| | |
| Rare, small nucleoli are visible with the 10x objective. The tumour nuclei are approximately 15 micrometers.
| |
|
| |
|
| ==Multilocular cystic renal cell carcinoma== | | ==Multilocular cystic renal cell carcinoma== |
| ===General===
| | {{Main|Multilocular cystic renal cell carcinoma}} |
| *No recurrences or metastasis in the literature.<ref name=Ref_WMSP292>{{Ref WMSP|292}}</ref>
| |
| **This makes one wonder... is it really cancer.
| |
| *Case report rare.<ref name=pmid21366448>{{Cite journal | last1 = Agarwal | first1 = S. | last2 = Agrawal | first2 = U. | last3 = Mohanty | first3 = NK. | last4 = Saxena | first4 = S. | title = Multilocular cystic renal cell carcinoma: a case report of a rare entity. | journal = Arch Pathol Lab Med | volume = 135 | issue = 3 | pages = 290-2 | month = Mar | year = 2011 | doi = 10.1043/2010-0243-LE.1 | PMID = 21366448 }}</ref>
| |
| | |
| ===Gross===
| |
| Features:<ref name=Ref_WMSP292>{{Ref WMSP|292}}</ref>
| |
| *Cystic with thin septa.
| |
| *Well circumscribed.
| |
| | |
| Note:
| |
| *This tumour, radiologically, can often be separated from other cystic tumours.<ref name=pmid21722289>{{Cite journal | last1 = You | first1 = D. | last2 = Shim | first2 = M. | last3 = Jeong | first3 = IG. | last4 = Song | first4 = C. | last5 = Kim | first5 = JK. | last6 = Ro | first6 = JY. | last7 = Hong | first7 = JH. | last8 = Ahn | first8 = H. | last9 = Kim | first9 = CS. | title = Multilocular cystic renal cell carcinoma: clinicopathological features and preoperative prediction using multiphase computed tomography. | journal = BJU Int | volume = | issue = | pages = | month = Jul | year = 2011 | doi = 10.1111/j.1464-410X.2011.10247.x | PMID = 21722289 }}</ref>
| |
| ===Microscopic===
| |
| Features:<ref name=Ref_WMSP292>{{Ref WMSP|292}}</ref>
| |
| *Polygonal cells within the septa.
| |
| *Clear cytoplasm.
| |
| *+/-Calcification (common).
| |
| | |
| DDx:
| |
| *Cystic renal disease with macrophages in the septa.
| |
| *Cystic clear cell renal cell carcinoma.
| |
| ===IHC===
| |
| *EMA +ve.
| |
| *Keratins +ve.
| |
| *CD68 -ve.
| |
|
| |
|
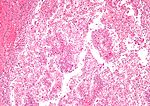
| ==Papillary renal cell carcinoma== | | ==Papillary renal cell carcinoma== |
| *Abbreviated ''PRCC'', ''PaRCC'' and ''papillary RCC''.
| | {{Main|Papillary renal cell carcinoma}} |
| ===General===
| |
| *Often subclassified<ref name=Ref_GUP289>{{Ref GUP|289}}</ref> into ''type 1'' and ''type 2'' -- see ''microscopic''.
| |
| **Type 1 and Type 2 are different on a cytogenetic and molecular basis.<ref>{{Cite journal | last1 = Klatte | first1 = T. | last2 = Pantuck | first2 = AJ. | last3 = Said | first3 = JW. | last4 = Seligson | first4 = DB. | last5 = Rao | first5 = NP. | last6 = LaRochelle | first6 = JC. | last7 = Shuch | first7 = B. | last8 = Zisman | first8 = A. | last9 = Kabbinavar | first9 = FF. | title = Cytogenetic and molecular tumor profiling for type 1 and type 2 papillary renal cell carcinoma. | journal = Clin Cancer Res | volume = 15 | issue = 4 | pages = 1162-9 | month = Feb | year = 2009 | doi = 10.1158/1078-0432.CCR-08-1229 | PMID = 19228721 }}</ref>
| |
| | |
| ====Epidemiology====
| |
| *Associated with ''[[acquired renal cystic disease]]''.<ref>{{Ref DARP|438}}</ref>
| |
| *May be familial.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_PBoD1017-8>{{Ref PBoD|1017-8}}</ref>
| |
| *Cuboidal or low columnar cell in papillae.
| |
| *Interstitial foam cells in vascular cores - '''key feature'''.<ref>ALS Feb 9, 2009.</ref>
| |
| **Most sensitive and specific feature of PRCC.<ref>{{cite journal |author=Granter SR, Perez-Atayde AR, Renshaw AA |title=Cytologic analysis of papillary renal cell carcinoma |journal=Cancer |volume=84 |issue=5 |pages=303?8 |year=1998 |month=October |pmid=9801205 |doi= |url=http://dx.doi.org/10.1002/(SICI)1097-0142(19981025)84:5<303::AID-CNCR6>3.0.CO;2-7}}</ref>
| |
| *Highly vascular.
| |
| | |
| Size criterion:
| |
| *Papillary lesions '''''must''''' be >0.5 cm to be called ''carcinoma''; smaller lesions (<=0.5 cm) are called ''[[renal papillary adenoma|papillary adenoma]]s''.<ref name=Ref_GUP288>{{Ref GUP|288}}</ref>
| |
| | |
| Mnemonic ''HIP'': '''h'''ighly vascular, '''i'''nterstitial foam cells, '''p'''apillae.
| |
| | |
| DDx:
| |
| *Clear cell RCC.
| |
| **Papillary: +histiocytes, +intracellular hemosiderin, [[CK7]]+.
| |
| *[[Clear cell papillary renal cell carcinoma]].
| |
| *[[Metanephric adenoma]] - esp. solid PRCC type 1.
| |
| *[[Collecting duct carcinoma]] - esp. PRCC type 2.
| |
| *[[Renal papillary adenoma]].
| |
| | |
| ====Histological subtyping====
| |
| Subtypes:<ref name=Ref_GUP289>{{Ref GUP|289}}</ref>
| |
| *''Type 1'' - single layer of cells on basement membrane.
| |
| ** usually low grade nuclear features, i.e. low Fuhrman grade.
| |
| *''Type 2'' - pseudostratification of cells.
| |
| ** Usually high grade nuclear features, i.e. high Fuhrman grade.
| |
| | |
| Others:
| |
| *''Oncocytic'' - oncocytic cytoplasm.
| |
| **Extremely rare ~ largest series is 12 cases.<ref name=pmid19494850 >{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 }}</ref>
| |
| | |
| ===IHC===
| |
| Features:<ref name=Ref_GUP289>{{Ref GUP|289}}</ref>
| |
| *AMACR +ve.<ref>ALS Feb 9, 2009.</ref>
| |
| *HMWCK (34betaE12) +ve.
| |
| *Panker (AE1/AE3) +ve.
| |
| *CK7 +ve ~90% of type 1, 20% of type 2.
| |
| | |
| More reading:
| |
| *[http://www.e-immunohistochemistry.info/web/Papillary_renal_cell_carcinoma.htm e-immunohistochemistry.info]
| |
| | |
| ===Molecular===
| |
| Features:<ref name=Ref_PBoD1016>{{Ref PBoD|1016}}</ref>
| |
| *Sporadic: trisomies 7, 16, 17.
| |
| *Familial: trisomy 7.
| |
| **Chromosome 7 = location of MET gene.
| |
| | |
| Note:
| |
| *Not used for diagnosis.<ref>{{Ref WMSP|292}}</ref>
| |
| | |
| ===Sign out===
| |
| <pre>
| |
| KIDNEY, RIGHT, NEPHRECTOMY:
| |
| - PAPILLARY RENAL CELL CARCINOMA, ONCOCYTIC -- SEE COMMENT;
| |
| - FUHRMANN GRADE 2;
| |
| - SURGICAL MARGINS NEGATIVE;
| |
| - PLEASE SEE TUMOUR SUMMARY.
| |
| | |
| COMMENT:
| |
| The oncocytic variant of papillary renal cell carcinoma (RCC) is uncommon and not widely
| |
| recognized as a subtype of papillary RCC. The prognostic significance of the oncocytic
| |
| cytoplasm is uncertain.[1] The histomorphology in this case is compatible with a type 1
| |
| papillary RCC.
| |
| | |
| 1. Ann Diagn Pathol. 2006 Jun;10(3):133-9.
| |
| </pre>
| |
|
| |
|
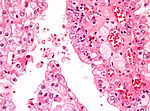
| ==Chromophobe renal cell carcinoma== | | ==Chromophobe renal cell carcinoma== |
| *Abbreviated ''ChRCC''.
| | {{Main|Chromophobe renal cell carcinoma}} |
| ===General===
| |
| *Least common of the common types of RCC.
