Difference between revisions of "Placenta"
| (57 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
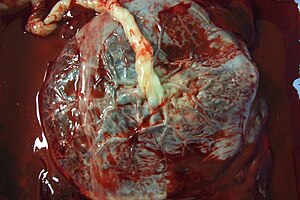
The '''placenta''' feeds the developing baby, breathes for it and disposes of its waste. | [[Image:Human_placenta.jpg|thumb|right|A placenta (fetal aspect) with attached umbilical cord. (WC/Asturnut)]] | ||
The '''placenta''' feeds the developing baby, breathes for it and disposes of its waste. | |||
=Clinical= | The organ is one that seems to be left behind; at least one review suggests it isn't done so well by general pathologists.<ref name=pmid12033960>{{Cite journal | last1 = Sun | first1 = CC. | last2 = Revell | first2 = VO. | last3 = Belli | first3 = AJ. | last4 = Viscardi | first4 = RM. | title = Discrepancy in pathologic diagnosis of placental lesions. | journal = Arch Pathol Lab Med | volume = 126 | issue = 6 | pages = 706-9 | month = Jun | year = 2002 | doi = 10.1043/0003-9985(2002)1260706:DIPDOP2.0.CO;2 | PMID = 12033960 }}</ref> | ||
''Placental pathology'' redirects to this article. | |||
=Clinical= | |||
==Examination of the placenta== | ==Examination of the placenta== | ||
*Most placentas are ''not'' examined by a pathologist. | *Most placentas are ''not'' examined by a pathologist. | ||
| Line 23: | Line 28: | ||
====Most common==== | ====Most common==== | ||
Most common reasons for submitting a placenta to pathology:<ref> | Most common reasons for submitting a placenta to pathology:<ref>Sherman C. 8 February 2011.</ref> | ||
# Prematurity. | # Prematurity. | ||
# PROM / possible [[chorioamnionitis]]. | # PROM / possible [[chorioamnionitis]]. | ||
| Line 45: | Line 50: | ||
*PPROM = preterm premature ruptures of membranes. | *PPROM = preterm premature ruptures of membranes. | ||
*IUGR = [[intrauterine growth restriction]]. | *IUGR = [[intrauterine growth restriction]]. | ||
*IOL = induction of labour. | |||
=Normal histology= | =Normal histology= | ||
| Line 109: | Line 115: | ||
**Focal small deposits are considered to be a normal finding - seen in ~15% of cases.<ref name=pmid21393870>{{Cite journal | last1 = Narasimha | first1 = A. | last2 = Vasudeva | first2 = DS. | title = Spectrum of changes in placenta in toxemia of pregnancy. | journal = Indian J Pathol Microbiol | volume = 54 | issue = 1 | pages = 15-20 | month = | year = | doi = 10.4103/0377-4929.77317 | PMID = 21393870 |URL = http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2011;volume=54;issue=1;spage=15;epage=20;aulast=Narasimha }}</ref><ref>URL: [http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf]. Accessed on: 17 August 2012.</ref> | **Focal small deposits are considered to be a normal finding - seen in ~15% of cases.<ref name=pmid21393870>{{Cite journal | last1 = Narasimha | first1 = A. | last2 = Vasudeva | first2 = DS. | title = Spectrum of changes in placenta in toxemia of pregnancy. | journal = Indian J Pathol Microbiol | volume = 54 | issue = 1 | pages = 15-20 | month = | year = | doi = 10.4103/0377-4929.77317 | PMID = 21393870 |URL = http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2011;volume=54;issue=1;spage=15;epage=20;aulast=Narasimha }}</ref><ref>URL: [http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf]. Accessed on: 17 August 2012.</ref> | ||
***The pathologic counterpart of this is ''[[perivillous fibrin deposition]]''. | ***The pathologic counterpart of this is ''[[perivillous fibrin deposition]]''. | ||
Image: | |||
*[http://www.ijpmonline.org/viewimage.asp?img=IndianJPatholMicrobiol_2011_54_1_15_77317_u5.jpg Subchorionic fibrin deposition (ijpmonline.org)]. | |||
==Common terms== | ==Common terms== | ||
| Line 187: | Line 196: | ||
===Linear regression - placental mass-gestational age=== | ===Linear regression - placental mass-gestational age=== | ||
Based on the table in the AFIP book<ref>AFIP Placental pathol. ISBN: 1-881041-89-1. P.312</ref> | Based on the table in the AFIP book<ref>AFIP Placental pathol. ISBN: 1-881041-89-1. P.312</ref> one can generate the following regression lines: | ||
{| class="wikitable" | {| class="wikitable" | ||
| ||'''50%''' ||'''10%''' ||'''90%''' | | ||'''50%''' ||'''10%''' ||'''90%''' | ||
| Line 211: | Line 220: | ||
*Is it required? | *Is it required? | ||
**Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.<ref>{{cite book |author= Fox, Harold; Sebire, Neil J. |title=[http://www.amazon.com/Pathology-Placenta-Major-Problems/dp/1416025928/ref=sr_1_fkmr0_1?ie=UTF8&qid=1297259619&sr=1-1-fkmr0 Pathology of the Placenta (Major Problems in Pathology)]|publisher=Saunders |location= |year=2007 |pages= 559-561 |edition=3rd |isbn=978-1416025924 |oclc= |doi= |accessdate=}}</ref> | **Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.<ref>{{cite book |author= Fox, Harold; Sebire, Neil J. |title=[http://www.amazon.com/Pathology-Placenta-Major-Problems/dp/1416025928/ref=sr_1_fkmr0_1?ie=UTF8&qid=1297259619&sr=1-1-fkmr0 Pathology of the Placenta (Major Problems in Pathology)]|publisher=Saunders |location= |year=2007 |pages= 559-561 |edition=3rd |isbn=978-1416025924 |oclc= |doi= |accessdate=}}</ref> | ||
***In the context of quality, a measure (even if somewhat flawed) | ***In the context of quality, a measure (even if somewhat flawed) is probably more reproducible and objective than arbitrary descriptors which require experience and a continuing case volume to calibrate. | ||
===Placentomegaly=== | ===Placentomegaly=== | ||
