Cytopathology
Cytopathology, often called cytology, is the study of pathologic changes in cells.
It is often divided into gynecologic and non-gynecologic. Gynecologic in this context usually refers to Pap test specimens, i.e. uterine cervix, vaginal vault; other gynecologic specimens are considered non-gynecologic.
Slide-marking conventions
Conventions are important for facilitating communication between various team members.
Common conventions:[1]
- The slide is placed with the label on the right hand side.
- "Marks-of-interest", e.g. dots, are place above the field of interest (when viewed through a microscope - that does not correct for image inversion).
- Microscopes used for surgical pathology, generally, do not correct for image inversion.
- The "marks-of-interest" appear below the field of interest when the slide is viewed with the naked eye.
- Microscopes used for surgical pathology, generally, do not correct for image inversion.
Marks-of-interest:
- Dot - region of interest.
- Inverted "V" - transformation zone (in cervical cytology specimen).
- Inverted "Y" - benign finding.
Notes:
- Image inversion in the microscope comes about as light travels in a straight line.
- Marks should draw attention to the best examples of the highest grade lesion present.
- More than 7 marks on slide is generally considered excessive.
Dictums of cytopathology
- Malignant cells are malignant because they have malignant features.
- Benign cells are benign because they lack malignant features and have benign features.
Corollaries:
- Cells lacking malignant features are not malignant.
- Cells lacking benign features are not malignant.
Cytologic features of malignancy
Cytologic features of malignancy:
- High nuclear-to-cytoplasmic ratio.
- Nuclear membrane irregularities.
- Notches/sharp discontinuities.
- Chromatin abnormalities.
- Clumped chromatin, esp. differences between quadrants of a nucleus.
- Chromatin clumping at the nuclear membrane (chromatin margination).
- Hyperchromatic nucleus (when compared to other cells).
- Nuclear pleomorphism (comparison of neighbouring cells).
- Def'n: variable staining, shape, and size.
Notes:
- Not all features of malignancy will be present in one cell.[2]
Cell types
WG's cell typing guide:[3]
| Cell type | Nucleus location | Nucleus shape | Cytoplasm | Chromatin | Nucleoli | Other | Architecture |
|---|---|---|---|---|---|---|---|
| Squamous | Center | Oval/Spindle | Solid/dense | Coarse | Absent | Squamous pearls, streaming | Streaming |
| Secretory/ glandular (adenocarcinoma) |
Eccentric | Oval | Vacuoles | Fine | Present | Columnar | Acini (glandular structures), (true) papillae |
| Neuroendocrine | Center (?) | Oval | Fine granules (neuroendocrine granules - seen on Romanowsky type stains) |
Reticulated "stippled" | Absent | Perinuclear blue bodies (not seen in lymphoid cells) |
Clusters, may appear dyscohesive |
| Lymphoid | Eccentric | Oval | Very scant, basophilic | Coarse | Usually absent | Lymphoglandular bodies, dyscohesive |
Single cells |
| Germ cell | Central/variable | Oval | Variable | Variable | (?), present in seminoma | Tigroid background in seminoma (Romanowsky stains) |
Usu. in clusters |
| Mesenchymal | Central | Spindle | (?) | Fine (?) | Absent | Variable | Clusters, streaming |
The big list of hole-y cells
- Large Golgi apparatus.
- May be seen in melanoma.
- Phagocytic vacuole
- Contains foreign material.
- Fat.
- Usually small.
- Glycogen.
- Mucin.
- Hydropic.
Notes:
- The last two are the most important.
Vacuoles
Hydropic vacuoles and secretory vacuoles:[4]
| Contents | Distorts nucleus | Significance | Classic description | |
|---|---|---|---|---|
| Hydropic vacuole | empty (clear) | less common | dying cell | diamond engagement ring |
| Secretory vacuole | "globs" of stuff (usu. pink) | more common | secretory cell/consider adenocarcinoma | signet ring |
Notes:
- Size the vacuole is not discriminative.[5]
- Nuclear distortion (by the vacuole) is probably the strongest indicator the vacuole is secretory.
