Difference between revisions of "Testis"
m (→Images) |
|||
| Line 408: | Line 408: | ||
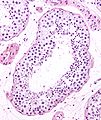
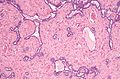
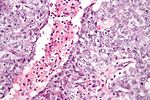
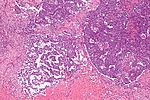
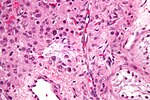
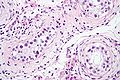
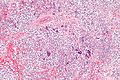
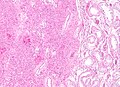
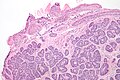
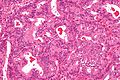
Image:Seminoma_high_mag.jpg |Seminoma - high mag. (WC/Nephron) | Image:Seminoma_high_mag.jpg |Seminoma - high mag. (WC/Nephron) | ||
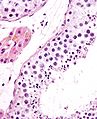
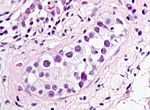
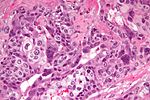
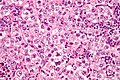
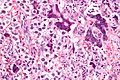
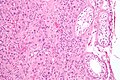
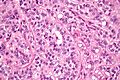
Image:Seminoma_intermed_mag.jpg |Seminoma - intermed. mag. (WC/Nephron) | Image:Seminoma_intermed_mag.jpg |Seminoma - intermed. mag. (WC/Nephron) | ||
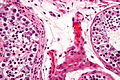
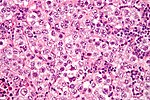
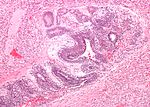
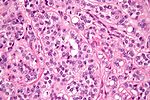
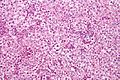
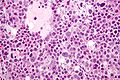
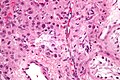
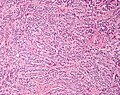
Image:Rete_testis_with_seminoma.jpg |Seminoma in the rete testis (WC/Nephron) | Image:Rete_testis_with_seminoma.jpg |Seminoma in the rete testis. (WC/Nephron) | ||
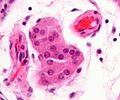
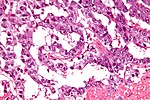
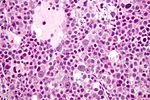
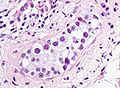
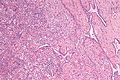
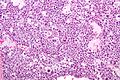
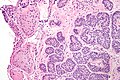
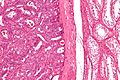
Image:Seminoma_with_syncytiotrophoblasts_-_intermed_mag.jpg |Seminoma with syncytiotrophoblasts - intermed. mag. (WC/Nephron) | Image:Seminoma_with_syncytiotrophoblasts_-_intermed_mag.jpg |Seminoma with syncytiotrophoblasts - intermed. mag. (WC/Nephron) | ||
Image:Seminoma_with_syncytiotrophoblasts_-_very_high_mag.jpg |Seminoma with syncytiotrophoblasts - very high mag. (WC/Nephron) | Image:Seminoma_with_syncytiotrophoblasts_-_very_high_mag.jpg |Seminoma with syncytiotrophoblasts - very high mag. (WC/Nephron) | ||
</gallery> | </gallery> | ||
===IHC=== | ===IHC=== | ||
*D2-40 +ve ~100% of cases.<ref name=pmid17277761>{{Cite journal | last1 = Lau | first1 = SK. | last2 = Weiss | first2 = LM. | last3 = Chu | first3 = PG. | title = D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30. | journal = Mod Pathol | volume = 20 | issue = 3 | pages = 320-5 | month = Mar | year = 2007 | doi = 10.1038/modpathol.3800749 | PMID = 17277761 }}</ref> | *D2-40 +ve ~100% of cases.<ref name=pmid17277761>{{Cite journal | last1 = Lau | first1 = SK. | last2 = Weiss | first2 = LM. | last3 = Chu | first3 = PG. | title = D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30. | journal = Mod Pathol | volume = 20 | issue = 3 | pages = 320-5 | month = Mar | year = 2007 | doi = 10.1038/modpathol.3800749 | PMID = 17277761 }}</ref> | ||
Revision as of 03:14, 19 May 2013
The testis, plural testes, are important for survival of the species. Tumours occasionally arise in 'em. They generally are not biopsied.
