Difference between revisions of "Basics"
m (→Pathology reports: repl. ref) |
(found by AC - fixed) |
||
| (175 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
==Pathology simplified== | ==Pathology simplified== | ||
===Blue & pink=== | |||
H&E is the standard... | H&E is the standard... | ||
*Too much '''PINK''' = DEAD (necrosis). | *Too much '''PINK''' = DEAD ([[necrosis]]). | ||
*Too much '''BLUE''' = BAD. | *Too much '''BLUE''' = BAD. | ||
In words: | In words: | ||
*''Blue is bad and pink is dead!''<ref> | *''Blue is bad and pink is dead!''<ref>Streutker, C. 8 June 2013.</ref> | ||
Note: | Note: | ||
*Lymph | *There is a lengthy list of things that are blue and ''not'' "bad"... that why a pathology residency is years. | ||
**[[Lymph node]]s are very blue... they aren't necessarily bad. | |||
**Reactive processes can be very blue... they aren't bad. | |||
===Three questions=== | |||
Pathology can be boiled down to: | |||
#What is it? | |||
#*Biopsies. | |||
#Did I get it all? | |||
#*Resections. | |||
#Did I get the right thing? | |||
#*Most other things. | |||
==Terms== | ==Terms== | ||
=== | ===Staining=== | ||
*Eosinophilic - pink. | *Eosinophilic - pink. | ||
*Hyperchromatic - blue. | *Hyperchromatic - blue. | ||
*Amphophilic - ''bluish-red'' colour when referring to H&E stained section.<ref>URL:[http://pancreaticcancer2000.com/page1.htm http://pancreaticcancer2000.com/page1.htm]. Accessed on: 3 June 2010.</ref> | |||
**''Amphophilic'' means stains with both acidic & basic dyes. | |||
* | **Images: [http://pancreaticcancer2000.com/immunoblast1.jpg amphophilic material - arrow (pancreaticcancer2000.com)], [http://www.webpathology.com/image.asp?n=4&Case=20 amphophilic cytoplasm in prostate carcinoma (webpathology.com)]. | ||
*''Argyrophilic'' means has an affinity for silver<ref>URL: [http://www.merriam-webster.com/medical/argyrophilic http://www.merriam-webster.com/medical/argyrophilic]. Accessed on: 29 August 2011.</ref><ref>URL: [http://en.wiktionary.org/wiki/argyrophilic http://en.wiktionary.org/wiki/argyrophilic]. Accessed on: 29 August 2011.</ref>/loves silver/stains with silver. | |||
**Images: [http:// | ===Morphologic patterns=== | ||
* | {{Main|Morphologic patterns}} | ||
This covers things like ''cribriform'', ''hobnail'', ''herring bone'' and many others. | |||
===Nuclear destruction words=== | ===Nuclear destruction words=== | ||
| Line 30: | Line 43: | ||
Image: | Image: | ||
*[http:// | *[http://en.wikipedia.org/wiki/File:Nuclear_changes.jpg Karyolysis, pyknosis, karyorrhexis (WP)]. | ||
===Erosions and ulcers=== | |||
*Ulcer = lesion through skin or mucous membrane. | |||
*Erosion = limited to the mucosa - superficial ulceration. | |||
**In dermatopathology - through the epidermis. | |||
Image: | |||
<gallery> | |||
Image:Ulcers,_fissures,_and_erosions.svg | Ulcers and erosions - schematic. (WC) | |||
</gallery> | |||
====Microscopic - erosion==== | |||
Features - require 1 and 2: | |||
#Loss of epithelium. | |||
#Vital response at site of lost epithelium. | |||
#*[[Neutrophil]]ic infiltrate. | |||
#*+/-Fibrin. | |||
#*+/-Cellular debris. | |||
Image: | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400158/figure/f4-cln_67p705/ Mucosal erosion (nih.gov)].<ref name=pmid22892912>{{Cite journal | last1 = Arashiro | first1 = RT. | last2 = Teixeira | first2 = MG. | last3 = Rawet | first3 = V. | last4 = Quintanilha | first4 = AG. | last5 = Paula | first5 = HM. | last6 = Silva | first6 = AZ. | last7 = Nahas | first7 = SC. | last8 = Cecconello | first8 = I. | title = Histopathological evaluation and risk factors related to the development of pouchitis in patients with ileal pouches for ulcerative colitis. | journal = Clinics (Sao Paulo) | volume = 67 | issue = 7 | pages = 705-10 | month = Jul | year = 2012 | doi = | PMID = 22892912 | PMC = 3400158 | URL = http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400158/}}</ref> | |||
