Difference between revisions of "Placenta"
(→Infection: wikify) |
|||
| (339 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
The '''placenta''' feeds the developing baby, breathes for it and disposes of its waste. | [[Image:Human_placenta.jpg|thumb|right|A placenta (fetal aspect) with attached umbilical cord. (WC/Asturnut)]] | ||
The '''placenta''' feeds the developing baby, breathes for it and disposes of its waste. | |||
==Normal== | The organ is one that seems to be left behind; at least one review suggests it isn't done so well by general pathologists.<ref name=pmid12033960>{{Cite journal | last1 = Sun | first1 = CC. | last2 = Revell | first2 = VO. | last3 = Belli | first3 = AJ. | last4 = Viscardi | first4 = RM. | title = Discrepancy in pathologic diagnosis of placental lesions. | journal = Arch Pathol Lab Med | volume = 126 | issue = 6 | pages = 706-9 | month = Jun | year = 2002 | doi = 10.1043/0003-9985(2002)1260706:DIPDOP2.0.CO;2 | PMID = 12033960 }}</ref> | ||
Amnion - | |||
*Characterized by a single layer of cells.<ref> | ''Placental pathology'' redirects to this article. | ||
=Clinical= | |||
==Examination of the placenta== | |||
*Most placentas are ''not'' examined by a pathologist. | |||
===Indications for exam by pathology=== | |||
Some indications for exam by a pathologist: | |||
*Abnormalities in the: | |||
*#Fetus: | |||
*#*Bad fetal outcome. | |||
*#*Suspected or known congenital abnormalities ''or'' chromosomal abnormalities. | |||
*#*[[IUGR]]. | |||
*#Mother: | |||
*#*Infection/suspected infection. | |||
*#*Pre-term labour. | |||
*#*Maternal disease (e.g. [[SLE]], coagulopathy). | |||
*#*Complicated pregnancy (preclampsia, pregnancy induced hypertension, gestational diabetes). | |||
*#Placenta: | |||
*#*Unusual gross characteristics.<ref name=pmid9518951>{{cite journal |author=Yetter JF |title=Examination of the placenta |journal=Am Fam Physician |volume=57 |issue=5 |pages=1045–54 |year=1998 |month=March |pmid=9518951 |doi= |url=}}</ref> | |||
A more detailed list is given by Hargitai et al.<ref name=pmid15280396>{{cite journal |author=Hargitai B, Marton T, Cox PM |title=Best practice no 178. Examination of the human placenta |journal=J. Clin. Pathol. |volume=57 |issue=8 |pages=785–92 |year=2004 |month=August |pmid=15280396 |pmc=1770400 |doi=10.1136/jcp.2003.014217 |url=}}</ref> and Chang.<ref>URL: [http://smj.sma.org.sg/5012/5012ra1.pdf http://smj.sma.org.sg/5012/5012ra1.pdf]. Accessed on: 11 February 2011.</ref> | |||
====Most common==== | |||
Most common reasons for submitting a placenta to pathology:<ref>Sherman C. 8 February 2011.</ref> | |||
# Prematurity. | |||
# PROM / possible [[chorioamnionitis]]. | |||
# Multiple gestation. | |||
==Bleeding in late pregnancy== | |||
DDx of bleeding in late pregnancy: | |||
*[[Placental abruption]] (most common). | |||
*Placenta previa. | |||
*Vasa previa (fetus losing blood). | |||
==Clinical screening tests== | |||
{{main|Pregnancy}} | |||
*PAPP-A - low values seen in aneuploidy.<ref>URL: [http://www.ncbi.nlm.nih.gov/sites/entrez?Db=gene&Cmd=ShowDetailView&TermToSearch=5069 http://www.ncbi.nlm.nih.gov/sites/entrez?Db=gene&Cmd=ShowDetailView&TermToSearch=5069]. Accessed on: 7 July 2010.</ref> | |||
==Abbreviations== | |||
*C/S = Caesarean section. | |||
*LSCS = lower segment C-section. | |||
*FTP = failure to progress. | |||
*PROM = premature rupture of membranes. | |||
*PPROM = preterm premature ruptures of membranes. | |||
*IUGR = [[intrauterine growth restriction]]. | |||
*IOL = induction of labour. | |||
=Normal histology= | |||
==Villi== | |||
{{Main|Chorionic villi}} | |||
This is dealt with in a separate article that also covers the types of trophoblast ([[cytotrophoblast]], [[syncytiotrophoblast]], intermediate trophoblast). | |||
==Cord== | |||
===Omphalomesenteric duct remnant=== | |||
*[[AKA]] vitelline duct. | |||
*Benign embryologic remnant. | |||
Features: | |||
*Duct with benign looking cuboidal epithelium. | |||
===Allantoic duct remnant=== | |||
*Benign embryologic remnant. | |||
Features: | |||
*Duct with benign looking flat epithelium. | |||
===Vitelline artery remnant=== | |||
Features: | |||
*Small artery in the cord. | |||
==Membranes== | |||
Fetus to mother: | |||
*Amnion - thin layer: one cell layer, basement membrane, connective tissue. | |||
*Cleft - artifactual - empty space. | |||
*Chorion - vascular. | |||
*Decidua (maternal tissue) - may contain obsolete chorionic villi; place to look for hypertensive changes. | |||
===Amnion=== | |||
General: | |||
*Next to fetus, surrounds amniotic fluid, avascular. | |||
Characteristics: | |||
*Characterized by a single layer of cells.<ref name=Ref_H4P2_974>{{Ref H4P2|974}}</ref> | |||
**Cuboidal/squamoid shape. | **Cuboidal/squamoid shape. | ||
**Eosinophilic cytoplasm. | **Eosinophilic cytoplasm. | ||
| Line 9: | Line 93: | ||
*Squamous metaplasia may be seen at cord insertion. | *Squamous metaplasia may be seen at cord insertion. | ||
*Basement membrane. | *Basement membrane. | ||
*'Compact layer'.<ref> | *'Compact layer'.<ref name=Ref_H4P2_974>{{Ref H4P2|974}}</ref> | ||
*'Fibroblastic layer'.<ref> | *'Fibroblastic layer'.<ref name=Ref_H4P2_974>{{Ref H4P2|974}}</ref> | ||
Chorion | ===Chorion=== | ||
*Layers:<ref> | General: | ||
*Surrounds amnion. | |||
Characteristics: | |||
*Layers:<ref name=Ref_H4P2_977>{{Ref H4P2|977}}</ref> | |||
**'Reticular layer' - cellular (inner aspect). | **'Reticular layer' - cellular (inner aspect). | ||
**'Pseudo-basemement membrane'. | **'Pseudo-basemement membrane'. | ||
**'Outer trophoblastic layer'. | **'Outer trophoblastic layer'. | ||
*Has blood vessels. | *Has blood vessels. | ||
*Opposed to "trophoblastic X cells" on side opposite of amnion.<ref> | *Opposed to "trophoblastic X cells" on side opposite of amnion.<ref name=Ref_H4P2_974>{{Ref H4P2|974}}</ref> | ||
**Beneath of the "trophoblastic X cells" is ''decidua'' (mnemonic ''NEW'' = nucleus central, eosinophilic, well-defined cell border), which is maternal tissue. | **Beneath of the "trophoblastic X cells" is ''decidua'' (mnemonic ''NEW'' = nucleus central, eosinophilic, well-defined cell border), which is maternal tissue. | ||
Note: | |||
*Fibrin deposition may be found deep to the chorion - known as ''subchorionic fibrin deposition''. | |||
**Gross: subchorionic, white/yellow, laminated, classically has a triangular-shape with the base of triangle parallel to fetal aspect of disc. | |||
***Arises due to localized stasis of the inter-villous maternal blood. | |||
**Focal small deposits are considered to be a normal finding - seen in ~15% of cases.<ref name=pmid21393870>{{Cite journal | last1 = Narasimha | first1 = A. | last2 = Vasudeva | first2 = DS. | title = Spectrum of changes in placenta in toxemia of pregnancy. | journal = Indian J Pathol Microbiol | volume = 54 | issue = 1 | pages = 15-20 | month = | year = | doi = 10.4103/0377-4929.77317 | PMID = 21393870 |URL = http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2011;volume=54;issue=1;spage=15;epage=20;aulast=Narasimha }}</ref><ref>URL: [http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf]. Accessed on: 17 August 2012.</ref> | |||
***The pathologic counterpart of this is ''[[perivillous fibrin deposition]]''. | |||
Image: | |||
*[http://www.ijpmonline.org/viewimage.asp?img=IndianJPatholMicrobiol_2011_54_1_15_77317_u5.jpg Subchorionic fibrin deposition (ijpmonline.org)]. | |||
== | ==Common terms== | ||
*Chorionic plate - fetal aspect of placenta. | *Chorionic plate - fetal aspect of placenta. | ||
*Basal plate - maternal aspect of placenta. | *Basal plate - maternal aspect of placenta. | ||
| Line 27: | Line 125: | ||
**Place to look for maternal vessels. | **Place to look for maternal vessels. | ||
== | =Grossing= | ||
This is often very quick. The gross is quite important, as some things cannot be diagnosed microscopically. | |||
==General== | |||
*Dimensions: | *Dimensions: | ||
**Disc. | **Disc. | ||
**Length of cord, diameter of cord. | **Length of cord, diameter of cord. | ||
*Mass (weight) | **Accessory lobes - dimensions. | ||
***Two lobes of equal size + cord arises in between = bilobate placenta. | |||
*Mass (weight). | |||
**Should be done 'trimmed' (cord cut-off, membrane cut-off). | |||
**Should be done when placenta is "fresh", i.e. not fixed -- as mass tables are based on fresh state. | |||
*Umbilical cord | *Umbilical cord | ||
**Attachment. | **Attachment. | ||
| Line 38: | Line 142: | ||
