Ditzels
This article collects ditzels, which are, in the context of pathology, little specimens that are typically one or two slides and usually of little interest.[1]
The challenge in ditzels is not falling asleep... so one misses the unexpected (subtle) tumour.
The big table of ditzels
Gastrointestinal pathology
Hernia sac
- Inguinal hernia redirects here.
General
- Hernia repair (herniorrhaphy).
- Pathologic findings are very unusual and if present known to the surgeon.
Microscopic
Features:
- Fibrous tissue.
- +/-Adipose tissue.
- +/-Mesothelial cells.
Notes:
- One should not see vas deferens.
- Things worthy of some comment: granulation tissue, inflammation.
Sign out
Incarcerated without mesothelium
SOFT TISSUE ("HERNIA SAC"), RESECTION/HERNIA REPAIR:
- FIBROADIPOSE TISSUE WITH FAT NECROSIS -- CONSISTENT WITH HERNIA SAC.
- NEGATIVE FOR MALIGNANCY.
Micro
The sections show fibrofatty tissue with hemosiderin-laden macrophages, plump activated fibroblasts with pale staining nuclei, histiocytes with small nuclei and abundant grey vacuolated cytoplasm, fat necrosis and focal necrosis of the fibrous tissue.
Mesothelial lining present
Submitted as "Hernia Sac", Excision: - Benign fibroadipose tissue partially covered by mesothelium, consistent with hernia sac. - NEGATIVE for malignancy.
Block letters
SOFT TISSUE ("HERNIA SAC"), RESECTION/HERNIA REPAIR:
- FIBROADIPOSE TISSUE PARTIALLY COVERED BY MESOTHELIUM -- CONSISTENT WITH HERNIA SAC.
- NEGATIVE FOR MALIGNANCY.
Inflamed
SOFT TISSUE ("HERNIA SAC"), LEFT, RESECTION/HERNIA REPAIR:
- FIBROADIPOSE TISSUE PARTIALLY COVERED BY MESOTHELIUM WITH FOCAL CHRONIC
INFLAMMATION AND REACTIVE CHANGES -- CONSISTENT WITH HERNIA SAC.
- NEGATIVE FOR MALIGNANCY.
Gross only
SOFT TISSUE, RIGHT INGUINAL, HERNIA REPAIR: - HERNIA SAC (GROSS ONLY).
SOFT TISSUE, LEFT INGUINAL, HERNIA REPAIR: - HERNIA SAC (GROSS ONLY).
Stoma
- Ostomy, ileostomy and colostomy redirect here.
General
- See: Colon and Small intestine.
- Reversal of ileostomy or colostomy.
- The (generic) encompassing term for ileostomy and colostomy is ostomy.[4]
Stomas are created for a number of reasons:
- Perforated viscous/peritonitis.
- Trauma.
- Colorectal adenocarcinoma.
- Diverticulosis.
Microscopic
Features:
- Colonic-type or small intestinal-type bowel wall.
- Lymphoid hyperplasia (abundant lymphocytes) - very common.
- +/-Fibromuscular hyperplasia of the lamina propria and submucosa.
- Skin.
- Typically has findings of mild irritation:
- Mild dermal inflammation (usu. lymphocyte predominant).
- Acanthosis (thickened stratum spinosum).
- Hypergranulosis (thickened stratum granulosum).
- Hyperkeratosis (thickened stratum corneum).
- Typically has findings of mild irritation:
Notes:
- One is looking for malignancy (e.g. colorectal carcinoma), especially if that is in the history.
DDx:
Sign out
Colostomy
COLOSTOMY, COLOSTOMY REVERSAL: - LARGE BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. - SKIN WITHOUT SIGNIFICANT PATHOLOGY. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Ileostomy
Submitted as "Ileostomy", Excision: - Small bowel with submucosal fibrosis, otherwise within normal limits. - Skin without significant pathology. - NEGATIVE for dysplasia and NEGATIVE for malignancy.
Block letters
ILEOSTOMY, ILEOSTOMY REVERSAL: - SMALL BOWEL WALL WITH SUBMUCOSAL FIBROSIS -- OTHERWISE WITHIN NORMAL LIMITS. - SKIN WITHOUT SIGNIFICANT PATHOLOGY. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY.
Vagus nerve
General
- Seen from vagotomy.
Typical indication:
- Gastric outlet obstruction.[5]
Notes:
- Left vagus nerve -> anterior vagal trunk.
- Right vagus nerve -> posterior vagal trunk.
Microscopic
Features:
- Peripheral nerve.
DDx:
- Smooth muscle.
IHC
- S-100 +ve.
- Desmin -ve.
Sign out
A. VAGUS NERVE, POSTERIOR, VAGOTOMY: - PERIPHERAL NERVE WITHIN NORMAL LIMITS. B. VAGUS NERVE, ANTERIOR, VAGOTOMY: - SMOOTH MUSCLE WITHIN NORMAL LIMITS. - PERIPHERAL NERVE NOT IDENTIFIED, SEE COMMENT. COMMENT: The tissue was stained with desmin and S-100; it is positive for desmin. S-100 marks only small nerves fibres that innervate the muscle.
Pediatric
Bands of Ladd
General
- Associated with intestinal malrotation.