== | ==The general differential diagnosis== | ||
Mnemonic ''CINE-TV-DATE'': | Mnemonic ''CINE-TV-DATE'': | ||
*Congenital. | *Congenital. | ||
| Line 47: | Line 80: | ||
In diagnostic pathology, most stuff falls into the ''neoplastic'' category. | In diagnostic pathology, most stuff falls into the ''neoplastic'' category. | ||
=== | ===Features of malignancy=== | ||
====Cytologic features of malignancy==== | |||
It is said that:<ref name=boerner>S. Boerner. 12 September 2011.</ref> | |||
#It is the nuclear abnormalities that make a cell malignant. | |||
#The cytoplasm that gives one clues as to the cell of origin. | |||
Nuclear features and malignancy:<ref name=boerner>S. Boerner. 12 September 2011.</ref> | |||
{| class="wikitable sortable" style="margin-left:auto;margin-right:auto" | |||
! Feature | |||
! Strength in predicting malignancy? | |||
|- | |||
| Large nuclear size | |||
| weak | |||
|- | |||
| [[Nuclear-to-cytoplasmic ratio]] | |||
| strong | |||
|- | |||
| Nuclear pleomorphism | |||
| weak | |||
|- | |||
| Nucleoli shape (angulated, spiked, complex) | |||
| strong | |||
|- | |||
| Nucleoli size | |||
| weak - generally; strong if like in a [[Hodgkin lymphoma|RS cell]] | |||
|- | |||
| High nucleoli number | |||
| weak negative; finding favours benign | |||
|- | |||
| Chromatin hyperchromasia | |||
| weak | |||
|- | |||
| Chromatin granularity | |||
| strong | |||
|- | |||
| Nuclear membrane irregularities | |||
| strong (clefting, flat edges, sharp angles), <br>scalloped (suggests benign) | |||
|- | |||
| Mitoses | |||
| weak § | |||
|- | |||
| Atypical mitoses | |||
| strong | |||
|} | |||
§ mitoses are seen in poorly differentiated tumour and regeneration. High mitotic rate in the context of unremarkable nuclear morphology is usually not malignant. | |||
====Other features==== | |||
In the context of [[soft tissue lesions]], it is said that the two most important features of malignancy are: | |||
#[[Necrosis]]. | |||
#High vascularity. | |||
Notes: | |||
*Benign soft tissue lesions may have marked [[nuclear atypia]] and abundant mitotic activity. | |||
===General differential diagnosis of malignant lesion=== | |||
This should ''always'' be considered: | |||
<center> | |||
<!-- | |||
DDX OF MALIGNANCY - FIRST STEP | |||
--> | |||
{{familytree/start}} | |||
{{familytree | | | |A11| | | | |A11 = Malignancy }} | |||
{{familytree | |,|-|-|^|-|-|.|}} | |||
{{familytree | B11 | | | | B12 |B11=Primary|B12=[[metastasis|Metastatic]] }} | |||
{{familytree/end}} | |||
</center> | |||
Q. Why? <br> | |||
A. (1) The site of the tumour can considerably change the differential diagnosis. (2) The management is usually totally different.<br><br> | |||
===A general clinico-histomorphologically motivated differential diagnosis of malignancy=== | |||
<center> | |||
<!-- | <!-- | ||
DDX OF MALIGNANCY | DDX OF MALIGNANCY - THE NEXT STEP | ||
--> | --> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | A | | | | | | | | | | |A=Malignancy}} | {{familytree | | | | | | | | | | | A | | | | | | | | | | |A=Malignancy}} | ||
{{familytree | |,|-|-|-|v|-|-|-|v|-|^|-|v|-|-|-|v|-|-|-|.| |}} | {{familytree | |,|-|-|-|v|-|-|-|v|-|^|-|v|-|-|-|v|-|-|-|.| |}} | ||