| |
| *''Fuhrman grading'' for this entity is controversial, as it does not appear to have any predictive value.<ref name=pmid17527087>{{Cite journal | last1 = Delahunt | first1 = B. | last2 = Sika-Paotonu | first2 = D. | last3 = Bethwaite | first3 = PB. | last4 = McCredie | first4 = MR. | last5 = Martignoni | first5 = G. | last6 = Eble | first6 = JN. | last7 = Jordan | first7 = TW. | title = Fuhrman grading is not appropriate for chromophobe renal cell carcinoma. | journal = Am J Surg Pathol | volume = 31 | issue = 6 | pages = 957-60 | month = Jun | year = 2007 | doi = 10.1097/01.pas.0000249446.28713.53 | PMID = 17527087 }}</ref>
| |
| | |
| There are two subtypes:<ref name=Ref_GUP293>{{Ref GUP|293}}</ref>
| |
| *Classic.
| |
| *Eosinophilic variant.
| |
| | |
| ===Gross===
| |
| *Tan, light-brown.
| |
| *Solitary.
| |
| *Well-circumscribed.
| |
| | |
| Image:
| |
| *[http://www.flickr.com/photos/35441329@N05/4273199789/in/photostream/ Chromophobe RCC (flickr.com)].
| |
| | |
| ===Microscopic===
| |
| ====Classic====
| |
| Features - classic type (3 P's [[mnemonic]]):<ref>{{Ref PBoD|1016-7}}</ref><ref name=Ref_GUP293>{{Ref GUP|293}}</ref>
| |
| *Pale cytoplasm, with wisps of eosinophilic material; the cells are not completely clear, they have "cobwebs".
| |
| *Perinuclear clearing, i.e. a pale halo surrounds the nucleus - '''key feature'''.
| |
| *Periphery of cell distinct, i.e. cell membrane is easy to discern.
| |
| | |
| Notes:
| |
| *May have [[psammoma bodies]].
| |
| *May be described as "plant-like"; plant cells have (thick) cell walls.
| |
| *The perinuclear clearing is often somewhat patchy, i.e. it is usually not present in very tumour cell.
| |
| | |
| DDx:
| |
| *Clear cell RCC (classic).
| |
| **Perinuclear clearing is ''not'' seen in clear cell RCC.
| |
| **ChRCC has wisps in the cytoplasm.
| |
| | |
| ====Eosinophilic variant====
| |
| Features - eosinophilic variant:<ref name=Ref_GUP293>{{Ref GUP|293}}</ref>
| |
| *'''Eosinophilic''' (finely granular) cytoplasm.
| |
| *Perinuclear clearing - '''key feature'''.
| |
| *Periphery of cell distinct.
| |
| *'''Smaller cells''' than classic subtype.
| |
| | |
| Notes:
| |
| #May have [[psammoma bodies]].
| |
| | |
| DDx:
| |
| #[[Renal oncocytoma|Oncocytoma]] - particularly the eosinophilic variant.
| |
| #*IHC may be useful to differentiate (CK7: oncocytoma = cytoplasm +ve, chromophobe = cell membrane +ve).
| |
| #*A comparison based on histomorphology: ''[[Kidney_tumours#Tabular_comparison_of_oncocytoma_and_chromophobe_RCC|Tabular comparison between ChRCC & oncocytoma]]''.
| |
| #**Oncocytoma typically has: no perinuclear clearing, no raisinoid nuclei, no binucleation.
| |
| #Clear cell RCC, eosinophilic variant.
| |
| #*Perinuclear clearing is ''not'' seen in clear cell RCC.
| |
| #*ChRCC has wisps in the cytoplasm.
| |
| | |
| Image:
| |
| *[http://commons.wikimedia.org/wiki/File:Oncocytic_chromophobe_rcc_high_mag.jpg Oncocytic chromophobe RCC (WC)].
| |
| *[http://path.upmc.edu/cases/case333.html Chromophobe RCC - several images (upmc.edu)].
| |
| | |
| ===Stains===
| |
| *[[Hale's colloidal iron]] +ve (blue granular cytoplasmic).
| |
| | |
| Images:
| |
| *[http://www.nature.com/modpathol/journal/v18/n2/fig_tab/3800286f1.html ChRCC Hale's colloidal iron - several images (nature.com)].
| |
| *[http://www.ultrapath.org/oldsite/cases99/sep99/images/figure-3.jpg ChRCC Hale's colloidal iron (ultrapath.org)].<ref>URL: [http://www.ultrapath.org/oldsite/cases99/sep99/cotm9-2.html http://www.ultrapath.org/oldsite/cases99/sep99/cotm9-2.html]. Accessed on: 9 October 2011.</ref>
| |
| *[http://www.diagnosticpathology.org/content/4/1/21/figure/f1?highres=n ChRCC Hale's colloidal iron (diagnosticpathology.org)].
| |
| | |
| ===IHC===
| |
| *CK7 +ve cell membrane.<ref name=Ref_GUP293>{{Ref GUP|293}}</ref>
| |
| *CD117 +ve.
| |
| *Vimentin -ve.
| |
| | |
| ===Molecular===
| |
| *Extensive aneusomy (monosomy?):<ref name=Ref_WMSP292>{{Ref WMSP|292}}</ref>
| |
| **Loss of chromosomes: 1, 2, 6, 10, 13, 17, 21.
| |
| | |
| ===Sign out===
| |
| <pre>
| |
| KIDNEY, RIGHT UPPER POLE, PARTIAL NEPHRECTOMY:
| |
| - CHROMOPHOBE RENAL CELL CARCINOMA.
| |
| | |
| COMMENT:
| |
| The sections show a mix of clear cells with wispy cytoplasm, and cells with eosinophilic
| |
| cytoplasm and perinuclear halos. There are no true papillae.
| |
| | |
| Stains and immunostains:
| |
| Positive: CK7, CAM5.2, EMA, pankeratin, CD117, colloidal iron.
| |
| Negative: AMACR, CD10, CD68, RCC, vimentin.
| |
| </pre>
| |
| | |
| ==Clear cell papillary renal cell carcinoma==
| |
| *[[AKA]] ''clear cell tubulopapillary renal cell carcinoma''.<ref name=pmid21602815>{{Cite journal | last1 = Rohan | first1 = SM. | last2 = Xiao | first2 = Y. | last3 = Liang | first3 = Y. | last4 = Dudas | first4 = ME. | last5 = Al-Ahmadie | first5 = HA. | last6 = Fine | first6 = SW. | last7 = Gopalan | first7 = A. | last8 = Reuter | first8 = VE. | last9 = Rosenblum | first9 = MK. | title = Clear-cell papillary renal cell carcinoma: molecular and immunohistochemical analysis with emphasis on the von Hippel-Lindau gene and hypoxia-inducible factor pathway-related proteins. | journal = Mod Pathol | volume = 24 | issue = 9 | pages = 1207-20 | month = Sep | year = 2011 | doi = 10.1038/modpathol.2011.80 | PMID = 21602815 }}</ref>
| |
| *Abbreviation ''CCPRCC''.
| |
| | |
| ===General===
| |
| *New entity not in the WHO classification.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=pmid21602815/>
| |
| *Features of both:
| |
| *#Clear cell RCC.
| |
| *#Papillary RCC.
| |
| *#*Often do not have true papillae.
| |
| *Apical nuclei - '''key feature'''.<ref>{{Cite journal | last1 = Bing | first1 = Z. | last2 = Tomaszewski | first2 = JE. | title = Case Report: Clear Cell Papillary Renal Cell Carcinoma in the Bilateral Native Kidneys after 2 Years of Renal Transplantation: Report of a Case and Review of the Literature. | journal = Case Reports in Transplantation | volume = 2011 | issue = | pages = | month = | year = 2011 | doi = 10.1155/2011/387645 | PMID = | url = http://www.hindawi.com/crim/transplantation/2011/387645/cta/ }}</ref>
| |
| **In most glandular structures the nuclei are usu. basally located, i.e. in the cytoplasm adjacent to the basement membrane.
| |
| | |
| DDx:
| |
| *[[Papillary renal cell carcinoma]].
| |
| *[[Clear cell renal cell carcinoma]]
| |
| *[[Xp11.2 translocation carcinoma]].
| |
| | |
| Images:
| |
| *www:
| |
| **[http://path.upmc.edu/cases/case682.html Clear cell papillary RCC - several images (upmc.edu)].
| |
| **[http://www.flickr.com/photos/40764007@N08/7177459461/ CCPRCC (flickr.com)].
| |
| *[[WC]]:
| |
| **[http://commons.wikimedia.org/wiki/File:Clear_cell_papillary_renal_cell_carcinoma_-_high_mag.jpg CCPRCC - high mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Clear_cell_papillary_renal_cell_carcinoma_-_very_high_mag.jpg CCPRCC - very high mag. (WC)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid21602815/>
| |
| *CK7 +ve.
| |
| **Usu. -ve in clear cell RCC.
| |
| *CD10 -ve.
| |
| **Usu. +ve in clear cell RCC.
| |
| *TFE3 -ve.
| |
| **By definition +ve in [[Xp11.2 translocation carcinoma]].
| |
| *AMACR -ve.
| |
| **Usu. +ve in [[Papillary RCC]].
| |
|
| |
|
| Others:<ref name=pmid21602815/>
| | ==Clear cell papillary renal cell tumour== |
| *HIF-1alpha +ve.
