Difference between revisions of "Breast pathology"
(get a few more images from the WikiCommons) |
(→Gynecomastoid hyperplasia: +images) |
||
| Line 344: | Line 344: | ||
*[[Micropapillary DCIS]] - buds not narrower toward the centre of the lumen. | *[[Micropapillary DCIS]] - buds not narrower toward the centre of the lumen. | ||
Images | ====Images==== | ||
<gallery> | |||
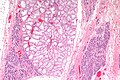
Image:Gynecomastoid_hyperplasia_-_intermed_mag.jpg | Gynecomastoid hyperplasia - intermed. mag. (WC/Nephron) | |||
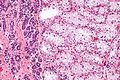
Image:Gynecomastoid_hyperplasia_-_very_high_mag.jpg | Gynecomastoid hyperplasia - very high mag. (WC/Nephron) | |||
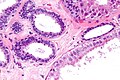
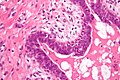
Image:Gynecomastoid_hyperplasia_-2-_intermed_mag.jpg | Gynecomastoid hyperplasia - 2 - intermed. mag. (WC/Nephron) | |||
</gallery> | |||
www: | |||
*[http://www.hsc.stonybrook.edu/breast-atlas/XIII-03.htm Gynecomastoid hyperplasia (stonybrook.edu)]. | |||
*[http://radiology.uchc.edu/eAtlas/Breast/1693.htm Gynecomastia (radiology.uchc.edu)]. | |||
=Lesions with increased risk of malignancy= | =Lesions with increased risk of malignancy= | ||
Revision as of 01:53, 15 May 2013
The breast is an important organ for the continuance of the species and one that pathologists see quite often because it is often afflicted by cancer. Before women started smoking in large numbers, it was the number one cause of cancer death in women (in Canada).
Fortunately, breast cancer, these days, has a relatively good prognosis if it is detected early... and this is why there are week-ends to end breast cancer -- there are large numbers of breast cancer survivors that are well, wealthy and can advocate for better care and research into breast cancer.
The world of pathology can neatly be divided into two... those that like the breast and those that don't.
Clinical
Classic presentation:
- Nipple discharge.
- Pain.
- Breast lump/mass.
- New nipple inversion.
- Skin changes, e.g. peau d'orange.
Most common presentation:
- Abnormal/suspicious screening mammogram - suspicious microcalcifications and/or suspicious mass.
Breast cancer screening
Breast cancer screening, for normal risk individuals, starts at age 50 in Canada. In the USA, breast screening starts at age 40.
Radiologic screening is less effective in younger individual as:
- The breast is more dense and thus radiologically more difficult to interpret, and
- The incidence of breast cancer is lower.
Breast radiology
BI-RADS = Breast Imaging Reporting And Data System:[1]
- 0: Incomplete - come back for more imaging (radiologist cha-ching).
- 1: Negative.
- 2: Benign finding(s).
- 3: Probably benign -- often short follow-up.
- 4: Suspicious abnormality -- needs biopsy.
- 5: Highly suggestive of malignancy.
- 6: Pathologist says there is a malignancy.
Specimens
Breast comes in three main flavours:
- Core needle biopsy (CNB).
- Lumpectomy.
- Modified radical mastectomy.
Note:
- Breast cytopathology is dealt with in the breast cytopathology article. It is almost dead, as it is not as sensitive and specific as CNB.
Core needle biopsy
Work-up of CNBs is dependent on the clinical abnormality:[2]
- Mass lesion - usu. obvious what is going on; typically 3 levels.
- Calcifications - abnormality may be very small; typically 10 levels.
Lumpectomy
Lumpectomies are usually oriented with short and long suture; short is typically superior (aspect) and long is typically lateral (aspect).
Modified radical mastectomy
- Usually done with sentinel lymph node biopsy - as one cannot go back later to do this.
Normal
Resting
- Glands -- normally has two cell layers (like the prostate).
- Myoepithelial cells
- Frequently spindle-like, often hard to see.
- Secretory cells.
- Myoepithelial cells
- Stroma:
- Not cellular.
- Not myxoid.
May be present:
- Calcification:
- Purple globs (with concentric rings) on H&E = calcium phosphate.
- Q. How to remember? A. Purple = Phosphate.
- Calcium oxalate visible with (light) polarization - not assoc. with malignancy.
- Often in the lumen of a gland, may be in the stroma.
- Calcific material typically has a well-demarcated border +/- "sharp corners".
- Radiologists can pick-up calcs (calcifications) that are approximately 100 micrometers; if "calcs" is on the requisition one needs to find calcs this size.[3]
- The large calcs seen on radiology are approximately 1/5 - 1/6 the size of a HPF, if the field of view (FOV) is ~0.55 mm (as is the case with 22 mm-10x eye pieces and a 40x objective).
- Purple globs (with concentric rings) on H&E = calcium phosphate.
Image:
Notes:
- The architecture is more important than the cytologic features in the diagnosis of malignancy in the breast;[4] low grade tumours have distorted architecture but normal/near normal cytology.
Lactational changes
General
- May be present focally in non-pregnant females.
ASIDE:
- Some believe lactational change and secretory change aren't the same...
- Lactational change = only in lactation.
- Secretory change = other times.
- This hair splitting is clinically irrelevant-- both are benign. Also, experts use the terms interchangeably.[6]
Microscopic
Features:[7]
- Glands dilated.
- Increased number of lobules.
- Relative decrease in intralobular and extralobular stroma.
- Luminal cells enlarged.
- Vacuolated cytoplasm.
- Hobnail morphology - hang into the lumen.
- Myoepithelial cells indistinct - after second trimester.
DDx:
Images
www:
- Lactational changes (gfmer.ch).
- Lactational changes in an angiosarcoma of the breast (webpathology.com).
- Lactating breast (uwa.edu.au).