If the testis is biopsied, it is usually for fertility -- to understand whether the man is really azoospermic.
Normal testis
Gross
Anatomy - deep to superficial:
- Tunica albuginea - fibrous layer.
- Tunica vaginalis - thin mesothelial layer.
Microscopic
Seminiferous tubules
- Sertoli cells (AKA sustentacular cell AKA nurse cell).
- Large cells with oval nucleus.
- Primary spermatocyte.
- Small cells with dark nucleus on basement membrane.
- Secondary spermatocyte.
- Rarely seen on light microscopy.
- Spermatids.
- Round small.
- Usually close to the centre of the lumen.
- Spermatozoa.
- You don't see the tail on light microscopy.
Images
Interstitial
- Leydig cell (AKA interstitial cell).
- Large eosinophilic cell.
- Blood vessels.
Image
Associated structures
- Epididymis - stores the sperm.
- Pseudostratified epithelium with cilia.
Image:
Rete testis
- Receives stuff from the tubules.
- Very rarely give rise to an adenocarcinoma of the rete testis.
- May be involved by seminoma - increases risk of relapse in a univariate analysis.[1]
Microscopic:
- Delicate anastomosing channels lined by cuboid epithelium.
Images
www:
Appendix of testis
Muellerian duct remnant.
Microscopic:
- Polypoid structure.
Images:
Sign out
TESTICLE, RIGHT, ORCHIECTOMY: - TESTICLE WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR INTRATUBULAR GERM CELL NEOPLASIA. - NEGATIVE FOR MALIGNANCY.
Diagnoses (overview)
- Benign.
- Spermatid present/not present.
- Infertility - azoospermic.
- No sperm present.
- Germ cell tumours (GCTs).
- Intratubular germ cell neoplasia.
- Seminoma.
- Spermatocytic seminoma.
- Yolk sac tumour (endodermal sinus tumour).
- Embryonal carcinoma.
- Choriocarcinoma.
- Teratoma.
- Mixed GCT - 60% of GCTs are mixed.
- Common combinations:
- teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- seminoma + embryonal (SE).
- embryonal + teratoma (TE).
- Common combinations:
- Sex-cord stromal tumour.
- Leydig cell tumour.
- Sertoli cell tumour.
IHC for GCTs
ABCDs of GCTs:
- AFP - yolk sac tumour.
- Beta-hCG - choriocarcinoma.
- CD30 - embryonal carcinoma.
- D2-40 - seminoma.