***Membranous or velamentous (veil-like) insertion. | ***Membranous or velamentous (veil-like) insertion. | ||
****Vessels separate/branch prior to reaching placental disc. | ****Vessels separate/branch prior to reaching placental disc. | ||
***Furcate insertion - | ***Furcate insertion - blood vessels separate before reaching placenta disc/not surrounded by Wharton's jelly - vessels more exposed to trauma (risk for vasa previa). | ||
**Knots (false vs. true). | **Knots (false vs. true). | ||
***False knots are nothing to worry about -- look like a knot but aren't really one. | ***False knots are nothing to worry about -- look like a knot but aren't really one. | ||
**Twisting/coiling. | **Twisting/coiling - 1-3 coils/10 cm is normal. | ||
**Number of vessels. | **Number of vessels. | ||
***Normal: 2 arteries, 1 vein. | ***Normal: 2 arteries, 1 vein. | ||
*Membranes - shiny, | *Membranes - shiny & translucent - normal (green, opaque/dull - chorioamnionitis). | ||
**Attachment: marginal (normal), circummarginate (inside edge), | **Attachment (insertion): marginal (normal), circummarginate (inside edge), [[circumvallate placenta|circumvallate]] (folding on self). | ||
**Site of rupture - if obvious; low point of rupture suggests low-lying placenta. | |||
*Placental disc. | *Placental disc. | ||
**Fetal surface - normal is shinny | **Fetal surface - normal is shinny. | ||
**Maternal surface | ***Dull in chorioamnionitis. | ||
**Maternal surface | |||
***Are the cotyledons intact? | |||
***Adherent clot? | |||
**Parenchyma - after sectioning: | |||
***White vs. red nodules. | |||
Notes: | |||
*Parenchymal nodules - a brief DDx: | |||
**White: [[placental infarct|infarct]] (chronic), thrombi, [[chorangioma]], [[perivillous fibrin deposition]]. | |||
**Red: infarct (acute), thrombi. | |||
==Sections== | |||
#Cord two sections. | |||
#Membranes (rolled), two rolls or more.<ref name=pmid19061291>{{cite journal |author=Winters R, Waters BL |title=What is adequate sampling of extraplacental membranes?: a randomized, prospective analysis |journal=Arch. Pathol. Lab. Med. |volume=132 |issue=12 |pages=1920–3 |year=2008 |month=December |pmid=19061291 |doi= |url=}}</ref> | |||
#Cord at insertion + disc. | |||
#Placenta - full thickness (maternal and fetal surface). | |||
#*Sections should not be taken at the margin of the disc. | |||
==Placental membranes== | |||
Appearance:<ref>Lester | Appearance:<ref name=Ref_Lester461>{{Ref Lester|461}}</ref> | ||
*Normal - shiny. | *Normal - shiny. | ||
* | *[[Chorioamnionitis]] - opaque/dull. | ||
*Meconium - green. | *Meconium - green. | ||
*Amnion nodosum. | *[[Amnion nodosum]] - yellow patches. | ||
** | **Some describe 'em as white.<ref>CS. 7 February 2011.</ref> | ||
** | |||
** | ==Placental mass== | ||
It is considered routine to obtain a mass for the placenta. This is usually done when the placenta is fresh and with the membranes and cord trimmed, as most tables of placental mass were created with these parameters. | |||
Placental mass by gestational age:<ref>AFIP Placental pathol. ISBN: 1-881041-89-1. P.312</ref> | |||
{| class="wikitable" | |||
|Gest. Age/Percentile ||'''25%''' ||'''50%''' ||'''75%''' | |||
|- | |||
|'''32 weeks''' ||275 g ||318 g ||377 g | |||
|- | |||
|'''36 weeks''' ||369 g ||440 g ||508 g | |||
|- | |||
|'''40 weeks''' ||440 g ||501 g ||572 g | |||
|- | |||
|} | |||
===Linear regression - placental mass-gestational age=== | |||
Based on the table in the AFIP book<ref>AFIP Placental pathol. ISBN: 1-881041-89-1. P.312</ref> one can generate the following regression lines: | |||
{| class="wikitable" | |||
| ||'''50%''' ||'''10%''' ||'''90%''' | |||
|- | |||
|slope (g/week) ||21.58088235 ||19.70588235 ||25.40196078 | |||
|- | |||
|y-intercept (g) ||-357.4558824 ||-397.2352941 ||-366.7254902 | |||
|- | |||
|Pearson (r) ||0.988670724 ||0.988268672 ||0.982206408 | |||
|- | |||
|} | |||
placental mass = slope x gestational age + intercept | |||
===What to remember...=== | |||
Extrapolated from the linear regression (see above): | |||
*50% at term = 500 grams. | |||
*50% at 26 weeks = 200 grams. | |||
*The change in mass/week is approximately linear and equal to 300 grams / 14 weeks ~ 20 grams/week. | |||
*The spread in mass between 10% and 90%, crudely estimated, is 200 grams (for GA=26-40). | |||
Notes: | |||
*Is it required? | |||
**Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.<ref>{{cite book |author= Fox, Harold; Sebire, Neil J. |title=[http://www.amazon.com/Pathology-Placenta-Major-Problems/dp/1416025928/ref=sr_1_fkmr0_1?ie=UTF8&qid=1297259619&sr=1-1-fkmr0 Pathology of the Placenta (Major Problems in Pathology)]|publisher=Saunders |location= |year=2007 |pages= 559-561 |edition=3rd |isbn=978-1416025924 |oclc= |doi= |accessdate=}}</ref> | |||
***In the context of quality, a measure (even if somewhat flawed) is probably more reproducible and objective than arbitrary descriptors which require experience and a continuing case volume to calibrate. | |||
===Placentomegaly=== | |||
*[[AKA]] ''large placenta''. | |||
Associations:<ref>URL: [http://quizlet.com/5793113/ob-flash-cards/ http://quizlet.com/5793113/ob-flash-cards/]. Accessed on: 13 January 2012.</ref> | |||
*Maternal [[diabetes]] - esp. poorly controlled.<ref name=pmid2771897>{{Cite journal | last1 = Clarson | first1 = C. | last2 = Tevaarwerk | first2 = GJ. | last3 = Harding | first3 = PG. | last4 = Chance | first4 = GW. | last5 = Haust | first5 = MD. | title = Placental weight in diabetic pregnancies. | journal = Placenta | volume = 10 | issue = 3 | pages = 275-81 | month = | year = | doi = | PMID = 2771897 }}</ref> | |||
*Maternal [[anemia]]/low maternal iron stores.<ref>{{Cite journal | last1 = Hindmarsh | first1 = PC. | last2 = Geary | first2 = MP. | last3 = Rodeck | first3 = CH. | last4 = Jackson | first4 = MR. | last5 = Kingdom | first5 = JC. | title = Effect of early maternal iron stores on placental weight and structure. | journal = Lancet | volume = 356 | issue = 9231 | pages = 719-23 | month = Aug | year = 2000 | doi = | PMID = 11085691 }}</ref> | |||
*Fetal malformations. | |||
*Neoplasms of the placenta, e.g. [[chorangioma]]. | |||
*Twin-twin transfusion syndrome. | |||
*Chronic intrauterine infections, e.g. [[syphilis]], [[toxoplasmosis]], [[cytomegalovirus]]. | |||
Lame causes of a heavy placenta: | |||
*Dates wrong - error in determining the estimated date of confinement. | |||
*Adherent blood clot. | |||
Comment: | |||
*Most of causes seem to have one thing in common: | |||
**There is a decreased oxygen delivery to the fetus. | |||
====Sign out==== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: | |||
- LARGE PLACENTA (819 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). | |||
- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI. | |||
</pre> | |||
===Placental growth restriction=== | |||
*[[AKA]] ''placenta small for gestational age''. | |||
*''Small placenta'' redirects here. | |||
Associations: | |||
*Maternal vascular disease, e.g. [[hypertrophic decidual vasculopathy|hypertension]]. | |||
*Fetal malformations. | |||
====Sign out==== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: | |||
- PLACENTA SMALL FOR GESTATIONAL AGE (160 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). | |||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITH: | |||
-- OLD CENTRAL TRANSMURAL INFARCT (1.7 CM MAXIMAL DIMENSION). | |||
COMMENT: | |||
The 10th percentile placental mass (pre-fixation) for 34 weeks and 2 days is approximately 390 grams. | |||
</pre> | |||
=Overview of placental pathology= | |||
==Approach== | |||
The pathology of the placenta is diverse and is not easy to group. | |||
==Sign | It terms of remembering things. It is probably easiest to take a combined anatomical, etiologic and morphologic approach. | ||
Anatomical basis: | |||
*Cord. | |||
*Membranes. | |||
*Disc. | |||
Etiologic: | |||
*Congential. | |||
*Infectious. | |||
*Neoplastic. | |||
*Endocrine. | |||
*Trauma. | |||
*Vascular. | |||
*Degenerative. | |||
*Autoimmune. | |||
*Toxic. | |||
*Idiopathic. | |||
Compartmental: | |||
*Vasculature. | |||
*Membranes. | |||
*Parenchyma: | |||
**Maternal part (decidua). | |||
**Fetal part (villi, cord). | |||
==Common entities/diagnoses== | |||
*Normal. | |||
*[[Chorioamnionitis]]. | |||
*[[Placental abruption]]. | |||
*[[Meconium]]. | |||
*Hypertensive changes. | |||
=Sign out= | |||
What should be commented on... | What should be commented on... | ||
| Line 78: | Line 318: | ||
***Fetal. | ***Fetal. | ||
*Membranes. | *Membranes. | ||
**Membranitis? | **[[Membranitis]]? | ||
**Chorioamnionitis? | **[[Chorioamnionitis]]? | ||
*Cord: | *Cord: | ||
