Difference between revisions of "Thyroid gland"
(→Hyalinizing trabecular tumour: more images) |
(→Solid cell nest of the thyroid gland: +images) |
||
| Line 107: | Line 107: | ||
**Round/ovoid nuclei with finely granular chromatin. | **Round/ovoid nuclei with finely granular chromatin. | ||
*+/-Goblet cells (~30% of cases).<ref name=pmid7509563>{{cite journal |author=Mizukami Y, Nonomura A, Michigishi T, ''et al.'' |title=Solid cell nests of the thyroid. A histologic and immunohistochemical study |journal=Am. J. Clin. Pathol. |volume=101 |issue=2 |pages=186–91 |year=1994 |month=February |pmid=7509563 |doi= |url=}}</ref> | *+/-Goblet cells (~30% of cases).<ref name=pmid7509563>{{cite journal |author=Mizukami Y, Nonomura A, Michigishi T, ''et al.'' |title=Solid cell nests of the thyroid. A histologic and immunohistochemical study |journal=Am. J. Clin. Pathol. |volume=101 |issue=2 |pages=186–91 |year=1994 |month=February |pmid=7509563 |doi= |url=}}</ref> | ||
DDx:<ref name=pmid12527712/> | DDx:<ref name=pmid12527712/> | ||
| Line 120: | Line 112: | ||
*[[Medullary thyroid carcinoma|Medullary carcinoma]]. | *[[Medullary thyroid carcinoma|Medullary carcinoma]]. | ||
*Squamous lesions. | *Squamous lesions. | ||
====Images==== | |||
<gallery> | |||
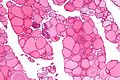
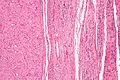
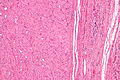
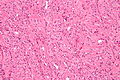
Image:Solid_cell_nest_of_the_thyroid_gland_-_intermed_mag.jpg | Solid cell nest of the thyroid gland - intermed. mag. (WC) | |||
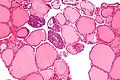
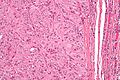
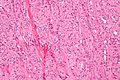
Image:Solid_cell_nest_of_the_thyroid_gland_-_high_mag.jpg | Solid cell nest of the thyroid gland - high mag. (WC) | |||
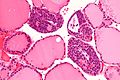
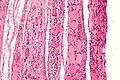
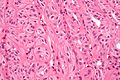
Image:Solid_cell_nest_of_the_thyroid_gland_-_very_high_mag.jpg | Solid cell nest of the thyroid gland - very high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://farm6.static.flickr.com/5143/5685400518_c4f506d370.jpg Solid cell next (flickr.com)]. | |||
*[http://www.nature.com/modpathol/journal/v16/n1/fig_tab/3880708f1.html#figure-title Crappy B&W of solid cell nest (nature.com)]. | |||
===IHC=== | ===IHC=== | ||
Revision as of 11:06, 4 September 2013
The thyroid gland is an important little endocrine organ in the anterior neck. It is frequently afflicted by cancer... but the common cancer has such a good prognosis there is debate about how aggressively it should be treated. The cytopathology of the thyroid gland is dealt with in the thyroid cytology article.
The gland frustrates a significant number of pathologists, as the criteria for cancer are considered a bit wishy-washy.
Thyroid specimens
They come in three common varieties
- FNA (fine needle aspiration).
- Done to triage patients/rule-out malignancy - discussed in the article thyroid cytopathology.
- Hemithyroid.
- Done to get a definitive diagnosis.
- May be a "completion" - removal of the other half following definitive diagnosis.
- Total thyroid.
- Done for malignancy or follicular lesion.
Gross pathology
- White nodules - think:
- Lymphoid tissue.
- Papillary thyroid carcinoma - may be calcified.[1]
Diagnoses
Common
- Nodular hyperplasia -- most common.
- Lymphocytic thyroiditis.
- Papillary thyroid carcinoma (PTC) -- most common cancer.
- Parathyroid tissue.
Pitfalls/weird stuff
- Thyroid tissue lateral to the jugular vein (often referred to as lateral aberrant thyroid tissue) is generally considered metastatic thyroid carcinoma (papillary thyroid carcinoma) even if it looks benign.[2]
- This dictum is disputed.[3]
- The level VI and VII lymph nodes are medial to the jugular.
- Hashimoto's disease may have so many lymphocytes that it mimics a lymph node -- may lead to misdiagnosis of PTC.
- Parasitic nodule: clump of thyroid that is attached by a thin thread... but looks like a separate nodule; may lead to misdiagnosis of PTC.
Image:
Diagnostic keys
The following should prompt careful examination:[5]
- Architecture: microfollicular, trabecular, solid, insular.
- Thick capsule.
- Necrosis - rare in the thyroid.
Thyroid IHC - general comments
- Not really useful.
- Papers with very small sample sizes abound.
Follicular thyroid carcinoma vs. papillary thyroid carcinoma
- CD31 more frequently positive in follicular lesions.[6]
- CD31 is a marker for microvessel density.
- Galectin-3 thought to be positive in papillary carcinoma.[6]
- HBME-1 thought to be positive in papillary lesions.[7]
Thyroid lesions per WHO
- Adapted from the Washington Manual of Surgical Pathology.[8]
Adenoma
- Follicular adenoma.
- Hyalinizing trabecular tumour.
Carcinoma
- Papillary carcinoma.
- Follicular carinoma.
- Medullary carcinoma.
- Undifferentiated (anaplastic) carcinoma.
- Poorly differentiated carcinoma.
- Squamous cell carcinoma.