Tabular summary of GCTs
| Tumour | Key feature | Microscopic | IHC | Other | Image |
|---|---|---|---|---|---|
| Intratubular germ cell neoplasia (ITGCN) | nests of small fried egg cells | large central nucleus, clear cytoplasm, round or polygonal nuclear membrane, nucleoli[2] |
CD117 | appearance similar to seminoma | |
| Seminoma | fried egg cells | fried egg-like cells (central nucleus, clear cytoplasm) with squared-off nuclear membrane, nucleoli, lymphocytic infiltrate, granulomata, syncytiotrophoblastic giant cells[3] |
D2-40 | Dysgerminoma = female version of this tumour | |
| Yolk sac tumour (endodermal sinus tumour) | Schiller-Duval bodies | Schiller-Duval b. = central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells, variable arch. | AFP | patterns: microcystic, solid, hepatoid | |
| Embryonal carcinoma | prominent nucleoli, vescicular nuclei | var. arch.: tubulopapillary, glandular, solid, embryoid bodies (ball of cells in surrounded by empty space on three sides), +/-nuclear overlap, mitoses common | CD30 | usu. part of a mixed GCT | |
| Choriocarcinoma | marked nuclear atypia | cells with clear cytoplasm (cytotrophoblast), multinucleated cells (syncytiotrophoblast) | beta-hCG | not commonly pure, usu. a component of a mixed GCT | |
| Teratoma | skin, GI tract-like epithelium | skin (epidermis, adnexal structures - sebaceous glands, hair follicles), GI tract-like glands (simple tall columnar epithelium), fat +/-primitive neuroepithelium (pseudostratified epithelium in rosettes) | None | testicular teratomas in post-pubertal males are all considered malignant[4] | |
| Spermatocytic seminoma | population of 3 cells | pop.: (1) small cell with high NC ratio (mature lymphocyte-like), (2) medium with nucleoli, (3) large cells with filamentous chromatin - few present | ? | does not arise from ITGCN, no lymphocytic infiltrate (like in seminoma) | |
| Mixed germ cell tumour | NA | common combinations: teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE); seminoma + embryonal (SE); embryonal + teratoma (TE) | NA | - |
Tabular summary of (male) SCSTs
| Tumour | Key feature | Microscopic | IHC | Other | Image |
|---|---|---|---|---|---|
| Leydig cell tumour | intersitial cell cluster with eosinophilic cytoplasm | cytoplasmic vacuolization, uniform nuclei with nucleoli | MART-1, calretinin, inhibin | +/-Reinke crystals (cylindrical crystalloid eosinophilic cytoplasmic bodies) | |
| Sertoli cell tumour | cells in cords or trabeculae | light staining bubbly cytoplasm +/- large cytoplasmic vacuoles, granular chromatin | ? | usu. no significant nuclear atypia, no mitoses |
Benign
Testicular atrophy
- Cryptorchidism redirects here.
General
- Microscopic appearance identical to cryptorchidism (undescended testis).[5]
Gross
- Decreased size.
Microscopic
Features:[5]
- Thickening of seminiferous tubule basement membrane.
- Intertubular fibrosis.
- Decreased sperm/no sperm present.
Note:
- End-stage testicle - only has Sertoli cell within the seminiferous tubules.
Image:
Sign out
TESTICLE, RIGHT, ORCHIECTOMY: - ATROPHIC TESTICLE. - NEGATIVE FOR INTRATUBULAR GERM CELL NEOPLASIA. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show seminiferous tubules surrounded by thick hyaline sleeves. In a large number of sections only Sertoli cells are found in the tubules.
In some sections poorly defined paucicellular tubular structures reminiscent of seminiferous tubules composed of hyaline material are present; these probably represent obsolete seminiferous tubules. Focally, fibrosis is seen without definite tumour outlines. There is no significant inflammation. The rete testis is identified.
Rare seminiferous tubules have spermatid within. The germ cells seen do not have appreciable nuclear atypia.
Numerous small Leydig cell clusters are seen in some sections.
Spermatocele
General
- Benign.
- Cyst of the epididymis (classic).
- May arise in the rete testis or vas deferens.[6]
Clinical:
- Often asymptomatic.
- Excised due to pain or mass effect.[7]
Microscopic
Features:
- Cyst lined by a simple ciliated epithelium.
- Contain sperm.
- Head: ~1/2 the size of a RBC, black.
- Tail: infrequently seen.
Note:
- Small cellular clusters may be present.
- May mimic small cell carcinoma.[8]
DDx:
- Hydrocele testis - do not contain sperm.
Images
www:
Hydrocele testis
- AKA hydrocele.
General
- Benign.
Clinical:
- Scrotal mass.
Microscopic
Features:
- Cyst lined by a simple ciliated epithelium.
- Does not contain sperm.
DDx:
- Spermatocele - contains sperm.
Idiopathic granulomatous orchitis
- Granulomatous orchitis redirects here.
General
- Rare.
- Unknown etiology -- possibly trauma + immune reaction to sperm.[9]
Microscopic
Features:[9]
- Granulomas +/- necrosis.
- +/-Destruction of seminiferous tubules.
- Prominent collagen fibrosis.
DDx:
- ITGCN.