{{familytree | B | | C | | D | | E | | F | |G |B=Carcinoma|C=Sarcoma|D=Germ | {{familytree | B | | C | | D | | E | | F | |G |B=Epithelial<br>(Carcinoma)|C=Mesenchymal<br>([[Sarcoma]])|D=[[Germ cell tumours|Germ cell<br>tumour]]|E=[[Neuroendocrine carcinoma|Neuroendocrine<br>carcinoma]]|F=Hematologic|G=[[Melanoma|Malignant<br>melanoma]]}} | ||
{{familytree/end}} | {{familytree/end}} | ||
</center> | |||
Notes: | Notes: | ||
*'' | *''[[Malignant melanoma]]'', also ''melanoma'', is a separate category as it can look like almost anything under the microscope. | ||
*'' | *''Hematologic'' includes [[lymphoma]], [[leukemia]], [[plasma cell neoplasms]] and others. | ||
*The above is a useful clinical classification. The problem is it isn't that useful for difficult cases as: | |||
**Germ cell tumours are often not distinctive. | |||
**Numerous epithelioid sarcomas can mimic carcinomas. | |||
**Spindle cell carcinomas can mimic sarcomas very well. | |||
**Neuroendocrine differentiation is not always readily apparent. | |||
**The ''[[modified general morphologic DDx of malignancy]]'' is better for approaching difficult tumours. | |||
Memory device ''HMN GEM'': hematologic, melanoma, neuroendocrine carcinoma, germ cell, epithelial, mesenchymal. | |||
===Morphologic | ====Morphologic categorization==== | ||
=====Factors to consider===== | |||
Factors to consider when attempting to group by morphology: | Factors to consider when attempting to group by morphology: | ||
#Cell shape (spindle cell, epithelioid, plasmacytoid, mixed). | |||
#Cell size (small or large) - size in relation to a neutrophil or [[red blood cell]]. | |||
#Cell cohesion - dyscohesive vs. cohesive. | #Cell cohesion - dyscohesive vs. cohesive. | ||
#*If one sees several groups of 5+ cells... probably cohesive. | #*If one sees several groups of 5+ cells... probably cohesive. | ||
#*Presence of cell cohesion strongly disfavours lymphoma. | #*Presence of cell cohesion strongly disfavours lymphoma. | ||
#Cytoplasm - abundance (scant, moderate, abundant). | #Cytoplasm - abundance (scant, moderate, abundant). | ||
#*Eosinophilic cytoplasm disfavours lymphoma. | #*Eosinophilic cytoplasm disfavours lymphoma. | ||
#*Oncocytic - possessing copious eosinophilic granular cytoplasm. | |||
#**Benign lesions composed of oncocytes - oncocytoma | |||
#**Oncocytic metaplasia (alteration of cytoplasm) can effect all or a part of a lesion. | |||
#**Oncocytic neoplasms are common in the kidneys, thyroid and salivary glands. | |||
#**Oncocytic change increases with age | |||
#**May represent senescent accumulation of mitochondria in secretory epithelial. | |||
#Chromatin - coarseness (fine, granular). | #Chromatin - coarseness (fine, granular). | ||
#Nucleoli - number (absent, present, multiple). | #Nucleoli - number (absent, present, multiple). | ||
#*Large nucleoli (nucleoli seen with the 10x objective) pretty much exclude neuroendocrine. | #*Large [[nucleoli]] (nucleoli seen with the 10x objective) pretty much exclude neuroendocrine. | ||
======Types of cells====== | |||
{| class="wikitable sortable" | |||
! Type | |||
! Morphology | |||
! Significance | |||
* | |- | ||
* | | [[Spindle cell]] | ||
| tapered at both ends<ref>URL: [http://www.medterms.com/script/main/art.asp?articlekey=25657 http://www.medterms.com/script/main/art.asp?articlekey=25657]. Accessed on: 18 January 2010.</ref> | |||
| suggestive of sarcoma - compatible with melanoma and some carcinomas | |||
|- | |||
| Epithelioid cell | |||
| cell shape round/oval, nucleus round/oval, looks like epithelium (cell borders touch neighbouring cells - collectively form a barrier) | |||
| suggests epithelial lesion (carcinoma) - compatible with others | |||