- Mucoepidermoid carcinoma.
- Sclerosing mucoepidermoid carcinoma with eosinophilia.
- Mucinous carcinoma.
- Mixed medullary and follicular carinoma.
- Spindle cell tumour with thymus-like differentiation.
- Carcinoma showing thymus-like differentiation.
Others
- Teratoma.
- Lymphoma.
- Ectopic thymoma.
- Angiosarcoma + other soft tissue lesions.
- Paraganglioma.
- Solitary fibrous tumour.
- Follicular dendritic cell tumour.
- Langerhans cell histiocytosis.
- Metastasis.
Parathyroid glands
- May make an appearance in the context of thyroid surgery.
Benign
Solid cell nest of the thyroid gland
- AKA solid cell nest of thyroid.
General
- Embryonic remnants endodermal origin.[9]
- Incidental finding.
Note:
- Hypothesized to have some relation to mucoepidermoid carcinoma of the thyroid gland;[10] however, another study suspects a relationship with papillary thyroid carcinoma.[11]
Microscopic
Features:[9]
- Cellular solid or cystic cluster of variable size with:
- Cuboidal cellular morphology.
- May have columnar morphology.
- Moderate-to-scant eosinophilic cytoplasm.
- Round/ovoid nuclei with finely granular chromatin.
- Cuboidal cellular morphology.
- +/-Goblet cells (~30% of cases).[12]
DDx:[9]
- C-cell hyperplasia.
- Medullary carcinoma.
- Squamous lesions.
Images
www:
IHC
Features:[9]
- p63 +ve.
- -ve in clear cells.
- CEA +ve (polyconal).[12]
- +ve also in clear cells.
- Chromogranin A +ve ~45% of cases.[12]
Sign out
Solid cell nests of the thyroid gland are usually not reported.
Thyroid gland nodular hyperplasia
- AKA nodular hyperplasia.
- AKA adenomatoid nodule.
General
- Clinical diagnosis: goitre, AKA sporadic goitre, AKA multinodular goitre (MNG).
- Most common diagnosis in the thyroid.
- If you've seen a handful of thyroids you've seen this.
Notes:
- Large lesions may be clonal; however, this is clinically irrelevant.
Gross
Features:
- Enlarge thyroid gland.
- +/-Distinct (well-circumscribed) nodules.
Microscopic
Features:
- Follicles of variable size - key feature.
- Should be obvious at low power, i.e. with the 2.5x objective.
- +/-Nodules.
- Do not have a thick fibrous capsule.
- May have a high cellularity.
- Architecture: solid or microfollicular.[13]
Negatives:
- No nuclear features suggestive of malignancy (at lower power).
- One should not look at high power.
- Not cellular.
DDx:
- Papillary thyroid carcinoma - esp. papillary thyroid carcinoma follicular variant.
- Follicular thyroid adenoma - contained in a fibrous capsule.
- Follicular thyroid carcinoma - has fibrous capsule and invasion through it.
Sign out
HEMITHYROID, RIGHT, HEMITHYROIDECTOMY: - NODULAR HYPERPLASIA. - NEGATIVE FOR MALIGNANCY.
HEMITHYROID, RIGHT, HEMITHYROIDECTOMY: - CELLULAR ADENOMATOID NODULE ON A BACKGROUND OF NODULAR HYPERPLASIA. - NEGATIVE FOR MALIGNANCY.
Follicular thyroid adenoma
General
- Most common neoplasm of thyroid.[14]
- Encapusled lesion (surrounded by fibrous capsule).
Gross
- Thick capsule.
Notes:
- The entire capsule should be submitted.[15]
- A good start for most thyroid specimens with a thick capsule is 10 blocks.
Microsopic
Features:
- Cellular.
- Thick capsule - key feature.
Negatives.
- No invasion of the capsule (see follicular thyroid carcinoma section).
- No nuclear features suggestive of papillary thyroid carcinoma.
DDx:
- Thyroid gland nodular hyperplasia with an encapsulated nodule - not as cellular.
Graves disease
General
- Often misspelled "Grave's disease".
- Autoimmune disease leading to hyperthyroidism.
- Eye problems not resolved with thyroid removal.[citation needed]
- Higher risk of papillary thyroid carcinoma.
Clinical:
- TSH-receptor antibody +ve.[16]
Gross
Features:[17]
- Enlarged 50-150 g.
- "Beefy-red" appearance, looks like raw beef.
Microscopic
Features:
- Classic:
- Hypercellular
- Patchy lymphocytes.
- Little colloid.
- Scalloping of colloid; colloid has undulating border.
- Non-specific finding.
- +/-Nuclear clearing.
- +/-Papillae (may mimic papillary thyroid carcinoma in this respect).
Notes:
- Usually has an unimpressive appearance... as it is treated, i.e. history is important.
- Nuclear clearing and papillae are usu. diffuse in Graves disease - unlike in papillary thyroid carcinoma.
Image:
Idiopathic granulomatous thyroiditis
- AKA granulomatous thyroiditis - non-specific term; granulomas may be due a number of causes.
- AKA subacute thyroiditis.
- AKA de Quervain thyroiditis.
- Should not be confused with de Quervain's disease (AKA gamer's thumb) something completely unrelated to the thyroid.
General
- Women > men.
- Etiology: possibly viral.[19]
Clinical:
- Tenderness.[20]
Microscopic
- Granulomas with multinucleated giant cells - usu. with engulfed colloid.
- Lymphocytes.
- Plasma cells.
- +/-Fibrosis.
DDx:
- Infectious granulomatous disease (fungal, microbacterial).
- Palpation thyroiditis.