Subtyping adenocarcinoma
Adenocarcinoma can be subtyped:[6]
| Architecture | Group borders | Group cellular/nuclear pleomorphism | Vacuoles (cytoplasmic) | Nucleoli | Other | |
|---|---|---|---|---|---|---|
| Serous carcinoma | Micropapillae | Knobby | Marked size variation, +/-second benign pop. | Hydropic | Large, red | Psammoma bodies |
| Gastric (signet ring) carcinoma | Single cells, groups | Community border (?) | Limited, cells uniform, +/-second benign pop. | Mucin | Usu. inconspicuous | - |
| Breast ductal carcinoma | Clusters (tubular) | Community border | Limited, cells uniform, +/-second benign pop. | Mucin | Inconspicuous/small | - |
| Adenocarcinoma not otherwise specified (NOS) | 3-D clusters | Community border | Limited, malignant cells uniform, +/-second benign pop. | Mucin | Inconspicuous/small | - |
| Mesothelioma (see Note 1) | Clusters (usu. large), single cells | Knobby border | Usu. uniform size, one cell population | Hydropic | Often large | Intercellular windows, cytoplasmic blebs |
Note 1:
- Mesothelioma is a type of carcinoma,[7] yet is not an adenocarcinoma; it is added to the table to make the point that it is similar to adenocarcinoma.
- Mesothelioma arises from the mesothelium, a type of epithelium. Carcinomas are epithelial derived malignant tumours (by definition).
Staining
There are two standard stains:
- Papanicolaou stain (Pap stain).
- Is a modified H&E stain.
- Done on alcohol-fixed material.
- Romanowsky stain.
- Many variants exist.
- Used on air-dried specimens; air-dried cells are much larger, it is easier to see the nuclear detail.
Processing:
- Carnoy's solution (ethanol, glacial acetic acid) - used to lyze RBCs to get rid of 'em.
Further details are in the main article on staining.
Notes:
- Jörundsson et al. compare the types of stains.[8]
- Romanowsky type staining is uncommon in the Canadian cytopathology community and not on FRCPC exams.
Pap stain
Interpretation:[9]
- Blue = nucleus, basophilic cytoplasm.
- Pink = cytoplasm.
- Orange = keratin.
DDx of orange:
- Keratin.
- Dying/dead cell.
- Center of cluster effect/diffusion effect.
- The center of large clumps of cells are often artifactually pink/orange, as the eosin (a small molecule) get there but the azure (a large molecule) does not.
Romanowsky stains
Variants:
- Diff-Quik.
- Field's stain.
- May-Grünwald-Giemsa.
- Wright stain.
Interpretation (Romanowsky stain):[10]
- Red - RBCs, eosinophil granules, neuroendocrine granules.[11]
- Blue (basophilic) - lymphocyte cytoplasm.
- Purple - nuclear chromatin, neutrophil granules, platelets.
Notes:
- May have air-drying artifact.
- Usually on slide periphery.
- Appearance: white holes.
- Air-drying may mimic the appearance of nuclear pseudoinclusions.
- Cells tend to be larger than on Pap stain.
Adequacy of specimens
Standards are lacking for most types of specimens. A generally accepted standard is established only for cervical cytology specimens.
Non-gynecologic
Standards at one large centre for non-gyne specimens:[12]
- Breast: >= 6 cell groups (6 cells/cluster).
- Thyroid: >= 20 cell cluster (20 cells/cluster).
- Urine: >=50 urothelial cells.
- Sputum: >= 10 pulmonary macrophages.
Gynecologic
There is a generally accepted standard for cervical (liquid-based) cytology specimens:[13]
- >5000 squamous cells/slide, if no abnormality is present.
- If abnormal cells are present, any number of cells is acceptable.
- This works-out to approx. 4 cells/HPF.
- Where: HPF = area seen at 400X with an eye piece diameter is ~22 mm.
- 10 HPFs are counted and a table is used to see whether the sample is adequate.
- This works-out to approx. 4 cells/HPF.
- If abnormal cells are present, any number of cells is acceptable.
Note:
- The standard for conventional pap smears is: 8000-12000 squamous cells/slide.[14]
Transformation zone (TZ)
The presence of the TZ should be commented on:[15]
- An adequate TZ is 10 cells - endocervical cells or squamous metaplastic cells (per Bethesda).
Difficulties in obtaining a TZ may arise in the following populations:
- Pregnant (endocervical canal not sampled).
- Menopausal.
- Young nulliparous.
Principles of FNA
General:
- Fine needle aspiration is an oxymoron.[16]
- One does not really aspirate.
Principles:[17]
- Use a small needle - 22 gauge.
- Use minimal suction - aspiration per se is not the key; the sample is obtained by coring.
- Use minimal back and forth angulation - it destroys blood vessels
History:
- Popularized by the Swedes.[18]
Triage of specimens
At some large centres the specimens are triaged. This is an uncommon practise in the world of cytopathology.
Options:
- Smear.