- Seminoma.
- Tertiary syphilis - classically, plasma cell rich.[10]
- Syphilis, unlike other infections of the GU tract, is said to affect the testis before the epididymis.[11]
- Tuberculosis.
- Lymphoma.[9]
- Malakoplakia.[9]
Stains
- AFB -ve -- for tuberculosis.
- Dieterle stain -ve -- for syphilis.
Premalignant
Intratubular germ cell neoplasia
- Abbreviated ITGCN.
General
- Considered the precursor lesion for germ cell tumours.
- Not all germ cell tumours (GCTs) arise from intratubular germ cell neoplasia.
The following testicular GCTs do not arise from ITGCN:
- Spermatocytic seminoma.[12]
- Yolk sac tumours (endodermal sinus tumour).[13]
- Teratoma.[citation needed]
Classification:[14]
- Undifferentiated ITGCN.
- Differentiated ITGCN.[15]
- Intratubular embryonal carcinoma.
- Intratubular seminoma.
Microscopic
- "Large" round or polygonal nuclei.
- Size in relation to normal often not defined.
- Rakheja et al. say >= 5x a lymphocyte for intratubular embryonal carcinoma.[14]
- Polygonal nuclei = squared-off nuclear membrane.
- Size in relation to normal often not defined.
- Prominent nucleoli - key feature.
- Clear cytoplasm.
- +/-Cells fill the tubule.
DDx:
- Sertoli cell-only syndrome - Sertoli cells also have nucleoli, wind swept appearance.[18]
Images
www:
IHC
Features:[19]
- PLAP +ve.[20]
- CD117 +ve.
- Disputed: doesn't differentiate neoplastic from non-neoplastic according to Biermann et al.[21]
- OCT3/4 +ve.
Note:
- Normal testis PLAP -ve, CD117 -ve.[22]
Germ cell tumours
Seminoma
- Should not be confused with the unrelated tumour called spermatocytic seminoma.
General
- Male counterpart of the dysgerminoma, which arise in the ovary.
- Most common germ cell tumour of the testis.
Clinical:
- Elevated serum LDH.
- Normal serum alpha fetoprotein.
- Usually normal beta-hCG.
Note:
- Rarely, it may present a retroperitoneal mass.[23]
Epidemiology & etiology
- Arises from intratubular germ cell neoplasia (ITGCN).
Microsopic
Features:
- Cells with fried egg appearance - key feature:
- Clear cytoplasm.
- Central nucleus, with prominent nucleolus.
- Nucleus may have "corners", i.e. it is not round.
- +/-Lymphoctyes - interspersed (very common).
- +/-Syncytiotrophoblasts, AKA syncytiotrophoblastic giant cells (STGCs),[3] present in ~10-20% of seminoma.[24]
- Large + irregular, vesicular nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- Syncytiotrophoblasts = closest to mom in normal chorionic villi - covers cytotrophoblast.[25]
- +/-Florid granulomatous reaction.
Memory device: 3 Cs - clear cytoplasm, central nucleus, corners on the nuclear membrane.
DDx:
- Embryonal carcinoma.
- Solid variant of yolk sac tumour.
- Lacks fibrous septae and lymphocytes.[26]
- Mixed germ cell tumour.
- Choriocarcinoma - esp. if (multinucleated) syncytiotrophoblasts are present.[27]
- Granulomatous orchitis - if granulomas are present.
Images
IHC
- D2-40 +ve ~100% of cases.[28]
- CD117 +ve (ckit) ~92% of cases.[28]
- CD30 -ve.[29]
- Done to r/o embryonal carcinoma.
- Cytokeratins usu. -ve, may have weak focal positivity.[29]
- OCT3/4 +ve.[30]
Sign out
RETROPERITONEAL SOFT TISSUE, RIGHT, CORE BIOPSY: - SEMINOMA.
Micro
The sections show large atypical, discohesive cells with prominent nucleoli, central nuclei and moderate clear cytoplasm, intermixed with mature lymphocytes. Mitotic activity is present.