- Sarcoidosis (classically intrafollicular distribution).
Images:
Stains
- ZN -ve.
- GMS -ve.
Palpation thyroiditis
General
- Granulomatous inflammation due to palpation.
- Incidence of granulomas higher in surgical thyroid specimens than autopsies.[19]
Microscopic
Features:[19]
- Granulomas involving the follicle.
- Histiocytes within the colloid.
DDx:
- Idiopathic granulomatous thyroiditis.
- Sarcoidosis.
- Infectious granulomatous thyroiditis.
Stains
- ZN -ve.
- GMS -ve.
Riedel thyroiditis
General
Clinical features:[22]
- Extremely rare.
- Women > men.
- Usually smokers.
- May be associated with retroperitoneal fibrosis.
- May be hypothyroid.
- +/-Obstructive symptoms.
Microscopic
Features:
- Fibrosis.
- Specimen often fragmented as it was difficult to remove.
DDx:
- Anaplastic carcinoma, spindle cell variant.
Hashimoto thyroiditis
General
- This is a clinical diagnosis.
- The histomorphologic findings, generally, are not diagnostic.
Etiology:
- Autoimmune disease leading to hypothyroidism.
- Often genetic/part of a syndrome.
Clinical
Serology:[23]
- Antimicrosomal (antithyroid peroxidase) +ve.
- Antithyroglobulin +ve.
Associated pathology:[23]
- Increased risk of B-cell lymphoma; these are classically:[24]
- MALT lymphoma.
- Diffuse large B cell lymphoma (DLBCL).
Microscopic
Features:
- Lymphocytic infiltrate - key feature.
- Nuclear clearing common.
- May confuse with papillary thyroid carcinoma.
- Polymorphous lymphoplasmacytic infiltrate with germinal centres.[25]
- +/-Oncocytic metaplasia.
Notes:
- Histologically often not possible to separate from "non-specific" thyroiditis.[26]
DDx:
IHC
- Panel to exclude lymphoma may be required, e.g. CD3, CD20, CD10, BCL6, BCL2, kappa, lambda.
Molecular
- Occasionally done to exclude lymphoma - see MALT lymphoma and DLBCL.
C-cell hyperplasia
- Abbreviated CCH.
General
- Screening for C-cell hyperplasia/medullary thyroid carcinoma done with serum calcitonin level.[27]
Gross
- Not visible.
Microscopic
Features:
- Location:[28]
- Mid portion of lobe to upper third of lobe.
- Not at the poles.
- Not in the isthmus.
- Mid portion of lobe to upper third of lobe.
- Definitions vary.[29]
One definition - either of the following:[27]
- >50 C-cells per low-power field (x100).
- This part of the definition suffers from LPFitis. The paper should have been rejected.
- Confined to the thyroid gland and no larger than 10 mm in greatest dimension.
Another definition:
- Invasion of the basement membrane with stromal reaction.
A third definition:
- "Several clusters" of more than six C cells.
Images
- CCH - crappy B&W image (nature.com).[30]
- CCH - crappy B&W image (nature.com).
- CCH (forpath.org).[31]
- CCH (unibas.ch).
- Nodular CCH (unibas.ch).
Malignant neoplasm
There are a bunch of 'em. The most common, by far, is papillary.
Papillary thyroid carcinoma
- Abbreviated PTC.
General
Medical school memory device P's:
- Palpable nodes.
- Popular (most common malignant neoplasm of the thyroid).
- Prognosis is good.
- Pre-Tx iodine scan.
- Post-Sx iodine scan.
- Psammoma bodies.
Notes:
- PTC is associated with radiation exposure.[32]
- Papillary thyroid microcarcinoma is defined as a tumour with a maximal dimension of 1.0 cm or less.[33]
Prognosis
Prognosis can be predicted by MAICS score. It which includes:[34]
- Metastases.
- Age.
- Invasion of surround tissues.
- Ccompleteness of excision.
- Size of tumour.
Microscopic
Features:
- Nuclear changes - key feature.
- "Shrivelled nuclei"/"raisin" like nuclei, nuclei with a wavy ("textured", convoluted) nuclear membrane -- usu. easy to find.
- Nuclear pseudoinclusions -- usu. harder to find; have high specificity (nuclear pseudoinclusions appear as a result of the very convoluted nuclear membrane wrapping around parts of the cytoplasm; true nuclear inclusions in contrast are seen only in viral infections).
- Nuclear grooves, seen as a result of the highly "textured" nuclear membrane.
- Nuclear clearing (only on permanent section) - also known as "Orphan Annie eyes".
- Overlap of nuclei - "cells do not respect each other's borders" (easy to see at key feature at low power).
- Classically has papillae (nipple-like shape); papilla (definition): epithelium on fibrovascular core.
- Absence of papillae does not exclude diagnosis.
- Psammoma bodies.
- Circular, acellular, eosinophilic whorled bodies.
- Not necessary to make diagnosis - but very specific in the context of a specimen labeled "thyroid".
- Arise from infarction & calcification of papilla tips.[35]
Notes:
- Psammoma bodies are awesome if you see 'em, i.e. useful for arriving at the diagnosis.
- If there are no papillae structures -- you're unlikely to see psammoma bodies.
- At low power look for cellular areas/loss of follicles.
- Nuclear clearing seen in:
- Nuclear overlapping is easy to see at lower power-- should be the tip-off to look at high power for nuclear features.
- Nuclear inclusions are quite rare and not required to make the diagnosis -- but a very convincing feature if seen.
- Papillae may be seen in Graves disease.
DDx:
Subtypes of papillary thyroid carcinoma
There are many.