- Removed by Ladd's procedure.
- Usually associated with duodenal and (other) small bowel obstructions.[6]
Microscopic
Features:
- Benign fibrous tissue.
Sign out
Adhesive band, Ladd's procedure: - Vascular fibrous tissue consistent with bands of Ladd.
Cholesteatoma
General
- Squamous epithelium in the middle ear - leading to accumulation of keratinaceous debris.[7]
- The etiology is not well understood.[10][11]
- Theories include migration/hyperplasia, and metaplasia.[11]
- Rarely transforms into squamous cell carcinoma.[12][13]
Classification
May be subdivided into:[10]
- Acquired - due to trauma, surgery or infection.
- Congenital.
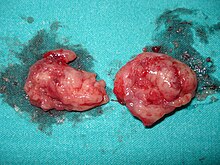
Gross
- Whitish mass in the middle ear.[14]
Image:
Microscopic
Features:[15]
- Keratinaceous debris - key feature.
- Squamous epithelium.
- Macrophages +/- giant cell (containing keratinceous debris).
- Chronic inflammation (lymphocytes).
DDx:
- Cholesterol granuloma.[16]
- Squamous cell carcinoma.[12]
Sign out
SOFT TISSUE (CHOLESTEATOMA), SITE NOT FURTHER SPECIFIED, REMOVAL: - KERATINACEOUS DEBRIS, COMPATIBLE WITH CHOLESTEATOMA.
Soft tissue, left ear ("left ear keratosis"), excision:
- Keratinaceous debris, squamous epithelium and bone (consistent with cholesteatoma).
TISSUE ("CHOLESTEATOMA"), LEFT, REMOVAL:
- KERATINACEOUS DEBRIS AND GIANT CELLS, COMPATIBLE WITH CHOLESTEATOMA.
Genitourinary pathology
Foreskin
General
Indications:
Main considerations:
- Squamous cell carcinoma.
- Lichen sclerosus, AKA balanitis xerotica obliterans.
- Lichen planus.
- Infection, e.g. syphilis, candidiasis.
- Zoon balanitis - abundant plasma cells.
Microscopic
Features:
- Usu. fibrotic dermis.
- +/-Inflammation.
DDx:
- See Penis.
Sign out
Foreskin, Circumcision: - Benign squamous mucosa within normal limits, consistent with foreskin.
Paraurethral cyst
General
- Rare.
- Benign.
Clinical:[17]
- Presentation: mass lesion, dyspareunia or dysuria.
- Multipareous.
Microscopic
Features:
- Cystic space with epithelial lining - diagnosis based on epithelial lining.
- Epithelial inclusion cyst.
- Müllerian cyst.
- Gartner duct cyst (AKA mesonephric duct cyst AKA Wolffian duct cyst).[20]
- Skene duct cyst.
Labia
General
- Operation labioplasty.
Microscopic
Features:
- Squamous epithelium with compact keratin.
- Fibrous stroma.
Sign out
LABIA MINORA, RIGHT, LABIOPLASTY: - BENIGN SKIN WITH A THIN LAYER OF COMPACT KERATIN FIBROTIC STROMA -- CONSISTENT WITH LABIA MINORA.
Head and neck pathology
Tonsillitis
General
- Commonly removed (tonsillectomy) when enlarged.
- Very low probability of malignancy (<0.2%) in tonsilectomies in individuals <19 years old if no clinical suspicion.[21]
Gross
- Symmetrical and equal size.
Note:
- Gross exam is considered sufficient if there is no asymmetry.[22]
Microscopic
Features:
- Follicular hyperplasia - see lymph node pathology.
- +/-Colonies (clusters) of actinomycetes in the tonsillar crypts.
DDx:
IHC
If there is a clinical suspicion - a panel to exclude (small cell) non-Hodgkin lymphomas:
- CD3.
- CD20.
- CD5.
- CD10.
- CD23.
- Cyclin D1.
Sign out
A. TONSIL, LEFT, TONSILLECTOMY: - REACTIVE FOLLICULAR HYPERPLASIA. - REACTIVE SQUAMOUS MUCOSA. B. TONSIL, RIGHT, TONSILLECTOMY: - REACTIVE FOLLICULAR HYPERPLASIA. - REACTIVE SQUAMOUS MUCOSA.
Without squamous mucosa
A. TONSIL, LEFT, TONSILLECTOMY: - REACTIVE FOLLICULAR HYPERPLASIA. B. TONSIL, RIGHT, TONSILLECTOMY: - REACTIVE FOLLICULAR HYPERPLASIA.
Obstructive sleep apnea
- Uvula redirects here.
- Abbreviated OSA.
General
Microscopic
Features:
- Benign oropharyneal mucosa (stratified squamous epithelium).
- +/-Skeletal muscle.
- +/-Salivary glands (minor) - mucinous.
Sign out
UVULA, RESECTION: - OROPHARYNGEAL MUCOSA, CONSISTENT WITH UVULA.
Cardiovascular pathology
Vascular thrombus
- Venous thrombus and arterial thrombus redirect here.
General
- Uncommonly comes to pathology.
Risk factors - think Virchow's triad:
- Stasis, e.g. atrial fibrillation.
- Hypercoagulable states, e.g. cancer - see risks factors venous thromboembolism.