Where to start
The following entities are a starting point for understanding routine breast pathology & some of challenges in breast pathology:
- Apocrine change.
- Pink benign cells.
- Columnar cell change.
- Columnar cells with blebs ("snouts") - often have calcifications (purple).
- Fibroadenoma.
- Abundant myxoid (light/blanched) stroma - very common.
- Florid epithelial hyperplasia.
- Too many cells in a duct, cells overlap & form slit-like spaces.
- Ductal carcinoma in situ (DCIS).
- Too many cells in a duct, nuclei do not touch - "cells are spaced".
- Cells line-up around ovoid/circular spaces - "punch-out" appearance/"cookie cutter" look.
- Myoepithelial cells present.
- Invasive ductal carcinoma.
- Bread & butter cancer - in sheets or glands.
- Lobular carcinoma.
- Dyscohesive cells - can easily be missed.
- Tubular carcinoma.
- Glands have one cell layer... but near normal appearance.
The key to breast pathology is... seeing the two cell layers (at low power). The myoepithelial layer is hard to see at times and that is the challenge.
Common diagnoses - overview
- Normal.
- Benign.
- Columnar cell change.
- Calcification often in lumen.
- Columnar cell change.
- Neoplastic.
- Benign neoplastic:
- Epithelial/myoepithelial - intraductal papilloma.
- Stromal - fibroadenoma, benign phyllodes.
- Malignant neoplastic:
- Epithelial/myoepithelial - most common, e.g. ductal carcinoma, lobular carcinoma.
- Breast stroma - malignant phyllodes tumour.
- Stromal, e.g. angiosarcoma - quite rare.
- Benign neoplastic:
A tree diagram (overview)
General classification
| Breast pathology | |||||||||||||||||||||||||||||||||||||||||||||||||
| Stromal pathology | Miscellaneous | Glandular pathology | |||||||||||||||||||||||||||||||||||||||||||||||
| Myxoid | Long slit-like spaces | Simple epithelium | Dilated | Cellular lesions | |||||||||||||||||||||||||||||||||||||||||||||
| Fibroadenoma | Malignant features | Benign features | Tubular carcinoma | FEA, FCC, CCC | FEHUT, Neoplastic, Malignant | ||||||||||||||||||||||||||||||||||||||||||||
| Malignant phyllodes | Benign phyllodes | ||||||||||||||||||||||||||||||||||||||||||||||||
Notes:
- The challenges in breast pathology are in: the Simple epithelium category and the Cellular lesions category.
- Neoplastic includes: ADH and LDH.
- Malignant includes: DCIS, LCIS, ductal carcinoma (DC) and lobular carcinoma (LC), some papillary lesions.
- Lobular carcinoma (a pitfall) may appear to be a stromal problem, i.e. the stroma looks too cellular.
- Miscellaneous includes rare tumours of the breast that do not fit into another category, i.e. metastases, lymphomas, melanoma, sarcomas. Skin-related pathology is dealt within the dermatologic neoplasms article. Paget disease of the breast, which may be seen in the context of malignant breast lesions, is discussed in its own article.
Cellular lesions
| Cellular lesions (Glandular) | |||||||||||||||||||||||||||||||||||||||||||||||
| Equal spacing, punched-out | Streaming, periph. slit-like spaces. | Discohesive cells, expanded gl. | Single cells or single file | Fibrovascular cores | |||||||||||||||||||||||||||||||||||||||||||
| Ductal lesion | FEHUT | Lobular lesion | Lobular carcinoma | Papillary lesions | |||||||||||||||||||||||||||||||||||||||||||
| Two cell layers | One cell layer | <50% of gl. | >50% of gl. | ||||||||||||||||||||||||||||||||||||||||||||
| Ductal non-inv. neoplasm | Ductal carcinoma | ALH | LCIS | ||||||||||||||||||||||||||||||||||||||||||||
| Large extent | Small extent | ||||||||||||||||||||||||||||||||||||||||||||||
| DCIS | ADH | ||||||||||||||||||||||||||||||||||||||||||||||
Notes:
- The largest challenge is: differentiating between the first two categories on level 2, i.e. equal spacing' vs. streaming.
- The fibrovascular cores must arise from a tuft, i.e. if they are arising directly from the wall of glands only it is likely papillary DCIS.
Papillary lesions
| Papillary lesions | |||||||||||||||||||||||||||||||||||||||
| Myoepithelial cells present | Myoepithelial cells absent | ||||||||||||||||||||||||||||||||||||||
| Unremarkable papillae | Atypia or arch. abnorm. or cellular proliferation | Neoplastic cells present | |||||||||||||||||||||||||||||||||||||
| Benign intraductal papilloma | High grade atypia | Low grade atypia or abnorm. arch. | Only cellular proliferation | Intracystic (encapsulated) papillary ca. | |||||||||||||||||||||||||||||||||||
| DCIS in papilloma | FEHUT in papilloma | ||||||||||||||||||||||||||||||||||||||
| >3 mm extent | <3 mm extent | ||||||||||||||||||||||||||||||||||||||
| DCIS in papilloma | ADH in papilloma | ||||||||||||||||||||||||||||||||||||||
Notes:
- Adapted from Mulligan & O'Malley.[8]
- The most important decision is the first one: myoepithelial cells present vs. absent.
- abnorm. arch. = abnormal architecture present.
- DCIS = ductal carcinoma in situ.
- FEHUT = florid epithelial hyperplasia of the usual type.
- extent refers to the size of the abnormal cell population within the papillary lesion.
Malignant lesions
Non-invasive breast cancer
This includes the in situ lesions - DCIS and LCIS.
Invasive breast cancer
This is includes descriptions of the usual types... and the not so common ones.
Common benign lesions
The breast has lots of benign things. Unlike the prostate, the where benign is called benign, everything has a name. It is more common among breast pathologists to sign-out things like: apocrine metaplasia (benign), columnar cell change (benign), and florid epithelial hyperplasia of the usual type (FEHUT) - instead of - benign breast tissue.