**3 vessel? | **3 vessel? | ||
| Line 86: | Line 326: | ||
Mnemonic: ''chorio, cord, vessels, villi (maturity, infarction)''. | Mnemonic: ''chorio, cord, vessels, villi (maturity, infarction)''. | ||
== | ==Normal placenta== | ||
<pre> | |||
* | PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: | ||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
</pre> | |||
===C-section=== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CAESAREAN SECTION: | |||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
</pre> | |||
=Cord pathology= | |||
*[[Two vessel cord]]. | |||
*Hypercoiling/Hypocoiling. | |||
*Abnormal insertion. | |||
*[[Cord knot]]s (true vs. false). | |||
*Strictures. | |||
*Hematoma. | |||
*[[Hemangioma]]. | |||
*Benign cyst. | |||
==Two vessel umbilical cord== | |||
*[[AKA]] ''two vessel cord''. | |||
*[[AKA]] ''single umbilical artery''. | |||
{{Main|Two vessel umbilical cord}} | |||
==Insertion== | |||
===Marginal insertion=== | |||
Definition: | |||
*The umbilical cord is attached to the placental disc at its margin. | |||
Prevalence: | |||
*Approximately 12% of placentas.<ref name=Ref_WMSP464>{{Ref WMSP|464}}</ref> | |||
Relevance: | |||
*None according to WMSP.<ref name=Ref_WMSP464>{{Ref WMSP|464}}</ref> | |||
**In theory, the cord, dependent on its relation to the internal os, is at greater risk of injury (leading to vasa previa) and compression (fetal hypoxia). A retrospective study found cord position in relation to the internal os is predictive for vasa previa.<ref name=pmid20872421>{{cite journal |author=Hasegawa J, Farina A, Nakamura M, ''et al.'' |title=Analysis of the ultrasonographic findings predictive of vasa previa |journal=Prenat. Diagn. |volume=30 |issue=12-13 |pages=1121–5 |year=2010 |month=December |pmid=20872421 |doi=10.1002/pd.2618 |url=}}</ref> | |||
===Velamentous insertion=== | |||
Definition: | |||
*The umbilical cord inserts into the fetal membranes.<ref name=Ref_WMSP464>{{Ref WMSP|464}}</ref> | |||
**The vessels are ''not'' protected by Wharton's jelly. | |||
***Wharton's jelly = the connective tissue surrounding the vessels in the cord. | |||
Details:<ref name=Ref_WMSP464>{{Ref WMSP|464}}</ref> | |||
*3/4 of the time the vessel also branch; in the remaining 1/4 the vessels stay together. | |||
Relevance: | |||
*Increased risk of vasa previa.<ref name=pmid20872421>{{cite journal |author=Hasegawa J, Farina A, Nakamura M, ''et al.'' |title=Analysis of the ultrasonographic findings predictive of vasa previa |journal=Prenat. Diagn. |volume=30 |issue=12-13 |pages=1121–5 |year=2010 |month=December |pmid=20872421 |doi=10.1002/pd.2618 |url=}}</ref> | |||
====Sign out==== | |||
<pre> | |||
PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: | |||
- THREE VESSEL UMBILICAL CORD WITH A VELAMENTOUS INSERTION, OTHERWISE WITHIN NORMAL LIMITS. | |||
- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS. | |||
</pre> | |||
==Umbilical knot== | |||
*[[AKA]] ''umbilical cord knot''. | |||
*[[AKA]] ''cord knot''. | |||
*[[AKA]] ''true knot''. | |||
===General=== | |||
*Prevalence ~1.25%.<ref name=pmid12012287>{{cite journal |author=Airas U, Heinonen S |title=Clinical significance of true umbilical knots: a population-based analysis |journal=Am J Perinatol |volume=19 |issue=3 |pages=127–32 |year=2002 |month=April |pmid=12012287 |doi=10.1055/s-2002-25311 |url=}}</ref><ref name=Ref_WMSP>{{Ref WMSP|464}}</ref> | |||
*Increase risk of [[stillbirth]]; odds ratio 3.93.<ref name=pmid12012287/> | |||
===Gross=== | |||
Work-up:<ref name=Ref_WMSP>{{Ref WMSP|464}}</ref> | |||
*Diameter measures and colour on both sides of the knot. | |||
*Knot should be untied to assess for deformation of Wharton's jelly. | |||
*Sections from both sides of the knot - to look for thrombi. | |||
Note: | |||
*False knots (large diameter - focally) are common - they cannot be untied. | |||
===Microscopic=== | |||
Features: | |||
*+/-[[thrombosis|Thrombi]]. | |||
**Fibrin deposition. | |||
*+/-Lines of Zahn. | |||
Images: | |||
*[http://library.med.utah.edu/WebPath/ATHHTML/ATH031.html Lines of Zahn (utah.edu)]. | |||
*[http://pathhsw5m54.ucsf.edu/case9/image94.html Lines of Zahn (ucsf.edu)]. | |||
==Coiling== | |||
*Hypo- and hypercoiling are both considered problematic.<ref name=Ref_WMSP464>{{Ref WMSP|464}}</ref> | |||
**Normal: 1-3 coils/10 cm.<ref>CS. 7 February 2011.</ref> | |||
*Associated with cord stricture, which is usu. at the fetal end of the cord.<ref name=Ref_WMSP465>{{Ref WMSP|465}}</ref> | |||
Notes: | |||
*There is little uniformity in how coiling is assessed in the medical literature - though 10% and 90% are considered the cut-points for normal.<ref name=pmid21080869>{{cite journal |author=Khong TY |title=Evidence-based pathology: umbilical cord coiling |journal=Pathology |volume=42 |issue=7 |pages=618–22 |year=2010 |month=December |pmid=21080869 |doi=10.3109/00313025.2010.520309 |url=}}</ref> | |||
**What are the 10% and 90% cut-points? They are not given in WMSP. UT access to a journal article<ref name=pmid16076615>PMID 16076615.</ref> that might have it is screwed-up. | |||
==Cord hematoma== | |||
Features:<ref name=Ref_WMSP465>{{Ref WMSP|465}}</ref> | |||
*Rare ~ 1/5500. | |||
*Mortality ~50% is severe. | |||
= | =Membranes= | ||
* | *Squamous metaplasia. | ||
*[[Chorioamnionitis]] - see ''infection'' section. | |||
* | |||
=== | ==Amnion nodosum== | ||
{{Main|Amnion nodosum}} | |||
== | ==Placental meconium== | ||
DDx of | {{Main|Placental meconium}} | ||
* | |||
* | ==Squamous metaplasia of the amnion== | ||
* | ===General=== | ||
*Benign common finding thought to be of no clinical significance.<ref name=Ref_WMSP463>{{Ref WMSP|463}}</ref> | |||
**One case report suggesting an association with [[chorioamnionitis]].<ref>{{Cite journal | last1 = Chew | first1 = RH. | last2 = Silberberg | first2 = BK. | title = Possible association of acute inflammatory exudate in chorioamnionitis and amniotic squamous metaplasia. | journal = Am J Clin Pathol | volume = 93 | issue = 4 | pages = 582-5 | month = Apr | year = 1990 | doi = | PMID = 2321592 }}</ref> | |||
*Needs to be separated from amnion nodosum - '''important'''.<ref>CS. 7 February 2011.</ref> | |||
===Gross=== | |||
Features:<ref name=pmid18081444>{{Cite journal | last1 = Adeniran | first1 = AJ. | last2 = Stanek | first2 = J. | title = Amnion nodosum revisited: clinicopathologic and placental correlations. | journal = Arch Pathol Lab Med | volume = 131 | issue = 12 | pages = 1829-33 | month = Dec | year = 2007 | doi = 10.1043/1543-2165(2007)131[1829:ANRCAP]2.0.CO;2 | PMID = 18081444 }}</ref> | |||
*White (or yellow) plaques - irregular outline. | |||
DDx: | |||
*[[Amnion nodosum]] - small (~1-5 mm), round, classically yellow. | |||
Images: | |||
*[http://www.archivesofpathology.org/action/showFullPopup?id=i1543-2165-131-12-1829-f01&doi=10.1043%2F1543-2165%282007%29131%5B1829%3AANRCAP%5D2.0.CO%3B2 Amnion nodosum & squamous metaplasia of the amnion (archivesofpathology.org)].<ref name=pmid18081444/> | |||
<!-- annoying use of '[' and ']' - had to go find escape characters here: http://www.w3schools.com/tags/ref_urlencode.asp --> | |||
===Microscopic=== | |||
Features:<ref name=pmid18081444/> | |||
*Dense, paucicellular (pink) compact keratin - '''key feature'''. | |||
Image: | |||
*[http://flylib.com/books/2/953/1/html/2/43%20-%20Placenta_files/DA10C43FF29.png Squmous metaplasia of the amnion (flylib.com)].<ref>URL: [http://flylib.com/books/en/2.953.1.49/1/ http://flylib.com/books/en/2.953.1.49/1/]. Accessed on: 10 January 2011.</ref> | |||
==Circumvallate placenta== | |||
*[[AKA]] ''circumvallate insertion of the membranes''. | |||
===General=== | |||
*May be associated with [[placental abruption]].<ref name=pmid18226129>{{Cite journal | last1 = Suzuki | first1 = S. | title = Clinical significance of pregnancies with circumvallate placenta. | journal = J Obstet Gynaecol Res | volume = 34 | issue = 1 | pages = 51-4 | month = Feb | year = 2008 | doi = 10.1111/j.1447-0756.2007.00682.x | PMID = 18226129 }}</ref> | |||
Note: | |||
*Membranes usually attach to the edge of the placenta. | |||
===Gross=== | |||
*Fetal membranes attach to the fetal surface of the placenta away from the margin of the placental disc. | |||
Classification: | |||
*Partial - not circumferential. | |||
*Complete. | |||
DDx: | |||
*[[Circummarginate placenta]]. | |||
Images: | |||
*[http://library.med.utah.edu/nmw/mod2/Tutorial2/pics/circumvallate.jpg Circumvallate placenta - partial and complete (utah.edu)]. | |||