| Line 242: | Line 251: | ||
===Placental growth restriction=== | ===Placental growth restriction=== | ||
*[[AKA]] ''placenta small for gestational age''. | *[[AKA]] ''placenta small for gestational age''. | ||
*''Small placenta'' redirects here. | |||
Associations: | Associations: | ||
*Maternal vascular disease, e.g. [[hypertrophic decidual vasculopathy|hypertension]]. | *Maternal vascular disease, e.g. [[hypertrophic decidual vasculopathy|hypertension]]. | ||
| Line 248: | Line 258: | ||
====Sign out==== | ====Sign out==== | ||
<pre> | <pre> | ||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, | PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: | ||
- PLACENTA SMALL FOR GESTATIONAL AGE (160 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). | - PLACENTA SMALL FOR GESTATIONAL AGE (160 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). | ||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | ||
| Line 345: | Line 355: | ||
*[[AKA]] ''two vessel cord''. | *[[AKA]] ''two vessel cord''. | ||
*[[AKA]] ''single umbilical artery''. | *[[AKA]] ''single umbilical artery''. | ||
{{Main|Two vessel umbilical cord}} | |||
==Insertion== | ==Insertion== | ||
| Line 445: | Line 429: | ||
*Rare ~ 1/5500. | *Rare ~ 1/5500. | ||
*Mortality ~50% is severe. | *Mortality ~50% is severe. | ||
=Membranes= | =Membranes= | ||
| Line 453: | Line 435: | ||
==Amnion nodosum== | ==Amnion nodosum== | ||
{{Main|Amnion nodosum}} | |||
==Placental meconium== | ==Placental meconium== | ||
| Line 493: | Line 447: | ||
===Gross=== | ===Gross=== | ||
Features:<ref name=pmid18081444/> | Features:<ref name=pmid18081444>{{Cite journal | last1 = Adeniran | first1 = AJ. | last2 = Stanek | first2 = J. | title = Amnion nodosum revisited: clinicopathologic and placental correlations. | journal = Arch Pathol Lab Med | volume = 131 | issue = 12 | pages = 1829-33 | month = Dec | year = 2007 | doi = 10.1043/1543-2165(2007)131[1829:ANRCAP]2.0.CO;2 | PMID = 18081444 }}</ref> | ||
*White (or yellow) plaques - irregular outline. | *White (or yellow) plaques - irregular outline. | ||
| Line 567: | Line 521: | ||
==Villous hypoplasia== | ==Villous hypoplasia== | ||
*[[AKA]] ''terminal villus deficiency''.<ref name= | *[[AKA]] ''terminal villus deficiency''.<ref name=Ref_Placenta346>{{Ref Placenta|346}}</ref> | ||
{{Main|Villous hypoplasia}} | |||
=Diseases of the placental attachment= | =Diseases of the placental attachment= | ||
==Placenta creta== | ==Placenta creta== | ||
Includes ''placenta accreta'', ''placenta increta'', and ''placenta percreta''. | |||
{{Main|Placenta creta}} | |||
==Placental abruption== | ==Placental abruption== | ||
{{Main|Placental abruption}} | |||
=Inflammatory pathologies= | =Inflammatory pathologies= | ||
| Line 697: | Line 575: | ||
<pre> | <pre> | ||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: | PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: | ||
- FETAL MEMBRANES WITH CHORIONITIS. | |||
- THREE VESSEL UMBILICAL CORD WITH VASCULITIS. | - THREE VESSEL UMBILICAL CORD WITH VASCULITIS. | ||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI. | - PLACENTAL DISC WITH THIRD TRIMESTER VILLI. | ||
</pre> | |||
====Waffle==== | |||
<pre> | |||
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: | |||
- FETAL MEMBRANES WITH MECONIUM-LADEN MACROPHAGES AND ABUNDANT DECIDUAL NEUTROPHILS | |||
SUSPICIOUS FOR EARLY CHORIONITIS. | |||
- PLACENTAL DISC WITH THIRD TRIMESTER VILLI. | |||
- THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. | |||
</pre> | </pre> | ||
| Line 706: | Line 593: | ||
==Umbilical cord vasculitis== | ==Umbilical cord vasculitis== | ||
{{Main|Umbilical cord vasculitis}} | |||
Umbilical cord vasculitis | |||
==Funisitis== | ==Funisitis== | ||
{{Main|Funisitis}} | |||
* | *Inflammation of Wharton's jelly - the connective tissue of the umbilical cord. | ||
==Acute villitis== | ==Acute villitis== | ||
{{main|Acute villitis}} | |||
==Villitis of unknown etiology== | ==Villitis of unknown etiology== | ||
| Line 800: | Line 626: | ||
==Chronic deciduitis== | ==Chronic deciduitis== | ||
*[[AKA]] plasma cell deciduitis. | *[[AKA]] plasma cell deciduitis. | ||
{{Main|Chronic deciduitis}} | |||
=Placental infarction= | =Placental infarction= | ||
==True infarcts== | ==True infarcts== | ||
{{Main| | {{Main|Placental infarct}} | ||
==Perivillous fibrin deposition== | ==Perivillous fibrin deposition== | ||
*Abbreviation ''PFD''. | *Abbreviation ''PFD''. | ||
===General=== | ===General=== | ||