Poor prognosis variants:
- Tall cell variant.[38]
- Columnar cell variant.[38]
- Solid variant.[38]
- Diffuse sclerosing variant.[39]
Papillary thyroid carcinoma tall cell variant
General
- ~10% of PTC.[40]
- Often large > 6 cm.
Microscopic
Features:[41]
- 50% of cells with height 2x the width.[42]
- Eosinophilic cytoplasm.
- Well-defined cell borders.
- Nucleus stratified; basal location, i.e. closer to the basement membrane.
Negative:
- Nuclei not pseudostratified, if pseudostratified consider columnar cell variant.
Images:
Papillary thyroid carcinoma columnar cell variant
General
Epidemiology:
- Poor prognosis.
- Very rare.
Microscopic
Features:[44]
- Elongated nuclei (similar to colorectal adenocarcinoma) - key feature.
- +/-Pseudostratification of the nuclei (like in colorectal adenocarcinoma), differentiates from tall cell variant.
- Nuclear stratification - key feature.
- "Minimal" papillary features.
- "Tall cells".
- Clear-eosinophilic cytoplasm.
- Mitoses common.
Image: Columnar variant PTC (wiley.com).
Papillary thyroid carcinoma follicular variant
General
- May be confused with follicular carcinoma or follicular adenoma.
- Pathologists often disagree about this diagnosis.[45]
Microscopic
Features:[46]
- Small tightly packed follicles - key feature.
- Hypereosinophilic colloid.
- Nuclear features of PTC.
- Large nuclei.
- Typically have less nuclear pseudoinclusions than the conventional type.
- +/-Fibrous capsule (common).
DDx:
- Follicular thyroid carcinoma - has a fibrous capsule and invasion though it.
- Follicular thyroid adenoma - surrounded by a fibrous capsule.
- Adenomatoid nodule - round nuclei, no nuclear features of PTC.
Images:
- PTC follicular variant (surgicalpathologyatlas.com).
- PTC follicular variant (surgicalpathologyatlas.com).
- PTC follicular variant (thyroidcancercanada.org).[47]
Papillary thyroid carcinoma cribriform-morular variant
General
- Associated with familial adenomatous polyposis (FAP).[48]
Microscopic
Features:
- Cribriform architectural pattern.
- Morules - balls of tissue.
Papillary thyroid carcinoma diffuse sclerosing variant
General
- Usually young adults, children.
Microscopic
Features:[49]
- Papillae - usu. prominent.
- Squamous morules - key features.[50]
- Lymphocytes - abundant.
- Fibrosis.
DDx:
- Lymphocytic thyroiditis (esp. Hashimoto's thyroiditis).
Papillary thyroid carcinoma warthin-like variant
- Resemble Warthin tumour.
Microscopic
Features:[44]
- Eosinophilic cytoplasm.
- Lymphocytic thyroiditis.
- Papillae.
Papillary thyroid carcinoma solid variant
Features:[38]
- Some studies suggest this has a poor prognosis.
- More common in children.
- Associated with Chernobyl nuclear accident.
Microscopic
Features:
- Solid sheets >50% of tumour mass.[38]
IHC
Thyroid versus something else:
- Thyroglobulin +ve.
- TTF-1 (thyroid transcription factor-1) +ve.
- CD15 +ve.[citation needed]
PTC versus benign:[51]
- HBME-1 +ve (strong, diffuse).
- CK19 +ve (strong, diffuse).
- Galectin-3 +ve (strong, diffuse).
Molecular
- Currently not widely used in a diagnostic context.
Tabular summary
Molecular changes in papillary thyroid carcinoma as per Adeniran et al:[52]
| Molecular change | Frequency | Histology | Notes |
|---|---|---|---|
| BRAF point mutations | ~ 40% | tall cell variant | poorer prognosis, older individuals |
| RET/PTC rearrangments | ~ 20% | papillary architecture, psammoma bodies | younger individuals |
| RAS point mutations | ~ 15% | exclusively follicular variant | - |
Sign out
HEMITHYROID, RIGHT, COMPLETION OF TOTAL THYROIDECTOMY: - PAPILLARY THYROID CARCINOMA, FOLLICULAR VARIANT. -- TUMOUR SIZE: 4 MM (MAXIMAL). -- ARCHITECTURE: FOLLICULAR. -- CYTOMORPHOLOGY: CLASSICAL. -- HISTOLOGIC GRADE: G1 (WELL DIFFERENTIATED). -- NO TUMOUR CAPSULE IDENTIFIED. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. -- NEGATIVE FOR EXTRATHYROIDAL EXTENSION. -- SURGICAL MARGINS NEGATIVE FOR MALIGNANCY.
Note:
- If it is a completion thyroidectomy and the staging changes one should do a full synoptic report.
Insular carcinoma
General
Features:[53]
- Rare - approximately 5% of all thyroid carcinomas.
- Thought to be a separate tumour from papillary thyroid carcinoma and follicular thyroid carcinoma with a focal insular pattern.
- Some lump this entity with papillary carcinoma, i.e. consider it a variant of papillary thyroid carcinoma.
Microscopic
Features:[53]
- Islands of cells - key feature.
- Scant cytoplasm.
- Nuclei monomorphic and round.
DDx:[54]
- Medullary thyroid carcinoma.
- Poorly differentiated thyroid carcinoma.
Follicular thyroid carcinoma
- AKA follicular carcinoma.
Clinical
Medical school memory device 4 Fs:
- FNA NOT diagnosable.
- Far away mets (sometimes).
- Female predominant.
- Favourable prognosis.