*[http://library.med.utah.edu/WebPath/jpeg2/PLAC027.jpg Circumvallate placenta (utah.edu)]. | |||
=Twin placentas= | |||
{{Main|Twin placentas}} | |||
These are often submitted... even if they are normal. In these specimens, usually, the chorion is the key. | |||
It covers: | |||
*Monozygotic vs. dizygotic twins. | |||
*Twin-to-twin transfusion syndrome. | |||
=Placental disc= | |||
==Villous edema== | |||
===General=== | |||
*Non-specific finding. | |||
*Reported in associated with congenital adrenal hyperplasia for the stem villi.<ref name=pmid11045335>{{Cite journal | last1 = Furuhashi | first1 = M. | last2 = Oda | first2 = H. | last3 = Nakashima | first3 = T. | title = Hydrops of placental stem villi complicated with fetal congenital adrenal hyperplasia. | journal = Arch Gynecol Obstet | volume = 264 | issue = 2 | pages = 101-4 | month = Sep | year = 2000 | doi = | PMID = 11045335 }}</ref> | |||
===Microscopic=== | |||
Features: | |||
*"Swiss chesse-like" appearance / bubbly appearance. | |||
*Usually patchy and focal. | |||
Note: | |||
*Cistern formation is reported in the stem villi in association with congenital adrenal hyperplasia.<ref name=pmid11045335/> | |||
DDx: | |||
*[[Chorioamnionitis]]. | |||
*Fetal edema. | |||
*Idiopathic (no cause apparent). | |||
*[[Placental villous immaturity]]. | |||
Image: | |||
*[http://www.med.yale.edu/obgyn/kliman/placenta/articles/EOR_Placenta/Image19.gif villous edema (yale.edu)].<ref>URL: [http://www.med.yale.edu/obgyn/kliman/placenta/articles/EOR_Placenta/Trophtoplacenta.html http://www.med.yale.edu/obgyn/kliman/placenta/articles/EOR_Placenta/Trophtoplacenta.html]. Accessed on: 28 May 2011.</ref> | |||
==Placental villous immaturity== | |||
{{Main|Placental villous immaturity}} | |||
==Villous hypoplasia== | |||
*[[AKA]] ''terminal villus deficiency''.<ref name=Ref_Placenta346>{{Ref Placenta|346}}</ref> | |||
{{Main|Villous hypoplasia}} | |||
=Diseases of the placental attachment= | |||
==Placenta creta== | |||
Includes ''placenta accreta'', ''placenta increta'', and ''placenta percreta''. | |||
{{Main|Placenta creta}} | |||
==Placental abruption== | ==Placental abruption== | ||
{{Main|Placental abruption}} | |||
=Inflammatory pathologies= | |||
===Overview of infections=== | |||
General:<ref name=Ref_PBoD1106>{{Ref PBoD|1106}}</ref> | General:<ref name=Ref_PBoD1106>{{Ref PBoD|1106}}</ref> | ||
*Infection usually ascending, i.e. from vagina up through cervix. | *Infection usually ascending, i.e. from vagina up through cervix. | ||
** | **Associated with intercourse. | ||
*Hematogenous rare - manifest as villitis. | *Hematogenous rare - manifest as villitis. | ||
**Think ''[[TORCH infections]]'' (toxoplasmosis, others (syphilis, TB, listeriosis), rubella, cytomegalovirus, herpes simplex virus). | **Think ''[[TORCH infections]]'' ([[toxoplasmosis]], others ([[syphilis]], [[TB]], listeriosis), rubella, [[cytomegalovirus]], [[herpes simplex virus]]). | ||
*Funisitis usually follows chorioamnionitis. | *Funisitis usually follows chorioamnionitis. | ||
**Inflammatory cells in umbilical cord are fetal (trivia). | **Inflammatory cells in umbilical cord are fetal (trivia). | ||
=== | ====Types==== | ||
Membranitis<ref>Sternberg | By site:<ref name=Ref_PBoD1106>{{Ref PBoD|1106}}</ref> | ||
*Fetal membranes: chorioamnionitis, membranitis.<ref name=Ref_Sternberg4_2311>{{Ref Sternberg4|2311}}</ref> | |||
*Umbilical cord: funisitis. | |||
*Placenta: placentitis, villitis. | |||
==Membranitis== | |||
:''Chorionitis'' redirects here. | |||
===General=== | |||
*Early [[chorioamnionitis]].<ref>{{Cite journal | last1 = Vedovato | first1 = S. | last2 = Zanardo | first2 = V. | title = [Chorioamnionitis and inflammatory disease in the premature newborn infant]. | journal = Minerva Pediatr | volume = 62 | issue = 3 Suppl 1 | pages = 155-6 | month = Jun | year = 2010 | doi = | PMID = 21090086 }}</ref> | |||
*Controversial.{{fact}} | |||
===Microscopic=== | |||
Features: | |||
*[[PMN]]s in the decidua. | |||
*+/-PMNs in subamniotic tissue. | |||
*+/-Necrosis in decidua or chorion/subamniotic tissue. | |||
Note: | |||
*Plasma cells in the decidua = [[chronic deciduitis]]. | |||
DDx: | |||
*[[Chorioamnionitis]]. | |||
====Grading membranitis==== | |||
''Sternberg'':<ref name=Ref_Sternberg4_2311>{{Ref Sternberg4|2311}}</ref> | |||
# PMNs - decidua only. | # PMNs - decidua only. | ||
# PMNs - in subamniotic tissue. | # PMNs - in subamniotic tissue. | ||
# 1 or 2 + necrosis in decidua or chorion/subamniotic tissue | # 1 or 2 + [[necrosis]] in decidua or chorion/subamniotic tissue. | ||
===Sign out=== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: | |||
- FETAL MEMBRANES WITH CHORIONITIS. | |||
- THREE VESSEL UMBILICAL CORD WITH VASCULITIS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI. | |||
</pre> | |||
====Waffle==== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: | |||
- FETAL MEMBRANES WITH MECONIUM-LADEN MACROPHAGES AND ABUNDANT DECIDUAL NEUTROPHILS | |||
SUSPICIOUS FOR EARLY CHORIONITIS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI. | |||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
</pre> | |||
==Chorioamnionitis== | |||
{{Main|Chorioamnionitis}} | |||
==Umbilical cord vasculitis== | |||
{{Main|Umbilical cord vasculitis}} | |||
== | ==Funisitis== | ||
{{Main|Funisitis}} | |||
* | *Inflammation of Wharton's jelly - the connective tissue of the umbilical cord. | ||
== | ==Acute villitis== | ||
{{main|Acute villitis}} | |||
== | ==Villitis of unknown etiology== | ||
{{Main|Villitis of unknown etiology}} | |||
== | ==Chronic intervillitis== | ||
*> | *[[AKA]] ''chronic intervillositis''.<ref name=pmid8215826>{{Cite journal | last1 = Jacques | first1 = SM. | last2 = Qureshi | first2 = F. | title = Chronic intervillositis of the placenta. | journal = Arch Pathol Lab Med | volume = 117 | issue = 10 | pages = 1032-5 | month = Oct | year = 1993 | doi = | PMID = 8215826 }}</ref> | ||
===General=== | ===General=== | ||
* | *Rare. | ||
*Massive chronic intervillitis - associated [[IUGR]], spontaneous abortion, perinatal fetal death.<ref name=pmid17088773>{{Cite journal | last1 = Rota | first1 = C. | last2 = Carles | first2 = D. | last3 = Schaeffer | first3 = V. | last4 = Guyon | first4 = F. | last5 = Saura | first5 = R. | last6 = Horovitz | first6 = J. | title = [Perinatal prognosis of pregnancies complicated by placental chronic intervillitis]. | journal = J Gynecol Obstet Biol Reprod (Paris) | volume = 35 | issue = 7 | pages = 711-9 | month = Nov | year = 2006 | doi = | PMID = 17088773 }}</ref> | |||
=== | *Recurs. | ||
* | ===Microscopic=== | ||
* | Features:<ref name=pmid8215826/><ref name=pmid17088773/> | ||
** | *Intervillous inflammatory cells: | ||
** | **Lymphocytes. | ||
* | **Histiocytes. | ||
*Fibrinoid deposition. | |||
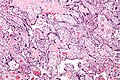
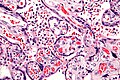
=== | ====Images==== | ||
* | <gallery> | ||
Image:Intervillitis_-_intermed_mag.jpg | Intervillitis - intermed. mag. (WC) | |||
Image:Intervillitis_-_very_high_mag.jpg | Intervillitis - very high mag. (WC) | |||
</gallery> | |||
==Chronic deciduitis== | |||
*[[AKA]] plasma cell deciduitis. | |||
{{Main|Chronic deciduitis}} | |||
=Placental infarction= | |||
==True infarcts== | |||
{{Main|Placental infarct}} | |||
==Perivillous fibrin deposition== | ==Perivillous fibrin deposition== | ||
* | *Abbreviation ''PFD''. | ||
* | ===General=== | ||
*Thought to be an immunologic problem - resulting in platelet activation and fibrin deposition.<ref name=pmid12066949>{{Cite journal | last1 = Sebire | first1 = NJ. | last2 = Backos | first2 = M. | last3 = Goldin | first3 = RD. | last4 = Regan | first4 = L. | title = Placental massive perivillous fibrin deposition associated with antiphospholipid antibody syndrome. | journal = BJOG | volume = 109 | issue = 5 | pages = 570-3 | month = May | year = 2002 | doi = | PMID = 12066949 }}</ref> | |||
*May be associated with [[diabetes mellitus]].<ref name=Ref_Placenta327>{{Ref Placenta|327}}</ref> | |||
===Gross=== | ===Gross=== | ||
| Line 207: | Line 643: | ||
*White fibrous sepatae. | *White fibrous sepatae. | ||
=== | ===Microscopic=== | ||
Features: | |||
*Acellular eosinophilic material around formed villi. | *Acellular eosinophilic material around formed villi. | ||
*Obliteration of intervillous space. | |||
**Intervillous distance increased vis-a-vis normal - '''key feature'''. | |||
* | |||
* | |||
Notes: | |||
* | *Nuclei of villi are usually preserved. | ||