| | In the past, it was known as ''clear cell papillary renal cell carcinoma''. |
| *GLUT-1 +ve.
| | {{Main|Clear cell papillary renal cell tumour}} |
| | |
| How to remember: ''The two key stains are opposite of what the name implies''.
| |
| *''Clear cell'' RCC: CK7 negative. In this tumour it is the opposite - CK7 is positive.
| |
| *''Papillary'' RCC: AMACR positive. In this tumour it is the opposite - AMACR is negative.
| |
|
| |
|
| ==Unclassified renal cell carcinoma== | | ==Unclassified renal cell carcinoma== |
| *Abbreviated ''URCC''. | | *Abbreviated ''URCC''. |
| ===General===
| | {{Main|Unclassified renal cell carcinoma}} |
| *Uncommon.
| |
| *A WHO classification ''diagnosis of exclusion''.
| |
| *Worse prognosis than [[clear cell renal cell carcinoma]].<ref name=pmid17822461>{{Cite journal | last1 = Karakiewicz | first1 = PI. | last2 = Hutterer | first2 = GC. | last3 = Trinh | first3 = QD. | last4 = Pantuck | first4 = AJ. | last5 = Klatte | first5 = T. | last6 = Lam | first6 = JS. | last7 = Guille | first7 = F. | last8 = de La Taille | first8 = A. | last9 = Novara | first9 = G. | title = Unclassified renal cell carcinoma: an analysis of 85 cases. | journal = BJU Int | volume = 100 | issue = 4 | pages = 802-8 | month = Oct | year = 2007 | doi = 10.1111/j.1464-410X.2007.07148.x | PMID = 17822461 }}</ref>
| |
| *High variation in the prevalence (when comparing institutions); this suggests a lack of uniformity in the diagnosis of this subtype.<ref name=pmid17822461/>
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Malignant tumour that is one of the following:<ref name=Ref_WMSP293>{{Ref WMSP|293}}</ref><ref name=pmid22404824>{{Cite journal | last1 = Lopez-Beltran | first1 = A. | last2 = Kirkali | first2 = Z. | last3 = Montironi | first3 = R. | last4 = Blanca | first4 = A. | last5 = Algaba | first5 = F. | last6 = Scarpelli | first6 = M. | last7 = Yorukoglu | first7 = K. | last8 = Hartmann | first8 = A. | last9 = Cheng | first9 = L. | title = Unclassified renal cell carcinoma: a report of 56 cases. | journal = BJU Int | volume = 110 | issue = 6 | pages = 786-93 | month = Sep | year = 2012 | doi = 10.1111/j.1464-410X.2012.10934.x | PMID = 22404824 }}</ref>
| |
| *#A combination of other RCC histologic types (~35% of cases of URCC).
| |
| *#Has a "non-identifiable" pattern/unrecognizable cell type (~60% of cases of URCC).
| |
| *#Pure [[sarcomatoid RCC]] without an identifiable (epithelioid) RCC subtype (~5% of cases of URCC).<ref name=pmid22404824/>
| |
| | |
| DDx:
| |
| *[[Clear cell renal cell carcinoma]].
| |
| *[[Collecting duct carcinoma]].
| |
| *Undifferentiated carcinoma.
| |
| *[[Metastatic]] carcinoma.
| |
|
| |
|
| =Renal translocation carcinomas= | | =Renal translocation carcinomas= |
| ==Renal tumour with Xp11.2 translocation== | | ==Renal tumour with Xp11.2 translocation== |
| ===General===
| | {{Main|Renal tumour with Xp11.2 translocation}} |
| *Defined by the presence of a fusion gene formed with TFE3 @ Xp11.2.
| |
| *TFE3 is the gene involved in the translocation seen in [[alveolar soft part sarcoma]] (ASPS).
| |
| *Poor prognosis ~ 50% present at stage IV, majority of lymph node metastases.
| |
| *~1/3 of childhood RCC.<ref name=pmid17667536>{{Cite journal | last1 = Argani | first1 = P. | last2 = Olgac | first2 = S. | last3 = Tickoo | first3 = SK. | last4 = Goldfischer | first4 = M. | last5 = Moch | first5 = H. | last6 = Chan | first6 = DY. | last7 = Eble | first7 = JN. | last8 = Bonsib | first8 = SM. | last9 = Jimeno | first9 = M. | title = Xp11 translocation renal cell carcinoma in adults: expanded clinical, pathologic, and genetic spectrum. | journal = Am J Surg Pathol | volume = 31 | issue = 8 | pages = 1149-60 | month = Aug | year = 2007 | doi = 10.1097/PAS.0b013e318031ffff | PMID = 17667536 }}</ref>
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_WMSP285>{{Ref WMSP|285}}</ref>
| |
| *Large cells.
| |
| *Clear or eosinophilic cytoplasm.
| |
| *Papillae or nests.
| |
| *[[Psammoma bodies]] - common.<ref name=pmid17102051>{{Cite journal | last1 = Prasad | first1 = SR. | last2 = Humphrey | first2 = PA. | last3 = Catena | first3 = JR. | last4 = Narra | first4 = VR. | last5 = Srigley | first5 = JR. | last6 = Cortez | first6 = AD. | last7 = Dalrymple | first7 = NC. | last8 = Chintapalli | first8 = KN. | title = Common and uncommon histologic subtypes of renal cell carcinoma: imaging spectrum with pathologic correlation. | journal = Radiographics | volume = 26 | issue = 6 | pages = 1795-806; discussion 1806-10 | month = | year = | doi = 10.1148/rg.266065010 | PMID = 17102051 }}</ref>
| |
| **Calcification is considered the '''classic histomorphologic feature'''.
| |
| *[[Hyaline bodies]] - common.
| |
| | |
| Notes:
| |
| *Looks clear cell RCC ''or'' papillary RCC ''or'' a hybrid between the two.
| |
| *May resemble [[alveolar soft part sarcoma]].
| |
| | |
| DDx:
| |
| *Clear cell RCC.
| |
| *Papillary RCC.
| |
| *Epithelioid angiomyolipoma.
| |
| | |
| Images:
| |
| *[[WC]]:
| |
| **[http://commons.wikimedia.org/wiki/File:Xp11.2_translocation_renal_cell_carcinoma_-_intermed_mag.jpg Xp11.2 translocation RCC - intermed. mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Xp11.2_translocation_renal_cell_carcinoma_-_high_mag.jpg Xp11.2 translocation RCC - high mag. (WC)].
| |
| *www:
| |
| **[http://www.flickr.com/photos/40764007@N08/7403237732/in/photostream/ Translocation carcinoma (flickr.com)].
| |
| | |
| ===IHC===
| |
| *TFE3 +ve (nucleus) - '''key feature'''.<ref name=Ref_WMSP285>{{Ref WMSP|285}}</ref>
| |
| *CD10 +ve.
| |
| *Vimentin +ve.
| |
| | |
| Others:
| |
| *HMB-45 & Melan A -ve.
| |
| **Positive in ''epithelioid [[angiomyolipoma]]''.
| |
| | |
| ===Molecular===
| |
| *[[Translocation]] involving TFE3, e.g. t(X;1)(p11.2;q21).<ref name=Ref_WMSP285>{{Ref WMSP|285}}</ref>
| |
|
| |
|
| ==Renal tumour with t(6;11) translocation== | | ==Renal tumour with t(6;11) translocation== |
| ===General===
| | *[[AKA]] ''t(6;11) renal cell carcinoma''. |
| *Not common.
| | {{main|Renal tumour with t(6;11) translocation}} |
| *[[Lymph node metastases]] are common. | |
| *Essentially a pediatric tumour - case report of an adult.<ref name=pmid21884304>{{Cite journal | last1 = Ishihara | first1 = A. | last2 = Yamashita | first2 = Y. | last3 = Takamori | first3 = H. | last4 = Kuroda | first4 = N. | title = Renal carcinoma with (6;11)(p21;q12) translocation: Report of an adult case. | journal = Pathol Int | volume = 61 | issue = 9 | pages = 539-45 | month = Sep | year = 2011 | doi = 10.1111/j.1440-1827.2011.02711.x | PMID = 21884304 }}</ref>
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Hyaline material between nests.
| |
| *Large cells with clear to eosinophilic cytoplasm.
| |
| | |
| ===Molecular===
| |
| *t(6;11)(p21;q12) Alpha/TFEB.<ref name=Ref_WMSP281>{{Ref WMSP|281}}</ref>
| |
|
| |
|
| =Benign tumours= | | =Benign tumours= |
| ==Papillary adenoma of the kidney== | | ==Papillary adenoma of the kidney== |
| *[[AKA]] ''renal papillary adenoma''. | | *[[AKA]] ''renal papillary adenoma''. |
| ===General===
| | {{Main|Papillary adenoma of the kidney}} |
| *Benign.
| |
| *Considered a precursor for ''[[papillary renal cell carcinoma]]'' (PaRCC).<ref name=pmid17056094>{{Cite journal | last1 = Wang | first1 = KL. | last2 = Weinrach | first2 = DM. | last3 = Luan | first3 = C. | last4 = Han | first4 = M. | last5 = Lin | first5 = F. | last6 = Teh | first6 = BT. | last7 = Yang | first7 = XJ. | title = Renal papillary adenoma--a putative precursor of papillary renal cell carcinoma. | journal = Hum Pathol | volume = 38 | issue = 2 | pages = 239-46 | month = Feb | year = 2007 | doi = 10.1016/j.humpath.2006.07.016 | PMID = 17056094 }}</ref>
| |
| **Stains like PaRCC.
| |
| **Found with an increased frequency within the content of PaRCC.