|- | |||
| [[Small round blue cell tumour]]/lymphoid: | |||
| small cells with scant cytoplasm - usually round; "small" is classically 2x a "resting lymphocyte" diameter † | |||
| common in children; in adults often lymphoma | |||
|- | |||
| Small lymphoid ([[small cell lymphoma]]). | |||
| "small" in the context of lymphoid is classically ~1x a "resting lymphocyte" diameter; often not malignant by cytology | |||
| suggests [[small cell lymphoma]], reactive changes or infection | |||
|- | |||
| Plasmacytoid cell | |||
| resemble a plasma cell: eccentric nucleus, moderate basophilic cytoplasm, +/-"clockface" chromatin pattern (clumping of chromatin at the periphery of the nucleus), +/-perinuclear hof (crescentic cytoplasmic clearing adjacent to the nucleus; represents abundant Golgi apparatus | |||
| suggests [[plasma cell neoplasm]] or infection | |||
|} | |||
Note: | |||
*† Diameter of a "resting lymphocyte" ~ diameter of a [[red blood cell]] (RBC) ~ 8 micrometres. | |||
**Most carcinoma cells are 3-4x the size of a RBC. | |||
====Dyscohesive | ======Dyscohesive versus cohesive====== | ||
Deciding cells are dyscohesive vs. cohesive is important, as it is a strong determinant of whether one is dealing with a lymphoid lesion or not. | Deciding cells are dyscohesive vs. cohesive is important, as it is a strong determinant of whether one is dealing with a lymphoid lesion or not. | ||
{| class="wikitable" | {| class="wikitable sortable" | ||
!| | !| | ||
!| Cell spacing | !| Cell spacing | ||
| Line 92: | Line 235: | ||
|- | |- | ||
| '''Cohesive''' | | '''Cohesive''' | ||
| equal spacing ''or'' 3-D clusters | | equal spacing ''or'' 3-D clusters ''or'' intracellular bridges | ||
| visible | | visible & opposed (in >50% of cells) | ||
| scant to abundant | | scant to abundant | ||
| any | | any | ||
|- | |- | ||
| '''Dyscohesive''' | | '''Dyscohesive''' | ||
| unequal spacing | | unequal spacing, thin space surrounds cell | ||
| not apparent | | not apparent | ||
| usually scant | | usually scant | ||
| Line 104: | Line 247: | ||
|- | |- | ||
| Value/utility | | Value/utility | ||
| equal or 3-D clusters | | equal or 3-D clusters suggests cohesive, pericellular space/rim suggests dyscohesive | ||
| visible opposed membrane r/i cohesive | | visible opposed membrane r/i cohesive | ||
| abundant usu. cohesive | | abundant usu. cohesive | ||
| Line 110: | Line 253: | ||
|} | |} | ||
Strong predictors of ''cohesive'': | |||
*Intracellular bridges. | |||
* | *3-D clusters. | ||
** | *Nuclear moulding. | ||
* | |||
* | Weak predictors of ''cohesive'': | ||
* | *Eosinophilic cytoplasm. | ||
* | *Abundant cytoplasm. | ||
*>2 X RBC diameter (most lymphoma smaller). | |||
Weak predictors of ''dyscohesive'': | |||
*Pericellular space/rim. | |||
*Scant cytoplasm. | |||
*Basophilic cytoplasm. | |||
=====Probable category by morphology===== | |||
*Carcinoma = cohesive, relatively large (>~2X neutrophil), +/-nucleolus, +/-gland formation (circular structures), often moderate to abundant cytoplasm. | |||
*Sarcoma = cohesive, composed of spindle cells (cells taper at both ends, nucleus oval/cigar-shaped). | |||
*Germ cell tumour = appearance often similar to ''carcinoma'', site (location) very useful - esp. gonadal, midline, retroperitoneal. | |||
*[[Neuroendocrine carcinoma]] = cohesive, fine granular chromatin and no [[nucleolus]]. | |||
*Lymphoma = dyscohesive, relatively small (usually <=2X neutrophil diameter), usu. scant basophilic (blue) cytoplasm. | |||