* | *Villi may have secondary infarction, i.e. there may be [[Basics#Nuclear destruction words|nuclear destruction]] (karyolysis, karyorrhexis, pyknosis). | ||
DDx: | |||
* | *[[Placental infarction]] - loss of nuclei in the villi (below the edge of the lesion). | ||
* | *[[Massive perivillous fibrin deposition]] (maternal floor infarct). | ||
Images: | Images: | ||
*[http:// | *[http://path.upmc.edu/cases/case75.html APLA syndrome (upmc.edu)]. | ||
=== | ===Sign out=== | ||
====Thrombi==== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: | |||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
- FETAL MEMBRANES WITHIN NORMAL LIMITS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI AND THREE LARGE INTERVILLOUS | |||
THROMBI (BLOCKS A7-A9). | |||
</pre> | |||
== | ==Maternal floor infarction== | ||
* | *Abbreviated ''MFI''. | ||
* | *Formally ''placental maternal floor infarction''. | ||
*[[AKA]] ''massive perivillous fibrin deposition''.<ref name=Ref_Placenta367>{{Ref Placenta|367}}</ref> | |||
{{Main|Maternal floor infarction}} | |||
== | =Fetal disease= | ||
==Fetal thrombotic vasculopathy== | |||
{| | *Abbreviated ''FTV''. | ||
| | *A large number of terms are used for this including:<ref name=pmid19237859>{{Cite journal | last1 = Marchetti | first1 = D. | last2 = Belviso | first2 = M. | last3 = Fulcheri | first3 = E. | title = A case of stillbirth: the importance of placental investigation in medico-legal practice. | journal = Am J Forensic Med Pathol | volume = 30 | issue = 1 | pages = 64-8 | month = Mar | year = 2009 | doi = 10.1097/PAF.0b013e318187387e | PMID = 19237859 }}</ref> | ||
|- | **''Fibrinous vasculosis''. | ||
| | **''Fibromuscular sclerosis''. | ||
| | **''Fetal artery stem thrombosis''. | ||
*The multitude of terms reflects the confusion about this finding and that it has numerous etiologies.<ref name=pmid19237859/> | |||
{{Main|Fetal thrombotic vasculopathy}} | |||
|} | |||
=== | ==Hemorrhagic endovasculitis== | ||
*Abbreviated ''HEV''. | |||
{| | ===General=== | ||
| | *Associated with stillbirth.<ref name=pmid6151926>{{cite journal |author=Stevens NG, Sander CH |title=Placental hemorrhagic endovasculitis: risk factors and impact on pregnancy outcome |journal=Int J Gynaecol Obstet |volume=22 |issue=5 |pages=393–7 |year=1984 |month=October |pmid=6151926 |doi= |url=}}</ref> | ||
| | |||
| | |||
|} | |||
===Microscopic=== | |||
Features:<ref name=pmid11825110>{{cite journal |author=Sander CM, Gilliland D, Akers C, McGrath A, Bismar TA, Swart-Hills LA |title=Livebirths with placental hemorrhagic endovasculitis: interlesional relationships and perinatal outcomes |journal=Arch. Pathol. Lab. Med. |volume=126 |issue=2 |pages=157–64 |year=2002 |month=February |pmid=11825110 |doi= |url=}}</ref> | |||
=== | *Walls of the (fetal) placental blood vessels (in the villi) are disrupted. | ||
*+/-Intraluminal necrotic debris. | |||
*[[RBC]] fragmentation. | |||
* | |||
* | |||
=Maternal disease= | |||
==Hypertensive changes== | ==Hypertensive changes== | ||
===General=== | |||
Associated pathologic changes:<ref name=pmid6754249>{{cite journal |author=Soma H, Yoshida K, Mukaida T, Tabuchi Y |title=Morphologic changes in the hypertensive placenta |journal=Contrib Gynecol Obstet |volume=9 |issue= |pages=58–75 |year=1982 |pmid=6754249 |doi= |url=}}</ref> | |||
*Placental infarcts. | *Placental infarcts. | ||
*Increased syncytial knots. | *Increased syncytial knots. | ||
| Line 287: | Line 707: | ||
*Thickening of the trophoblastic basement membrane. | *Thickening of the trophoblastic basement membrane. | ||
=== | ===Microscopic=== | ||
Features:<ref name= | Features:<ref name=pmid6754249>{{cite journal |author=Soma H, Yoshida K, Mukaida T, Tabuchi Y |title=Morphologic changes in the hypertensive placenta |journal=Contrib Gynecol Obstet |volume=9 |issue= |pages=58–75 |year=1982 |pmid=6754249 |doi= |url=}}</ref> | ||
* | *Enlarged endothelial cells - fetal capillaries. | ||
*Atherosis of the spiral arteries - placental bed (maternal). | |||
* | |||
Notes: | |||
* | *One should look for the changes in the membrane roll, not the maternal surface.<ref>Sherman, C. 7 February 2011.</ref> | ||
Images: | Images: | ||
*[http:// | *[http://www.pathxchange.org/case/19711 Pregnancy-induced hypertension (pathxchange.org)]. | ||
==Hypertrophic decidual vasculopathy== | |||
:[[AKA]] ''decidual vasculopathy''. | |||
{{Main|Hypertrophic decidual vasculopathy}} | |||
==HELLP syndrome== | ==HELLP syndrome== | ||
{{Main|HELLP syndrome}} | |||
==Malaria== | |||
{{Main|Malaria}} | |||
===General=== | ===General=== | ||
* | *Uncommon in Canada. | ||
*May lead to fetal demise. | |||
===Microscopic=== | |||
Feature: | |||
*[[RBC]]s with basophilic dots ~1-2 micrometres. | |||
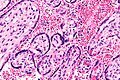
====Image==== | |||
* | <gallery> | ||
* | Image:Maternal_malaria_placenta_-_very_high_mag.jpg | Maternal malaria - very high mag. (WC) | ||
* | </gallery> | ||
=Tumours= | |||
{{main|Gestational trophoblastic disease}} | |||
==Chorangioma== | |||
{{Main|Chorangioma}} | |||
==Chorangiomatosis== | |||
===General=== | |||
Associated with: | |||
*Preeclampsia. | |||
*[[IUGR]]. | |||
===Gross=== | |||
*Multiple tan nodules. | |||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref | Features: | ||
* | *Multiple chorangiomas - the difference between chorangioma and chorangiomatosis is not well defined.<ref>URL: [http://path.upmc.edu/cases/case655/dx.html http://path.upmc.edu/cases/case655/dx.html]. Accessed on: 28 January 2012.</ref> | ||
** | |||
Images: | |||
*[http://path.upmc.edu/cases/case655.html Chorangiomatosis - several images (upmc.edu)]. | |||
==Chorangiosis== | |||
{{Main|Chorangiosis}} | |||
=Other= | |||
==Fetus papyraceus== | |||
*May be spelled ''foetus papyraceus''. | |||
*[[AKA]] ''fetus compressus''. | |||
{{Main|Fetus papyraceus}} | |||
==Placental mesenchymal dysplasia== | |||
*Abbreviated ''PMD''. | |||
{{Main|Placental mesenchymal dysplasia}} | |||
== | =Placental cysts and pseudocysts= | ||
{{ | Types:<ref name=Ref_Placenta219-220>{{Ref Placenta|219-220}}</ref> | ||
*Amnionic epithelial inclusion cyst (amniotic cyst). | |||
*[[Epidermal inclusion cyst]] - lined by keratinized squamous epithelium. | |||
*Chorionic cyst ([[AKA]] chorionic pseudocyts). | |||
*Cell island cyst. | |||
Other considerations:<ref name=pmid12054300>{{Cite journal | last1 = Brown | first1 = DL. | last2 = DiSalvo | first2 = DN. | last3 = Frates | first3 = MC. | last4 = Davidson | first4 = KM. | last5 = Genest | first5 = DR. | title = Placental surface cysts detected on sonography: histologic and clinical correlation. | journal = J Ultrasound Med | volume = 21 | issue = 6 | pages = 641-6; quiz 647-8 | month = Jun | year = 2002 | doi = | PMID = 12054300 }}</ref> | |||
*Hematoma. | |||
*Fibrin-lined pseudocyst. | |||
= | General:<ref name=pmid12054300/> | ||
* | *Usually good outcome. | ||
*Large cysts (>4.5 cm) or multiple cysts (>3) are associated with [[IUGR]]. | |||
Images: | |||
*[http://www.jultrasoundmed.org/content/21/6/641/F5.expansion.html Subchorionic cysts (jultrasoundmed.org)].<ref name=pmid12054300/> | |||
=See also= | |||
*[[Chorionic villi]]. | *[[Chorionic villi]]. | ||
*[[Endometrium]]. | *[[Endometrium]]. | ||
*[[Pregnancy]]. | *[[Pregnancy]]. | ||
*[[Gestational trophoblastic disease]]. | |||
*[[TORCH infections]]. | |||
=References= | |||
{{reflist|2}} | {{reflist|2}} | ||
[[Category: | =Recommended reading= | ||
*{{cite journal |author=Langston C, Kaplan C, Macpherson T, ''et al.'' |title=Practice guideline for examination of the placenta: developed by the Placental Pathology Practice Guideline Development Task Force of the College of American Pathologists |journal=Arch. Pathol. Lab. Med. |volume=121 |issue=5 |pages=449–76 |year=1997 |month=May |pmid=9167599 |doi= |url=}} | |||
*{{cite book |author= Baergen, Rebecca N. |title=[http://www.amazon.com/Manual-Benirschke-Kaufmanns-Pathology-Placenta/dp/0387220895/ref=sr_1_1?ie=UTF8&qid=1297169019&sr=8-1 Manual of Benirschke and Kaufmann's Pathology of the Human Placenta] |publisher=Springer |location= |year=2005 |pages= {{{1|}}} |edition=1st |isbn=978-0387220895 |oclc= |doi= |accessdate=}} | |||
=External links= | |||
*[http://emedicine.medscape.com/article/262470-overview Cord complications (emedicine.medscape.com)]. | |||
*[http://www.palpath.com/MedicalTestPages/placenta2.htm Placenta notes (palpath.com)]. | |||
[[Category:Placenta]] | |||
Latest revision as of 15:27, 10 May 2018
The placenta feeds the developing baby, breathes for it and disposes of its waste.