*Thought to be an immunologic problem - resulting in platelet activation and fibrin deposition.<ref name=pmid12066949/> | *Thought to be an immunologic problem - resulting in platelet activation and fibrin deposition.<ref name=pmid12066949>{{Cite journal | last1 = Sebire | first1 = NJ. | last2 = Backos | first2 = M. | last3 = Goldin | first3 = RD. | last4 = Regan | first4 = L. | title = Placental massive perivillous fibrin deposition associated with antiphospholipid antibody syndrome. | journal = BJOG | volume = 109 | issue = 5 | pages = 570-3 | month = May | year = 2002 | doi = | PMID = 12066949 }}</ref> | ||
*May be associated with [[diabetes mellitus]].<ref name=Ref_Placenta327>{{Ref Placenta|327}}</ref> | *May be associated with [[diabetes mellitus]].<ref name=Ref_Placenta327>{{Ref Placenta|327}}</ref> | ||
| Line 913: | Line 674: | ||
*Formally ''placental maternal floor infarction''. | *Formally ''placental maternal floor infarction''. | ||
*[[AKA]] ''massive perivillous fibrin deposition''.<ref name=Ref_Placenta367>{{Ref Placenta|367}}</ref> | *[[AKA]] ''massive perivillous fibrin deposition''.<ref name=Ref_Placenta367>{{Ref Placenta|367}}</ref> | ||
{{Main|Maternal floor infarction}} | |||
=Fetal disease= | =Fetal disease= | ||
| Line 974: | Line 684: | ||
**''Fetal artery stem thrombosis''. | **''Fetal artery stem thrombosis''. | ||
*The multitude of terms reflects the confusion about this finding and that it has numerous etiologies.<ref name=pmid19237859/> | *The multitude of terms reflects the confusion about this finding and that it has numerous etiologies.<ref name=pmid19237859/> | ||
{{Main|Fetal thrombotic vasculopathy}} | |||
==Hemorrhagic endovasculitis== | ==Hemorrhagic endovasculitis== | ||
*Abbreviated ''HEV''. | *Abbreviated ''HEV''. | ||
| Line 1,028: | Line 719: | ||
==Hypertrophic decidual vasculopathy== | ==Hypertrophic decidual vasculopathy== | ||
: | :[[AKA]] ''decidual vasculopathy''. | ||
{{Main|Hypertrophic decidual vasculopathy}} | |||
==HELLP syndrome== | ==HELLP syndrome== | ||
{{Main|HELLP syndrome}} | |||
==Malaria== | ==Malaria== | ||
| Line 1,144: | Line 768: | ||
*May be spelled ''foetus papyraceus''. | *May be spelled ''foetus papyraceus''. | ||
*[[AKA]] ''fetus compressus''. | *[[AKA]] ''fetus compressus''. | ||
{{Main|Fetus papyraceus}} | |||
==Placental mesenchymal dysplasia== | ==Placental mesenchymal dysplasia== | ||
*Abbreviated ''PMD''. | *Abbreviated ''PMD''. | ||
{{Main|Placental mesenchymal dysplasia}} | |||
=Placental cysts and pseudocysts= | =Placental cysts and pseudocysts= | ||
| Line 1,237: | Line 808: | ||
=External links= | =External links= | ||
*[http://emedicine.medscape.com/article/262470-overview Cord complications (emedicine.medscape.com)]. | *[http://emedicine.medscape.com/article/262470-overview Cord complications (emedicine.medscape.com)]. | ||
*[http://www.palpath.com/MedicalTestPages/placenta2.htm Placenta notes (palpath.com)]. | |||
[[Category:Placenta]] | [[Category:Placenta]] | ||
Latest revision as of 15:27, 10 May 2018
The placenta feeds the developing baby, breathes for it and disposes of its waste.
The organ is one that seems to be left behind; at least one review suggests it isn't done so well by general pathologists.[1]
Placental pathology redirects to this article.
Clinical
Examination of the placenta
- Most placentas are not examined by a pathologist.
Indications for exam by pathology
Some indications for exam by a pathologist:
- Abnormalities in the:
- Fetus:
- Bad fetal outcome.
- Suspected or known congenital abnormalities or chromosomal abnormalities.
- IUGR.
- Mother:
- Infection/suspected infection.
- Pre-term labour.
- Maternal disease (e.g. SLE, coagulopathy).
- Complicated pregnancy (preclampsia, pregnancy induced hypertension, gestational diabetes).
- Placenta:
- Unusual gross characteristics.[2]
- Fetus:
A more detailed list is given by Hargitai et al.[3] and Chang.[4]
Most common
Most common reasons for submitting a placenta to pathology:[5]
- Prematurity.
- PROM / possible chorioamnionitis.
- Multiple gestation.
Bleeding in late pregnancy
DDx of bleeding in late pregnancy:
- Placental abruption (most common).
- Placenta previa.
- Vasa previa (fetus losing blood).
Clinical screening tests
- PAPP-A - low values seen in aneuploidy.[6]
Abbreviations
- C/S = Caesarean section.
- LSCS = lower segment C-section.
- FTP = failure to progress.
- PROM = premature rupture of membranes.
- PPROM = preterm premature ruptures of membranes.
- IUGR = intrauterine growth restriction.
- IOL = induction of labour.
Normal histology
Villi
This is dealt with in a separate article that also covers the types of trophoblast (cytotrophoblast, syncytiotrophoblast, intermediate trophoblast).
Cord
Omphalomesenteric duct remnant
- AKA vitelline duct.
- Benign embryologic remnant.
Features:
- Duct with benign looking cuboidal epithelium.
Allantoic duct remnant
- Benign embryologic remnant.
Features:
- Duct with benign looking flat epithelium.
Vitelline artery remnant
Features:
- Small artery in the cord.
Membranes
Fetus to mother:
- Amnion - thin layer: one cell layer, basement membrane, connective tissue.