Notes:
- Usu. has a hematologic spread.
- PTC usu. spread via lymphatics.
Microscopic
Features:
- Defined by either:
- Invasion through the capsule:
- Should be all the way through.[55]
- 1/2 does not count.
- Fibrous reaction does not count.
- "Above the contour" does not count.
- Should be all the way through.[55]
- Vascular invasion (all of the following):
- In a small vein (not a capillary), that is outside of the tumour mass.
- Tumour adherent to the side of the vessel.
- Tumour must be re-endothelialized.
- Invasion through the capsule:
Notes:
- Impossible to differentiate from follicular adenoma on FNA (no cytologic differences).
- Described as "over-diagnosed" ... misdiagnoses: PTC follicular variant, follicular adenoma, multinodular goitre with a thick capsule.
Images:
Medullary thyroid carcinoma
- Abbreviated MTC.
General
Medical school memory device - 3 M's:
- aMyloid.
- Median node dissection done.
- MEN IIa syndrome/MEN IIb syndrome.
- Medullary thyroid carcinoma.
- Pheochromocytoma.
- Parathyroid adenoma.
Epidemiology:
- Very rare.
- Poor prognosis.
- May be genetic (MEN IIa/b syndrome).
- Arises from C cells (which produce calcitonin).
Syndromic tumours - typically:[56]
- Present in 30s or 40s.
- +/-Multifocal.
- +/-Bilateral.
- C-cell hyperplasia.
Gross
Features:[56]
- Usu. well-circumscribed.
- White, gray or yellow.
- Gritty.
- Firm.
Image:
Microscopic
Features:
- Nuclei with "neuroendocrine features".
- Small, round nuclei.
- Coarse chromatin (salt and pepper nuclei).
- +/-Amyloid deposits - fluffy appearing acellular eosinophilic material in the cytoplasm.
- +/-C-cell hyperplasia - seen with familial forms of MTC.
- C cells (AKA parafollicular cell): abundant cytoplasm - clear/pale.
Note:
- The amyloid is formed from calcitonin.[57]
Images:
- www:
- WC:
IHC
Features:[58]
- Calcitonin +ve - it arises from C cells (which produce calcitonin).
- Congo-red +ve (amyloid present) - mnemonic: CRAP -- congo red amyloid protein.
- Neuroendocrine markers.
- CEA +ve (often better staining than calcitonin).[59]
- Thyroglobulin usu. -ve.[60]
EM
- Neurosecretory granules.
- Feature seen in neuroendocrine tumours.
Images: Neurosecretory granules (ucsf.edu).
Anaplastic thyroid carcinoma
Epidemiology
- Very rare.
- Horrible prognosis.
- Often presents with obstruction.
- Typically there is a history of a thyroid mass.
Microscopic
Features:
Notes:
- May have features of other thyroid carcinomas, e.g. psammoma bodies, papillae, nuclear changes of PTC.
Image: Anaplastic thyroid carcinoma with a component of papillary thyroid carcinoma (WC).
DDx:
IHC
- Keratin (AE1/AE3) +ve.
- Vimentin +ve, >90%.[61]
- Thyroglobulin - rarely +ve (~15%).[61]
- CEA -ve, calcitonin -ve; to r/o medullary.
- p53 +ve.
- TTF-1 +ve.
Lymphomas of the thyroid
General
- Rare.
- Increased risk with chronic inflammatory conditions.
- Fit in the the greater category of MALT lymphoma.
Microscopic
Features:
- Lymphoepithelial lesion - key feature.
- Plasma cells.
- "Overgrowth" - thyroid parenchyma displaced by lymphocytes.
Weird stuff
Hyalinizing trabecular tumour
- AKA hyalinizing trabecular adenoma.
- Abbreviated HTT.
General
- Considered by some (e.g. Silvia Asa) to be a variant of papillary thyroid carcinoma.[62]
- Behaviour similar to papillary thyroid carcinoma - indolent.
Microscopic
Features:
- Trabecular arrangement of cells.
- May have "curved" trabeculae.
- Extracellular space has hyaline material - key feature.
- Cytoplasm mimics hyaline material in the extracellular space.
DDx:
- Papillary thyroid carcinoma (if one believes this is a separate entity).
- Medullary thyroid carcinoma - not trabecular, nuclei not PTC-like.
- Paraganglioma.[63]
Images
www:
IHC
- Thyroglobulin +ve.
- NSE +ve.
Hürthle cell neoplasm
- AKA oncocytic neoplasm.
- Also spelled Hurthle cell neoplasm.
General
- Incidence: uncommon.
- This is a general category - includes:
- Hürthle cell adenoma.
- Hürthle cell carcinoma.
- Some advocate total thyroidectomy for all Hürthle cell neoplasms, as it is difficult to reliably differentiate adenomas and carcinomas.[66]
- It can be understood as a special type of follicular neoplasm (including follicular thyroid adenoma and follicular thyroid carcinoma).[67]
Adenoma vs. carcinoma
Suggestive for carcinoma:[66]
- Male.
- >4 cm
- Adenomas usu. <3 cm.
Definite for carcinoma:[66]
- Lymphovascular invasion.
- Capsular invasion.
Gross
- Yellow.
- Encapsulated.
Microscopic
Features:[67]
- Oncocytes >= 75% of cells:
- Abundant granular, eosinophilic cytoplasm.
- Round regular nucleus +/- prominent nucleolus.
- +/-Degenerative changes.
Negatives:
- Lack nuclear features of papillary thyroid carcinoma.
- Lack features of medullary thyroid carcinoma.