Mild epithelial hyperplasia
General
- No increased risk of malignancy.
- Often not reported - as it has not clinical signficance.
- Has to be separated from moderate epithelial hyperplasia / florid epithelial hyperplasia.
Microscopic
Features:[9]
- Breast glands with three or four cell layers above the basement membrane.
- Variable cells.
Note:
- No nuclear atypia.
DDx:
- Flat epithelial atypia.
- Moderate epithelial hyperplasia / florid epithelial hyperplasia.
- Atypical ductal hyperplasia.
Apocrine metaplasia
General
- Benign/not significant. Can be considered to be pretty wallpaper in the house of breast pathology.
Etiology
- Increased number of mitochondria.
- In other body sites this has different names, e.g. Hurthle cell change (thyroid), oncocytic change (kidney - oncocytoma, thyroid).
Microscopic
Features:
- Eosinophilic cytoplasm - key feature.
Note:
- Apocrine changes, i.e. cytoplasmic eosinophilia, can appear in malignant tumours; eosinophilia doesn't make something benign.
- Apocrine snouts may be present. (???)
- Small globules at the apical aspect of the cell (composed of cytoplasm and plasma membrane).
Images
Fibrocystic change
- Abbreviated FCC.
- AKA fibrocystic changes.
General
- Really common.
- Benign.
Microscopic
Features:
- Dilated glands - key change.
- Glands normal: two cell layers present.
- Often seen together with apocrine metaplasia.
Image:
- WC:
Columnar cell change
General
- Columnar cell change is associated with (benign) calcification - key point.
Microscopic
Features:
- Secretory cells (line gland lumen) have columnar morphology.
- May have "apical snouts".
- Blebs or round balls eosinophilic material appear to be adjacent to the cell at their luminal surface.
- The snouts are attached to the cell-- appear as round ball only in the plane of section.
- Cytoplasm +/-eosinophilia.
DDx:
- Flat epithelial atypia (>2 cell layers).[citation needed]
Image:
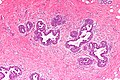
Gynecomastoid hyperplasia
- AKA gynecomastia.
General
- Benign enlargement of breasts in males.
- Histologic changes may be seen in females.[10]
May be seen in the context of:
- Liver failure.
- Klinefelter syndrome.
- Testicular estrogen-producing germ cell tumour.
Microscopic
Features:[10]
- Moderate hyperplasia.
- Glands have more than 2 cell layers.
- "Budding" - individual cells jut into the lumen - key feature.
- Buds may be multicellular; however, narrower toward the centre of the lumen.
- Stromal palor.[11]
DDx:
- Micropapillary DCIS - buds not narrower toward the centre of the lumen.
Images
www:
Lesions with increased risk of malignancy
Florid epithelial hyperplasia
- AKA florid epithelial hyperplasia, abbreviated FEH.
- AKA florid epithelial hyperplasia of the usual type, abbreviated FEHUT.
- AKA epithelial hyperplasia - term should be avoid as it could lead to confusion with mild epithelial hyperplasia.
General
- Mild increased risk of malignancy ~ 1.5-2x.[12]
- Has to be separated from mild epithelial hyperplasia.
Note:
- Moderate epithelial hyperplasia redirects to this section.
- It is generally not separated from FEH, as the prognosis is thought to be the same.
Microscopic
Features:[13]
- Breast glands with more than four cell layers above the basement membrane - key feature.
- Irregular cell spacing; streaming.
- Slit-like lumina, esp. at the periphery of the duct.
- No DCIS-like architecture (not cribriform, not papillary, not micropapillary, not solid).
- No nuclear atypia - usually no nucleoli.
Memory device CLEAN:
- Cell spacing is irregular, Lumina are slit-like, Extent is less than 2 mm or 2 ducts, Architecture not DCIS-like, Nuclear atypia not present.
DDx:
Sclerosing adenosis
General
- Can be scary... can look like ductal carcinoma.
- Derived from sclerosing[14] (hardening) and adenosis (glandular enlargement).
- Think scaring + lotsa glands and you're pretty close.
- Management: follow-up, no further treatment.[15]
Microscopic
Features:
- Acini are smaller than usual and there are more of them.
- Acini often slit-like.
- Fibrosis (scleroses) - pink on H&E surrounds the acini.
- Can mimic a desmoplastic reaction.
Notes:
- The acini should:
- Be in lobular arrangements, i.e. in groups (benign appearance at low power) - key feature.
- Have two cell layers like well-behaved breast glands do.
DDx:
- Low-grade ductal carcinoma.
- Tubular adenoma of the breast.
- Adenomyoepithelioma.[16]
Flat epithelial atypia
General
Epidemiology:
- Associated with ADH & DCIS; may represent a non-obligate precursor lesion of ADH & DCIS.[17]
- Low risk of progression to invasive malignancy.[18]
Management:
- Excision.
Microscopic
Features:
- "Flat" ~ three cells thick.
- Hypercellular gland -- several layers.
- Columnar cell morphology.
- +/-Apical snouts.
DDx:
- Columnar cell change.
- Columnar cell hyperplasia.
- ADH.
- Low grade DCIS.
- Apocrine cyst - granular cytoplasm.
- Tubular carcinoma - should be considered due to the association.
Molecular
- Loss of 16q.
- Not used for diagnosis.
Complex sclerosing lesion
- AKA radial scar.
General
- The term radial scar is a misnomer. It isn't a scar. It isn't associated with prior trauma or surgery.[19]
- May appear malignant on imaging.[20]
- Associated with subsequent elevated risk of breast cancer.[21]
- Management - usu. surgical excision.[22]
Gross
- Spiculated mass.
- Usually small - 3-7 mm.
Image:
Microscopic
- Stellate appearance (low magnification).