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| #Histomorphology of ''[[papillary renal cell carcinoma]]''.
| |
| #'''''Must''''' be <=0.5 cm.<ref name=Ref_GUP288>{{Ref GUP|288}}</ref><ref name=pmid18846240>{{Cite journal | last1 = Algaba | first1 = F. | title = Renal adenomas: pathological differential diagnosis with malignant tumors. | journal = Adv Urol | volume = | issue = | pages = 974848 | month = | year = 2008 | doi = 10.1155/2008/974848 | PMID = 18846240 | PMC = 2563151 | URL = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563151/?tool=pubmed }}</ref>
| |
| #*[[Diagnostic size cutoff]] - larger lesions are ''papillary renal cell carcinoma''.
| |
| | |
| DDx:
| |
| *[[Papillary renal cell carcinoma]].
| |
| *[[Metanephric adenoma]].
| |
| | |
| Images:
| |
| *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563151/figure/fig2/ Renal papillary adenoma (nih.gov)].<ref name=pmid18846240/>
| |
| | |
| ===IHC===
| |
| *AMACR +ve.<ref name=pmid17056094/>
| |
|
| |
|
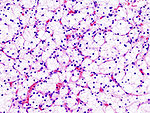
| ==Renal oncocytoma== | | ==Renal oncocytoma== |
| ===General===
| | {{Main|Renal oncocytoma}} |
| *Can be difficult to distinguish radiologically from RCC (chromophobe subtype).
| |
| ** ... and pathologists occasionally struggle like the radiologists.
| |
| *Benign tumour - the reason it is excised is... one cannot be certain it isn't a RCC.
| |
| | |
| ===Gross===
| |
| *Brown, mahogany brown.
| |
| *1/3 have a characteristic central scar.<ref name=Ref_GUP302>{{Ref GUP|302}}</ref>
| |
| | |
| Image:
| |
| *[http://en.wikipedia.org/wiki/File:Renal_oncocytoma.jpg Renal oncocytoma with central scar (WP)].
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Eosinophilic cytoplasm - slightly granular '''key feature'''.
| |
| *Cells arranged in nests.
| |
| *Nuclei uniform and round.<ref name=Ref_GUP302>{{Ref GUP|302}}</ref>
| |
| **Slightly enlarged nuclei, but '''no significant''' pleomorphism (size variation) - '''important'''.
| |
| | |
| Notes:
| |
| *May look like eosinophilic variant of chromophobe RCC -- this is the main DDx.
| |
| **A comparison based on histomorphology: ''[[Kidney_tumours#Tabular_comparison_of_oncocytoma_and_chromophobe_RCC|Tabular comparison between ChRCC & oncocytoma]]''.
| |
| ***Oncocytoma typically has: no perinuclear clearing, no raisinoid nuclei, no binucleation.
| |
| | |
| DDx:
| |
| *[[Chromophobe renal cell carcinoma]], eosinophilic variant.
| |
| *[[Clear cell renal cell carcinoma]], eosinophilic variant.
| |
| | |
| Images:
| |
| *[http://commons.wikimedia.org/wiki/File:Renal_oncocytoma2.jpg High mag. oncocytoma (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Renal_oncocytoma3.jpg Intermed. mag. oncocytoma (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Renal_oncocytoma4.jpg Low mag. oncocytoma (WC)].
| |
| | |
| ===Stains===
| |
| *[[Hale's colloidal iron]] -ve
| |
| **[[ChRCC]] +ve (blue granular cytoplasmic).
| |
| | |
| ===IHC===
| |
| *CK7 -ve<ref name=pmid17683191>{{Cite journal | last1 = Liu | first1 = L. | last2 = Qian | first2 = J. | last3 = Singh | first3 = H. | last4 = Meiers | first4 = I. | last5 = Zhou | first5 = X. | last6 = Bostwick | first6 = DG. | title = Immunohistochemical analysis of chromophobe renal cell carcinoma, renal oncocytoma, and clear cell carcinoma: an optimal and practical panel for differential diagnosis. | journal = Arch Pathol Lab Med | volume = 131 | issue = 8 | pages = 1290-7 | month = Aug | year = 2007 | doi = 10.1043/1543-2165(2007)131[1290:IAOCRC]2.0.CO;2 | PMID = 17683191 }}</ref>/+ve (cytoplasmic) .
| |
| **Chromophobe renal cell carcinoma = cell membrane +ve.
| |
| | |
| ===Sign out===
| |
| <pre>
| |
| PORTION OF KIDNEY, RIGHT, PARTIAL NEPHRECTOMY:
| |
| - ONCOCYTOMA.
| |
| </pre>
| |
| | |
| ====Micro====
| |
| The sections show a tumour with cells arranged in nests. The tumour cells have abundant
| |
| eosinophilic cytoplasm. The tumour cell nuclei are round and have round nucleoli. No
| |
| perinuclear halos are apparent. Binucleation is not apparent. No zonal necrosis is
| |
| identified. Focally, tumour nests are spaced reminiscent of an archipelago. Mitoses are not
| |
| apparent. The tumour is moderately circumscribed.
| |
| | |
| The thin rim of renal parenchyma has no apparent pathology on the H&E stained sections.
| |
|
| |
|
| ==Angiomyolipoma== | | ==Angiomyolipoma== |
| *Abbreviated ''AML''. | | *Abbreviated ''AML''. |
| ===General===
| | {{Main|Angiomyolipoma}} |
| *Benign mesenchymal tumour.
| |
| *Presentations: flank pain, hematuria, incidentaloma.<ref name=pmid18805573>{{Cite journal | last1 = Seyam | first1 = RM. | last2 = Bissada | first2 = NK. | last3 = Kattan | first3 = SA. | last4 = Mokhtar | first4 = AA. | last5 = Aslam | first5 = M. | last6 = Fahmy | first6 = WE. | last7 = Mourad | first7 = WA. | last8 = Binmahfouz | first8 = AA. | last9 = Alzahrani | first9 = HM. | title = Changing trends in presentation, diagnosis and management of renal angiomyolipoma: comparison of sporadic and tuberous sclerosis complex-associated forms. | journal = Urology | volume = 72 | issue = 5 | pages = 1077-82 | month = Nov | year = 2008 | doi = 10.1016/j.urology.2008.07.049 | PMID = 18805573 }}</ref>
| |
| **Tumours >4 cm considered a risk for bleeding.<ref name=pmid21571778>{{Cite journal | last1 = Abrams | first1 = J. | last2 = Yee | first2 = DC. | last3 = Clark | first3 = TW. | title = Transradial embolization of a bleeding renal angiomyolipoma. | journal = Vasc Endovascular Surg | volume = 45 | issue = 5 | pages = 470-3 | month = Jul | year = 2011 | doi = 10.1177/1538574411408352 | PMID = 21571778 }}</ref>
| |
| *AMLs occur may be elsewhere in the body, e.g. liver,<ref name=pmid15498214>{{Cite journal | last1 = Zhang | first1 = SH. | last2 = Cong | first2 = WM. | last3 = Xian | first3 = ZH. | last4 = Wu | first4 = WQ. | last5 = Dong | first5 = H. | last6 = Wu | first6 = MC. | title = [Morphologic variants and immunohistochemical features of hepatic angiomyolipoma.] | journal = Zhonghua Bing Li Xue Za Zhi | volume = 33 | issue = 5 | pages = 437-40 | month = Oct | year = 2004 | doi = | PMID = 15498214 }}
| |
| </ref> but are most common in the kidney.
| |
| *In the [[PEComa]] group of tumours.
| |
| | |
| ====Epidemiology====
| |
| *May be associated with [[tuberous sclerosis]] -- 70% have an AML.
| |
| **When compared to sporadic cases:
| |
| ***More often bilateral.
| |
| ***Usually bigger.
| |
| *There is a suggestion that an ''epithelioid'' variant is more worisome.<ref name=pmid12352384>{{Cite journal | last1 = Nelson | first1 = CP. | last2 = Sanda | first2 = MG. | title = Contemporary diagnosis and management of renal angiomyolipoma. | journal = J Urol | volume = 168 | issue = 4 Pt 1 | pages = 1315-25 | month = Oct | year = 2002 | doi = 10.1097/01.ju.0000028200.86216.b2 | PMID = 12352384 }}</ref>
| |
| **This is not confirmed by all studies.<ref name=pmid18852677>{{Cite journal | last1 = Aydin | first1 = H. | last2 = Magi-Galluzzi | first2 = C. | last3 = Lane | first3 = BR. | last4 = Sercia | first4 = L. | last5 = Lopez | first5 = JI. | last6 = Rini | first6 = BI. | last7 = Zhou | first7 = M. | title = Renal angiomyolipoma: clinicopathologic study of 194 cases with emphasis on the epithelioid histology and tuberous sclerosis association. | journal = Am J Surg Pathol | volume = 33 | issue = 2 | pages = 289-97 | month = Feb | year = 2009 | doi = 10.1097/PAS.0b013e31817ed7a6 | PMID = 18852677 }}</ref>
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Smooth muscle.