DDx:[68]
- Papillary thyroid carcinoma oncocytic variant.
- Medullary thyroid carcinoma oncocytic variant.
- Others.
Minocycline associated thyroid pigmentation
- AKA minocycline thyroid.
General
- Benign pigmentation of the thyroid due to minocycline, an antibiotic.
- Reported at other sites, e.g. heart valves,[69] coronary arteries.
Gross
- Black thyroid.[70]
Images:
- Pigmented thyroid gland (rheumatology.org).
- Minocycline thyroid - gross and microscopic (archivesofpathology.org).[71]
Microscopic
Features:
- Granular yellow blobs:
- Location:
- Intracytoplasmic in the follicule-lining cells, i.e. follicular cells.
- Intrafollicular.
- Variable size ~0.5-4 micrometers.
- Location:
Notes:
- Pigment described as lipofuscin-like.[72]
Images:
- Pigmentation due to minocycline (flylib.com).[73]
- Minocycline thyroid - gross and microscopic (archivesofpathology.org).[71]
Stains
- Fontana-Masson stain +ve.[69]
See also
References
- ↑ BEC. 20 October 2009.
- ↑ JOHNSON, RW.; SAHA, NC. (Jun 1962). "The so-called lateral aberrant thyroid.". Br Med J 1 (5293): 1668-9. PMC 1958877. PMID 14452106. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1958877/.
- ↑ Escofet, X.; Khan, AZ.; Mazarani, W.; Woods, WG. (Jan 2007). "Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant?". J R Soc Promot Health 127 (1): 45-6. PMID 17319317.
- ↑ URL: http://radiopaedia.org/articles/lymph-node-levels-of-the-neck. Accessed on: 5 November 2012.
- ↑ SR. 17 January 2011.
- ↑ 6.0 6.1 Rydlova, M.; Ludvikova, M.; Stankova, I. (Jun 2008). "Potential diagnostic markers in nodular lesions of the thyroid gland: an immunohistochemical study.". Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 152 (1): 53-9. PMID 18795075.
- ↑ Papotti, M.; Rodriguez, J.; De Pompa, R.; Bartolazzi, A.; Rosai, J. (Apr 2005). "Galectin-3 and HBME-1 expression in well-differentiated thyroid tumors with follicular architecture of uncertain malignant potential.". Mod Pathol 18 (4): 541-6. doi:10.1038/modpathol.3800321. PMID 15529186.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 331. ISBN 978-0781765275.
- ↑ 9.0 9.1 9.2 9.3 Reis-Filho JS, Preto A, Soares P, Ricardo S, Cameselle-Teijeiro J, Sobrinho-Simões M (January 2003). "p63 expression in solid cell nests of the thyroid: further evidence for a stem cell origin". Mod. Pathol. 16 (1): 43–8. doi:10.1097/01.MP.0000047306.72278.39. PMID 12527712. http://www.nature.com/modpathol/journal/v16/n1/full/3880708a.html.
- ↑ Ozaki, O.; Ito, K.; Sugino, K.; Yasuda, K.; Yamashita, T.; Toshima, K.. "Solid cell nests of the thyroid gland: precursor of mucoepidermoid carcinoma?". World J Surg 16 (4): 685-8; discussion 688-9. PMID 1413837.
- ↑ Prichard, RS.; Lee, JC.; Gill, AJ.; Sywak, MS.; Fingleton, L.; Robinson, BG.; Sidhu, SB.; Delbridge, LW. (Feb 2012). "Mucoepidermoid carcinoma of the thyroid: a report of three cases and postulated histogenesis.". Thyroid 22 (2): 205-9. doi:10.1089/thy.2011.0276. PMID 22224821.
- ↑ 12.0 12.1 12.2 Mizukami Y, Nonomura A, Michigishi T, et al. (February 1994). "Solid cell nests of the thyroid. A histologic and immunohistochemical study". Am. J. Clin. Pathol. 101 (2): 186–91. PMID 7509563.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 36. ISBN 978-0443066856.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 51. ISBN 978-0443066856.
- ↑ SR. 17 January 2011.
- ↑ Massart, C.; Gibassier, J.; d'Herbomez, M. (Sep 2009). "Clinical value of M22-based assays for TSH-receptor antibody (TRAb) in the follow-up of antithyroid drug treated Graves' disease: comparison with the second generation human TRAb assay.". Clin Chim Acta 407 (1-2): 62-6. doi:10.1016/j.cca.2009.06.033. PMID 19576193.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 30. ISBN 978-0443066856.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/enfrm.html. Accessed on: 4 December 2011.
- ↑ 19.0 19.1 19.2 19.3 Lloyd, Ricardo V. (2002). Endocrine Diseases (AFIP Atlas of Nontumor Pathology). Toronto: American Registry of Pathology. ISBN 978-1881041733. http://www.amazon.com/Endocrine-Diseases-Atlas-Nontumer-Pathology/dp/1881041735.
- ↑ Szczepanek-Parulska, E.; Zybek, A.; Biczysko, M.; Majewski, P.; Ruchała, M. (2012). "What might cause pain in the thyroid gland? Report of a patient with subacute thyroiditis of atypical presentation.". Endokrynol Pol 63 (2): 138-42. PMID 22538753.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 559. ISBN 978-0781740517.
- ↑ 22.0 22.1 Fatourechi, MM.; Hay, ID.; McIver, B.; Sebo, TJ.; Fatourechi, V. (Jul 2011). "Invasive fibrous thyroiditis (Riedel thyroiditis): the Mayo Clinic experience, 1976-2008.". Thyroid 21 (7): 765-72. doi:10.1089/thy.2010.0453. PMID 21568724.