- Cleft - artifactual - empty space.
- Chorion - vascular.
- Decidua (maternal tissue) - may contain obsolete chorionic villi; place to look for hypertensive changes.
Amnion
General:
- Next to fetus, surrounds amniotic fluid, avascular.
Characteristics:
- Characterized by a single layer of cells.[7]
- Cuboidal/squamoid shape.
- Eosinophilic cytoplasm.
- Central nucleus.
- Squamous metaplasia may be seen at cord insertion.
- Basement membrane.
- 'Compact layer'.[7]
- 'Fibroblastic layer'.[7]
Chorion
General:
- Surrounds amnion.
Characteristics:
- Layers:[8]
- 'Reticular layer' - cellular (inner aspect).
- 'Pseudo-basemement membrane'.
- 'Outer trophoblastic layer'.
- Has blood vessels.
- Opposed to "trophoblastic X cells" on side opposite of amnion.[7]
- Beneath of the "trophoblastic X cells" is decidua (mnemonic NEW = nucleus central, eosinophilic, well-defined cell border), which is maternal tissue.
Note:
- Fibrin deposition may be found deep to the chorion - known as subchorionic fibrin deposition.
- Gross: subchorionic, white/yellow, laminated, classically has a triangular-shape with the base of triangle parallel to fetal aspect of disc.
- Arises due to localized stasis of the inter-villous maternal blood.
- Focal small deposits are considered to be a normal finding - seen in ~15% of cases.[9][10]
- The pathologic counterpart of this is perivillous fibrin deposition.
- Gross: subchorionic, white/yellow, laminated, classically has a triangular-shape with the base of triangle parallel to fetal aspect of disc.
Image:
Common terms
- Chorionic plate - fetal aspect of placenta.
- Basal plate - maternal aspect of placenta.
- Has extravillous trophoblast.
- Place to look for maternal vessels.
Grossing
This is often very quick. The gross is quite important, as some things cannot be diagnosed microscopically.
General
- Dimensions:
- Disc.
- Length of cord, diameter of cord.
- Accessory lobes - dimensions.
- Two lobes of equal size + cord arises in between = bilobate placenta.
- Mass (weight).
- Should be done 'trimmed' (cord cut-off, membrane cut-off).
- Should be done when placenta is "fresh", i.e. not fixed -- as mass tables are based on fresh state.
- Umbilical cord
- Attachment.
- Location: central, eccentric, marginal.
- Marginal attachment assoc. with hypertension[11]
- Membranous or velamentous (veil-like) insertion.
- Vessels separate/branch prior to reaching placental disc.
- Furcate insertion - blood vessels separate before reaching placenta disc/not surrounded by Wharton's jelly - vessels more exposed to trauma (risk for vasa previa).
- Location: central, eccentric, marginal.
- Knots (false vs. true).
- False knots are nothing to worry about -- look like a knot but aren't really one.
- Twisting/coiling - 1-3 coils/10 cm is normal.
- Number of vessels.
- Normal: 2 arteries, 1 vein.
- Attachment.
- Membranes - shiny & translucent - normal (green, opaque/dull - chorioamnionitis).
- Attachment (insertion): marginal (normal), circummarginate (inside edge), circumvallate (folding on self).
- Site of rupture - if obvious; low point of rupture suggests low-lying placenta.
- Placental disc.
- Fetal surface - normal is shinny.
- Dull in chorioamnionitis.
- Maternal surface
- Are the cotyledons intact?
- Adherent clot?
- Parenchyma - after sectioning:
- White vs. red nodules.
- Fetal surface - normal is shinny.
Notes:
- Parenchymal nodules - a brief DDx:
- White: infarct (chronic), thrombi, chorangioma, perivillous fibrin deposition.
- Red: infarct (acute), thrombi.
Sections
- Cord two sections.
- Membranes (rolled), two rolls or more.[12]
- Cord at insertion + disc.
- Placenta - full thickness (maternal and fetal surface).
- Sections should not be taken at the margin of the disc.
Placental membranes
Appearance:[13]
- Normal - shiny.
- Chorioamnionitis - opaque/dull.
- Meconium - green.
- Amnion nodosum - yellow patches.
- Some describe 'em as white.[14]
Placental mass
It is considered routine to obtain a mass for the placenta. This is usually done when the placenta is fresh and with the membranes and cord trimmed, as most tables of placental mass were created with these parameters.
Placental mass by gestational age:[15]
| Gest. Age/Percentile | 25% | 50% | 75% |
| 32 weeks | 275 g | 318 g | 377 g |
| 36 weeks | 369 g | 440 g | 508 g |
| 40 weeks | 440 g | 501 g | 572 g |
Linear regression - placental mass-gestational age
Based on the table in the AFIP book[16] one can generate the following regression lines:
| 50% | 10% | 90% | |
| slope (g/week) | 21.58088235 | 19.70588235 | 25.40196078 |
| y-intercept (g) | -357.4558824 | -397.2352941 | -366.7254902 |
| Pearson (r) | 0.988670724 | 0.988268672 | 0.982206408 |
placental mass = slope x gestational age + intercept
What to remember...
Extrapolated from the linear regression (see above):
- 50% at term = 500 grams.
- 50% at 26 weeks = 200 grams.
- The change in mass/week is approximately linear and equal to 300 grams / 14 weeks ~ 20 grams/week.
- The spread in mass between 10% and 90%, crudely estimated, is 200 grams (for GA=26-40).
Notes:
- Is it required?
- Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.[17]
- In the context of quality, a measure (even if somewhat flawed) is probably more reproducible and objective than arbitrary descriptors which require experience and a continuing case volume to calibrate.