*Melanoma = classically pigmented, often a prominent [[red nucleolus]], a mix of spindle cells and epithelioid cells, mix of cohesive and dyscohesive cells. | |||
===A practical histomorphologic differential diagnosis of malignancy=== | |||
====General morphologic DDx of malignancy==== | |||
{{familytree/start}} | |||
{{familytree | | | | | | | A01 | | | | | | | | A01=Malignancy}} | |||
{{familytree | |,|-|-|-|v|-|^|-|v|-|-|-|.| | |}} | |||
{{familytree | B01 | | B02 | | B03 | | B04 | |B01=[[Large epithelioid tumours]]|B02=[[spindle cell lesions|Spindle cell tumours]]|B03=[[small round cell tumours|Small blue cell tumours]]|B04=[[Pleomorphic tumours]]}} | |||
{{familytree/end}} | |||
====Modified general morphologic DDx of malignancy==== | |||
<center> | |||
{{familytree/start}} | |||
{{familytree | | | | | | | | | | | A | | | | | | | | | | |A=Malignancy}} | |||
{{familytree | |,|-|-|-|v|-|-|-|v|-|^|-|v|-|-|-|v|-|-|-|.| |}} | |||
{{familytree | B | | C | | D | | E | | F | |G |B=[[Large epithelioid tumours]]|C=[[spindle cell lesions|Spindle cell tumours]]|D=[[small round cell tumours|Small blue cell tumours]]|E=[[Pleomorphic tumours]]|F=[[Clear cell tumours]]|G=[[myxoid lesions|Myxoid tumours]]}} | |||
{{familytree/end}} | |||
</center> | |||
The above is more useful than the ''general clinico-histomorphologically motivated differential diagnosis of malignancy''. | |||
==Differential diagnosis by site== | |||
{{Main|Short power list}} | |||
It is essential to have a concept of what is common. The ''[[short power list]]'' gives a short [[differential diagnosis]] for the common sites. | |||
{{Main|Long power list}} | |||
The ''[[long power list]]'' is a longer list for the common sites. | |||
==Finding the elements== | ==Finding the elements== | ||
| Line 126: | Line 306: | ||
*Nucleus darker (hyperchromatic) - '''key feature'''. | *Nucleus darker (hyperchromatic) - '''key feature'''. | ||
*No nuclear membrane - '''key feature'''. | *No nuclear membrane - '''key feature'''. | ||
*In prophase chromatin may have a scalloped border/beaded border.<ref>URL: [http://www.microbehunter.com/wp/wp-content/uploads/2009/lily_prophase.jpg http://www.microbehunter.com/wp/wp-content/uploads/2009/lily_prophase.jpg] and [http://www.microbehunter.com/2009/12/06/mitosis-stages-of-the-lily/ http://www.microbehunter.com/2009/12/06/mitosis-stages-of-the-lily/]. Accessed on: 3 November 2010.</ref> | |||
DDx: | DDx: | ||
*Apoptotic cell -- has nuclear condensation (pyknosis), eosinophilic cytoplasm. | *Apoptotic cell -- has nuclear condensation (pyknosis), eosinophilic cytoplasm. | ||
====Images==== | |||
<gallery> | |||
Image:Atypical_mitosis.jpg| Mitoses and an atypical mitosis. (WC) | |||
Image:Tripolar_Mitosis_-_breast_carcinoma.jpg| Tripolar mitosis. (WC) | |||
</gallery> | |||
www: | |||
*[http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/Lab4/IMAGES/MITOSIS%20IN%20GUT.JPG Mitoses (vetmed.vt.edu)]. | |||
*[http://www.flickr.com/photos/euthman/426956752/ Starburst mitosis (flicker.com)]. | |||
====Phases of mitosis==== | |||
*Prophase - chromatin condenses to chromosomes. | |||
*Metaphase - chromosome aligned. | |||
*Anaphase - spindles separated. | |||
*Telophase - reversal of prophase. | |||
===Neutrophils=== | ===Neutrophils=== | ||
{{Main|Neutrophils}} | |||
*Little dots = the multilobular nucleus - '''key feature'''. | *Little dots = the multilobular nucleus - '''key feature'''. | ||
*Neutrophils are often found with friends, i.e. lymphocytes, plasma cells. | *Neutrophils are often found with friends, i.e. lymphocytes, plasma cells. | ||
| Line 143: | Line 340: | ||