- ↑ 23.0 23.1 Poropatich C, Marcus D, Oertel YC (1994). "Hashimoto's thyroiditis: fine-needle aspirations of 50 asymptomatic cases". Diagn. Cytopathol. 11 (2): 141–5. PMID 7813361. http://www3.interscience.wiley.com/journal/112701408/abstract?CRETRY=1&SRETRY=0.
- ↑ Ohye, H.; Fukata, S.; Hirokawa, M. (Nov 2007). "[Malignant lymphoma of the thyroid].". Nihon Rinsho 65 (11): 2092-8. PMID 18018576.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 672. ISBN 978-1416025887.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 560. ISBN 978-0781740517.
- ↑ 27.0 27.1 Machens A, Hoffmann F, Sekulla C, Dralle H (December 2009). "Importance of gender-specific calcitonin thresholds in screening for occult sporadic medullary thyroid cancer". Endocr. Relat. Cancer 16 (4): 1291–8. doi:10.1677/ERC-09-0136. PMID 19726541. http://erc.endocrinology-journals.org/cgi/content/full/16/4/1291.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Thyroid_11protocol.pdf. Accessed on: 7 April 2012.
- ↑ SR. 17 January 2011.
- ↑ Guyétant, S.; Josselin, N.; Savagner, F.; Rohmer, V.; Michalak, S.; Saint-André, JP. (Aug 2003). "C-cell hyperplasia and medullary thyroid carcinoma: clinicopathological and genetic correlations in 66 consecutive patients.". Mod Pathol 16 (8): 756-63. doi:10.1097/01.MP.0000081727.75778.0C. PMID 12920219.
- ↑ URL: http://www.forpath.org/workshops/0201/html/case_7.asp. Accessed on: 21 May 2013.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 564. ISBN 978-0781740517.
- ↑ Sethom, A.; Riahi, I.; Riahi, K.; Akkari, K.; Benzarti, S.; Miled, I.; Chebbi, MK. (Jan 2011). "[Management of thyroid microcarcinoma. Report of 13 cases].". Tunis Med 89 (1): 23-5. PMID 21267823.
- ↑ Hay, ID.; Thompson, GB.; Grant, CS.; Bergstralh, EJ.; Dvorak, CE.; Gorman, CA.; Maurer, MS.; McIver, B. et al. (Aug 2002). "Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients.". World J Surg 26 (8): 879-85. doi:10.1007/s00268-002-6612-1. PMID 12016468.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 565. ISBN 978-0781740517.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 566. ISBN 978-0781740517.
- ↑ Baloch, ZW.; LiVolsi, VA. (Jun 2006). "Cytologic and architectural mimics of papillary thyroid carcinoma. Diagnostic challenges in fine-needle aspiration and surgical pathology specimens.". Am J Clin Pathol 125 Suppl: S135-44. PMID 16830963.
- ↑ 38.0 38.1 38.2 38.3 38.4 Gonzalez-Gonzalez, R.; Bologna-Molina, R.; Carreon-Burciaga, RG.; Gómezpalacio-Gastelum, M.; Molina-Frechero, N.; Salazar-Rodríguez, S. (2011). "Papillary thyroid carcinoma: differential diagnosis and prognostic values of its different variants: review of the literature.". ISRN Oncol 2011: 915925. doi:10.5402/2011/915925. PMC 3302055. PMID 22432054. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3302055/.
- ↑ URL: http://emedicine.medscape.com/article/849000-overview#a0104. Accessed on: 1 May 2012.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 505. ISBN 978-0781779425.
- ↑ Urano M, Kiriyama Y, Takakuwa Y, Kuroda M (April 2009). "Tall cell variant of papillary thyroid carcinoma: Its characteristic features demonstrated by fine-needle aspiration cytology and immunohistochemical study". Diagn. Cytopathol.. doi:10.1002/dc.21086. PMID 19373912.
- ↑ 42.0 42.1 Ghossein R, Livolsi VA (November 2008). "Papillary thyroid carcinoma tall cell variant". Thyroid 18 (11): 1179–81. doi:10.1089/thy.2008.0164. PMID 18925842.
- ↑ S. Raphael. 17 January 2011.
- ↑ 44.0 44.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 506. ISBN 978-0781779425.
- ↑ Daniels, GH.. "What if many follicular variant papillary thyroid carcinomas are not malignant? A review of follicular variant papillary thyroid carcinoma and a proposal for a new classification.". Endocr Pract 17 (5): 768-87. doi:10.4158/EP10407.RA. PMID 21940284.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 88. ISBN 978-0443066856.
- ↑ URL: http://www.thyroidcancercanada.org/types-of-thyroid-cancer.php?lang=en. Accessed on: 9 January 2013.
- ↑ Groen EJ, Roos A, Muntinghe FL, et al. (September 2008). "Extra-intestinal manifestations of familial adenomatous polyposis". Ann. Surg. Oncol. 15 (9): 2439–50. doi:10.1245/s10434-008-9981-3. PMC 2518080. PMID 18612695. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518080/?tool=pubmed.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1122. ISBN 978-1416031215.
- ↑ Hirokawa, M.; Kuma, S.; Miyauchi, A.; Qian, ZR.; Nakasono, M.; Sano, T.; Kakudo, K.. "Morules in cribriform-morular variant of papillary thyroid carcinoma: Immunohistochemical characteristics and distinction from squamous metaplasia.". APMIS 112 (4-5): 275-82. doi:10.1111/j.1600-0463.2004.apm11204-0508.x. PMID 15233643.