- Fancy (automated) thin layer preparations:
- Cytospin - centrifuged onto slide.
- ThinPrep - centrifuged onto filter then onto slide.
- Smear + IHC.
- Cell block. + IHC.
Triage of cytopathology specimens:
| Triage of specimens | |||||||||||||||||||||||||||||||||||||||||||||||
| Morphologic analysis | |||||||||||||||||||||||||||||||||||||||||||||||
| Abnormal | Normal | ||||||||||||||||||||||||||||||||||||||||||||||
| Lymphoid | Non-lymphoid | Unknown | Rest to morphology | ||||||||||||||||||||||||||||||||||||||||||||
Management (liquid):
- Lymphoid:
- Fresh:
- Flow cytometry (FC) or laser scanning cytometry (LSC) if sufficient.
- Additional preps (i.e. CytoSpin) not usually useful.
- Fixed:
- Minimal material: smear + immunostains.
- Abundant material: cell block + immunostains.
- Fresh:
- Non-lymphoid:
- Cell block immunostains.
- Unknown:
- Minimal material: smear + immunostains, possibly cell block + immunostains.
- Abundant material: cell block + immunostains and flow cytometry.
Management (solid/clot):
- Cell block +/- immunostains.
Notes:
- It may be hard to diagnose large B cell lymphoma from LSC; thus, a cell block is useful if you have the material.[19]
- Abundant macrophages cause problems with LSC.[20]
- It is not worthwhile to do LSC if there is a scant amount of lymphoid tissue present in the specimen.[21]
- LSC is (usually) not done on CSF specimens with less than 7 mL of volume.[22]
Number of cells for LSC - calculation
Parameters
-- number of cells needed.
-- volume of sample.
-- est. volume of rapid assessment (RA).
-- est. rapid assessment (RA) area.
-- area with 20x obj. on microscope with 18 mm eye piece.
Rule
Application of rule
- Count cells in one field (on the microscope with the 18 mm eye piece) at 20x.
- Divide 167.36 cells ml by the volume of the sample.
- If the cell count in (1) is greater than the number of cells in (2) there are enough cells for a full panel.
Prepartions
| Cost | Cells required | Fixation | Disadvantages/problems | |
|---|---|---|---|---|
| Smear | Minimal ~$5/slide | 1+ | Air dry/alcohol | Layering of cells |
| CytoSpin | Expensive | 50 | ? | Expensive |
| ThinPrep (liquid-based cytology) | Expensive ~$35/slide; intermediate for several slides |
300-400 | Always alcohol (methanol) | Filter damage at edge of prep. |
| Sure-Path (liquid-based cytology) - see Note 1 | Expensive (?) | 300-400 (?) | Always alcohol (ethanol) | (?) |
| Cell block | Expensive | >500 | Usually formalin | Expensive, loss of cells large, truncation artifact in FISH |
| Laser scanning cytometry |
Expensive | ~50,000 for full B cell panel + minimal T cell panel - see Note 2 | None | Tissue needs to be fresh |
Note 1:
- Sure-Path (from TriPath) is not used at many teaching centres (in Ontario) as it has some short coming for non-gyne specimens vis-a-vis ThinPrep (from Cytyc).[23]
- It is used by the private labs in Ontario and seems to be better for Pap tests.
- A comparison between SurePath and ThinPrep/experience from one lab in the USA is here: http://www.palpath.com/MedicalTestPages/papthin1.htm.
Note 2 - see lymphoma article for detailed description of markers:
- The typical "full" panel is:
Notes (general):
- CytoSpin used for CSF specimens.
Cytologic features
Large clusters
- Large clusters - fibrin (junk) vs. other:
- Small (~1/10 of RBC diameter) ovoid, purple staining (on Field stain) = platelets.
- If you see platelets think fibrin.
- Small (~1/10 of RBC diameter) ovoid, purple staining (on Field stain) = platelets.
Necrosis
- Blobs of acellular material.
- No nucleus or pyknosis of nucleus.
- Disrupted/frayed cellular membrane.
- Orangeophilic material (orange material) - on Pap stained material.
Granulomata
Cytology (six features):[24]
- Foamy/bubbly cytoplasm, abundant - low power.
- Epithelioid morphology - cell borders near indistinct - key feature.
- "Footprint" pattern nuclei/bean-shaped nuclei - key feature.
- Macrophages usu. have an ovoid nucleus.
- +/-Nucleoli, small.
- +/-Fibrosis.
- +/-Palisading at edge.