- Endothelial injury.
Gross
- See pulmonary embolism.
Features:
- Dull appearance.
- Laminations.
Microscopic
Features:
- Layers consisting of platelets and fibrin.
- Classically alternating with layers of RBCs - known as Lines of Zahn.[26]
Note:
- Multiple laminations (layers), in general, suggest that clot was formed in a dynamic environment, i.e. in the context of blood flow.
DDx:
- Tumour embolus - malignant cells.
- Thromboembolus - may require clinical history.
- Fat embolism.
- Amniotic fluid embolus - in the context of pregnancy/postpartum.
- Foreign body.
Images:
- www:
- WC:
Sign out
BLOOD CLOT, LEFT ILIAC ARTERY, THROMBECTOMY: - THROMBUS. - NEGATIVE FOR MALIGNANCY.
BLOOD CLOT, LEFT ARM - BRACHIAL ARTERY, THROMBECTOMY/EMBOLECTOMY: - THROMBUS. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show layers of red blood cells alternating with fibrin and white blood cells (Lines of Zahn).
Leg amputation
Toe amputation
General - overview
- Like leg ampuations.
Sign out
Finger amputation
General - overview
- Similar to toe amputations.
May be done due to:
- Contractures leading to ulcerations.
- Scleroderma - leading to ischemia.[27]
Sign out
Atherosclerotic peripheral vascular disease
- Diabetic foot redirects here.
- AKA peripheral vascular disease.
General
- Very strong association with diabetes mellitus.
Gross
- +/-Ulceration.
- +/-Gangrene - black skin - subclassified:
- "Wet" = moist/oozing fluid.
- "Dry" = shriveled, no moisture apparent.
- +/-Loss of hair.
DDx - gross:
Image:
Sections - grossing:
- Resection margin (check for viability).
- Gangrenous area.
- Blood vessels.
- Bone (check for osteomyelitis).
Microscopic
Features:
- Atherosclerosis.
- Coagulative necrosis (gangrene).
- Inflammation (wet gangrene).
- Neutrophils.
- Lymphocytes.
- Plasma cells.
- +/-Thrombosis.
- +/-Chronic osteomyelitis.
- +/-Reactive fibroblasts.
Note:
- Ischemia may be associated with marked nuclear changes. Uninitiated eyes may think they are seeing a sarcoma.
DDx:
- Vasculitis associated with a connective tissue disorder.
- Drug use, e.g. cocaine.[28]
- Chronic osteomyelitis.
- Cholesterol embolism.
Sign out
Forefoot amputation
RIGHT FOREFOOT, AMPUTATION: - ULCERATED SKIN. - MODERATE-TO-SEVERE ATHEROSCLEROSIS. - BLOOD VESSEL WITH RECANALIZATION. - NEGATIVE FOR MALIGNANCY.
Leg amputation
LEFT LEG, BELOW KNEE AMPUTATION: - MODERATE-TO-SEVERE ATHEROSCLEROSIS. - COAGULATIVE NECROSIS OF SOFT TISSUE. - NECROTIC BONE. - MARROW CAVITY FIBROSIS WITH SIDEROPHAGES. - RESECTION MARGIN WITH VIABLE TISSUE.
Revision
SKIN AND SOFT TISSUE, RIGHT UPPER LEG, REVISION OF AMPUTATION: - ULCERATED SKIN WITH NECROTIC SOFT TISSUE WITH IMPETIGINIZATION, AND MICROABSCESS FORMATION. - SEVERE ATHEROSCLEROSIS. - NEGATIVE FOR MALIGNANCY.
Leg amputation - gross only
LOWER EXTREMITY, LEFT, BELOW THE KNEE AMPUTATION: - ULCERS AND ISCHEMIC CHANGES WITH FOCAL COMPLETE ARTERIAL OCCLUSION (GROSS ONLY).
LEG, RIGHT, ABOVE THE KNEE AMPUTATION: - ULCERS AND ISCHEMIC CHANGES WITH EXTENSIVE ARTERIAL DISEASE (GROSS ONLY).
LEG, RIGHT, ABOVE THE KNEE AMPUTATION: - EXTENSIVE ISCHEMIC CHANGES WITH SEVERE ARTERIAL DISEASE (GROSS ONLY).
Toe amputation
Mild
THIRD TOE, RIGHT, AMPUTATION: - SKIN WITH MARKED DERMAL FIBROSIS. - MILD ATHEROSCLEROSIS. - NEGATIVE FOR MALIGNANCY.
SECOND TOE, RIGHT, AMPUTATION: - SKIN WITH MARKED DERMAL FIBROSIS AND ULCERATION WITH IMPETIGINIZATION. - MILD ATHEROSCLEROSIS. - NEGATIVE FOR MALIGNANCY.
Moderate
SECOND TOE, LEFT, AMPUTATION: - MODERATE ATHEROSCLEROSIS. - BONE WITH A FATTY BONE MARROW CAVITY WITH FOCAL FAT NECROSIS AND RARE PLASMA CELLS. - SKIN WITH FIBROUS DERMIS AND A NON-SPECIFIC DERMAL PERIVASCULAR LYMPHOPLASMACYTIC INFILTRATE.