Small biopsy
A mixed germ cell tumour cannot be excluded; given the small quantity of tumour, this biopsy is at a high risk for having undersampled other tumour components should they be present. Correlation with serology and consideration of re-biopsy is suggested.
Spermatocytic seminoma
General
- Rare tumour.
- Only one case of metastases in 200 cases.[31]
- Orchiectomy is curative.
- Not reported/found in females.[31]
- Typically older - mean age 50s.[31]
Epidemiology
- Does NOT arise from intratubular germ cell neoplasia (ITGCN)[32] - not considered a subtype of seminoma.
Microscopic
Features:[33]
- Population of three cells.
- Mucoid lakes.
- Intratubular spread.
Notes:
- Spireme = the tangle of filaments in prophase portion of mitosis.[34]
- May have eosinophilic cytoplasm (dependent on lab).
- Usually larger than Leydig cell tumour.
DDx:
Images
IHC
Features:[35]
- PLAP -ve (0 positive/17).
- CD117 -ve (7 positive/17).
- CAM5.2 -ve (1 positive/17).
Yolk sac tumour
- Most common GCT in infants and young boys.
Microscopic
Classic feature:
- Schiller-Duval bodies.
- Look like glomerulus - central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells
- Architecure - variable.
- Most common microcystic pattern.[36]
Embryonal carcinoma
These often look like a poorly differentiated carcinoma.
General
- Affects young adults.
- May be seen in women.
Microscopic
Features:[37]
- Nucleoli - key feature.
- Vesicular nuclei (clear, empty appearing nuclei) - key feature.
- Nuclei overlap.
- Necrosis - common.
- Not commonly present in seminoma.
- Indistinct cell borders
- Mitoses - common.
- Variable architecture:
- Tubulopapillary.
- Glandular.
- Solid.
- Embryoid bodies - ball of cells in surrounded by empty space on three sides.
Notes:
- Cytoplasmic staining variable (eosinophilic to basophilic).
Choriocarcinoma
These are aggressive tumours.
Microscopic
Features:
- Syncytiotrophoblasts:
- Large + many irreg. or lobular hyperchromatic nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- Cytotrophoblasts:
- Clear cytoplasm.
- Polygonal shaped cells in cords/masses.
- Distinct cell borders.
- Single uniform nucleus.
- +/-Hemorrhage.
- +/-Necrosis.
Teratoma of the testis
In post-pubertal males these (testicular) tumours are considered malignant. They usually consist of all three germ layers.[38]
Sex cord stromal tumours
Leydig cell tumour
- AKA interstitial cell tumour.
General
- Arises from interstitial cell.
- May be associated with increased testosterone.
Gross
- Solid, lobulated.
- Red/tan.
Image:
Microscopic
Features:[39]
- Vacuolization (cytoplasm) - key feature.
- Cytoplasm - clear to eosinophilic - important.
- Reinke crystals - classic finding, usually not present.
- Cylindrical crystalloid eosinophilic cytoplasmic bodies.
- Nucleoli common.
- Round nuclei.
DDx:
- Spermatocytic seminoma - may have eosinophilic cytoplasm.
- Pregnancy luteoma - occurs during pregnancy, as the name implies.
Images
www:
IHC
- Inhibin-alpha.
- Calretinin.[40][41]
- Melan A.[42]
- AKA MART-1.
- Expressed in melanoma, adrenal tissue, steroid-secreting tumours.
Sertoli cell nodule
- AKA Pick's adenoma.
- AKA testicular tubular adenoma.
- AKA tubular adenoma of the testis.
General
- Benign proliferation of Sertoli cells - associated with cryptorchidism (undescended testis).
- Not composed of a clonal cell population, i.e. not neoplastic; thus, technically, should not be called an adenoma.[43]
Gross
- Usually an incidental finding, rarely presents as a testicular mass.[44]
Microscopic
- Unencapsulated nodules composed of well-formed tubules.
- May contain eosinophilic (hyaline) blob in lumen (centre).
- Cells - vaguely resemble immature Sertoli cells:
- Bland hyperchromatic oval/round nuclei that are stratified.