Notes:
- Granulomas are not always nice and round, as in non-cytology specimens.
DDx:
- Infectious:
- AFB:
- Fungal:
- Bacterial:
- Bartonella (gram -ve) (Cat-scratch disease).[25]
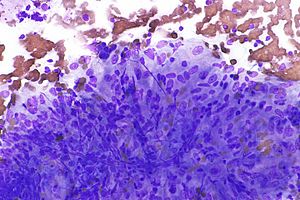
Images
Detail articles
Details are dealt with in separate articles.
Gynecologic cytopathology
Gynecologic cytopathology is the origins of cytopathology and still a large part of cytopathology practise. It is deal with in separate article.
CNS cytopathology
The above article deals with CNS cytopathology, i.e. lumbar puncture specimens.
Pulmonary cytopathology
The above article deals with pulmonary cytopathology, i.e. FNA specimens and sputum specimens.
Fluid from mesothelial-lined space cytopathology
The above article deals with cytopathology specimens from spaces lined with mesothelium.
Urine cytopathology
The above article deals with urine cytopathology.
Thyroid cytopathology
The above article deals with thyroid cytopathology.
Head & neck cytopathology
The above article deals with head and neck cytopathology, excluding thyroid cytopathology.
Breast cytopathology
The above article deals with breast cytopathology.
Gastrointestinal cytopathology
The above article deals with gastrointestinal cytopathology.
Kidney cytopathology
Grab bag of stuff
The following is a grab bag of stuff that is:
- Not covered in the above articles.
- Something that applies to multiple sites (e.g. melanoma).
Mediastinum
DDx:
- Teratoma and other germ cell tumours (GCTs).
- Seminoma/dysgerminoma is the most common.
- Terrible lymphoma.
- Thymoma.
- Mix of epithelial cells and small lymphoid cells.
- Thyroid gland.
- Metastasis.
Thymoma
Cytopathology
Features:[27]
- Mixed population of cells:
- Epithelial cells.
- Circular nuclei with well seen micronucleoli (seen at ~10X objective).
- +/-Nuclear membrane invaginations.
- Mature Lymphocytes.
- Epithelial cells.
DDx (pitfalls):
- Lymphoproliferative disorder (when epithelial component sparse).
- Carcinoma (when lymphoid population small).
- Should not have nuclear features of malignancy.
- Adenocarcinoma: marked size variation, larger nucleoli.
- Squamous carcinoma: often no nucleoli. (???)
- Should not have nuclear features of malignancy.
Notes:
- May have necrosis.
- Should not mistake for granuloma... as nuclei of epithelial cells round not oval.
Image
Benign ovarian cyst
General
- Common - typically serous cystadenoma.
Cytology
Features:
- Benign epithelial cells - often ciliated.
- Macrophages.
- +/-Rare squamous cells.
DDx:
Sign out
Ovarian Cyst, Left, Fine Needle Aspiration: - Compatible with cyst contents; consisting of macrophages, small groups of ciliated cells and rare squamous cells. - Low cellularity. - NEGATIVE for atypia and NEGATIVE for malignancy.
Germ cell tumours
Seminoma
General
Classic scenario:
- Retroperitoneal lymph node enlargement and testicular mass.
Cytology
Features:
- +/-"Corners" in the nuclear membrane.
- Cells cohesive.
- Central nucleus.
- Clear cytoplasm - may be stripped.
- Background with "viscous" or "tigroid" appearance on (air dried) Romanowsky type stains - key feature.
- Tigroid = striped or spotted appearance.[28]
- Related to the presence of glycogen.
- Tigroid pattern not seen on Pap stain.
- Not always seen.
- Tigroid = striped or spotted appearance.[28]
- +/-Small mature lymphocytes (common).
- +/-Granulomas.
Images:
Crystals in fluids
The above article covers gout, pseudogout and urine crystals.
Skin
Malignant melanoma
Classic features:
- Loosely cohesive cells and single cells.
- Mixure of epithelioid cells and spindle cells.
- Malignant cells have:
- Prominent red nucleolus.
- Pigmented cytoplasm - key feature (often not pigmented).
- Pigment may only be present in macrophages
- Occasional large binucleated cells (bug-eyed monster cell).
- Nuclei are often at opposite poles of the cell, i.e. the nuclei are as far apart as possible ("divorce cells").[30]
- Intranuclear inclusions.
- Pigmented macrophages (useful feature - but less specific for melanoma than pigment in malignant looking cells).
Notes:
- Large nucleolus - may vaguely resemble adenocarcinoma.