- Sebire and Fox have advocated abandoning the practise of obtaining a placental mass, due to the large number of uncontrolled variables inherent in these measures. Instead, they have advocated using mushy descriptors such as "small", "average" and "large", which require experience in examining the organ.[17]
Placentomegaly
- AKA large placenta.
Associations:[18]
- Maternal diabetes - esp. poorly controlled.[19]
- Maternal anemia/low maternal iron stores.[20]
- Fetal malformations.
- Neoplasms of the placenta, e.g. chorangioma.
- Twin-twin transfusion syndrome.
- Chronic intrauterine infections, e.g. syphilis, toxoplasmosis, cytomegalovirus.
Lame causes of a heavy placenta:
- Dates wrong - error in determining the estimated date of confinement.
- Adherent blood clot.
Comment:
- Most of causes seem to have one thing in common:
- There is a decreased oxygen delivery to the fetus.
Sign out
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: - LARGE PLACENTA (819 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). - FETAL MEMBRANES WITHIN NORMAL LIMITS. - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI.
Placental growth restriction
- AKA placenta small for gestational age.
- Small placenta redirects here.
Associations:
- Maternal vascular disease, e.g. hypertension.
- Fetal malformations.
Sign out
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - PLACENTA SMALL FOR GESTATIONAL AGE (160 GRAMS -- TRIMMED, POST-FIXATION WEIGHT). - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITH: -- OLD CENTRAL TRANSMURAL INFARCT (1.7 CM MAXIMAL DIMENSION). COMMENT: The 10th percentile placental mass (pre-fixation) for 34 weeks and 2 days is approximately 390 grams.
Overview of placental pathology
Approach
The pathology of the placenta is diverse and is not easy to group.
It terms of remembering things. It is probably easiest to take a combined anatomical, etiologic and morphologic approach.
Anatomical basis:
- Cord.
- Membranes.
- Disc.
Etiologic:
- Congential.
- Infectious.
- Neoplastic.
- Endocrine.
- Trauma.
- Vascular.
- Degenerative.
- Autoimmune.
- Toxic.
- Idiopathic.
Compartmental:
- Vasculature.
- Membranes.
- Parenchyma:
- Maternal part (decidua).
- Fetal part (villi, cord).
Common entities/diagnoses
- Normal.
- Chorioamnionitis.
- Placental abruption.
- Meconium.
- Hypertensive changes.
Sign out
What should be commented on...
- Placenta:
- Maturity of villi (2nd or 3rd trimester).
- Infarction?
- Subchorionic less important than maternal aspect.
- Peripheral aspect of placental disc less important than central region of disc.
- Blood vessels.
- Maternal.
- Fetal.
- Membranes.
- Cord:
- 3 vessel?
- Vasculitis/inflammation?
Mnemonic: chorio, cord, vessels, villi (maturity, infarction).
Normal placenta
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
C-section
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CAESAREAN SECTION: - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Cord pathology
- Two vessel cord.
- Hypercoiling/Hypocoiling.
- Abnormal insertion.
- Cord knots (true vs. false).
- Strictures.
- Hematoma.
- Hemangioma.
- Benign cyst.
Two vessel umbilical cord
Insertion
Marginal insertion
Definition:
- The umbilical cord is attached to the placental disc at its margin.
Prevalence:
- Approximately 12% of placentas.[21]
Relevance:
- None according to WMSP.[21]
- In theory, the cord, dependent on its relation to the internal os, is at greater risk of injury (leading to vasa previa) and compression (fetal hypoxia). A retrospective study found cord position in relation to the internal os is predictive for vasa previa.[22]
Velamentous insertion
Definition:
- The umbilical cord inserts into the fetal membranes.[21]
- The vessels are not protected by Wharton's jelly.
- Wharton's jelly = the connective tissue surrounding the vessels in the cord.
- The vessels are not protected by Wharton's jelly.
Details:[21]
- 3/4 of the time the vessel also branch; in the remaining 1/4 the vessels stay together.
Relevance:
- Increased risk of vasa previa.[22]
Sign out
PLACENTA, UMBILICAL CORDS AND FETAL MEMBRANES, BIRTH: - THREE VESSEL UMBILICAL CORD WITH A VELAMENTOUS INSERTION, OTHERWISE WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI WITHIN NORMAL LIMITS.
Umbilical knot
General
- Prevalence ~1.25%.[23][24]
- Increase risk of stillbirth; odds ratio 3.93.[23]
Gross
Work-up:[24]
- Diameter measures and colour on both sides of the knot.
- Knot should be untied to assess for deformation of Wharton's jelly.
- Sections from both sides of the knot - to look for thrombi.
Note:
- False knots (large diameter - focally) are common - they cannot be untied.
Microscopic
Features:
- +/-Thrombi.
- Fibrin deposition.
- +/-Lines of Zahn.
Images:
Coiling
- Hypo- and hypercoiling are both considered problematic.[21]
- Normal: 1-3 coils/10 cm.[25]
- Associated with cord stricture, which is usu. at the fetal end of the cord.[26]
Notes:
- There is little uniformity in how coiling is assessed in the medical literature - though 10% and 90% are considered the cut-points for normal.[27]
- What are the 10% and 90% cut-points? They are not given in WMSP. UT access to a journal article[28] that might have it is screwed-up.
Cord hematoma
Features:[26]
- Rare ~ 1/5500.
- Mortality ~50% is severe.
Membranes
- Squamous metaplasia.
- Chorioamnionitis - see infection section.
Amnion nodosum
Placental meconium
Squamous metaplasia of the amnion
General
- Benign common finding thought to be of no clinical significance.[29]
- One case report suggesting an association with chorioamnionitis.[30]
- Needs to be separated from amnion nodosum - important.[31]
Gross
Features:[32]
- White (or yellow) plaques - irregular outline.
DDx:
- Amnion nodosum - small (~1-5 mm), round, classically yellow.