| |
| *Adipose tissue - not always present<ref name=pmid15584043>{{Cite journal | last1 = Crapanzano | first1 = JP. | title = Fine-needle aspiration of renal angiomyolipoma: cytological findings and diagnostic pitfalls in a series of five cases. | journal = Diagn Cytopathol | volume = 32 | issue = 1 | pages = 53-7 | month = Jan | year = 2005 | doi = 10.1002/dc.20179 | PMID = 15584043 }}</ref> - '''key feature'''.
| |
| *Abundant blood vessels.
| |
| | |
| ====Epithelioid angiomyolipoma====
| |
| Features:
| |
| *Carcinoma-like morphology.
| |
| *+/-Spindle cells.
| |
| *"High grade" nuclei.
| |
| **Pleomorphic nuclei.
| |
| | |
| DDx:
| |
| *[[Clear cell renal cell carcinoma]] eosinophilic variant - esp. if epithelioid.
| |
| | |
| Images:
| |
| *[http://bjr.birjournals.org/content/82/984/e249/F3.expansion.html Epithelioid AML (birjournals.org)].
| |
| *[http://radiographics.rsna.org/content/30/6/1525/F2.expansion.html Epithelioid AML (rsna.org)].
| |
| | |
| ====Cytologic====
| |
| Features<ref name=pmid15584043>{{Cite journal | last1 = Crapanzano | first1 = JP. | title = Fine-needle aspiration of renal angiomyolipoma: cytological findings and diagnostic pitfalls in a series of five cases. | journal = Diagn Cytopathol | volume = 32 | issue = 1 | pages = 53-7 | month = Jan | year = 2005 | doi = 10.1002/dc.20179 | PMID = 15584043 }}</ref>
| |
| *Nuclei - round/ovoid.
| |
| *Chromatin - bland.
| |
| | |
| ===IHC===
| |
| *Melanocytic markers +ve<ref name=Ref_GUP324>{{Ref GUP|324}}</ref> (e.g. HMB-45 +ve).
| |
| *Epithelial markers -ve.<ref name=Ref_GUP324>{{Ref GUP|324}}</ref>
| |
| *SMA +ve.
| |
| *CD117 +ve/-ve.
| |
| | |
| *Ki-67:<ref name=pmid18839327>{{Cite journal | last1 = Ooi | first1 = SM. | last2 = Vivian | first2 = JB. | last3 = Cohen | first3 = RJ. | title = The use of the Ki-67 marker in the pathological diagnosis of the epithelioid variant of renal angiomyolipoma. | journal = Int Urol Nephrol | volume = 41 | issue = 3 | pages = 559-65 | month = | year = 2009 | doi = 10.1007/s11255-008-9473-1 | PMID = 18839327 }}</ref>
| |
| **Epithelioid variant of AML +ve.
| |
| **Conventional AML -ve.
| |
|
| |
|
| =Mimics= | | =Mimics= |
| ==Xanthogranulomatous pyelonephritis== | | ==Xanthogranulomatous pyelonephritis== |
| ===General===
| | *Abbreviated ''XGP''. |
| *May mimic [[RCC]] - espically radiologically. | | {{Main|Xanthogranulomatous pyelonephritis}} |
| *Usually lower pole.{{fact}}
| |
| *Associated with:
| |
| **[[Diabetes mellitus]].
| |
| **History of UTI.<ref name=pmid17987581>{{cite journal |author=Afgan F, Mumtaz S, Ather MH |title=Preoperative diagnosis of xanthogranulomatous pyelonephritis |journal=Urol J |volume=4 |issue=3 |pages=169–73 |year=2007 |pmid=17987581 |doi= |url=}}</ref>
| |
| **Nephrolithiasis.
| |
| **GU obstruction.<ref name=pmid17098659>{{cite journal |author=Al-Ghazo MA, Ghalayini IF, Matalka II, Al-Kaisi NS, Khader YS |title=Xanthogranulomatous pyelonephritis: Analysis of 18 cases |journal=Asian J Surg |volume=29 |issue=4 |pages=257–61 |year=2006 |month=October |pmid=17098659 |doi= |url=}}</ref>
| |
| *Occasionally an indication of nephrectomy.<ref name=pmid17987581/><ref name=pmid17098659/>
| |
| *Most common organism (in the context of nephrectomy specimens) - ''Proteus mirabilis''.<ref name=pmid17098659/>
| |
| | |
| ===Microscopic===
| |
| *Abundant macrophages.
| |
| *+/-Giant cells.
| |
| | |
| DDx:
| |
| *[[Malakoplakia]].
| |
| **Basophilic inclusions -- inside or outside of macrophages - often size of RBC or larger ([[Michaelis-Gutmann bodies]]).
| |
| *RCC - especially [[PRCC]] (as this has foamy macrophages).
| |
| *Granulomatous disease.
| |
| *[[Chronic pyelonephritis]].
| |
| *[[Interstitial nephritis]].
| |
| | |
| Image:
| |
| *[http://commons.wikimedia.org/wiki/File:Xanthogranulomatous_pyelonephritis_cd68.jpg Xanthogranulomatous pyelonephritis - CD68 IHC (WC)].
| |
| | |
| ===Stains===
| |
| *[[PAS-D]] -ve.
| |
| **Done to look for malakoplakia.
| |
| | |
| ===IHC===
| |
| *CD68 +ve.
| |
| *RCC markers (CD10, RCC) all negative.
| |
|
| |
|
| ==Malakoplakia== | | ==Malakoplakia== |
| Line 958: |
Line 389: |
| =Rare stuffs= | | =Rare stuffs= |
| ==Juxtaglomerular cell tumour== | | ==Juxtaglomerular cell tumour== |
| *[[AKA]] juxtaglomerular tumour, reninoma.<ref name=pmid18192852/> | | *[[AKA]] juxtaglomerular tumour, reninoma.<ref name=pmid18192852>{{Cite journal | last1 = Wong | first1 = L. | last2 = Hsu | first2 = TH. | last3 = Perlroth | first3 = MG. | last4 = Hofmann | first4 = LV. | last5 = Haynes | first5 = CM. | last6 = Katznelson | first6 = L. | title = Reninoma: case report and literature review. | journal = J Hypertens | volume = 26 | issue = 2 | pages = 368-73 | month = Feb | year = 2008 | doi = 10.1097/HJH.0b013e3282f283f3 | PMID = 18192852 }}</ref> |
| ===General===
| | {{Main|Juxtaglomerular cell tumour}} |
| *Rare.
| |
| *Etiology: increased renin.
| |
| | |
| Clinical:<ref name=pmid18192852>{{Cite journal | last1 = Wong | first1 = L. | last2 = Hsu | first2 = TH. | last3 = Perlroth | first3 = MG. | last4 = Hofmann | first4 = LV. | last5 = Haynes | first5 = CM. | last6 = Katznelson | first6 = L. | title = Reninoma: case report and literature review. | journal = J Hypertens | volume = 26 | issue = 2 | pages = 368-73 | month = Feb | year = 2008 | doi = 10.1097/HJH.0b013e3282f283f3 | PMID = 18192852 }}</ref>
| |
| *[[Hypertension]].
| |
| *Increased aldosterone.
| |
| **Causes hypokalemia.
| |
| *Increased plasma renin.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=pmid21191395/>
| |
| *Polygonal cells.
| |
| *Abundant granular, eosinophilic cytoplasm.<ref name=pmid436071/>
| |
| *Perinuclear halo.
| |
| | |
| DDx:
| |
| *[[Chromophobe renal cell carcinoma]], eosinophilic variant.
| |
| | |
| Image:
| |
| *[http://www.nature.com/ki/journal/v79/n2/fig_tab/ki2010445f1.html#figure-title Reninoma (nature.com)].<ref name=pmid21191395/>
| |
| | |
| ===Stains===
| |
| Cytoplasmic granules.<ref name=pmid436071>{{Cite journal | last1 = Hanna | first1 = W. | last2 = Tepperman | first2 = B. | last3 = Logan | first3 = AG. | last4 = Robinette | first4 = MA. | last5 = Colapinto | first5 = R. | last6 = Phillips | first6 = MJ. | title = Juxtaglomerular cell tumour (reninoma) with paroxysmal hypertension. | journal = Can Med Assoc J | volume = 120 | issue = 8 | pages = 957-9 | month = Apr | year = 1979 | doi = | PMID = 436071 PMC = 1819229 | URL = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1819229/?tool=pubmed }}</ref>
| |
| *PAS +ve.
| |
| *PASD +ve.