SECOND TOE, LEFT, AMPUTATION: - MODERATE ATHEROSCLEROSIS. - BONE WITH A FATTY BONE MARROW CAVITY WITH FOCAL FAT NECROSIS AND RARE PLASMA CELLS. - SKIN WITH FIBROUS DERMIS AND NON-SPECIFIC PERIVASCULAR LYMPHOPLASMACYTIC DERMAL INFILTRATE.
Severe
SECOND AND THIRD TOE, LEFT, AMPUTATION: - SEVERE ATHEROSCLEROSIS. - ACUTE AND CHRONIC OSTEOMYELITIS. - GANGRENE.
GREAT TOE, LEFT, AMPUTATION: - GANGRENE. - SEVERE ATHEROSCLEROSIS. - ULCERATED SKIN AND CHRONIC ISCHEMIC CHANGES. - BONE WITH NO SIGNIFICANT PATHOLOGY. - NEGATIVE FOR MALIGNANCY.
GREAT TOE, RIGHT, AMPUTATION: - GANGRENE. - ATHEROSCLEROSIS. - NECROTIC BONE WITH ABUNDANT COCCI ORGANISMS AND NEUTROPHILS WITHIN THE MARROW CAVITY. - NEGATIVE FOR MALIGNANCY.
Orthopaedic
Femoral head
Bone reamings
General
- Taken during the surgical repair of a fracture, e.g. intramedullary nail placement.
- Done to rule-out a pathologic fracture; considered reliable for detecting malignancy.[29]
- Hassan et al.[30] advocate against their use, suggesting the yield is low and a biopsy should be preferred.
Microscopic
Features:[31]
- Fragments of bone (scattered trabeculae).
- Necrotic bone = bone with empty lacunae, i.e. lacunae missing osteocytes.
- Bone marrow.
- Megakaryocytes - large cells, multinucleated, eosinophilic cytoplasm.
- Nucleated RBCs - perfectly round, dense nucleus, bright red cytoplasm.
- Myeloid cells and precursors.
- Adipocytes.
DDx:
- Metastatic carcinoma.
Sign out
BONE, LEFT FEMUR, REAMINGS: - FEATURES CONSISTENT WITH A RECENT FRACTURE. - NEGATIVE FOR MALIGNANCY.
Heterotopic ossification
- Abbreviated HO.
General
- Definition of heterotopic ossification: bone formation in soft tissue.[32]
- Injury at site.
- May be seen in the context of tetraplegia.
Clinical:[32]
- +/-Joint stiffness.
- +/-Swelling.
- +/-Pain.
Microscopic
Features:
- Lamellar bone - has layering/lines (best seen with polarized light).
- +/-Skeletal muscle (within the marrow space).
DDx:
- Myositis ossificans - inflammation, cellular.
- Osteosarcoma, extraskeletal.
- Osteochrondroma - at joint, has cartilage.[citation needed]
Sign out
Lesion, Distal Phalanx of Right Little Finger, Excision: - Dermal ossification without cartilage in benign skin with a thick keratin layer. - NEGATIVE for evidence of malignancy.
Block letters
LESION ("HETEROTOPIC OSSIFICATION"), RIGHT FEMUR, EXCISION:
- BONE -- CONSISTENT WITH MUSCLE HETEROTOPIC OSSIFICATION.
- NEGATIVE FOR MALIGNANCY.
Micro
The sections show laminar bone with a marrow space containing adipose tissue and benign skeletal muscle. The osteocytes show no nuclear atypia. No mitotic activity is appreciated.
Lumbar bone
General
- May be seen in the context of laminectomies to treat cauda equina syndrome.
Microscopic
Features:
- Degenerative fibrocartilage:
- Multiple chondrocytes in one pocket (lacuna) - regenerative change.
- Degenerative cartilage.
- Non-vital bone:
- Empty lacuna.
DDx:
- Occult malignancy.
Sign out
LUMBAR BONE, DECOMPRESSION: - BONE AND VERTEBRAL DISC FRAGMENTS WITH DEGENERATIVE CHANGES. - UNREMARKABLE BONE MARROW. - NEGATIVE FOR MALIGNANCY.
Bursa
- Bursitis redirects here.
General
- Uncommon specimen.
- Septic bursitis is usually due to S. aureus.[33]
- Usually associated with trauma to the overlying skin.[34]
Indication:
- Bursitis - may be treated with bursectomy.[35]
Note:
- Most bursitis is managed conservatively.[36]
Microscopic
Features:
- Dense connective tissue.
- Fibroadipose tissue.
Sign out
No apparent inflammation
BURSA, RIGHT HIP, BURSECTOMY: - BENIGN DENSE CONNECTIVE TISSUE WITH CALCIFICATIONS, AND FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
BURSA, LEFT TROCHANTERIC, BURSECTOMY: - BENIGN DENSE CONNECTIVE TISSUE AND BENIGN FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NEGATIVE FOR MALIGNANCY.
Rotator cuff tear
General
- Surgically repaired.
- Clinical diagnosis.
Microscopic
Features:[37]
- Collagen degeneration.
- Disordered arrangement of collagen fibres.
- Wavy fibres.
- Separation of the fibres.
- +/-Inflammation - associated with smaller tears.
- +/-Decreased cellularity - associated with larger tears.