- Center of lesion has "fibroelastosis" - stroma light pink (on H&E) - key feature.
- Scar like stroma with entrapped normal breast ducts and lobules.
- Glands appear to enlarge with distance from center of lesion.
Notes:
- Histomorphologic appearance may mimic a desmoplastic reaction of the stroma - leading to a misdiagnosis of malignancy.
- "Hyaline - pink stuff on H&E - is the key."[24]
DDx:
- Invasive ductal carcinoma - should be considered if the lesion is asymmetrical or glands are dilated centrally.
Image:
IHC
Features:
- p63 +ve.
- Calponin +ve.
Note:
- HMWK +ve/-ve. (???)
Stromal lesions
This section (below) covers stromal lesions of the breast, which vary from benign to malignant. The most common is (the benign) fibroadenoma.
Non-breast stroma stromal lesions are covered in the soft tissue lesions article. Angiosarcoma (dealt with in the vascular tumours article) is the most common (non-breast stroma) sarcoma of the breast, and classically arises after treatment for a breast carcinoma.
Fibroadenoma
General
- Very common benign finding.
- The pathology is in the stroma; so, the lesion is really a misnomer by the naming rules.
- It ought to be called adenofibroma (as a few occasionally do[25]), as the glandular component is benign and the stromal component lesional; there is no truth in names in pathology.
Management:
- Local excision -- without a large margin.
Gross
Features:[26]
- Well-circumscribed.
- Rubbery - classic descriptor.
- Tan/white.
- +/-Lobulated appearance.
- +/-Slit-like spaces - short.
- +/-Calcification.
Images:
- Fibroadenoma - slit-like spaces (webpathology.com).
- Fibroadenoma - lobulated appearance (webpathology.com).
- Fibroadenoma (surgical-tutor.org).
Microscopic
Features:[27]
- Abundant (intralobular) stroma - most key feature.
- Stroma is usually:
- White/pale, i.e. myxoid, on H&E (normal stroma is pink).
- May be hyalinized (dark pink) if infarcted.
- Paucicellular - typical.
- White/pale, i.e. myxoid, on H&E (normal stroma is pink).
- Stroma is usually:
- Compression of glandular elements - very commonly seen.
- Glandular elements have at least two cell layers - epithelial and myoepithelial.
Notes:
- There is stuff about intracanalicular vs. pericanalicular.[28] It is irrelevant; there is no prognostic difference between the two.
- Do not comment on the margin - it is irrelevant.
DDx:
- Phyllodes tumour - long slit-like spaces (seen grossly), stroma is more cellular.
- +/-Mitoses,
- +/-"Stromal overgrowth" = large area where there is a 'loss of glands'.
- Sarcoma.
- Pseudoangiomatous stromal hyperplasia.
- Small capillary-like structures in the stroma.
- Epithelial component often not compressed - as in fibroadenoma.
- Small capillary-like structures in the stroma.
- Adenomyoepithelioma - for tubular adenoma of the breast.
Images:
Variants
Four variants are described by the Washington Manual:[31]
- Juvenile.
- Complex.
- Myxoid.
- Cellular.
Considered a variant of fibroadenoma by many authorities:[32]
Juvenile fibroadenoma
- As the name suggests, is typically found in younger patients.
- Classic history: rapid growth.
Features (juvenile variant):[33]
- Stromal and epithelial hyperplasia - key feature.
- +/-Tapering, thin micropapillae (gynecomastoid hyperplasia).[32]
- Mitoses uncommon.
Myxoid fibroadenoma
- May be associated with Carney's complex.
Features:
Cellular fibroadenoma
Features (cellular variant):
- Cellular.
- Mitoses.
Complex fibroadenoma
- Contain proliferative epithelium which outside and inside a fibroadenoma is associated with an increased risk of malignancy.
Features:[34]
- Apocrine metaplasia.
- Cysts > 3 mm.
- Calcification.
- Sclerosing adenosis.
Memory devices:
- FACS: complex fibroadenoma, apocrine metaplasia, calcs & cysts, sclerosing adenosis.
- CAMS: calcs, apocrine metaplasia, microcysts, sclerosing adenosis.
Tubular adenoma of the breast
- Considered by many a variant of fibroadenoma.
Features:[32]
- Fibromyxoid stroma (like in a fibroadenoma).
- Small round glands.
Image:
Phyllodes tumour
- Previously cystosarcoma phyllodes.
General
- The name comes from the word "leaf".
- With imagination or psychotropic drugs, it may look like one: the epithelial component = the veins of the leaf.
- Wide excision -- this differs from fibroadenoma (just local excision).
- Approximately 6% are malignant.[36]
Notes:
- There are case reports of phyllodes tumours in the prostate gland.[37]
- Outside of the breast a phyllodes-like histomorphology may represent an adenosarcoma.[38]
Gross
- Clefts/leaf-like structures.
- Friable - especially vis-à-vis a fibroadenoma.
Image:
Microscopic
Features - either 1, 2 or both of the following:
- Large slit-like spaces - key feature. †
- Cellular stroma - key feature. †
- May be myxoid.
- +/-Infiltrative border.
- +/-Mitoses.
- +/-Nuclear atypia.
- +/-"Stromal overgrowth" ~ stroma fills microscopic field.
Notes:
- † Large slit-like spaces are required for a benign phyllodes tumour.
- Slit-like spaces may absent in a borderline phyllodes or a malignant phyllodes.
- A cellular tumour without features suggestive of malignancy and without slit-like spaces is a cellular fibroadenoma.
- Some pathologists don't believe in cellular fibroadenoma - they call everything with stromal cellularity a phyllodes tumour.[39]
DDx:
- Fibroadenoma.
- Sarcoma.
Images:
Grading
Phyllodes tumours are graded:
- Benign.
- Borderline.
- Malignant.