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid21191395>{{Cite journal | last1 = Chao | first1 = CT. | last2 = Chang | first2 = FC. | last3 = Wu | first3 = VC. | last4 = Chen | first4 = JC. | title = Reninoma. | journal = Kidney Int | volume = 79 | issue = 2 | pages = 260 | month = Jan | year = 2011 | doi = 10.1038/ki.2010.445 | PMID = 21191395 }}</ref>
| |
| *Actin +ve.
| |
| *Cytokeratin -ve.
| |
| *HMB-45 -ve.
| |
| | |
| ===EM===
| |
| Features:
| |
| *Vesicles - contain renin.<ref name=upmc29>URL: [http://path.upmc.edu/cases/case29/micro.html http://path.upmc.edu/cases/case29/micro.html]. Accessed on: 18 December 2011.</ref>
| |
|
| |
|
| ==Renomedullary interstitial cell tumour== | | ==Renomedullary interstitial cell tumour== |
| *[[AKA]] ''medullary fibroma''.<ref name=pmid11054036 >{{Cite journal | last1 = Bircan | first1 = S. | last2 = Orhan | first2 = D. | last3 = Tulunay | first3 = O. | last4 = Safak | first4 = M. | title = Renomedullary interstitial cell tumor. | journal = Urol Int | volume = 65 | issue = 3 | pages = 163-6 | month = | year = 2000 | doi = | PMID = 11054036 }}</ref> | | *[[AKA]] ''medullary fibroma''.<ref name=pmid11054036 >{{Cite journal | last1 = Bircan | first1 = S. | last2 = Orhan | first2 = D. | last3 = Tulunay | first3 = O. | last4 = Safak | first4 = M. | title = Renomedullary interstitial cell tumor. | journal = Urol Int | volume = 65 | issue = 3 | pages = 163-6 | month = | year = 2000 | doi = | PMID = 11054036 }}</ref> |
| | | {{Main|Renomedullary interstitial cell tumour}} |
| ===General===
| |
| *Benign.
| |
| *Common [[autopsy]] finding<ref name=Ref_WMSP295>{{Ref WMSP|295}}</ref> - one review says 26-41% of individuals at autopsy.<ref name=pmid10689882>{{Cite journal | last1 = Tsurukawa | first1 = H. | last2 = Iuchi | first2 = H. | last3 = Osanai | first3 = H. | last4 = Yamaguchi | first4 = S. | last5 = Hashimoto | first5 = H. | last6 = Kaneko | first6 = S. | last7 = Yachiku | first7 = S. | title = [Renomedullary interstitial cell tumor: a case report]. | journal = Nihon Hinyokika Gakkai Zasshi | volume = 91 | issue = 1 | pages = 37-40 | month = Jan | year = 2000 | doi = | PMID = 10689882 }}</ref>
| |
| **The commonality is somewhat in dispute.<ref name=pmid18655367>{{Cite journal | last1 = Kozłowska | first1 = J. | last2 = Okoń | first2 = K. | title = Renal tumors in postmortem material. | journal = Pol J Pathol | volume = 59 | issue = 1 | pages = 21-5 | month = | year = 2008 | doi = | PMID = 18655367 }}</ref>
| |
| | |
| ===Gross===
| |
| *Small, white well-circumscribed nodule in medulla.
| |
| **Typically less than 3 mm.<ref name=pmid10689882/>
| |
| | |
| Image:
| |
| *[http://library.med.utah.edu/WebPath/RENAHTML/RENAL155.html Renal medullary fibroma (utah.edu)].
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_WMSP295>{{Ref WMSP|295}}</ref><ref>URL: [http://webpathology.com/image.asp?n=16&Case=71 http://webpathology.com/image.asp?n=16&Case=71]. Accessed on: 17 October 2011.</ref>
| |
| *Small polygonal/stellate cells.
| |
| *Abundant loose/[[myxoid stroma]].
| |
| *+/-Entrapped renal tubules.<ref name=pmid12066202>{{Cite journal | last1 = Kuroda | first1 = N. | last2 = Toi | first2 = M. | last3 = Miyazaki | first3 = E. | last4 = Hayashi | first4 = Y. | last5 = Nakayama | first5 = H. | last6 = Hiroi | first6 = M. | last7 = Enzan | first7 = H. | title = Participation of alpha-smooth muscle actin-positive cells in renomedullary interstitial cell tumors. | journal = Oncol Rep | volume = 9 | issue = 4 | pages = 745-50 | month = | year = | doi = | PMID = 12066202 }}</ref>
| |
| | |
| Images:
| |
| *www:
| |
| **[http://webpathology.com/image.asp?case=71&n=15 Renomedullary interstitial cell tumour - low mag. (webpathology.com)].
| |
| **[http://webpathology.com/image.asp?n=16&Case=71 Renomedullary interstitial cell tumour - high mag. (webpathology.com)].
| |
| *[[WC]]:
| |
| **[http://commons.wikimedia.org/wiki/File:Renal_medullary_fibroma_-_low_mag.jpg Renal medullary fibroma - low mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Renal_medullary_fibroma_-_intermed_mag.jpg Renal medullary fibroma - intermed. mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Renal_medullary_fibroma_-_very_high_mag.jpg Renal medullary fibroma - very high mag. (WC)].
| |
|
| |
|
| ==Metanephric adenoma== | | ==Metanephric adenoma== |
| *Should '''not''' be confused ''[[mesonephric adenoma]]'', another term for ''nephrogenic adenoma''. | | *Should '''not''' be confused ''[[mesonephric adenoma]]'', another term for ''nephrogenic adenoma''. |
| **Memory device: me'''t'''anephric adenoma is a '''t'''umour. | | **Memory device: me'''t'''anephric adenoma is a '''t'''umour. |
| | | {{Main|Metanephric adenoma}} |
| ===General===
| |
| *Benign.
| |
| *Afflicts adults and occasionally children.
| |
| *May be associated with [[polycythemia]].<ref name=pmid21220212>{{Cite journal | last1 = Le Nué | first1 = R. | last2 = Marcellin | first2 = L. | last3 = Ripepi | first3 = M. | last4 = Henry | first4 = C. | last5 = Kretz | first5 = JM. | last6 = Geiss | first6 = S. | title = Conservative treatment of metanephric adenoma. A case report and review of the literature. | journal = J Pediatr Urol | volume = 7 | issue = 4 | pages = 399-403 | month = Aug | year = 2011 | doi = 10.1016/j.jpurol.2010.09.010 | PMID = 21220212 }}</ref>
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_WMSP284>{{Ref WMSP|284}}</ref>
| |
| *Small uniform cells with:
| |
| **Fine chromatin.
| |
| **No apparent [[nucleolus]].
| |
| **A relatively smooth nuclear membrane.
| |
| *Variable architecture - may be sheets or ductal.
| |
| | |
| DDx:
| |
| *Epithelioid nephroblastoma ([[Wilms tumour]]) - these typically have:
| |
| **Irregular nuclear membrane.
| |
| **Nucleoli.
| |
| **Mitoses (rare in ''metanephric adenoma'').
| |
| *[[Papillary renal cell carcinoma|Papillary RCC]].<ref name=Ref_WMSP284>{{Ref WMSP|284}}</ref>
| |
| | |
| Images:
| |
| *www:
| |
| **[http://www.nature.com/modpathol/journal/v16/n10/fig_tab/3880886f1.html Metanephric adenoma (nature.com)].
| |
| *[[WC]]:
| |
| **[http://commons.wikimedia.org/wiki/File:Metanephric_adenoma_high_mag.jpg Metanephric adenoma (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Metanephric_adenoma_high_mag_cropped.jpg Metanephric adenoma - cropped (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Metanephric_adenoma_-_intermed_mag.jpg Metanephric adenoma - PaRCC-like - intermed. mag. (WC)].
| |
| **[http://commons.wikimedia.org/wiki/File:Metanephric_adenoma_-_very_high_mag.jpg Metanephric adenoma - PaRCC-like - very high mag. (WC)].
| |
| | |
| ===IHC===
| |
| *WT-1 +ve.
| |
| *CD57 +ve.
| |
| *CK7 +ve.<ref name=pmid19730362/> (???)
| |
| *PAX2 +ve.<ref name=pmid16400326>{{Cite journal | last1 = Tong | first1 = GX. | last2 = Melamed | first2 = J. | last3 = Mansukhani | first3 = M. | last4 = Memeo | first4 = L. | last5 = Hernandez | first5 = O. | last6 = Deng | first6 = FM. | last7 = Chiriboga | first7 = L. | last8 = Waisman | first8 = J. | title = PAX2: a reliable marker for nephrogenic adenoma. | journal = Mod Pathol | volume = 19 | issue = 3 | pages = 356-63 | month = Mar | year = 2006 | doi = 10.1038/modpathol.3800535 | PMID = 16400326 }}</ref>
| |
| *MUC1 +ve.