- +/-Fatty replacement.[38]
Sign out
RIGHT SHOULDER ACROMIOM AND BURSAE, EXCISION: - UNREMARKABLE BONE (GROSS ONLY). - BENIGN SOFT TISSUE.
"BURSA AND ACROMION", LEFT SHOULDER, ROTATOR CUFF REPAIR: - BENIGN DENSE CONNECTIVE TISSUE AND BENIGN FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NO BONE IDENTIFIED. - NEGATIVE FOR MALIGNANCY.
"BURSA AND ACROMION", LEFT SHOULDER, ROTATOR CUFF REPAIR: - BENIGN DENSE WAVY CONNECTIVE TISSUE WITH FIBRE SEPARATION. - BENIGN FIBROADIPOSE TISSUE. - NO SIGNIFICANT INFLAMMATION. - NO BONE IDENTIFIED. - NEGATIVE FOR MALIGNANCY.
Other
Breast prosthesis
- This also deals with breast implants.
De Quervain syndrome
- Should not be confused with De Quervain's thyroiditis (subacute granulomatous thryoiditis).
- AKA de Quervain disease.
General
- Benign.
- Clinical diagnosis.[39]
Clinical:
- Pain.
Treatment:[39]
- Steroid.
- Surgery.
Microscopic
Features:
- Dense connective tissue consistent with tendon.
Sign out
FIRST EXTENSOR COMPARTMENT, RIGHT HAND, BIOPSY: - DENSE CONNECTIVE TISSUE CONSISTENT WITH TENDON. - FIBROUS TISSUE.
Tenosynovitis
Otosclerosis
- Stapes redirects here.
General
- Clinical diagnosis.
- Causes conductive hearing loss.[40]
- Etiology - genetic.
Treatment:
- Stapedectomy (removal of the stapes).[43]
Microscopic
Features (temporal bone):[44]
- Classically divided into four phases:
- Osteoclastic phase:
- Large spaces form in bone marrow.
- Replacement phase:
- Bone replaced by basophilic web-like tissue.
- Fibril phase:
- Fibrils deposited.
- Lamellar phase:
- Lamellar bone forms around the blood vessels.
- Osteoclastic phase:
Features - (stapes):
- Unremarkable bone.[citation needed]
DDx:
- Avascular necrosis ~ 25% of cases diagnosed as otosclerosis.[44]
- May be due to fat embolism.
Note:
- Avascular necrosis of the stapes crura and otosclerosis together is considered rare.[45]
Images:
Sign out
STAPES, RIGHT, STAPEDECTOMY: - BENIGN BONE CONSISTENT WITH STAPES.
STAPES, RIGHT, STAPEDECTOMY: - UNREMARKABLE BONE CONSISTENT WITH STAPES.
Missed stapes
STAPES, RIGHT, STAPEDECTOMY: - BENIGN FIBROFATTY TISSUE. - NO BONE IDENTIFIED.
External links
Abdominal pannus
- Pannus redirects here.
General
Gross
- Skin with abundant fat.
- Pieces usually triangular.
- Stretch marks (striae) are very common.
Notes:
- The gross pathology section of the report should say something like: On sectioning no lesions were identified.
- The cut-up is described in abdominal pannus grossing.
Microscopic
Features:
- Adipose tissue.
DDx:
Sign out
ABDOMINAL PANNUS, EXCISION: - BENIGN SKIN AND ADIPOSE TISSUE.
ABDOMINAL PANNUS, EXCISION: - DERMAL SCAR, BENIGN SKIN AND ADIPOSE TISSUE.
Gross only
ABDOMINAL PANNUS, EXCISION: - BENIGN SKIN AND ADIPOSE TISSUE (GROSS ONLY).
Empyema
- Empyema peel redirects here.
General
- Empyemas are often managed surgically.[47]
- Classically, divided into three stages.[48][49]
- I - exudative stage (acute).
- II - fibropurulent stage (acute).
- III - organizational stage (chronic).
Etiologies - common:
- Pneumonia - most common.
- Iatrogenic.
- Trauma.
Microscopic
Features:
- Neutrophils (pus) - key feature.
- Lymphocytes.
- Plasma cells.
- Reactive fibroblasts.
- Reactive mesothelial cells - not common.
DDx:
Sign out
PLEURA, LEFT, DECORTICATION: - MIXED INFLAMMATORY INFILTRATE WITH ABUNDANT NEUTROPHILS. - REACTIVE FIBROBLASTS AND FIBRIN. - NO MICROORGANISMS APPARENT WITH H&E STAINING. - NEGATIVE FOR MALIGNANCY.
Not labelled as a peel
Left Lung, Biopsy: - Fibrin, neutrophils, necrotic tissue and a fibroblastic response, compatible with empyema peel. - NO viable lung parenchyma identified. - NEGATIVE for evidence of malignancy.
Toenail
General
- Relatively common.
Indications for removal:
- Ingrown[50] - typically great toe.[51]
- Onychomycosis - fungal infection.[52]
- Pigmented lesion.
- Exclude melanoma.[53]
Microscopic
Features:
- Nail plate - paucicellular, dense connective tissue.
- Keratinized squamous epithelium.
- +/-Cocci organisms.
DDx:
- Malignant melanoma.