Grading phyllodes tumours - based on WMSP:[40]
| Feature | Benign phyllodes | Borderline phyllodes | Malignant phyllodes |
|---|---|---|---|
| Circumscription | Well | Well | Poor |
| Stromal overgrowth † | none | none | may be present |
| Nuclear atypia | mild | mild-to-moderate | moderate-to-marked |
| Mitoses per 10 HPFs ‡ | < 5 | 5-10 | >10 |
| Heterologous elements | +/- benign | +/- benign | +/- malignant |
| DDx | fibroadenoma | benign phyllodes, malignant phyllodes | metaplastic breast carcinoma, sarcoma |
Notes:
- † Stromal overgrowth = epithelial elements absent in one low power field (LPF), defined as x40;[41] LPF is not adequately defined - see LPFitis.
- ‡ HPF is not adequately defined - see HPFitis.
Pseudoangiomatous stromal hyperplasia
General
- Benign lesion.
- Thought to arise due to myofibroblast abnormality - though not well understood.[43]
Gross
Features:[43]
- May form mass: grey-white & firm, with well circumscribed borders.
Microscopic
- Abundant breast stromal.
- Small, complex, inter-anastomosing (blood vessel/capillary-like) channels - key feature.
- Pseudoangiomatous = blood vessel-like.
Notes:
- May mimic angiosarcoma at low power; PASH may have the same architecture but lack nuclear atypia.
DDx:
Images:
IHC
Findings:[43]
Weird stuff
Like in all niches of pathology... there is weird stuff.
Mammary hamartoma
- AKA breast hamartoma.
General
- Benign.
- Disordered growth - see hamartoma.
Gross
- Well-circumscribed - key feature.
Microscopic
Features:[48]
- Disordered arrangement of ductal and lobular structures.
- Normal arrangement of cells with in the ductal structures, i.e. myoepithelium and epithelium present.
- Variable features:[49]
- Adipose tissue - predominant.
- Dense fibrosis tissue - predominant.
- Cystic glandular dilation.
Notes:
- If adipose tissue predominates; it may be labeled adenolipoma.[49]
DDx:
- Fibroadenoma - may have adipose tissue.
- Phyllodes tumour - may have adipose tissue.
- Pseudoangiomatous stromal hyperplasia.
- Fibrocystic changes.
Images:
IHC
- None - it's a H&E diagnosis.
Collagenous spherulosis
General
- Benign.
- Almost always an incidental finding.
- Can mimic ADH, cribriform DCIS, adenoid cystic carcinoma.[52]
Microscopic
- Tubular/cribriform architecture.
- Intratubular eosinophilic material - key feature.
- Classical: Arranged like the spokes of a wheel ("radial spikes").
- Atypical: Granules ~ 1-2 micrometers.
- No mitotic activity.
- Two cells populations (epithelial & myoepithelial) - like a well-behaved breast gland.
Notes:
- Usually small lesions: < 50 spherules per lesion, <100 micrometers.
- May be multifocal.
- +/-Calcifications - may prompt biopsy.
DDx:
Images:
- WC:
- www:
Nipple adenoma
- AKA nipple duct adenoma.
- AKA nipple adenoma of breast.
- AKA adenoma of the nipple.
- AKA florid papillomatosis of the nipple.[54]
General
- Rare.
- Reported in men.[54]
Clinical DDx:
Microscopic
Features:
- Proliferation of epithelial and myoepithelial elements that extends into the breast stroma.[56]
Notes:
DDx:
- Intraductal papilloma.
- Found within the duct not the stroma.
- Often deeper - one should not see skin in the histologic section.
Images:
- Nipple adenoma - low mag. (WC).
- Nipple adenoma - very high mag. (WC).
- Florid papillomatosis of the nipple - several images (breastpathology.info).
Intraductal papilloma
- AKA papilloma.
General
- May cause nipple discharge.[59]
- Similar to papillary hidradenoma of the vulva.
Microscopic
Features:
- True papillae - nipple-shaped structures with fibrovascular cores.
- Intraductal proliferation of epithelial and myoepithelial elements.[56]
Notes:
- Lacks florid hyperplasia.[60]
- May degeneration and hyalinize to form a sclerosing papilloma.
DDx:
- Intraductal papilloma with florid epithelial hyperplasia.
- Intraductal papilloma with atypical ductal hyperplasia. †
- Intraductal papilloma with ductal carcinoma in situ. †
- Invasive papillary carcinoma of the breast.
† Size criteria are different in papillomas.
Images:
Lymphocytic mastitis
General
- If the individual has diabetes mellitus (DM) it is called diabetic mastopathy.[61]
- Rare.
Microscopic
Features:[62]
- Lymphocytic infiltrates - key feature:
- Lobules.
- Perivascular.
- Enlarged stromal fibroblasts.
- Stromal collagen with keloid-like changes.
DDx:
- Diabetic mastopathy - if individual has diabetes.
- Primary lymphoma of the breast.
Images:
- Lymphocytic mastitis - low mag. (webpathology.com).
- Lymphocytic mastitis - high mag. (webpathology.com).
IHC
- B cell predominant (CD20 > CD3).[61]
- B cells CD43 -ve.
Molecular
- Negative clonality studies.
Microglandular adenosis
- Not to be confused with microglandular hyperplasia.
- Abbreviated MGA.
General
- Controversial thingy.
Management:
- Excision.
Microscopic
Features:[63]
- Round glands lined by a single layer of cells.
- May extend into fat.
- Lack of desmoplastic stroma.
DDx:
- Tubular carcinoma - has apical snouts, desmoplasia among other things; see page by Collins.[63]
- Sclerosing adenosis.
Images:
- Microglandular adenosis (surgical pathologyatlas.com).
- MGA - low mag. (webpathology.com).
- MGA - high mag. (webpathology.com).
- MGA (breastpathology.info).
- MGA - several images (breastpathology.info).
IHC
Features:[64]
- S100 +ve.
- 34BE12 +ve -- focal!