| |
| **Marks distal renal tubule.<ref name=pmid19730362>{{Cite journal | last1 = Fromont | first1 = G. | last2 = Barcat | first2 = L. | last3 = Gaudin | first3 = J. | last4 = Irani | first4 = J. | title = Revisiting the immunophenotype of nephrogenic adenoma. | journal = Am J Surg Pathol | volume = 33 | issue = 11 | pages = 1654-8 | month = Nov | year = 2009 | doi = 10.1097/PAS.0b013e3181b40061 | PMID = 19730362 }}</ref>
| |
|
| |
|
| ==Renal epithelial and stromal tumour== | | ==Renal epithelial and stromal tumour== |
| | :Abbreviated ''REST''. |
| The lumping term for both:<ref name=pmid17414095>{{Cite journal | last1 = Turbiner | first1 = J. | last2 = Amin | first2 = MB. | last3 = Humphrey | first3 = PA. | last4 = Srigley | first4 = JR. | last5 = De Leval | first5 = L. | last6 = Radhakrishnan | first6 = A. | last7 = Oliva | first7 = E. | title = Cystic nephroma and mixed epithelial and stromal tumor of kidney: a detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumor (REST) as a unifying term. | journal = Am J Surg Pathol | volume = 31 | issue = 4 | pages = 489-500 | month = Apr | year = 2007 | doi = 10.1097/PAS.0b013e31802bdd56 | PMID = 17414095 }}</ref> | | The lumping term for both:<ref name=pmid17414095>{{Cite journal | last1 = Turbiner | first1 = J. | last2 = Amin | first2 = MB. | last3 = Humphrey | first3 = PA. | last4 = Srigley | first4 = JR. | last5 = De Leval | first5 = L. | last6 = Radhakrishnan | first6 = A. | last7 = Oliva | first7 = E. | title = Cystic nephroma and mixed epithelial and stromal tumor of kidney: a detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumor (REST) as a unifying term. | journal = Am J Surg Pathol | volume = 31 | issue = 4 | pages = 489-500 | month = Apr | year = 2007 | doi = 10.1097/PAS.0b013e31802bdd56 | PMID = 17414095 }}</ref> |
| #[[Mixed epithelial and stromal tumour]]. | | #[[Mixed epithelial and stromal tumour]]. |
| Line 1,074: |
Line 409: |
| ==Mixed epithelial and stromal tumour== | | ==Mixed epithelial and stromal tumour== |
| *Abbreviated ''MEST''. | | *Abbreviated ''MEST''. |
| | | {{Main|Mixed epithelial and stromal tumour of the kidney}} |
| ===General===
| |
| *Rare - approx. 1.5% of renal neoplasms.<ref name=pmid17454754>{{Cite journal | last1 = Mai | first1 = KT. | last2 = Elkeilani | first2 = A. | last3 = Veinot | first3 = JP. | title = Mixed epithelial and stromal tumour (MEST) of the kidney: report of 14 cases with male and PEComatous variants and proposed histopathogenesis. | journal = Pathology | volume = 39 | issue = 2 | pages = 235-40 | month = Apr | year = 2007 | doi = 10.1080/00313020701230799 | PMID = 17454754 }}</ref>
| |
| *Benign.
| |
| *Prevalence: males > females.
| |
| | |
| Note:
| |
| *Turbiner ''et al.''<ref name=pmid17414095>{{Cite journal | last1 = Turbiner | first1 = J. | last2 = Amin | first2 = MB. | last3 = Humphrey | first3 = PA. | last4 = Srigley | first4 = JR. | last5 = De Leval | first5 = L. | last6 = Radhakrishnan | first6 = A. | last7 = Oliva | first7 = E. | title = Cystic nephroma and mixed epithelial and stromal tumor of kidney: a detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumor (REST) as a unifying term. | journal = Am J Surg Pathol | volume = 31 | issue = 4 | pages = 489-500 | month = Apr | year = 2007 | doi = 10.1097/PAS.0b013e31802bdd56 | PMID = 17414095 }}</ref> have suggested that ''cystic nephroma'' and ''mixed epithelial and stromal tumour (MEST)'' are one tumour.
| |
| **The lumping term ''renal epithelial and stromal tumour'', abbreviated ''REST''.
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Cysts lined by simple epithelium with hobnailing - '''key feature'''.
| |
| *Stroma has an ovarian look:
| |
| **''Blue'' (basophilic).
| |
| **''Spindle cells''.
| |
| | |
| Notes:
| |
| *Parenchymal elements (e.g. glomueruli, tubules) are not found in the septa between the cysts.
| |
| | |
| Images:
| |
| *[http://commons.wikimedia.org/wiki/File:Cystic_nephroma_low_mag.jpg Cystic nephroma - low mag. (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Cystic_nephroma_intermed_mag.jpg Cystic nephroma - intermed. mag. (WC)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid17454754>{{Cite journal | last1 = Mai | first1 = KT. | last2 = Elkeilani | first2 = A. | last3 = Veinot | first3 = JP. | title = Mixed epithelial and stromal tumour (MEST) of the kidney: report of 14 cases with male and PEComatous variants and proposed histopathogenesis. | journal = Pathology | volume = 39 | issue = 2 | pages = 235-40 | month = Apr | year = 2007 | doi = 10.1080/00313020701230799 | PMID = 17454754 }}
| |
| </ref>
| |
| *ER +ve.
| |
| *PR +ve.
| |
| *CD10 +ve.
| |
| | |
| ===DDx===
| |
| *Tubulocystic carcinoma.
| |
|
| |
|
| ==Cystic nephroma== | | ==Cystic nephroma== |
| | | {{Main|Cystic nephroma}} |
| ===General===
| |
| *Turbiner ''et al.''<ref name=pmid17414095>{{Cite journal | last1 = Turbiner | first1 = J. | last2 = Amin | first2 = MB. | last3 = Humphrey | first3 = PA. | last4 = Srigley | first4 = JR. | last5 = De Leval | first5 = L. | last6 = Radhakrishnan | first6 = A. | last7 = Oliva | first7 = E. | title = Cystic nephroma and mixed epithelial and stromal tumor of kidney: a detailed clinicopathologic analysis of 34 cases and proposal for renal epithelial and stromal tumor (REST) as a unifying term. | journal = Am J Surg Pathol | volume = 31 | issue = 4 | pages = 489-500 | month = Apr | year = 2007 | doi = 10.1097/PAS.0b013e31802bdd56 | PMID = 17414095 }}</ref> has suggested that ''[[cystic nephroma]]'' and ''[[mixed epithelial and stromal tumour]] (MEST)'' are one tumour.
| |
| **The lumping term is ''renal epithelial and stromal tumour'', abbreviated ''REST''.
| |
| | |
| ===Gross===
| |
| *Bubble wrap-like appearance.
| |
| | |
| Image:
| |
| *[http://commons.wikimedia.org/wiki/File:Bubble_Wrap.jpg Bubble wrap (WC)].
| |
| | |
| ===Microscopic===
| |
| Features:
| |
| *Cysts lined by simple epithelium with hobnailing - '''key feature'''.
| |
| *Stroma has an ovarian look:
| |
| **''Blue'' (basophilic).
| |
| **''Spindle cells''.
| |
| | |
| Notes:
| |
| *Parenchymal elements (e.g. glomueruli, tubules) are not found in the septa between the cysts.
| |
| | |
| Images:
| |
| *[http://commons.wikimedia.org/wiki/File:Cystic_nephroma_low_mag.jpg Cystic nephroma - low mag. (WC)].
| |
| *[http://commons.wikimedia.org/wiki/File:Cystic_nephroma_intermed_mag.jpg Cystic nephroma - intermed. mag. (WC)].
| |
| | |
| ===IHC===
| |
| Features:
| |
| *ER +ve.
| |
| *PR +ve.
| |
| *CD10 +ve.
| |
|
| |
|
| ==Renal mucinous tubular and spindle cell carcinoma== | | ==Renal mucinous tubular and spindle cell carcinoma== |
| *[[AKA]] ''renal mucinous tubular spindle cell carcinoma''. | | *[[AKA]] ''renal mucinous tubular spindle cell carcinoma''. |
| *[[AKA]] ''mucinous tubular and spindle cell carcinoma of the kidney''.<ref name=pmid16258504>{{Cite journal | last1 = Brandal | first1 = P. | last2 = Lie | first2 = AK. | last3 = Bassarova | first3 = A. | last4 = Svindland | first4 = A. | last5 = Risberg | first5 = B. | last6 = Danielsen | first6 = H. | last7 = Heim | first7 = S. | title = Genomic aberrations in mucinous tubular and spindle cell renal cell carcinomas. | journal = Mod Pathol | volume = 19 | issue = 2 | pages = 186-94 | month = Feb | year = 2006 | doi = 10.1038/modpathol.3800499 | PMID = 16258504 }}</ref> | | *[[AKA]] ''mucinous tubular and spindle cell carcinoma of the kidney''.<ref name=pmid16258504>{{Cite journal | last1 = Brandal | first1 = P. | last2 = Lie | first2 = AK. | last3 = Bassarova | first3 = A. | last4 = Svindland | first4 = A. | last5 = Risberg | first5 = B. | last6 = Danielsen | first6 = H. | last7 = Heim | first7 = S. | title = Genomic aberrations in mucinous tubular and spindle cell renal cell carcinomas. | journal = Mod Pathol | volume = 19 | issue = 2 | pages = 186-94 | month = Feb | year = 2006 | doi = 10.1038/modpathol.3800499 | PMID = 16258504 }}</ref> |
| ===General===
| | {{Main|Renal mucinous tubular and spindle cell carcinoma}} |
| *Rare.<ref name=pmid19494850>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 }}</ref>
| |
| *Accepted by WHO in 2004 as a separate entity.<ref name=pmid19805959>{{cite journal |author=Geramizadeh B, Salehipour M, Moradi A |title=Mucinous tubular and spindle cell carcinoma of kidney: a rare case report and review of the literature |journal=Indian J Pathol Microbiol |volume=52 |issue=4 |pages=514–6 |year=2009 |pmid=19805959 |doi=10.4103/0377-4929.56144 |url=}}</ref>
| |
| *Relatively good prognosis.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=pmid19066686>{{cite journal |author=Trabelsi A, Stita W, Yacoubi MT, Rammeh S, Hmissa S, Korbi S |title=Renal mucinous tubular and spindle cell carcinoma |journal=Can Urol Assoc J |volume=2 |issue=6 |pages=635–6 |year=2008 |month=December |pmid=19066686 |pmc=2593603 |doi= |url=}}</ref>
| |
| *Mucin - may be scant.