- Trauma.
- Fungal infection (candidiasis).
- Bacteria infection, e.g. Pseudomonas (causes green nails).
Stains
For pigmented lesion:
- Prussian blue stain - trauma +ve, melanocytic lesion -ve.
- Fontana-Masson stain - trauma -ve, melanocytic lesion usu. +ve.
Query fungal infection:
Sign out
Pigmented nail
PARTIAL NAIL PLATE, RIGHT THIRD TOE, SCISSOR EXCISION: - NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM WITH PARAKERATOSIS AND FIBRIN. - NO APPARENT PIGMENT. - NO EVIDENCE OF MALIGNANCY.
Micro
The sections show a paucicellular nail plate, and a thin layer of squamous epithelium with keratinization and partial retention of the nuclei (parakeratosis). There is also a small amount of fibrin. No pigmentation is apparent with Prussian blue and Fontana-Masson staining. No melanocytes are apparent. No nuclear atypia is apparent. No mitotic activity is identified. No microorganisms are apparent. No significant inflammation is apparent.
Query infection
GREAT TOENAIL, RIGHT, EXCISION: - NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM. - SMALL CLUSTERS OF COCCI, FOCAL. - NO APPARENT FUNGAL ORGANISMS WITH PASF STAIN. - NO EVIDENCE OF MALIGNANCY.
Fungal organisms present
GREAT TOE NAIL, RIGHT, REMOVAL: - NAIL PLATE AND THIN LAYER OF KERATINIZED SQUAMOUS EPITHELIUM WITH PARAKERATOSIS AND SCANT SUBEPITHELIAL TISSUE. - FUNGAL ORGANISMS CONSISTENT WITH CANDIDA, DEMONSTRATED WITH PASF STAIN. - SMALL CLUSTERS OF COCCI, FOCAL. - NO EVIDENCE OF MALIGNANCY.
See also
References
- ↑ Weedman Molavi, Diana (2008). The Practice of Surgical Pathology: A Beginner's Guide to the Diagnostic Process (1st ed.). Springer. pp. 37. ISBN 978-0387744858.
- ↑ Siddiqui K, Nazir Z, Ali SS, Pervaiz S (February 2004). "Is routine histological evaluation of pediatric hernial sac necessary?". Pediatr. Surg. Int. 20 (2): 133–5. doi:10.1007/s00383-003-1106-2. PMID 14986035.
- ↑ Partrick DA, Bensard DD, Karrer FM, Ruyle SZ (July 1998). "Is routine pathological evaluation of pediatric hernia sacs justified?". J. Pediatr. Surg. 33 (7): 1090–2; discussion 1093–4. PMID 9694100.
- ↑ URL: http://www.nlm.nih.gov/medlineplus/ostomy.html. Accessed on: 27 January 2013.
- ↑ Okawada, M.; Okazaki, T.; Takahashi, T.; Lane, GJ.; Yamataka, A. (2009). "Gastric outlet obstruction possibly secondary to ulceration in a 2-year-old girl: a case report.". Cases J 2 (1): 8. doi:10.1186/1757-1626-2-8. PMID 19123936.
- ↑ Raphaeli, T.; Parimi, C.; Mattix, K.; Javid, PJ. (Mar 2010). "Acute colonic obstruction from Ladd bands: a unique complication from intestinal malrotation.". J Pediatr Surg 45 (3): 630-1. doi:10.1016/j.jpedsurg.2009.12.026. PMID 20223332.
- ↑ URL: http://www.harrisonspractice.com/practice/ub/view/Harrisons%20Practice/141015/all/otitis_media_and_mastoiditis. Accessed on: 16 March 2011.
- ↑ Piepergerdes MC, Kramer BM, Behnke EE (March 1980). "Keratosis obturans and external auditory canal cholesteatoma". Laryngoscope 90 (3): 383–91. PMID 7359960.
- ↑ Shire JR, Donegan JO (September 1986). "Cholesteatoma of the external auditory canal and keratosis obturans". Am J Otol 7 (5): 361–4. PMID 3538893.
- ↑ 10.0 10.1 Nevoux, J.; Lenoir, M.; Roger, G.; Denoyelle, F.; Ducou Le Pointe, H.; Garabédian, EN. (Sep 2010). "Childhood cholesteatoma.". Eur Ann Otorhinolaryngol Head Neck Dis 127 (4): 143-50. doi:10.1016/j.anorl.2010.07.001. PMID 20860924.
- ↑ 11.0 11.1 Louw, L. (Jun 2010). "Acquired cholesteatoma pathogenesis: stepwise explanations.". J Laryngol Otol 124 (6): 587-93. doi:10.1017/S0022215109992763. PMID 20156369.
- ↑ 12.0 12.1 Rothschild, S.; Ciernik, IF.; Hartmann, M.; Schuknecht, B.; Lütolf, UM.; Huber, AM.. "Cholesteatoma triggering squamous cell carcinoma: case report and literature review of a rare tumor.". Am J Otolaryngol 30 (4): 256-60. doi:10.1016/j.amjoto.2008.06.011. PMID 19563937.