The organ is one that seems to be left behind; at least one review suggests it isn't done so well by general pathologists.[1]
Placental pathology redirects to this article.
Clinical
Examination of the placenta
- Most placentas are not examined by a pathologist.
Indications for exam by pathology
Some indications for exam by a pathologist:
- Abnormalities in the:
- Fetus:
- Bad fetal outcome.
- Suspected or known congenital abnormalities or chromosomal abnormalities.
- IUGR.
- Mother:
- Infection/suspected infection.
- Pre-term labour.
- Maternal disease (e.g. SLE, coagulopathy).
- Complicated pregnancy (preclampsia, pregnancy induced hypertension, gestational diabetes).
- Placenta:
- Unusual gross characteristics.[2]
- Fetus:
A more detailed list is given by Hargitai et al.[3] and Chang.[4]
Most common
Most common reasons for submitting a placenta to pathology:[5]
- Prematurity.
- PROM / possible chorioamnionitis.
- Multiple gestation.
Bleeding in late pregnancy
DDx of bleeding in late pregnancy:
- Placental abruption (most common).
- Placenta previa.
- Vasa previa (fetus losing blood).
Clinical screening tests
- PAPP-A - low values seen in aneuploidy.[6]
Abbreviations
- C/S = Caesarean section.
- LSCS = lower segment C-section.
- FTP = failure to progress.
- PROM = premature rupture of membranes.
- PPROM = preterm premature ruptures of membranes.
- IUGR = intrauterine growth restriction.
- IOL = induction of labour.
Normal histology
Villi
This is dealt with in a separate article that also covers the types of trophoblast (cytotrophoblast, syncytiotrophoblast, intermediate trophoblast).
Cord
Omphalomesenteric duct remnant
- AKA vitelline duct.
- Benign embryologic remnant.
Features:
- Duct with benign looking cuboidal epithelium.
Allantoic duct remnant
- Benign embryologic remnant.
Features:
- Duct with benign looking flat epithelium.
Vitelline artery remnant
Features:
- Small artery in the cord.
Membranes
Fetus to mother:
- Amnion - thin layer: one cell layer, basement membrane, connective tissue.
- Cleft - artifactual - empty space.
- Chorion - vascular.
- Decidua (maternal tissue) - may contain obsolete chorionic villi; place to look for hypertensive changes.
Amnion
General:
- Next to fetus, surrounds amniotic fluid, avascular.
Characteristics:
- Characterized by a single layer of cells.[7]
- Cuboidal/squamoid shape.
- Eosinophilic cytoplasm.
- Central nucleus.
- Squamous metaplasia may be seen at cord insertion.
- Basement membrane.
- 'Compact layer'.[7]
- 'Fibroblastic layer'.[7]
Chorion
General:
- Surrounds amnion.
Characteristics:
- Layers:[8]
- 'Reticular layer' - cellular (inner aspect).
- 'Pseudo-basemement membrane'.
- 'Outer trophoblastic layer'.
- Has blood vessels.
- Opposed to "trophoblastic X cells" on side opposite of amnion.[7]
- Beneath of the "trophoblastic X cells" is decidua (mnemonic NEW = nucleus central, eosinophilic, well-defined cell border), which is maternal tissue.
Note:
- Fibrin deposition may be found deep to the chorion - known as subchorionic fibrin deposition.
- Gross: subchorionic, white/yellow, laminated, classically has a triangular-shape with the base of triangle parallel to fetal aspect of disc.
- Arises due to localized stasis of the inter-villous maternal blood.
- Focal small deposits are considered to be a normal finding - seen in ~15% of cases.[9][10]
- The pathologic counterpart of this is perivillous fibrin deposition.
- Gross: subchorionic, white/yellow, laminated, classically has a triangular-shape with the base of triangle parallel to fetal aspect of disc.
Image:
Common terms
- Chorionic plate - fetal aspect of placenta.
- Basal plate - maternal aspect of placenta.
- Has extravillous trophoblast.
- Place to look for maternal vessels.
Grossing
This is often very quick. The gross is quite important, as some things cannot be diagnosed microscopically.
General
- Dimensions:
- Disc.
- Length of cord, diameter of cord.
- Accessory lobes - dimensions.
- Two lobes of equal size + cord arises in between = bilobate placenta.
- Mass (weight).
- Should be done 'trimmed' (cord cut-off, membrane cut-off).
- Should be done when placenta is "fresh", i.e. not fixed -- as mass tables are based on fresh state.
- Umbilical cord
- Attachment.
- Location: central, eccentric, marginal.
- Marginal attachment assoc. with hypertension[11]
- Membranous or velamentous (veil-like) insertion.
- Vessels separate/branch prior to reaching placental disc.
- Furcate insertion - blood vessels separate before reaching placenta disc/not surrounded by Wharton's jelly - vessels more exposed to trauma (risk for vasa previa).
- Location: central, eccentric, marginal.
- Knots (false vs. true).
- False knots are nothing to worry about -- look like a knot but aren't really one.
- Twisting/coiling - 1-3 coils/10 cm is normal.
- Number of vessels.
- Normal: 2 arteries, 1 vein.
- Attachment.
- Membranes - shiny & translucent - normal (green, opaque/dull - chorioamnionitis).
- Attachment (insertion): marginal (normal), circummarginate (inside edge), circumvallate (folding on self).
- Site of rupture - if obvious; low point of rupture suggests low-lying placenta.
- Placental disc.
- Fetal surface - normal is shinny.
- Dull in chorioamnionitis.
- Maternal surface
- Are the cotyledons intact?
- Adherent clot?
- Parenchyma - after sectioning:
- White vs. red nodules.
- Fetal surface - normal is shinny.
Notes:
- Parenchymal nodules - a brief DDx:
- White: infarct (chronic), thrombi, chorangioma, perivillous fibrin deposition.
- Red: infarct (acute), thrombi.
Sections
- Cord two sections.
- Membranes (rolled), two rolls or more.[12]
- Cord at insertion + disc.
- Placenta - full thickness (maternal and fetal surface).
- Sections should not be taken at the margin of the disc.
Placental membranes
Appearance:[13]
- Normal - shiny.
- Chorioamnionitis - opaque/dull.
- Meconium - green.
- Amnion nodosum - yellow patches.
- Some describe 'em as white.[14]
Placental mass
It is considered routine to obtain a mass for the placenta. This is usually done when the placenta is fresh and with the membranes and cord trimmed, as most tables of placental mass were created with these parameters.
Placental mass by gestational age:[15]
| Gest. Age/Percentile | 25% | 50% | 75% |
| 32 weeks | 275 g | 318 g | 377 g |
| 36 weeks | 369 g | 440 g | 508 g |
| 40 weeks | 440 g | 501 g | 572 g |
Linear regression - placental mass-gestational age
Based on the table in the AFIP book[16] one can generate the following regression lines:
| 50% | 10% | 90% | |
| slope (g/week) | 21.58088235 | 19.70588235 | 25.40196078 |
| y-intercept (g) | -357.4558824 | -397.2352941 | -366.7254902 |
| Pearson (r) | 0.988670724 | 0.988268672 | 0.982206408 |
placental mass = slope x gestational age + intercept
What to remember...
Extrapolated from the linear regression (see above):
- 50% at term = 500 grams.
- 50% at 26 weeks = 200 grams.
- The change in mass/week is approximately linear and equal to 300 grams / 14 weeks ~ 20 grams/week.
- The spread in mass between 10% and 90%, crudely estimated, is 200 grams (for GA=26-40).
Notes:
- Is it required?
- Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.[17]
- In the context of quality, a measure (even if somewhat flawed) is probably more reproducible and objective than arbitrary descriptors which require experience and a continuing case volume to calibrate.
- Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.[17]
Placentomegaly
- AKA large placenta.
Associations:[18]
- Maternal diabetes - esp. poorly controlled.[19]
- Maternal anemia/low maternal iron stores.[20]
- Fetal malformations.
- Neoplasms of the placenta, e.g. chorangioma.
- Twin-twin transfusion syndrome.
- Chronic intrauterine infections, e.g. syphilis, toxoplasmosis, cytomegalovirus.
Lame causes of a heavy placenta:
- Dates wrong - error in determining the estimated date of confinement.
- Adherent blood clot.
Comment:
- Most of causes seem to have one thing in common:
- There is a decreased oxygen delivery to the fetus.
Sign out
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: - LARGE PLACENTA (819 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). - FETAL MEMBRANES WITHIN NORMAL LIMITS. - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI.
Placental growth restriction
- AKA placenta small for gestational age.
- Small placenta redirects here.
Associations:
- Maternal vascular disease, e.g. hypertension.
- Fetal malformations.
Sign out
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - PLACENTA SMALL FOR GESTATIONAL AGE (160 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITH: -- OLD CENTRAL TRANSMURAL INFARCT (1.7 CM MAXIMAL DIMENSION). COMMENT: The 10th percentile placental mass (pre-fixation) for 34 weeks and 2 days is approximately 390 grams.
Overview of placental pathology
Approach
The pathology of the placenta is diverse and is not easy to group.
It terms of remembering things. It is probably easiest to take a combined anatomical, etiologic and morphologic approach.
Anatomical basis:
- Cord.
- Membranes.
- Disc.
Etiologic:
- Congential.
- Infectious.
- Neoplastic.
- Endocrine.
- Trauma.
- Vascular.
- Degenerative.
- Autoimmune.
- Toxic.
- Idiopathic.
Compartmental:
- Vasculature.