- Prominent red nucleolus common in: serous carcinoma.
- The classic appearance of melanoma without pigment is closest to adenocarcinoma (which may have red nucleoli, large cells, abundant cytoplasm, occasional binucleation).
- Differentiating morphologic features: adenocarcinoma - 3-D clusters of cells, no spindle-shaped cells.
- Bug-eyed monster cells - may vaguely resemble Reed-Sternberg cells (RSCs) which are diagnostic of Hodgkin's lymphoma (HL).
- RSCs do not have the granular cytoplasm typical of melanoma.
- Nuclei usually adjacent, i.e. not at opposite poles of the cell.
- Background of melanoma different than HL.
Images
Bone marrow/vertebrae
Components:[31]
- One should see three lineages:
- Megakaryocytes.
- Large cells ~ 5-10X RBC.
- Eccentric nuclei.
- Erythrocyte precursor.
- Central nucleus.
- Chromatin - granular.
- One should see ejected nuclei of the same size.
- Granulocytes.
- Megakaryocytes.
- Fat.
- May be seen in a lymph node.
Notes:
- Megakaryocytes - reduced post-bone marrow transplant.
Short DDx:
- Plasma cell lesion, e.g. plasmacytoma.
- Carcinoma (metastatic).
- Lymphoma.
Soft tissue lesions
Nodular fasciitis
General
- Rapid growth - need clinical.
Cytology
Features:
- Tissue culture-like appearance - key feature.
- Myxoid background.
- Moderate nuclear pleomorphism.
Schwannoma
Cytology
Features:
- Bent fish hook-like nuclei - key feature.
- Variable cellularity (Antoni A = cellular, Antoni B = paucicellular).
Solitary fibrous tumour
Cytology
Features:
- Spindle cells with oval nuclei.
- Wire-like lamellar collagen.
IHC
- CD34 +ve.
- BCL2 +ve.
- CD99 +ve.
See also
References
- ↑ UHN Screening process. PCY50001.08.
- ↑ WG. 19 February 2010.
- ↑ WG. 6 January 2010.
- ↑ SM. 5 January 2010.
- ↑ SB. 27 January 2010.
- ↑ SM. 16 May 2008.
- ↑ URL: http://www.mesothelioma-peritoneum.info/. Accessed on: March 18, 2010.
- ↑ http://www3.interscience.wiley.com/journal/121642912/abstract?CRETRY=1&SRETRY=0
- ↑ Horobin RW, Walter KJ (1987). "Understanding Romanowsky staining. I: The Romanowsky-Giemsa effect in blood smears". Histochemistry 86 (3): 331–6. PMID 2437082. http://www.springerlink.com/content/r81x25451m841866/.
- ↑ Horobin RW, Walter KJ (1987). "Understanding Romanowsky staining. I: The Romanowsky-Giemsa effect in blood smears". Histochemistry 86 (3): 331–6. PMID 2437082. http://www.springerlink.com/content/r81x25451m841866/.
- ↑ Sapino A, Papotti M, Pietribiasi F, Bussolati G (September 1998). "Diagnostic cytological features of neuroendocrine differentiated carcinoma of the breast". Virchows Arch. 433 (3): 217–22.
- ↑ UHN PCY50001.08 P.11.
- ↑ UHN PCY50001.08 P.10.
- ↑ GR. 4 February 2010.
- ↑ GR. 4 February 2010.
- ↑ SB. 11 January 2010.
- ↑ SB. 11 January 2010.
- ↑ Diamantis A, Magiorkinis E, Koutselini H (2009). "Fine-needle aspiration (FNA) biopsy: historical aspects". Folia Histochem. Cytobiol. 47 (2): 191–7. doi:10.2478/v10042-009-0027-x. PMID 19995703. http://versita.metapress.com/content/p1p772662w5u373p/.
- ↑ WG. 16 February 2010.
- ↑ SB. March 8, 2010.
- ↑ SB. March 8, 2010.
- ↑ SB. March 11, 2010.
- ↑ SM. January 2010.
- ↑ GS. 26 January 2010.
- ↑ http://emedicine.medscape.com/article/781320-overview
- ↑ 26.0 26.1 URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-031-M.htm. Accessed on: 9 April 2012.
- ↑ FNAC PP.203-4.
- ↑ URL: http://www.merriam-webster.com/medical/tigroid. Accessed on: January 4, 2010.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-040-M.htm. Accessed on: 10 April 2012.
- ↑ GS. 24 February 2010.
- ↑ SB. 25 January 2010.