- ↑ Takahashi, K.; Yamamoto, Y.; Sato, K.; Sato, Y.; Takahashi, S. (Jan 2005). "Middle ear carcinoma originating from a primary acquired cholesteatoma: a case report.". Otol Neurotol 26 (1): 105-8. PMID 15699729.
- ↑ Al Balushi, T.; Naik, JZ.; Al Khabori, M. (Jan 2013). "Congenital cholesteatoma in identical twins.". J Laryngol Otol 127 (1): 67-9. doi:10.1017/S0022215112002757. PMID 23217274.
- ↑ Iino Y, Toriyama M, Ohmi S, Kanegasaki S (1990). "Activation of peritoneal macrophages with human cholesteatoma debris and alpha-keratin". Acta Otolaryngol. 109 (5-6): 444–9. PMID 1694387.
- ↑ URL: http://path.upmc.edu/cases/case273/dx.html. Accessed on: 14 January 2012.
- ↑ Isen, K.; Utku, V.; Atilgan, I.; Kutun, Y. (Aug 2008). "Experience with the diagnosis and management of paraurethral cysts in adult women.". Can J Urol 15 (4): 4169-73. PMID 18706145.
- ↑ Satani, H.; Yoshimura, N.; Hayashi, N.; Arima, K.; Yanagawa, M.; Kawamura, J. (Mar 2000). "[A case of female paraurethral cyst diagnosed as epithelial inclusion cyst].". Hinyokika Kiyo 46 (3): 205-7. PMID 10806582.
- ↑ Das, SP. (Jul 1981). "Paraurethral cysts in women.". J Urol 126 (1): 41-3. PMID 7195943.
- ↑ URL: http://webpathology.com/image.asp?n=3&Case=540. Accessed on: 5 February 2012.
- ↑ Erdag, TK.; Ecevit, MC.; Guneri, EA.; Dogan, E.; Ikiz, AO.; Sutay, S. (Oct 2005). "Pathologic evaluation of routine tonsillectomy and adenoidectomy specimens in the pediatric population: is it really necessary?". Int J Pediatr Otorhinolaryngol 69 (10): 1321-5. doi:10.1016/j.ijporl.2005.05.005. PMID 15963574.
- ↑ Williams, MD.; Brown, HM. (Oct 2003). "The adequacy of gross pathological examination of routine tonsils and adenoids in patients 21 years old and younger.". Hum Pathol 34 (10): 1053-7. PMID 14608541.
- ↑ Wang, XY.; Wu, N.; Zhu, Z.; Zhao, YF. (May 2010). "Computed tomography features of enlarged tonsils as a first symptom of non-Hodgkin's lymphoma.". Chin J Cancer 29 (5): 556-60. PMID 20426908.
- ↑ Shin, SH.; Ye, MK.; Kim, CG. (Jun 2009). "Modified uvulopalatopharyngoplasty for the treatment of obstructive sleep apnea-hypopnea syndrome: resection of the musculus uvulae.". Otolaryngol Head Neck Surg 140 (6): 924-9. doi:10.1016/j.otohns.2009.01.020. PMID 19467416.
- ↑ Sarkhosh, K.; Switzer, NJ.; El-Hadi, M.; Birch, DW.; Shi, X.; Karmali, S. (Jan 2013). "The Impact of Bariatric Surgery on Obstructive Sleep Apnea: A Systematic Review.". Obes Surg. doi:10.1007/s11695-012-0862-2. PMID 23299507.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 124. ISBN 978-1416031215.
- ↑ Jones, NF.; Imbriglia, JE.; Steen, VD.; Medsger, TA. (May 1987). "Surgery for scleroderma of the hand.". J Hand Surg Am 12 (3): 391-400. PMID 3584887.
- ↑ Dhawan, SS.; Wang, BW. (Feb 2007). "Four-extremity gangrene associated with crack cocaine abuse.". Ann Emerg Med 49 (2): 186-9. doi:10.1016/j.annemergmed.2006.08.001. PMID 17059855.
- ↑ Clarke, AM.; Rogers, S.; Douglas, DL. (Dec 1993). "Closed intramedullary biopsy for metastatic disease.". J R Coll Surg Edinb 38 (6): 368-9. PMID 7509409.
- ↑ Hassan, K.; Kalra, S.; Moran, C. (Aug 2007). "Intramedullary reamings for the histological diagnosis of suspected pathological fractures.". Surgeon 5 (4): 202-4. PMID 17849954.
- ↑ Tydings, JD.; Martino, LJ.; Kircher, M.; Alfred, RH.; Lozman, J. (Mar 1987). "Viability of intramedullary canal bone reamings for continued calcification.". Am J Surg 153 (3): 306-9. PMID 3548454.
- ↑ 32.0 32.1 Leblanc, E.; Trensz, F.; Haroun, S.; Drouin, G.; Bergeron, E.; Penton, CM.; Montanaro, F.; Roux, S. et al. (Jun 2011). "BMP-9-induced muscle heterotopic ossification requires changes to the skeletal muscle microenvironment.". J Bone Miner Res 26 (6): 1166-77. doi:10.1002/jbmr.311. PMID 21611960.
- ↑ Hanrahan, JA. (Oct 2013). "Recent developments in septic bursitis.". Curr Infect Dis Rep 15 (5): 421-5. doi:10.1007/s11908-013-0353-1. PMID 23933823.