Others:
- EMA -ve.
- Tubular carcinoma usu. +ve.
- GCDFP-15 -ve.[65]
- Ki-67 <3%.
Adenomyoepithelioma
General
- Rare lesion consisting of epithelial and myoepithelial elements.
- May occur in other sites, e.g. tonsil.[66]
- May be benign or malignant.[67][68]
Note:
- Possibly the same tumour as epithelial-myoepithelial carcinoma of the salivary gland.[69]
Microscopic
Features:[70]
- Well-circumscribed.
- Glandular architecture with:
- Easily identifiable myoepithelial cells - with clear cytoplasm - key feature.
- Eosinophilic cuboidal epithelial cells.
- Eosinophilic basement membrane material between glands.
DDx:
- Invasive ductal carcinoma of the breast (on core biopsy).
- Mammary pleomorphic adenoma.
- Ductal adenoma.
- Tubular adenoma of the breast - does not have a prominent (clear) myoepithelial component.
- Sclerosing adenosis.[16]
Images:
- Webpathology.com:
- WC:
Mammary myofibroblastoma
General
Note:
- In extra-mammary sites the tumour is known as a mammary-type myofibroblastoma may immunohistochemically and histomorphologically overlap with spindle cell lipoma.[73]
Microscopic
Features:[74]
- Well-circumscribed lesion.
- Spindle cells without nuclear atypia arranged in fascicles.
- Interspersed thick bundles of collagen.
Notes:
- No calcifications.
- No necrosis.
- No hemorrhage.
DDx:
- Metaplastic breast carcinoma.
- Fibromatosis.
- Leiomyoma of the breast.
- Nodular fasciitis.
- Phyllodes tumour.
Images:
- WC:
- www:
IHC
Features:[72]
Other
- S100 -ve.
- Beta-catenin -ve. (???)
Squamous metaplasia of lactiferous ducts
- Abbreviated SMOLD.
General
- Uncommon.[75]
- Associated with smoking.[75]
- Post-menopausal women.
- May be associated with subareolar abscess.
Gross
- +/-Nipple inversion.[76]
Microscopic
Features:
- Squamous epithelium - replaces (bilayered) lactiferous ducts - key feature.[76]
- Xanthomatous reaction.
Images:
Granular cell tumour of the breast
General
- Uncommon.
Gross
- May be a spiculated mass and thus mimic malignancy radiologically.[77]
Microscopic
- See granular cell tumour.
See also
References
- ↑ URL: http://breastcancer.about.com/od/diagnosis/a/birads.htm. Accessed on: 16 March 2011.
- ↑ MUA. 1 October 2010.
- ↑ MUA. 1 October 2010.
- ↑ RS. 4 May 2010.
- ↑ URL: [Breast_pathology#Lactational_changes Breast_pathology#Lactational_changes. Accessed on: 3 October 2011.
- ↑ Tavassoli, FA.; Yeh, IT. (Jan 1987). "Lactational and clear cell changes of the breast in nonlactating, nonpregnant women.". Am J Clin Pathol 87 (1): 23-9. PMID 2879437.
- ↑ URL: http://flylib.com/books/en/2.953.1.9/1/. Accessed on: 6 August 2011.
- ↑ Mulligan AM, O'Malley FP (March 2007). "Papillary lesions of the breast: a review". Adv Anat Pathol 14 (2): 108–19. doi:10.1097/PAP.0b013e318032508d. PMID 17471117.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 159-160. ISBN 978-0443066801.
- ↑ 10.0 10.1 URL: http://www.hsc.stonybrook.edu/breast-atlas/XIII-03.htm. Accessed on: 16 November 2011.
- ↑ URL: http://radiology.uchc.edu/eAtlas/Breast/1693.htm. Accessed on: 16 November 2011.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 542. ISBN 978-1416054542.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 159-160. ISBN 978-0443066801.
- ↑ URL: http://dictionary.reference.com/browse/sclerosis. Accessed on: 16 March 2011.
- ↑ URL: http://www.breastcancercare.org.uk/breast-cancer-information/breast-awareness/benign-breast-conditions/sclerosing-lesions. Accessed on: 30 April 2012.
- ↑ 16.0 16.1 Chu et al. (2006). Adenomyoepithelioma of the Breast — A Case Report. Tzu Chi Med J. Vol. 18 No. 1. URL:URL: http://www.tzuchi.com.tw/file/tcmj/95-1/2-8.pdf. Accessed on: 28 April 2012.
- ↑ Lerwill, MF. (Apr 2008). "Flat epithelial atypia of the breast.". Arch Pathol Lab Med 132 (4): 615-21. doi:10.1043/1543-2165(2008)132[615:FEAOTB]2.0.CO;2. PMID 18384213.
- ↑ Schnitt, SJ. (2003). "The diagnosis and management of pre-invasive breast disease: flat epithelial atypia--classification, pathologic features and clinical significance.". Breast Cancer Res 5 (5): 263-8. doi:10.1186/bcr625. PMID 12927037.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1072. ISBN 978-1416031215.
- ↑ Ung OA, Lee WB, Greenberg ML, Bilous M (January 2001). "Complex sclerosing lesion: the lesion is complex, the management is straightforward". ANZ J Surg 71 (1): 35–40. PMID 11167596.
- ↑ URL: http://www.cancer.org/docroot/NWS/content/NWS_1_1x_Radial_Scars.asp. Accessed on: 4 May 2010.
- ↑ 22.0 22.1 Kennedy M, Masterson AV, Kerin M, Flanagan F (October 2003). "Pathology and clinical relevance of radial scars: a review". J. Clin. Pathol. 56 (10): 721–4. PMC 1770086. PMID 14514771. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770086/.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 91. ISBN 978-0443066801.
- ↑ RS. May 2010.