- Membranes.
- Parenchyma:
- Maternal part (decidua).
- Fetal part (villi, cord).
Common entities/diagnoses
- Normal.
- Chorioamnionitis.
- Placental abruption.
- Meconium.
- Hypertensive changes.
Sign out
What should be commented on...
- Placenta:
- Maturity of villi (2nd or 3rd trimester).
- Infarction?
- Subchorionic less important than maternal aspect.
- Peripheral aspect of placental disc less important than central region of disc.
- Blood vessels.
- Maternal.
- Fetal.
- Membranes.
- Cord:
- 3 vessel?
- Vasculitis/inflammation?
Mnemonic: chorio, cord, vessels, villi (maturity, infarction).
Normal placenta
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
C-section
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CAESAREAN SECTION: - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Cord pathology
- Two vessel cord.
- Hypercoiling/Hypocoiling.
- Abnormal insertion.
- Cord knots (true vs. false).
- Strictures.
- Hematoma.
- Hemangioma.
- Benign cyst.
Two vessel umbilical cord
Insertion
Marginal insertion
Definition:
- The umbilical cord is attached to the placental disc at its margin.
Prevalence:
- Approximately 12% of placentas.[21]
Relevance:
- None according to WMSP.[21]
- In theory, the cord, dependent on its relation to the internal os, is at greater risk of injury (leading to vasa previa) and compression (fetal hypoxia). A retrospective study found cord position in relation to the internal os is predictive for vasa previa.[22]
Velamentous insertion
Definition:
- The umbilical cord inserts into the fetal membranes.[21]
- The vessels are not protected by Wharton's jelly.
- Wharton's jelly = the connective tissue surrounding the vessels in the cord.
- The vessels are not protected by Wharton's jelly.
Details:[21]
- 3/4 of the time the vessel also branch; in the remaining 1/4 the vessels stay together.
Relevance:
- Increased risk of vasa previa.[22]
Sign out
PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - THREE VESSEL UMBILICAL CORD WITH A VELAMENTOUS INSERTION, OTHERWISE WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Umbilical knot
General
- Prevalence ~1.25%.[23][24]
- Increase risk of stillbirth; odds ratio 3.93.[23]
Gross
Work-up:[24]
- Diameter measures and colour on both sides of the knot.
- Knot should be untied to assess for deformation of Wharton's jelly.
- Sections from both sides of the knot - to look for thrombi.
Note:
- False knots (large diameter - focally) are common - they cannot be untied.
Microscopic
Features:
- +/-Thrombi.
- Fibrin deposition.
- +/-Lines of Zahn.
Images:
Coiling
- Hypo- and hypercoiling are both considered problematic.[21]
- Normal: 1-3 coils/10 cm.[25]
- Associated with cord stricture, which is usu. at the fetal end of the cord.[26]
Notes:
- There is little uniformity in how coiling is assessed in the medical literature - though 10% and 90% are considered the cut-points for normal.[27]
- What are the 10% and 90% cut-points? They are not given in WMSP. UT access to a journal article[28] that might have it is screwed-up.
Cord hematoma
Features:[26]
- Rare ~ 1/5500.
- Mortality ~50% is severe.
Membranes
- Squamous metaplasia.
- Chorioamnionitis - see infection section.
Amnion nodosum
Placental meconium
Squamous metaplasia of the amnion
General
- Benign common finding thought to be of no clinical significance.[29]
- One case report suggesting an association with chorioamnionitis.[30]
- Needs to be separated from amnion nodosum - important.[31]
Gross
Features:[32]
- White (or yellow) plaques - irregular outline.
DDx:
- Amnion nodosum - small (~1-5 mm), round, classically yellow.
Images:
Microscopic
Features:[32]
- Dense, paucicellular (pink) compact keratin - key feature.
Image:
Circumvallate placenta
- AKA circumvallate insertion of the membranes.
General
- May be associated with placental abruption.[34]
Note:
- Membranes usually attach to the edge of the placenta.
Gross
- Fetal membranes attach to the fetal surface of the placenta away from the margin of the placental disc.
Classification:
- Partial - not circumferential.
- Complete.
DDx:
Images:
Twin placentas
These are often submitted... even if they are normal. In these specimens, usually, the chorion is the key.
It covers:
- Monozygotic vs. dizygotic twins.
- Twin-to-twin transfusion syndrome.
Placental disc
Villous edema
General
- Non-specific finding.
- Reported in associated with congenital adrenal hyperplasia for the stem villi.[35]
Microscopic
Features:
- "Swiss chesse-like" appearance / bubbly appearance.
- Usually patchy and focal.
Note:
- Cistern formation is reported in the stem villi in association with congenital adrenal hyperplasia.[35]
DDx:
- Chorioamnionitis.
- Fetal edema.
- Idiopathic (no cause apparent).
- Placental villous immaturity.
Image:
Placental villous immaturity
Villous hypoplasia
Diseases of the placental attachment
Placenta creta
Includes placenta accreta, placenta increta, and placenta percreta.
Placental abruption
Inflammatory pathologies
Overview of infections
General:[38]
- Infection usually ascending, i.e. from vagina up through cervix.
- Associated with intercourse.
- Hematogenous rare - manifest as villitis.
- Think TORCH infections (toxoplasmosis, others (syphilis, TB, listeriosis), rubella, cytomegalovirus, herpes simplex virus).
- Funisitis usually follows chorioamnionitis.
- Inflammatory cells in umbilical cord are fetal (trivia).
Types
By site:[38]
- Fetal membranes: chorioamnionitis, membranitis.[39]
- Umbilical cord: funisitis.
- Placenta: placentitis, villitis.
Membranitis
- Chorionitis redirects here.
General
- Early chorioamnionitis.[40]
- Controversial.[citation needed]
Microscopic
Features:
- PMNs in the decidua.
- +/-PMNs in subamniotic tissue.
- +/-Necrosis in decidua or chorion/subamniotic tissue.
Note:
- Plasma cells in the decidua = chronic deciduitis.
DDx:
Grading membranitis
Sternberg:[39]
- PMNs - decidua only.
- PMNs - in subamniotic tissue.
- 1 or 2 + necrosis in decidua or chorion/subamniotic tissue.
Sign out
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: - FETAL MEMBRANES WITH CHORIONITIS. - THREE VESSEL UMBILICAL CORD WITH VASCULITIS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI.
Waffle
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES WITH MECONIUM-LADEN MACROPHAGES AND ABUNDANT DECIDUAL NEUTROPHILS SUSPICIOUS FOR EARLY CHORIONITIS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI. - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS.
Chorioamnionitis
Umbilical cord vasculitis
Funisitis
- Inflammation of Wharton's jelly - the connective tissue of the umbilical cord.
Acute villitis
Villitis of unknown etiology
Chronic intervillitis
General
- Rare.
- Massive chronic intervillitis - associated IUGR, spontaneous abortion, perinatal fetal death.[42]
- Recurs.
Microscopic
- Intervillous inflammatory cells:
- Lymphocytes.
- Histiocytes.
- Fibrinoid deposition.
Images
Chronic deciduitis
- AKA plasma cell deciduitis.
Placental infarction
True infarcts
Perivillous fibrin deposition
- Abbreviation PFD.
General
- Thought to be an immunologic problem - resulting in platelet activation and fibrin deposition.[43]
- May be associated with diabetes mellitus.[44]
Gross
- Pale (white).
- Firm.
- White fibrous sepatae.
Microscopic
Features:
- Acellular eosinophilic material around formed villi.
- Obliteration of intervillous space.
- Intervillous distance increased vis-a-vis normal - key feature.
Notes:
- Nuclei of villi are usually preserved.
- Villi may have secondary infarction, i.e. there may be nuclear destruction (karyolysis, karyorrhexis, pyknosis).
DDx:
- Placental infarction - loss of nuclei in the villi (below the edge of the lesion).
- Massive perivillous fibrin deposition (maternal floor infarct).
Images:
Sign out
Thrombi
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI AND THREE LARGE INTERVILLOUS THROMBI (BLOCKS A7-A9).
Maternal floor infarction
- Abbreviated MFI.
- Formally placental maternal floor infarction.
- AKA massive perivillous fibrin deposition.[45]
Fetal disease
Fetal thrombotic vasculopathy
- Abbreviated FTV.
- A large number of terms are used for this including:[46]
- Fibrinous vasculosis.
- Fibromuscular sclerosis.
- Fetal artery stem thrombosis.
- The multitude of terms reflects the confusion about this finding and that it has numerous etiologies.[46]
Hemorrhagic endovasculitis
- Abbreviated HEV.
General
- Associated with stillbirth.[47]
Microscopic
Features:[48]
- Walls of the (fetal) placental blood vessels (in the villi) are disrupted.
- +/-Intraluminal necrotic debris.
- RBC fragmentation.
Maternal disease
Hypertensive changes
General
Associated pathologic changes:[49]
- Placental infarcts.
- Increased syncytial knots.
- Hypovascularity of the villi.
- Cytotrophoblastic proliferation.
- Thickening of the trophoblastic basement membrane.
Microscopic
Features:[49]
- Enlarged endothelial cells - fetal capillaries.
- Atherosis of the spiral arteries - placental bed (maternal).
Notes:
- One should look for the changes in the membrane roll, not the maternal surface.[50]
Images:
Hypertrophic decidual vasculopathy
- AKA decidual vasculopathy.
HELLP syndrome
Malaria
General
- Uncommon in Canada.
- May lead to fetal demise.
Microscopic
Feature:
- RBCs with basophilic dots ~1-2 micrometres.
Image
Tumours
Chorangioma
Chorangiomatosis
General
Associated with:
- Preeclampsia.
- IUGR.
Gross
- Multiple tan nodules.
Microscopic
Features:
- Multiple chorangiomas - the difference between chorangioma and chorangiomatosis is not well defined.[51]
Images:
Chorangiosis
Other
Fetus papyraceus
- May be spelled foetus papyraceus.