DDx:[44]
Images
IHC
Features:[44]
- Alpha-inhibin +ve (5/5 cases).
- OCT3/4 -ve (5/5 cases).
Sertoli cell tumour
General
- Arises from Sertoli cells (AKA nurse cells).
May be seen in several syndrome - esp. if there is calcification:
Microscopic
Features:
- Groups of cells in cords or trabeculae (beam-like arrangement).
- Cells have:
- Light staining bubbly cytoplasm +/- large cytoplasmic vacuoles.
- Slightly irregular nucleoli.
- Granular irregular appearing chromatin.
Negatives:
- Mitoses are rare.
- No significant nuclear atypia.
DDx:
- Granulosa cell tumour - may be very similar. Often has nuclear grooves.
- Epithelioid adenomatoid tumour.
- Sertoli cell nodule.
Images
www:
IHC
- Alpha-inhibin +ve. (???)
Other
These tumours are rare.
Adenocarcinoma of the rete testis
General
- Extremely rare - a few dozen cases in the world literature.[47]
- Possible association of diethylstilbestrol.[47]
Microscopic
Features:
- Adenocarcinoma:
- Tubular or papillary architecture.[47]
- Columnar cells with cigar-shaped nuclei.
Images
See also
References
- ↑ Soper, MS.; Hastings, JR.; Cosmatos, HA.; Slezak, JM.; Wang, R.; Lodin, K. (Dec 2012). "Observation Versus Adjuvant Radiation or Chemotherapy in the Management of Stage I Seminoma: Clinical Outcomes and Prognostic Factors for Relapse in a Large US Cohort.". Am J Clin Oncol. doi:10.1097/COC.0b013e318277d839. PMID 23275274.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 538. ISBN 978-0443066771.
- ↑ 3.0 3.1 Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 542. ISBN 978-0443066771.
- ↑ Carver, BS.; Al-Ahmadie, H.; Sheinfeld, J. (May 2007). "Adult and pediatric testicular teratoma.". Urol Clin North Am 34 (2): 245-51; abstract x. doi:10.1016/j.ucl.2007.02.013. PMID 17484929.
- ↑ 5.0 5.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 506-7. ISBN 978-1416054542.
- ↑ URL: http://emedicine.medscape.com/article/443432-overview. Accessed on: 5 March 2012.
- ↑ Walsh, TJ.; Seeger, KT.; Turek, PJ.. "Spermatoceles in adults: when does size matter?". Arch Androl 53 (6): 345-8. PMID 18357964.
- ↑ Lane, Z.; Epstein, JI. (Jan 2010). "Small blue cells mimicking small cell carcinoma in spermatocele and hydrocele specimens: a report of 5 cases.". Hum Pathol 41 (1): 88-93. doi:10.1016/j.humpath.2009.06.018. PMID 19740515.
- ↑ 9.0 9.1 9.2 9.3 Roy, S.; Hooda, S.; Parwani, AV. (May 2011). "Idiopathic granulomatous orchitis.". Pathol Res Pract 207 (5): 275-8. doi:10.1016/j.prp.2011.02.005. PMID 21458170.
- ↑ Sekita, N.; Nishikawa, R.; Fujimura, M.; Sugano, I.; Mikami, K. (Jan 2012). "[Syphilitic orchitis: a case report].". Hinyokika Kiyo 58 (1): 53-5. PMID 22343746.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 364. ISBN 978-0781765275.
- ↑ Müller J, Skakkebaek NE, Parkinson MC (February 1987). "The spermatocytic seminoma: views on pathogenesis". Int. J. Androl. 10 (1): 147–56. PMID 3583416.
- ↑ Manivel JC, Simonton S, Wold LE, Dehner LP (June 1988). "Absence of intratubular germ cell neoplasia in testicular yolk sac tumors in children. A histochemical and immunohistochemical study". Arch. Pathol. Lab. Med. 112 (6): 641–5. PMID 2837162.