- ↑ Guinebretière, JM.; Menet, E.; Tardivon, A.; Cherel, P.; Vanel, D. (Apr 2005). "Normal and pathological breast, the histological basis.". Eur J Radiol 54 (1): 6-14. doi:10.1016/j.ejrad.2004.11.020. PMID 15797289.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 550. ISBN 978-1416054542.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 110. ISBN 978-0443066801.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970216-9. Accessed on: 16 March 2011.
- ↑ Sabate, JM.; Clotet, M.; Torrubia, S.; Gomez, A.; Guerrero, R.; de las Heras, P.; Lerma, E. (Oct 2007). "Radiologic evaluation of breast disorders related to pregnancy and lactation.". Radiographics 27 Suppl 1: S101-24. doi:10.1148/rg.27si075505. PMID 18180221.
- ↑ URL: http://www.imagingpathways.health.wa.gov.au/includes/dipmenu/image/image.html. Accessed on: 15 February 2012.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 262. ISBN 978-0781765275.
- ↑ 32.0 32.1 32.2 O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 116. ISBN 978-0443066801.
- ↑ URL: http://www.breastpathology.info/fibro_variants.html#juvenile. Accessed on: 3 October 2011.
- ↑ URL: http://www.breastpathology.info/fibro_variants.html#complex. Accessed on: 3 October 2011.
- ↑ Maiorano, E.; Albrizio, M. (Dec 1995). "Tubular adenoma of the breast: an immunohistochemical study of ten cases.". Pathol Res Pract 191 (12): 1222-30. PMID 8927570.
- ↑ Guerrero MA, Ballard BR, Grau AM (July 2003). "Malignant phyllodes tumor of the breast: review of the literature and case report of stromal overgrowth". Surg Oncol 12 (1): 27–37. PMID 12689668. http://linkinghub.elsevier.com/retrieve/pii/S0960740403000057.
- ↑ Bannowsky, A.; Probst, A.; Dunker, H.; Loch, T. (2009). "Rare and challenging tumor entity: phyllodes tumor of the prostate.". J Oncol 2009: 241270. doi:10.1155/2009/241270. PMID 20069045.
- ↑ McCluggage, WG. (Mar 2010). "Mullerian adenosarcoma of the female genital tract.". Adv Anat Pathol 17 (2): 122-9. doi:10.1097/PAP.0b013e3181cfe732. PMID 20179434.
- ↑ URL: http://www.breastpathologyconsults.com/blog/wp-content/uploads/2011/03/FEL_poster.pdf. Accessed on: 23 February 2012.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 263. ISBN 978-0781765275.
- ↑ Taira N, Takabatake D, Aogi K, et al (October 2007). "Phyllodes tumor of the breast: stromal overgrowth and histological classification are useful prognosis-predictive factors for local recurrence in patients with a positive surgical margin". Jpn. J. Clin. Oncol. 37 (10): 730-6. doi:10.1093/jjco/hym099. PMID 17932112. http://jjco.oxfordjournals.org/cgi/reprint/37/10/730.
- ↑ Leon, ME.; Leon, MA.; Ahuja, J.; Garcia, FU.. "Nodular myofibroblastic stromal hyperplasia of the mammary gland as an accurate name for pseudoangiomatous stromal hyperplasia of the mammary gland.". Breast J 8 (5): 290-3. PMID 12199757.
- ↑ 43.0 43.1 43.2 Powell CM, Cranor ML, Rosen PP (March 1995). "Pseudoangiomatous stromal hyperplasia (PASH). A mammary stromal tumor with myofibroblastic differentiation". Am. J. Surg. Pathol. 19 (3): 270–7. PMID 7872425.
- ↑ Vuitch MF, Rosen PP, Erlandson RA (February 1986). "Pseudoangiomatous hyperplasia of mammary stroma". Hum. Pathol. 17 (2): 185–91. PMID 3949338.
- ↑ 45.0 45.1 Ferreira, M.; Albarracin, CT.; Resetkova, E. (Feb 2008). "Pseudoangiomatous stromal hyperplasia tumor: a clinical, radiologic and pathologic study of 26 cases.". Mod Pathol 21 (2): 201-7. doi:10.1038/modpathol.3801003. PMID 18084246.
- ↑ 46.0 46.1 Baker, M.; Chen, H.; Latchaw, L.; Memoli, V.; Ornvold, K. (Aug 2011). "Pseudoangiomatous stromal hyperplasia of the breast in a 10-year-old girl.". J Pediatr Surg 46 (8): e27-31. doi:10.1016/j.jpedsurg.2011.04.063. PMID 21843705.
- ↑ URL: http://surgpathcriteria.stanford.edu/breast/pash/printable.html. Accessed on: 28 April 2012.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 117. ISBN 978-0443066801.
- ↑ 49.0 49.1 URL: http://surgpathcriteria.stanford.edu/breast/mammhamart/. Accessed on: 4 October 2011.
- ↑ Tse, GM.; Law, BK.; Ma, TK.; Chan, AB.; Pang, LM.; Chu, WC.; Cheung, HS. (Dec 2002). "Hamartoma of the breast: a clinicopathological review.". J Clin Pathol 55 (12): 951-4. PMC 1769817. PMID 12461066. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1769817/.
- ↑ 51.0 51.1 URL: http://surgpathcriteria.stanford.edu/breast/collspher/. Accessed on: 4 September 2011.
- ↑ 52.0 52.1 Resetkova, E.; Albarracin, C.; Sneige, N. (Jan 2006). "Collagenous spherulosis of breast: morphologic study of 59 cases and review of the literature.". Am J Surg Pathol 30 (1): 20-7. PMID 16330938.
- ↑ URL: http://www.hsc.stonybrook.edu/breast-atlas/V-33.htm. Accessed on: 31 August 2011.
- ↑ 54.0 54.1 Boutayeb, S.; Benomar, S.; Sbitti, Y.; Harroudi, T.; Hassam, B.; Errihani, H. (2012). "Nipple adenoma in a man: An unusual case report.". Int J Surg Case Rep 3 (5): 190-2. doi:10.1016/j.ijscr.2011.05.008. PMID 22342578.