- AKA fetus compressus.
Placental mesenchymal dysplasia
- Abbreviated PMD.
Placental cysts and pseudocysts
Types:[52]
- Amnionic epithelial inclusion cyst (amniotic cyst).
- Epidermal inclusion cyst - lined by keratinized squamous epithelium.
- Chorionic cyst (AKA chorionic pseudocyts).
- Cell island cyst.
Other considerations:[53]
- Hematoma.
- Fibrin-lined pseudocyst.
General:[53]
- Usually good outcome.
- Large cysts (>4.5 cm) or multiple cysts (>3) are associated with IUGR.
Images:
See also
References
- ↑ Sun, CC.; Revell, VO.; Belli, AJ.; Viscardi, RM. (Jun 2002). "Discrepancy in pathologic diagnosis of placental lesions.". Arch Pathol Lab Med 126 (6): 706-9. doi:10.1043/0003-9985(2002)1260706:DIPDOP2.0.CO;2. PMID 12033960.
- ↑ Yetter JF (March 1998). "Examination of the placenta". Am Fam Physician 57 (5): 1045–54. PMID 9518951.
- ↑ Hargitai B, Marton T, Cox PM (August 2004). "Best practice no 178. Examination of the human placenta". J. Clin. Pathol. 57 (8): 785–92. doi:10.1136/jcp.2003.014217. PMC 1770400. PMID 15280396. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770400/.
- ↑ URL: http://smj.sma.org.sg/5012/5012ra1.pdf. Accessed on: 11 February 2011.
- ↑ Sherman C. 8 February 2011.
- ↑ URL: http://www.ncbi.nlm.nih.gov/sites/entrez?Db=gene&Cmd=ShowDetailView&TermToSearch=5069. Accessed on: 7 July 2010.
- ↑ 7.0 7.1 7.2 7.3 Sternberg, Stephen S. (1997). Histology for Pathologists (2nd ed.). Lippincott Williams & Wilkins. pp. 974. ISBN 978-0397517183.
- ↑ Sternberg, Stephen S. (1997). Histology for Pathologists (2nd ed.). Lippincott Williams & Wilkins. pp. 977. ISBN 978-0397517183.
- ↑ Narasimha, A.; Vasudeva, DS.. "Spectrum of changes in placenta in toxemia of pregnancy.". Indian J Pathol Microbiol 54 (1): 15-20. doi:10.4103/0377-4929.77317. PMID 21393870.
- ↑ URL: http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf. Accessed on: 17 August 2012.
- ↑ J Anat. Soc. India 49(2) 149-152 (2000). Available at: http://www.indmedica.com/anatomy/aindex1.cfm?anid=41. Accessed on: January 21, 2009.
- ↑ Winters R, Waters BL (December 2008). "What is adequate sampling of extraplacental membranes?: a randomized, prospective analysis". Arch. Pathol. Lab. Med. 132 (12): 1920–3. PMID 19061291.
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 461. ISBN 978-0443066450.
- ↑ CS. 7 February 2011.
- ↑ AFIP Placental pathol. ISBN: 1-881041-89-1. P.312
- ↑ AFIP Placental pathol. ISBN: 1-881041-89-1. P.312
- ↑ Fox, Harold; Sebire, Neil J. (2007). Pathology of the Placenta (Major Problems in Pathology) (3rd ed.). Saunders. pp. 559-561. ISBN 978-1416025924.
- ↑ URL: http://quizlet.com/5793113/ob-flash-cards/. Accessed on: 13 January 2012.
- ↑ Clarson, C.; Tevaarwerk, GJ.; Harding, PG.; Chance, GW.; Haust, MD.. "Placental weight in diabetic pregnancies.". Placenta 10 (3): 275-81. PMID 2771897.
- ↑ Hindmarsh, PC.; Geary, MP.; Rodeck, CH.; Jackson, MR.; Kingdom, JC. (Aug 2000). "Effect of early maternal iron stores on placental weight and structure.". Lancet 356 (9231): 719-23. PMID 11085691.
- ↑ 21.0 21.1 21.2 21.3 21.4 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 464. ISBN 978-0781765275.
- ↑ 22.0 22.1 Hasegawa J, Farina A, Nakamura M, et al. (December 2010). "Analysis of the ultrasonographic findings predictive of vasa previa". Prenat. Diagn. 30 (12-13): 1121–5. doi:10.1002/pd.2618. PMID 20872421.
- ↑ 23.0 23.1 Airas U, Heinonen S (April 2002). "Clinical significance of true umbilical knots: a population-based analysis". Am J Perinatol 19 (3): 127–32. doi:10.1055/s-2002-25311. PMID 12012287.
- ↑ 24.0 24.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 464. ISBN 978-0781765275.
- ↑ CS. 7 February 2011.
- ↑ 26.0 26.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 465. ISBN 978-0781765275.
- ↑ Khong TY (December 2010). "Evidence-based pathology: umbilical cord coiling". Pathology 42 (7): 618–22. doi:10.3109/00313025.2010.520309. PMID 21080869.
- ↑ PMID 16076615.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 463. ISBN 978-0781765275.
- ↑ Chew, RH.; Silberberg, BK. (Apr 1990). "Possible association of acute inflammatory exudate in chorioamnionitis and amniotic squamous metaplasia.". Am J Clin Pathol 93 (4): 582-5. PMID 2321592.
- ↑ CS. 7 February 2011.
- ↑ 32.0 32.1 32.2 Adeniran, AJ.; Stanek, J. (Dec 2007). "Amnion nodosum revisited: clinicopathologic and placental correlations.". Arch Pathol Lab Med 131 (12): 1829-33. doi:10.1043/1543-2165(2007)131[1829:ANRCAP]2.0.CO;2. PMID 18081444.
- ↑ URL: http://flylib.com/books/en/2.953.1.49/1/. Accessed on: 10 January 2011.
- ↑ Suzuki, S. (Feb 2008). "Clinical significance of pregnancies with circumvallate placenta.". J Obstet Gynaecol Res 34 (1): 51-4. doi:10.1111/j.1447-0756.2007.00682.x. PMID 18226129.
- ↑ 35.0 35.1 Furuhashi, M.; Oda, H.; Nakashima, T. (Sep 2000). "Hydrops of placental stem villi complicated with fetal congenital adrenal hyperplasia.". Arch Gynecol Obstet 264 (2): 101-4. PMID 11045335.
- ↑ URL: http://www.med.yale.edu/obgyn/kliman/placenta/articles/EOR_Placenta/Trophtoplacenta.html. Accessed on: 28 May 2011.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 346. ISBN 978-1441974938.
- ↑ 38.0 38.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1106. ISBN 0-7216-0187-1.
- ↑ 39.0 39.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 2311. ISBN 978-0781740517.
- ↑ Vedovato, S.; Zanardo, V. (Jun 2010). "[Chorioamnionitis and inflammatory disease in the premature newborn infant].". Minerva Pediatr 62 (3 Suppl 1): 155-6. PMID 21090086.
- ↑ 41.0 41.1 Jacques, SM.; Qureshi, F. (Oct 1993). "Chronic intervillositis of the placenta.". Arch Pathol Lab Med 117 (10): 1032-5. PMID 8215826.
- ↑ 42.0 42.1 Rota, C.; Carles, D.; Schaeffer, V.; Guyon, F.; Saura, R.; Horovitz, J. (Nov 2006). "[Perinatal prognosis of pregnancies complicated by placental chronic intervillitis].". J Gynecol Obstet Biol Reprod (Paris) 35 (7): 711-9. PMID 17088773.
- ↑ Sebire, NJ.; Backos, M.; Goldin, RD.; Regan, L. (May 2002). "Placental massive perivillous fibrin deposition associated with antiphospholipid antibody syndrome.". BJOG 109 (5): 570-3. PMID 12066949.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 327. ISBN 978-1441974938.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 367. ISBN 978-1441974938.
- ↑ 46.0 46.1 Marchetti, D.; Belviso, M.; Fulcheri, E. (Mar 2009). "A case of stillbirth: the importance of placental investigation in medico-legal practice.". Am J Forensic Med Pathol 30 (1): 64-8. doi:10.1097/PAF.0b013e318187387e. PMID 19237859.
- ↑ Stevens NG, Sander CH (October 1984). "Placental hemorrhagic endovasculitis: risk factors and impact on pregnancy outcome". Int J Gynaecol Obstet 22 (5): 393–7. PMID 6151926.
- ↑ Sander CM, Gilliland D, Akers C, McGrath A, Bismar TA, Swart-Hills LA (February 2002). "Livebirths with placental hemorrhagic endovasculitis: interlesional relationships and perinatal outcomes". Arch. Pathol. Lab. Med. 126 (2): 157–64. PMID 11825110.
- ↑ 49.0 49.1 Soma H, Yoshida K, Mukaida T, Tabuchi Y (1982). "Morphologic changes in the hypertensive placenta". Contrib Gynecol Obstet 9: 58–75. PMID 6754249.
- ↑ Sherman, C. 7 February 2011.
- ↑ URL: http://path.upmc.edu/cases/case655/dx.html. Accessed on: 28 January 2012.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 219-220. ISBN 978-1441974938.
- ↑ 53.0 53.1 53.2 Brown, DL.; DiSalvo, DN.; Frates, MC.; Davidson, KM.; Genest, DR. (Jun 2002). "Placental surface cysts detected on sonography: histologic and clinical correlation.". J Ultrasound Med 21 (6): 641-6; quiz 647-8. PMID 12054300.
Recommended reading
- Langston C, Kaplan C, Macpherson T, et al. (May 1997). "Practice guideline for examination of the placenta: developed by the Placental Pathology Practice Guideline Development Task Force of the College of American Pathologists". Arch. Pathol. Lab. Med. 121 (5): 449–76. PMID 9167599.
- Baergen, Rebecca N. (2005). Manual of Benirschke and Kaufmann's Pathology of the Human Placenta (1st ed.). Springer. ISBN 978-0387220895.