- ↑ 14.0 14.1 14.2 Rakheja, D.; Hoang, MP.; Sharma, S.; Albores-Saavedra, J. (Apr 2002). "Intratubular embryonal carcinoma.". Arch Pathol Lab Med 126 (4): 487-90. doi:10.1043/0003-9985(2002)1260487:IEC2.0.CO;2. PMID 11900581. http://www.archivesofpathology.org/doi/full/10.1043/0003-9985(2002)126%3C0487:IEC%3E2.0.CO;2.
- ↑ Lau, SK.; Weiss, LM.; Chu, PG. (Jul 2007). "Association of intratubular seminoma and intratubular embryonal carcinoma with invasive testicular germ cell tumors.". Am J Surg Pathol 31 (7): 1045-9. doi:10.1097/PAS.0b013e31802b8712. PMID 17592271.
- ↑ URL: http://www.webpathology.com/image.asp?case=30&n=1. Accessed on: 18 May 2010.
- ↑ Gondos, B.; Migliozzi, JA. (Nov 1987). "Intratubular germ cell neoplasia.". Semin Diagn Pathol 4 (4): 292-303. PMID 3328244.
- ↑ URL: http://www.webpathology.com/image.asp?n=3&Case=28. Accessed on: 25 March 2013.
- ↑ Honecker, F.; Stoop, H.; de Krijger, RR.; Chris Lau, YF.; Bokemeyer, C.; Looijenga, LH. (Jul 2004). "Pathobiological implications of the expression of markers of testicular carcinoma in situ by fetal germ cells.". J Pathol 203 (3): 849-57. doi:10.1002/path.1587. PMID 15221945.
- ↑ Schreiber, L.; Lifschitz-Mercer, B.; Paz, G.; Yavetz, H.; Elliott, DJ.; Kula, K.; Slowikowska-Hilczer, J.; Maymon, BB. (Jan 2003). "Double immunolabeling by the RBM and the PLAP markers for identifying intratubular (in situ) germ cell neoplasia of the testis.". Int J Surg Pathol 11 (1): 17-20. PMID 12598912.
- ↑ Biermann, K.; Stoop, H.; Looijenga, L. (May 2012). "c-KIT protein expression does not discriminate neoplastic from non-neoplastic intratubular germ cells.". Histopathology 60 (6): 1017-9. doi:10.1111/j.1365-2559.2011.04157.x. PMID 22340755.
- ↑ Hawkins, E.; Heifetz, SA.; Giller, R.; Cushing, B. (Apr 1997). "The prepubertal testis (prenatal and postnatal): its relationship to intratubular germ cell neoplasia: a combined Pediatric Oncology Group and Children's Cancer Study Group.". Hum Pathol 28 (4): 404-10. PMID 9104938.
- ↑ Preda, O.; Nicolae, A.; Loghin, A.; Borda, A.; Nogales, FF. (2011). "Retroperitoneal seminoma as a first manifestation of a partially regressed (burnt-out) testicular germ cell tumor.". Rom J Morphol Embryol 52 (1): 193-6. PMID 21424055.
- ↑ URL: http://www.webpathology.com/image.asp?case=31&n=10. Accessed on: 22 May 2012.
- ↑ URL: http://upload.wikimedia.org/wikipedia/commons/4/45/Gray37.png. Accessed on: 31 May 2010.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=8. Accessed on: March 8, 2010.
- ↑ Hedinger, C.; von Hochstetter, AR.; Egloff, B. (Jul 1979). "Seminoma with syncytiotrophoblastic giant cells. A special form of seminoma.". Virchows Arch A Pathol Anat Histol 383 (1): 59-67. PMID 157614.
- ↑ 28.0 28.1 Lau, SK.; Weiss, LM.; Chu, PG. (Mar 2007). "D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30.". Mod Pathol 20 (3): 320-5. doi:10.1038/modpathol.3800749. PMID 17277761.