| |
| *Spindle cells.
| |
| | |
| DDx:
| |
| *Sarcomatoid [[papillary renal cell carcinoma]].<ref name=pmid18941398>{{cite journal |author=Dhillon J, Amin MB, Selbs E, Turi GK, Paner GP, Reuter VE |title=Mucinous tubular and spindle cell carcinoma of the kidney with sarcomatoid change |journal=Am. J. Surg. Pathol. |volume=33 |issue=1 |pages=44–9 |year=2009 |month=January |pmid=18941398 |doi=10.1097/PAS.0b013e3181829ed5 |url=}}</ref>
| |
| | |
| Images:
| |
| *[http://moon.ouhsc.edu/kfung/jty1/OPAQ/PathQuiz-Answer/K1A001-PQ01-Ans.htm RMTSCC (ouhsc.edu)].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid16231179>{{cite journal |author=Ferlicot S, Allory Y, Compérat E, ''et al.'' |title=Mucinous tubular and spindle cell carcinoma: a report of 15 cases and a review of the literature |journal=Virchows Arch. |volume=447 |issue=6 |pages=978–83 |year=2005 |month=December |pmid=16231179 |doi=10.1007/s00428-005-0036-x |url=}}</ref>
| |
| *CD10 -ve.
| |
| *AE1/AE3 +ve.
| |
| *AMACR +ve.
| |
| *CK7 +ve.
| |
|
| |
|
| ==Collecting duct carcinoma== | | ==Collecting duct carcinoma== |
| *[[AKA]] ''Bellini duct carcinoma'',<ref name=pmid21393935>{{Cite journal | last1 = Stamatiou | first1 = K. | last2 = Zizi-Sermpetzoglou | first2 = A. | title = Bellini duct carcinoma accidentally found upon investigation of uric acid lithiasis. | journal = Indian J Pathol Microbiol | volume = 54 | issue = 1 | pages = 229-30 | month = | year = | doi = 10.4103/0377-4929.77425 | PMID = 21393935 }}</ref> [[AKA]] ''carcinoma of the collecting ducts of Bellini''.
| | {{Main|Collecting duct carcinoma}} |
| | |
| ===General===
| |
| *Rare.
| |
| *Poor prognosis.
| |
| *Usu. central location.
| |
| *Typically young adults.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=Ref_GUP295>{{Ref GUP|295}}</ref>
| |
| *Tubular structures with tapered ends.
| |
| **May be described as ''tubulopapillary''.
| |
| *[[Hobnail pattern]] - cell width smaller at basement membrane than free surface.<ref name=Ref_PBoD1018>{{Ref PBoD|1018}}</ref>
| |
| *High grade nuclear features (nuclear pleomorphism).
| |
| *High mitotic rate.
| |
| | |
| Notes:
| |
| *Benign urothelium must present to excluded urothelial carcinoma.
| |
| *Desmoplastic stroma may be prominent.
| |
| | |
| DDx:
| |
| *[[Papillary renal cell carcinoma]] - type 2.
| |
| *[[Urothelial carcinoma]].
| |
| | |
| ===IHC===
| |
| Features:<ref name=pmid19494850>{{Cite journal | last1 = Srigley | first1 = JR. | last2 = Delahunt | first2 = B. | title = Uncommon and recently described renal carcinomas. | journal = Mod Pathol | volume = 22 Suppl 2 | issue = | pages = S2-S23 | month = Jun | year = 2009 | doi = 10.1038/modpathol.2009.70 | PMID = 19494850 | URL = http://www.nature.com/modpathol/journal/v22/n2s/full/modpathol200970a.html }}</ref>
| |
| *CD117 +ve.
| |
| *E-cadherin +ve.
| |
| *CD10 -ve.
| |
| *AMACR -ve.
| |
|
| |
|
| ==Renal medullary carcinoma== | | ==Renal medullary carcinoma== |
| ===General===
| | {{Main|Renal medullary carcinoma}} |
| *Rare.
| |
| *Usually young adults.
| |
| *Associated with sickle cell trait (heterozygotes for the sickle cell allele).<ref name=pmid7528470>{{cite journal |author=Davis CJ, Mostofi FK, Sesterhenn IA |title=Renal medullary carcinoma. The seventh sickle cell nephropathy |journal=Am. J. Surg. Pathol. |volume=19 |issue=1 |pages=1–11 |year=1995 |month=January |pmid=7528470 |doi= |url=}}</ref>
| |
| *Aggressive/poor prognosis.<ref name=pmid17643096>{{Cite journal | last1 = Watanabe | first1 = IC. | last2 = Billis | first2 = A. | last3 = Guimarães | first3 = MS. | last4 = Alvarenga | first4 = M. | last5 = de Matos | first5 = AC. | last6 = Cardinalli | first6 = IA. | last7 = Filippi | first7 = RZ. | last8 = de Castro | first8 = MG. | last9 = Suzigan | first9 = S. | title = Renal medullary carcinoma: report of seven cases from Brazil. | journal = Mod Pathol | volume = 20 | issue = 9 | pages = 914-20 | month = Sep | year = 2007 | doi = 10.1038/modpathol.3800934 | PMID = 17643096 |url = http://www.nature.com/modpathol/journal/v20/n9/full/3800934a.html }}</ref>
| |
| | |
| Aside:
| |
| *Kidney disease assoc. with sickle cell disorders:<ref name=pmid7528470/>
| |
| *#Papillary necrosis.
| |
| *#[[Nephrotic syndrome]].
| |
| *#Renal [[infarction]].
| |
| *#[[Pyelonephritis]].
| |
| | |
| ===Gross===
| |
| Features:<ref name=pmid17643096>{{cite journal |author=Watanabe IC, Billis A, Guimarães MS, ''et al.'' |title=Renal medullary carcinoma: report of seven cases from Brazil |journal=Mod. Pathol. |volume=20 |issue=9 |pages=914–20 |year=2007 |month=September |pmid=17643096 |doi=10.1038/modpathol.3800934 |url=}}</ref>
| |
| *Well circumscribed.
| |
| *Renal medulla.
| |
| | |
| ===Microscopic===
| |
| Features:<ref name=pmid7528470/><ref name=pmid17643096>{{cite journal |author=Watanabe IC, Billis A, Guimarães MS, ''et al.'' |title=Renal medullary carcinoma: report of seven cases from Brazil |journal=Mod. Pathol. |volume=20 |issue=9 |pages=914–20 |year=2007 |month=September |pmid=17643096 |doi=10.1038/modpathol.3800934 |url=}}</ref>
| |
| *Variable architecture:
| |
| **Reticular - classic.
| |
| **[[Adenoid cystic carcinoma]]-like appearance:
| |
| ***Cystic spaces.
| |
| **Yolk sac-like.
| |
| **Tubular.
| |
| *Desmoplastic stroma - prominent.
| |
| *Inflammation:
| |
| **Lymphocytes.
| |
| **Neutrophils - margination in vessels.
| |
|
| |
|
| DDx:
| | ==Tubulocystic carcinoma of the kidney== |
| *[[Yolk sac tumour]].
| | {{Main|Tubulocystic carcinoma of the kidney}} |
| *[[Collecting duct carcinoma]].
| |
|
| |
|
| Image:
| | ==Acquired cystic disease-associated renal cell carcinoma== |
| *[http://www.nature.com/modpathol/journal/v20/n9/fig_tab/3800934f3.html#figure-title RMC (nature.com)].
| | {{Main|Acquired cystic disease-associated renal cell carcinoma}} |
|
| |
|
| ===IHC=== | | ==Kidney metastasis== |
| *SMARCB1 (INI1) -ve.<ref name=Ref_WMSP286>{{Ref WMSP|286}}</ref> | | *[[AKA]] ''renal metastasis'', ''metastatic kidney disease''. |
| | {{Main|Kidney metastasis}} |
|
| |
|
| =Pediatric= | | =Pediatric= |