- ↑ Mataraci, EA.; Ozgüven, BY.; Kabukçuoglu, F. (Mar 2012). "Expression of cytokeratin 19, HBME-1 and galectin-3 in neoplastic and nonneoplastic thyroid lesions.". Pol J Pathol 63 (1): 58-64. PMID 22535608.
- ↑ Adeniran, AJ.; Zhu, Z.; Gandhi, M.; Steward, DL.; Fidler, JP.; Giordano, TJ.; Biddinger, PW.; Nikiforov, YE. (Feb 2006). "Correlation between genetic alterations and microscopic features, clinical manifestations, and prognostic characteristics of thyroid papillary carcinomas.". Am J Surg Pathol 30 (2): 216-22. PMID 16434896.
- ↑ 53.0 53.1 Rufini V, Salvatori M, Fadda G, et al. (September 2007). "Thyroid carcinomas with a variable insular component: prognostic significance of histopathologic patterns". Cancer 110 (6): 1209–17. doi:10.1002/cncr.22913. PMID 17665497.
- ↑ Endo. fellow. 17 September 2009.
- ↑ SR. 17 January 2011.
- ↑ 56.0 56.1 Nosé, V. (Apr 2011). "Familial thyroid cancer: a review.". Mod Pathol 24 Suppl 2: S19-33. doi:10.1038/modpathol.2010.147. PMID 21455198.
- ↑ Khurana, R.; Agarwal, A.; Bajpai, VK.; Verma, N.; Sharma, AK.; Gupta, RP.; Madhusudan, KP. (Dec 2004). "Unraveling the amyloid associated with human medullary thyroid carcinoma.". Endocrinology 145 (12): 5465-70. doi:10.1210/en.2004-0780. PMID 15459123.
- ↑ URL: http://pathologyoutlines.com/thyroid.html#medullary. Accessed on: 17 January 2011.
- ↑ SB. 7 January 2010.
- ↑ de Micco, C.; Chapel, F.; Dor, AM.; Garcia, S.; Ruf, J.; Carayon, P.; Henry, JF.; Lebreuil, G. (Mar 1993). "Thyroglobulin in medullary thyroid carcinoma: immunohistochemical study with polyclonal and monoclonal antibodies.". Hum Pathol 24 (3): 256-62. PMID 8454270.
- ↑ 61.0 61.1 Ordóñez NG, El-Naggar AK, Hickey RC, Samaan NA (July 1991). "Anaplastic thyroid carcinoma. Immunocytochemical study of 32 cases". Am. J. Clin. Pathol. 96 (1): 15–24. PMID 1712540.
- ↑ Cheung CC, Boerner SL, MacMillan CM, Ramyar L, Asa SL (December 2000). "Hyalinizing trabecular tumor of the thyroid: a variant of papillary carcinoma proved by molecular genetics". Am. J. Surg. Pathol. 24 (12): 1622–6. PMID 11117782.
- ↑ URL: http://path.upmc.edu/cases/case465/dx.html. Accessed on: 17 January 2011.
- ↑ Baloch, ZW.; Puttaswamy, K.; Brose, M.; LiVolsi, VA. (2006). "Lack of BRAF mutations in hyalinizing trabecular neoplasm.". Cytojournal 3: 17. doi:10.1186/1742-6413-3-17. PMID 16867191.
- ↑ URL: http://www.ispub.com/journal/the-internet-journal-of-endocrinology/volume-2-number-1/hyalinizing-trabecular-neoplasm-of-the-thyroid-controversies-in-management.html. Accessed on: 1 January 2012.
- ↑ 66.0 66.1 66.2 Wasvary, H.; Czako, P.; Poulik, J.; Lucas, R. (Aug 1998). "Unilateral lobectomy for Hurthle cell adenoma.". Am Surg 64 (8): 729-32; discussion 732-3. PMID 9697901.
- ↑ 67.0 67.1 Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 104. ISBN 978-0443066856.
- ↑ Montone KT, Baloch ZW, LiVolsi VA (August 2008). "The thyroid Hürthle (oncocytic) cell and its associated pathologic conditions: a surgical pathology and cytopathology review". Arch. Pathol. Lab. Med. 132 (8): 1241–50. PMID 18684023.
- ↑ 69.0 69.1 Sant'Ambrogio, S.; Connelly, J.; DiMaio, D.. "Minocycline pigmentation of heart valves.". Cardiovasc Pathol 8 (6): 329-32. PMID 10615019.
- ↑ Noble, JG.; Christmas, TJ.; Chapple, C.; Katz, D.; Milroy, EJ. (Jan 1989). "The black thyroid: an unusual finding during neck exploration.". Postgrad Med J 65 (759): 34-5. PMC 2429157. PMID 2780449. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2429157/.
- ↑ 71.0 71.1 Raghavan, R.; Snyder, WH.; Sharma, S. (Mar 2004). "Pathologic quiz case: tumor in pigmented thyroid gland in a young man. Papillary thyroid carcinoma in a minocycline-induced, diffusely pigmented thyroid gland.". Arch Pathol Lab Med 128 (3): 355-6. doi:10.1043/1543-2165(2004)128355:PQCTIP2.0.CO;2. PMID 14987144.
- ↑ Gordon, G.; Sparano, BM.; Kramer, AW.; Kelly, RG.; Iatropoulos, MJ. (Oct 1984). "Thyroid gland pigmentation and minocycline therapy.". Am J Pathol 117 (1): 98-109. PMC 1900569. PMID 6435454. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1900569/.
- ↑ URL: http://flylib.com/books/en/2.953.1.50/1/. Accessed on: 11 March 2012.