- ↑ Canoso, JJ.; Sheckman, PR.. "Septic subcutaneous bursitis. Report of sixteen cases.". J Rheumatol 6 (1): 96-102. PMID 439118.
- ↑ Dillon, JP.; Freedman, I.; Tan, JS.; Mitchell, D.; English, S. (Jul 2012). "Endoscopic bursectomy for the treatment of septic pre-patellar bursitis: a case series.". Arch Orthop Trauma Surg 132 (7): 921-5. doi:10.1007/s00402-012-1494-7. PMID 22426936.
- ↑ Lustenberger, DP.; Ng, VY.; Best, TM.; Ellis, TJ. (Sep 2011). "Efficacy of treatment of trochanteric bursitis: a systematic review.". Clin J Sport Med 21 (5): 447-53. doi:10.1097/JSM.0b013e318221299c. PMID 21814140.
- ↑ Longo, UG.; Berton, A.; Khan, WS.; Maffulli, N.; Denaro, V. (Sep 2011). "Histopathology of rotator cuff tears.". Sports Med Arthrosc 19 (3): 227-36. doi:10.1097/JSA.0b013e318213bccb. PMID 21822106.
- ↑ Kuzel, BR.; Grindel, S.; Papandrea, R.; Ziegler, D. (Oct 2013). "Fatty infiltration and rotator cuff atrophy.". J Am Acad Orthop Surg 21 (10): 613-23. doi:10.5435/JAAOS-21-10-613. PMID 24084435.
- ↑ 39.0 39.1 Ilyas, AM.; Ilyas, A.; Ast, M.; Schaffer, AA.; Thoder, J. (Dec 2007). "De quervain tenosynovitis of the wrist.". J Am Acad Orthop Surg 15 (12): 757-64. PMID 18063716.
- ↑ Declau, F.; van Spaendonck, M.; Timmermans, JP.; Michaels, L.; Liang, J.; Qiu, JP.; van de Heyning, P. (2007). "Prevalence of histologic otosclerosis: an unbiased temporal bone study in Caucasians.". Adv Otorhinolaryngol 65: 6-16. doi:10.1159/000098663. PMID 17245017.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 166800
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 605727
- ↑ Redfors, YD.; Gröndahl, HG.; Hellgren, J.; Lindfors, N.; Nilsson, I.; Möller, C. (Aug 2012). "Otosclerosis: anatomy and pathology in the temporal bone assessed by multi-slice and cone-beam CT.". Otol Neurotol 33 (6): 922-7. doi:10.1097/MAO.0b013e318259b38c. PMID 22771999.
- ↑ 44.0 44.1 "Otosclerosis.". Br Med J 1 (6105): 63-4. Jan 1978. PMC 1602666. PMID 620199. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1602666/.
- ↑ Erdoglija, M.; Sotirovic, J.; Jacimovic, V.; Vukomanovic, B. (2012). "Avascular necrosis of stapes crura in one case of operated otosclerosis.". Acta Medica (Hradec Kralove) 55 (4): 193-7. PMID 23631292.
- ↑ URL: http://plasticsurgery.about.com/od/glossary/g/panniculectomy.htm. Accessed on: 18 July 2012.
- ↑ Ferguson, MK. (Mar 1999). "Surgical management of intrapleural infections.". Semin Respir Infect 14 (1): 73-81. PMID 10197399.
- ↑ Shiraishi, Y. (Jul 2010). "Surgical treatment of chronic empyema.". Gen Thorac Cardiovasc Surg 58 (7): 311-6. doi:10.1007/s11748-010-0599-6. PMID 20628845.
- ↑ Hamm, H.; Light, RW. (May 1997). "Parapneumonic effusion and empyema.". Eur Respir J 10 (5): 1150-6. PMID 9163661. http://erj.ersjournals.com/content/10/5/1150.long.
- ↑ Küçüktaş, M.; Kutlubay, Z.; Yardimci, G.; Khatib, R.; Tüzün, Y. (Feb 2013). "Comparison of effectiveness of electrocautery and cryotherapy in partial matrixectomy after partial nail extraction in the treatment of ingrown nails.". Dermatol Surg 39 (2): 274-80. doi:10.1111/dsu.12068. PMID 23227941.
- ↑ Jia, C.; Li, P.; Wu, Y.; Qiu, Y.; Cao, L.; Chang, C.; Zhang, Y. (Jul 2013). "[Modified surgical repair of severe ingrown toenail].". Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 27 (7): 869-71. PMID 24063180.
- ↑ 52.0 52.1 Reisberger, EM.; Abels, C.; Landthaler, M.; Szeimies, RM. (Apr 2003). "Histopathological diagnosis of onychomycosis by periodic acid-Schiff-stained nail clippings.". Br J Dermatol 148 (4): 749-54. PMID 12752134.
- ↑ Fanti, PA.; Dika, E.; Misciali, C.; Vaccari, S.; Barisani, A.; Piraccini, BM.; Cavrin, G.; Maibach, HI. et al. (Jun 2013). "Nail apparatus melanoma: is trauma a coincidence? Is this peculiar tumor a real acral melanoma?". Cutan Ocul Toxicol 32 (2): 150-3. doi:10.3109/15569527.2012.740118. PMID 23153047.