- ↑ 29.0 29.1 Cossu-Rocca, P.; Jones, TD.; Roth, LM.; Eble, JN.; Zheng, W.; Karim, FW.; Cheng, L. (Aug 2006). "Cytokeratin and CD30 expression in dysgerminoma.". Hum Pathol 37 (8): 1015-21. doi:10.1016/j.humpath.2006.02.018. PMID 16867864.
- ↑ Emerson, RE.; Ulbright, TM. (Jun 2010). "Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers.". Pathology 42 (4): 344-55. doi:10.3109/00313021003767355. PMID 20438407.
- ↑ 31.0 31.1 31.2 31.3 Eble JN (October 1994). "Spermatocytic seminoma". Hum. Pathol. 25 (10): 1035–42. PMID 7927308.
- ↑ Müller J, Skakkebaek NE, Parkinson MC (February 1987). "The spermatocytic seminoma: views on pathogenesis". Int. J. Androl. 10 (1): 147–56. doi:10.1111/j.1365-2605.1987.tb00176.x. PMID 3583416.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. ISBN 0-7216-0187-1.
- ↑ URL: http://www.thefreedictionary.com/spireme. Accessed on: 4 June 2010.
- ↑ Kraggerud, SM.; Berner, A.; Bryne, M.; Pettersen, EO.; Fossa, SD. (Mar 1999). "Spermatocytic seminoma as compared to classical seminoma: an immunohistochemical and DNA flow cytometric study.". APMIS 107 (3): 297-302. PMID 10223302.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=1. Accessed on: March 8, 2010.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 549. ISBN 978-0443066771.
- ↑ Moore, Keith L.; Persaud, T.V.N. (2002). The Developing Human: Clinically Oriented Embryology (7th ed.). Saunders. pp. 83. ISBN 978-0721694122.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 581. ISBN 978-0443066771.
- ↑ URL: http://www.antibodybeyond.com/reviews/cell-markers/leydig-cell-marker.htm. Accessed on: 18 May 2010.
- ↑ Bar-Shira Maymon B, Yavetz H, Yogev L, et al. (2005). "Detection of calretinin expression in abnormal immature Sertoli cells in non-obstructive azoospermia". Acta Histochem. 107 (2): 105–12. doi:10.1016/j.acthis.2005.02.002. PMID 15950053.
- ↑ Yao DX, Soslow RA, Hedvat CV, Leitao M, Baergen RN (September 2003). "Melan-A (A103) and inhibin expression in ovarian neoplasms". Appl. Immunohistochem. Mol. Morphol. 11 (3): 244–9. PMID 12966351.
- ↑ 43.0 43.1 Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 227. ISBN 978-0470519035.
- ↑ 44.0 44.1 44.2 Vallangeon, BD.; Eble, JN.; Ulbright, TM. (Dec 2010). "Macroscopic sertoli cell nodule: a study of 6 cases that presented as testicular masses.". Am J Surg Pathol 34 (12): 1874-80. doi:10.1097/PAS.0b013e3181fcab70. PMID 21107095.
- ↑ Ricco R, Bufo P (October 1980). "[Histologic study of 3 cases of so-called tubular adenoma of the testis]" (in Italian). Boll. Soc. Ital. Biol. Sper. 56 (20): 2110–5. PMID 6109541.
- ↑ Libé, R.; Horvath, A.; Vezzosi, D.; Fratticci, A.; Coste, J.; Perlemoine, K.; Ragazzon, B.; Guillaud-Bataille, M. et al. (Jan 2011). "Frequent phosphodiesterase 11A gene (PDE11A) defects in patients with Carney complex (CNC) caused by PRKAR1A mutations: PDE11A may contribute to adrenal and testicular tumors in CNC as a modifier of the phenotype.". J Clin Endocrinol Metab 96 (1): E208-14. doi:10.1210/jc.2010-1704. PMID 21047926.
- ↑ 47.0 47.1 47.2 Newbold, RR.; Bullock, BC.; McLachlan, JA. (Dec 1986). "Adenocarcinoma of the rete testis. Diethylstilbestrol-induced lesions of the mouse rete testis.". Am J Pathol 125 (3): 625-8. PMC 1888460. PMID 3799821. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888460/.