- ↑ HANDLEY, RS.; THACKRAY, AC. (Jun 1962). "Adenoma of nipple.". Br J Cancer 16: 187-94. PMC 2070922. PMID 13904317. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2070922/?tool=pubmed.
- ↑ 56.0 56.1 56.2 "Adenoma of Nipple.". Br Med J 1 (5330): 563. Mar 1963. PMC 2123505. PMID 20789667. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2123505/?page=1.
- ↑ URL: http://surgpathcriteria.stanford.edu/breast/nippleadenoma/printable.html. Accessed on: 6 August 2011.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 307 Q16. ISBN 978-1416025887.
- ↑ Zervoudis, S.; Iatrakis, G.; Economides, P.; Polyzos, D.; Navrozoglou, I. (Jan 2010). "Nipple discharge screening.". Womens Health (Lond Engl) 6 (1): 135-51. doi:10.2217/whe.09.81. PMID 20050819.
- ↑ URL: http://surgpathcriteria.stanford.edu/breast/nippleadenoma/printable.html. Accessed on: 6 August 2011.
- ↑ 61.0 61.1 Valdez, R.; Thorson, J.; Finn, WG.; Schnitzer, B.; Kleer, CG. (Mar 2003). "Lymphocytic mastitis and diabetic mastopathy: a molecular, immunophenotypic, and clinicopathologic evaluation of 11 cases.". Mod Pathol 16 (3): 223-8. doi:10.1097/01.MP.0000056627.21128.74. PMID 12640102.
- ↑ URL: http://www.breastpathology.info/Case_of_the_month/2007/COTM_0707%20discussion.html. Accessed on: 28 November 2010.
- ↑ 63.0 63.1 URL: http://www.uscap.org/site~/iap2006/slides08-4v.htm. Accessed on: 18 May 2011.
- ↑ Joshi, MG.; Lee, AK.; Pedersen, CA.; Schnitt, S.; Camus, MG.; Hughes, KS. (Jan 1996). "The role of immunocytochemical markers in the differential diagnosis of proliferative and neoplastic lesions of the breast.". Mod Pathol 9 (1): 57-62. PMID 8821958.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 296 Q20. ISBN 978-1416025887.
- ↑ Ren, J.; Song, L.; Dang, Q.; Zhang, X.; Jiang, SW.; Zhang, G.; Wang, N.; Liu, Z. et al. (2010). "Primary adenomyoepithelioma of tonsil.". Head Neck Oncol 2: 7. doi:10.1186/1758-3284-2-7. PMID 20356364.
- ↑ Howlett, DC.; Mason, CH.; Biswas, S.; Sangle, PD.; Rubin, G.; Allan, SM. (Mar 2003). "Adenomyoepithelioma of the breast: spectrum of disease with associated imaging and pathology.". AJR Am J Roentgenol 180 (3): 799-803. PMID 12591699. http://www.ajronline.org/content/180/3/799.full.
- ↑ Zizi-Sermpetzoglou, A.; Vasilakaki, T.; Grammatoglou, X.; Petrakopoulou, N.; Nikolaidou, ME.; Glava, C. (2009). "Malignant adenomyoepithelioma of the breast--case report.". Eur J Gynaecol Oncol 30 (2): 234-6. PMID 19480267.
- ↑ Seifert, G. (Sep 1998). "Are adenomyoepithelioma of the breast and epithelial-myoepithelial carcinoma of the salivary glands identical tumours?". Virchows Arch 433 (3): 285-8. PMID 9769134.
- ↑ URL: http://www.webpathology.com/image.asp?n=1&Case=322. Accessed on: 16 August 2011.
- ↑ Qureshi, A.; Kayani, N.. "Myofibroblastoma of breast.". Indian J Pathol Microbiol 51 (3): 395-6. PMID 18723968.
- ↑ 72.0 72.1 Mele, M.; Jensen, V.; Wronecki, A.; Lelkaitis, G. (2011). "Myofibroblastoma of the breast: Case report and literature review.". Int J Surg Case Rep 2 (6): 93-6. doi:10.1016/j.ijscr.2011.02.006. PMC 3199680. PMID 22096693. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199680/. Cite error: Invalid
<ref>tag; name "pmid22096693" defined multiple times with different content - ↑ 73.0 73.1 73.2 McMenamin, ME.; Fletcher, CD. (Aug 2001). "Mammary-type myofibroblastoma of soft tissue: a tumor closely related to spindle cell lipoma.". Am J Surg Pathol 25 (8): 1022-9. PMID 11474286.
- ↑ O'Malley, Frances P.; Pinder, Sarah E. (2006). Breast Pathology: A Volume in Foundations in Diagnostic Pathology series (1st ed.). Churchill Livingstone. pp. 131. ISBN 978-0443066801.
- ↑ 75.0 75.1 Lo, G.; Dessauvagie, B.; Sterrett, G.; Bourke, AG. (Nov 2012). "Squamous metaplasia of lactiferous ducts (SMOLD).". Clin Radiol 67 (11): e42-6. doi:10.1016/j.crad.2012.07.011. PMID 22964367.
- ↑ 76.0 76.1 Powell, BC.; Maull, KI.; Sachatello, CR. (Aug 1977). "Recurrent subareolar abscess of the breast and squamous metaplasia of the lactiferous ducts: a clinical syndrome.". South Med J 70 (8): 935-7. PMID 887978.
- ↑ Yang, WT.; Edeiken-Monroe, B.; Sneige, N.; Fornage, BD. (May 2006). "Sonographic and mammographic appearances of granular cell tumors of the breast with pathological correlation.". J Clin Ultrasound 34 (4): 153-60. doi:10.1002/jcu.20227. PMID 16615051.