Images:
Microscopic
Features:[32]
- Dense, paucicellular (pink) compact keratin - key feature.
Image:
Circumvallate placenta
- AKA circumvallate insertion of the membranes.
General
- May be associated with placental abruption.[34]
Note:
- Membranes usually attach to the edge of the placenta.
Gross
- Fetal membranes attach to the fetal surface of the placenta away from the margin of the placental disc.
Classification:
- Partial - not circumferential.
- Complete.
DDx:
Images:
Twin placentas
These are often submitted... even if they are normal. In these specimens, usually, the chorion is the key.
It covers:
- Monozygotic vs. dizygotic twins.
- Twin-to-twin transfusion syndrome.
Placental disc
Villous edema
General
- Non-specific finding.
- Reported in associated with congenital adrenal hyperplasia for the stem villi.[35]
Microscopic
Features:
- "Swiss chesse-like" appearance / bubbly appearance.
- Usually patchy and focal.
Note:
- Cistern formation is reported in the stem villi in association with congenital adrenal hyperplasia.[35]
DDx:
- Chorioamnionitis.
- Fetal edema.
- Idiopathic (no cause apparent).
- Placental villous immaturity.
Image:
Placental villous immaturity
Villous hypoplasia
Diseases of the placental attachment
Placenta creta
Includes placenta accreta, placenta increta, and placenta percreta.
Placental abruption
Inflammatory pathologies
Overview of infections
General:[38]
- Infection usually ascending, i.e. from vagina up through cervix.
- Associated with intercourse.
- Hematogenous rare - manifest as villitis.
- Think TORCH infections (toxoplasmosis, others (syphilis, TB, listeriosis), rubella, cytomegalovirus, herpes simplex virus).
- Funisitis usually follows chorioamnionitis.
- Inflammatory cells in umbilical cord are fetal (trivia).
Types
By site:[38]
- Fetal membranes: chorioamnionitis, membranitis.[39]
- Umbilical cord: funisitis.
- Placenta: placentitis, villitis.
Membranitis
- Chorionitis redirects here.
General
- Early chorioamnionitis.[40]
- Controversial.[citation needed]
Microscopic
Features:
- PMNs in the decidua.
- +/-PMNs in subamniotic tissue.
- +/-Necrosis in decidua or chorion/subamniotic tissue.
Note:
- Plasma cells in the decidua = chronic deciduitis.
DDx:
Grading membranitis
Sternberg:[39]
- PMNs - decidua only.
- PMNs - in subamniotic tissue.
- 1 or 2 + necrosis in decidua or chorion/subamniotic tissue.
Sign out
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, CESAERIAN SECTION: - FETAL MEMBRANES WITH CHORIONITIS. - THREE VESSEL UMBILICAL CORD WITH VASCULITIS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI.
Waffle
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - FETAL MEMBRANES WITH MECONIUM-LADEN MACROPHAGES AND ABUNDANT DECIDUAL NEUTROPHILS SUSPICIOUS FOR EARLY CHORIONITIS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI. - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS.
Chorioamnionitis
Umbilical cord vasculitis
Funisitis
- Inflammation of Wharton's jelly - the connective tissue of the umbilical cord.
Acute villitis
Villitis of unknown etiology
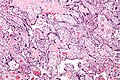
Chronic intervillitis
General
- Rare.
- Massive chronic intervillitis - associated IUGR, spontaneous abortion, perinatal fetal death.[42]
- Recurs.
Microscopic
- Intervillous inflammatory cells:
- Lymphocytes.
- Histiocytes.
- Fibrinoid deposition.
Images
Chronic deciduitis
- AKA plasma cell deciduitis.
Placental infarction
True infarcts
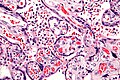
Perivillous fibrin deposition
- Abbreviation PFD.
General
- Thought to be an immunologic problem - resulting in platelet activation and fibrin deposition.[43]
- May be associated with diabetes mellitus.[44]
Gross
- Pale (white).
- Firm.
- White fibrous sepatae.
Microscopic
Features:
- Acellular eosinophilic material around formed villi.
- Obliteration of intervillous space.
- Intervillous distance increased vis-a-vis normal - key feature.
Notes:
- Nuclei of villi are usually preserved.
- Villi may have secondary infarction, i.e. there may be nuclear destruction (karyolysis, karyorrhexis, pyknosis).
DDx:
- Placental infarction - loss of nuclei in the villi (below the edge of the lesion).
- Massive perivillous fibrin deposition (maternal floor infarct).
Images:
Sign out
Thrombi
PLACENTA, UMBILICAL CORD AND FETAL MEMBRANES, BIRTH: - THREE VESSEL UMBILICAL CORD WITHIN NORMAL LIMITS. - FETAL MEMBRANES WITHIN NORMAL LIMITS. - PLACENTAL DISC WITH THIRD TRIMESTER VILLI AND THREE LARGE INTERVILLOUS THROMBI (BLOCKS A7-A9).
Maternal floor infarction
- Abbreviated MFI.
- Formally placental maternal floor infarction.
- AKA massive perivillous fibrin deposition.[45]
Fetal disease
Fetal thrombotic vasculopathy
- Abbreviated FTV.
- A large number of terms are used for this including:[46]
- Fibrinous vasculosis.
- Fibromuscular sclerosis.
- Fetal artery stem thrombosis.
- The multitude of terms reflects the confusion about this finding and that it has numerous etiologies.[46]
Hemorrhagic endovasculitis
- Abbreviated HEV.
General
- Associated with stillbirth.[47]
Microscopic
Features:[48]
- Walls of the (fetal) placental blood vessels (in the villi) are disrupted.
- +/-Intraluminal necrotic debris.
- RBC fragmentation.
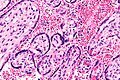
Maternal disease
Hypertensive changes
General
Associated pathologic changes:[49]
- Placental infarcts.
- Increased syncytial knots.
- Hypovascularity of the villi.
- Cytotrophoblastic proliferation.
- Thickening of the trophoblastic basement membrane.
Microscopic
Features:[49]
- Enlarged endothelial cells - fetal capillaries.
- Atherosis of the spiral arteries - placental bed (maternal).
Notes:
- One should look for the changes in the membrane roll, not the maternal surface.[50]
Images:
Hypertrophic decidual vasculopathy
- AKA decidual vasculopathy.
HELLP syndrome
Malaria
General
- Uncommon in Canada.
- May lead to fetal demise.
Microscopic
Feature:
- RBCs with basophilic dots ~1-2 micrometres.
Image
Tumours
Chorangioma
Chorangiomatosis
General
Associated with:
- Preeclampsia.
- IUGR.
Gross
- Multiple tan nodules.
Microscopic
Features:
- Multiple chorangiomas - the difference between chorangioma and chorangiomatosis is not well defined.[51]
Images:
Chorangiosis
Other
Fetus papyraceus
- May be spelled foetus papyraceus.
- AKA fetus compressus.
Placental mesenchymal dysplasia
- Abbreviated PMD.
Placental cysts and pseudocysts
Types:[52]
- Amnionic epithelial inclusion cyst (amniotic cyst).
- Epidermal inclusion cyst - lined by keratinized squamous epithelium.
- Chorionic cyst (AKA chorionic pseudocyts).
- Cell island cyst.
Other considerations:[53]
- Hematoma.
- Fibrin-lined pseudocyst.
General:[53]
- Usually good outcome.
- Large cysts (>4.5 cm) or multiple cysts (>3) are associated with IUGR.
Images:
See also
References
- ↑ Sun, CC.; Revell, VO.; Belli, AJ.; Viscardi, RM. (Jun 2002). "Discrepancy in pathologic diagnosis of placental lesions.". Arch Pathol Lab Med 126 (6): 706-9. doi:10.1043/0003-9985(2002)1260706:DIPDOP2.0.CO;2. PMID 12033960.
- ↑ Yetter JF (March 1998). "Examination of the placenta". Am Fam Physician 57 (5): 1045–54. PMID 9518951.
- ↑ Hargitai B, Marton T, Cox PM (August 2004). "Best practice no 178. Examination of the human placenta". J. Clin. Pathol. 57 (8): 785–92. doi:10.1136/jcp.2003.014217. PMC 1770400. PMID 15280396. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770400/.
- ↑ URL: http://smj.sma.org.sg/5012/5012ra1.pdf. Accessed on: 11 February 2011.
- ↑ Sherman C. 8 February 2011.
- ↑ URL: http://www.ncbi.nlm.nih.gov/sites/entrez?Db=gene&Cmd=ShowDetailView&TermToSearch=5069. Accessed on: 7 July 2010.
- ↑ 7.0 7.1 7.2 7.3 Sternberg, Stephen S. (1997). Histology for Pathologists (2nd ed.). Lippincott Williams & Wilkins. pp. 974. ISBN 978-0397517183.
- ↑ Sternberg, Stephen S. (1997). Histology for Pathologists (2nd ed.). Lippincott Williams & Wilkins. pp. 977. ISBN 978-0397517183.
- ↑ Narasimha, A.; Vasudeva, DS.. "Spectrum of changes in placenta in toxemia of pregnancy.". Indian J Pathol Microbiol 54 (1): 15-20. doi:10.4103/0377-4929.77317. PMID 21393870.
- ↑ URL: http://zulekhahospitals.com/uploads/files/Sub-chorionic.pdf. Accessed on: 17 August 2012.
- ↑ J Anat. Soc. India 49(2) 149-152 (2000). Available at: http://www.indmedica.com/anatomy/aindex1.cfm?anid=41. Accessed on: January 21, 2009.
- ↑ Winters R, Waters BL (December 2008). "What is adequate sampling of extraplacental membranes?: a randomized, prospective analysis". Arch. Pathol. Lab. Med. 132 (12): 1920–3. PMID 19061291.
- ↑ Lester, Susan Carole (2005). Manual of Surgical Pathology (2nd ed.). Saunders. pp. 461. ISBN 978-0443066450.
- ↑ CS. 7 February 2011.
- ↑ AFIP Placental pathol. ISBN: 1-881041-89-1. P.312
- ↑ AFIP Placental pathol. ISBN: 1-881041-89-1. P.312
- ↑ Fox, Harold; Sebire, Neil J. (2007). Pathology of the Placenta (Major Problems in Pathology) (3rd ed.). Saunders. pp. 559-561. ISBN 978-1416025924.
- ↑ URL: http://quizlet.com/5793113/ob-flash-cards/. Accessed on: 13 January 2012.
- ↑ Clarson, C.; Tevaarwerk, GJ.; Harding, PG.; Chance, GW.; Haust, MD.. "Placental weight in diabetic pregnancies.". Placenta 10 (3): 275-81. PMID 2771897.
- ↑ Hindmarsh, PC.; Geary, MP.; Rodeck, CH.; Jackson, MR.; Kingdom, JC. (Aug 2000). "Effect of early maternal iron stores on placental weight and structure.". Lancet 356 (9231): 719-23. PMID 11085691.
- ↑ 21.0 21.1 21.2 21.3 21.4 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 464. ISBN 978-0781765275.
- ↑ 22.0 22.1 Hasegawa J, Farina A, Nakamura M, et al. (December 2010). "Analysis of the ultrasonographic findings predictive of vasa previa". Prenat. Diagn. 30 (12-13): 1121–5. doi:10.1002/pd.2618. PMID 20872421.
- ↑ 23.0 23.1 Airas U, Heinonen S (April 2002). "Clinical significance of true umbilical knots: a population-based analysis". Am J Perinatol 19 (3): 127–32. doi:10.1055/s-2002-25311. PMID 12012287.
- ↑ 24.0 24.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 464. ISBN 978-0781765275.
- ↑ CS. 7 February 2011.
- ↑ 26.0 26.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 465. ISBN 978-0781765275.
- ↑ Khong TY (December 2010). "Evidence-based pathology: umbilical cord coiling". Pathology 42 (7): 618–22. doi:10.3109/00313025.2010.520309. PMID 21080869.
- ↑ PMID 16076615.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 463. ISBN 978-0781765275.
- ↑ Chew, RH.; Silberberg, BK. (Apr 1990). "Possible association of acute inflammatory exudate in chorioamnionitis and amniotic squamous metaplasia.". Am J Clin Pathol 93 (4): 582-5. PMID 2321592.
- ↑ CS. 7 February 2011.
- ↑ 32.0 32.1 32.2 Adeniran, AJ.; Stanek, J. (Dec 2007). "Amnion nodosum revisited: clinicopathologic and placental correlations.". Arch Pathol Lab Med 131 (12): 1829-33. doi:10.1043/1543-2165(2007)131[1829:ANRCAP]2.0.CO;2. PMID 18081444.
- ↑ URL: http://flylib.com/books/en/2.953.1.49/1/. Accessed on: 10 January 2011.
- ↑ Suzuki, S. (Feb 2008). "Clinical significance of pregnancies with circumvallate placenta.". J Obstet Gynaecol Res 34 (1): 51-4. doi:10.1111/j.1447-0756.2007.00682.x. PMID 18226129.
- ↑ 35.0 35.1 Furuhashi, M.; Oda, H.; Nakashima, T. (Sep 2000). "Hydrops of placental stem villi complicated with fetal congenital adrenal hyperplasia.". Arch Gynecol Obstet 264 (2): 101-4. PMID 11045335.
- ↑ URL: http://www.med.yale.edu/obgyn/kliman/placenta/articles/EOR_Placenta/Trophtoplacenta.html. Accessed on: 28 May 2011.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 346. ISBN 978-1441974938.
- ↑ 38.0 38.1 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1106. ISBN 0-7216-0187-1.
- ↑ 39.0 39.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 2311. ISBN 978-0781740517.
- ↑ Vedovato, S.; Zanardo, V. (Jun 2010). "[Chorioamnionitis and inflammatory disease in the premature newborn infant].". Minerva Pediatr 62 (3 Suppl 1): 155-6. PMID 21090086.
- ↑ 41.0 41.1 Jacques, SM.; Qureshi, F. (Oct 1993). "Chronic intervillositis of the placenta.". Arch Pathol Lab Med 117 (10): 1032-5. PMID 8215826.
- ↑ 42.0 42.1 Rota, C.; Carles, D.; Schaeffer, V.; Guyon, F.; Saura, R.; Horovitz, J. (Nov 2006). "[Perinatal prognosis of pregnancies complicated by placental chronic intervillitis].". J Gynecol Obstet Biol Reprod (Paris) 35 (7): 711-9. PMID 17088773.
- ↑ Sebire, NJ.; Backos, M.; Goldin, RD.; Regan, L. (May 2002). "Placental massive perivillous fibrin deposition associated with antiphospholipid antibody syndrome.". BJOG 109 (5): 570-3. PMID 12066949.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 327. ISBN 978-1441974938.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 367. ISBN 978-1441974938.
- ↑ 46.0 46.1 Marchetti, D.; Belviso, M.; Fulcheri, E. (Mar 2009). "A case of stillbirth: the importance of placental investigation in medico-legal practice.". Am J Forensic Med Pathol 30 (1): 64-8. doi:10.1097/PAF.0b013e318187387e. PMID 19237859.
- ↑ Stevens NG, Sander CH (October 1984). "Placental hemorrhagic endovasculitis: risk factors and impact on pregnancy outcome". Int J Gynaecol Obstet 22 (5): 393–7. PMID 6151926.
- ↑ Sander CM, Gilliland D, Akers C, McGrath A, Bismar TA, Swart-Hills LA (February 2002). "Livebirths with placental hemorrhagic endovasculitis: interlesional relationships and perinatal outcomes". Arch. Pathol. Lab. Med. 126 (2): 157–64. PMID 11825110.
- ↑ 49.0 49.1 Soma H, Yoshida K, Mukaida T, Tabuchi Y (1982). "Morphologic changes in the hypertensive placenta". Contrib Gynecol Obstet 9: 58–75. PMID 6754249.
- ↑ Sherman, C. 7 February 2011.
- ↑ URL: http://path.upmc.edu/cases/case655/dx.html. Accessed on: 28 January 2012.
- ↑ Baergen, Rebecca N. (2011). Manual of Pathology of the Human Placenta (2nd ed.). Springer. pp. 219-220. ISBN 978-1441974938.
- ↑ 53.0 53.1 53.2 Brown, DL.; DiSalvo, DN.; Frates, MC.; Davidson, KM.; Genest, DR. (Jun 2002). "Placental surface cysts detected on sonography: histologic and clinical correlation.". J Ultrasound Med 21 (6): 641-6; quiz 647-8. PMID 12054300.
Recommended reading
- Langston C, Kaplan C, Macpherson T, et al. (May 1997). "Practice guideline for examination of the placenta: developed by the Placental Pathology Practice Guideline Development Task Force of the College of American Pathologists". Arch. Pathol. Lab. Med. 121 (5): 449–76. PMID 9167599.
- Baergen, Rebecca N. (2005). Manual of Benirschke and Kaufmann's Pathology of the Human Placenta (1st ed.). Springer. ISBN 978-0387220895.