*A collection of PMNs... think about ''necrosis'' and ''abscess''. | *A collection of PMNs... think about ''necrosis'' and ''abscess''. | ||
===Lymph node | ===Lymph node metastasis=== | ||
{{Main|Lymph node metastasis}} | |||
*Take a good to look at the tumour first. | *Take a good to look at the tumour first. | ||
*Tumour in a node is often better differentiated than the most poorly differentiated part in the primary site. | *Tumour in a node is often better differentiated than the most poorly differentiated part in the primary site. | ||
*Subcapsular space - the first place to look for mets. | *Subcapsular space - the first place to look for mets. | ||
*Lymph node | *Lymph node metastasis are usually obvious. | ||
*Histiocytes may be difficult to separate from tumour - | **There are of course exceptions, e.g. [[small cell carcinoma]], [[invasive lobular carcinoma]]. | ||
**Histiocytes | *Histiocytes may be difficult to separate from tumour - especially for the novice. | ||
**Malignant cells have to have malignant features, i.e. the NC ratio is abnormal, there is nuclear pleomorphism. | **Histiocytes may be found in the germinal centres, i.e. the node architecture helps. | ||
**Malignant cells, generally, have to have malignant features, i.e. the [[NC ratio]] is abnormal, there is [[nuclear pleomorphism]]. | |||
*Several things can mimic metastases - see ''[[Lymph node metastasis]]''. | |||
See: ''[[Lymph node]]'' article for a detailed description of cell types in a lymph node. | See: ''[[Lymph node]]'' article for a detailed description of cell types in a lymph node. | ||
=== | ===Signet ring cell carcinoma=== | ||
{{Main|Signet ring cell carcinoma}} | |||
*It has been said that there are two types of pathologists... those that have missed SRCs ''and'' those that will miss SRCs. | |||
* | |||
Microscopic: | |||
* | *Cells resemble signet rings: | ||
**They contain a large amount of mucin, which pushes the nucleus to the cell periphery. | |||
**The pool of mucin in a signet ring cell mimics the appearance of a finger hole. | |||
**The nucleus mimics the appearance of the face of the ring in profile. | |||
*Cells typically 2-3x the size of a lymphocyte. | |||
**Smaller than the typical adipocyte. | **Smaller than the typical adipocyte. | ||
*Often have a | *Often have a crescent-shaped ''or'' ovoid nucleus. | ||
**Capillaries sectioned on their lumen have endothelial cells-- the nuclei of these are more spindled. | **Capillaries sectioned on their lumen have endothelial cells -- the nuclei of these are more spindled. | ||
*SRCs are usually close to friend | *SRCs are usually close to friend -- another SRC. | ||
**This helps differentiate SRCs from capillaries sectioned on their lumen. | **This helps differentiate SRCs from capillaries sectioned on their lumen. | ||
*The mucin is often clear on H&E... but maybe eosinophilic. | *The mucin is often clear on H&E... but maybe eosinophilic. | ||
DDx: | |||
*[[Fat atrophy]]. | |||
Stains: | Stains: | ||
| Line 195: | Line 378: | ||
*Alican blue-PAS stain. | *Alican blue-PAS stain. | ||
Images | ====Images==== | ||
<gallery> | |||
Image:Signet_ring_cells_5.jpg |SRCs - H&E stain. (WC/Nephron) | |||
*[http:// | Image:Gastric_signet_ring_cell_carcinoma_histopatholgy_(2)_PAS_stain.jpg | SRCs - AL-PAS stain. (WC) | ||
Image:Gastric_signet_ring_cell_carcinoma_histopatholgy_(1).jpg | SRC - H&E stain. (WC) | |||
</gallery> | |||
www: | |||
*[http://www.engravingarts.com/sales/LVX2.jpg Signet rings (engravingarts.com)]. | |||
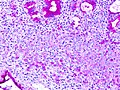
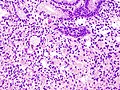
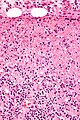
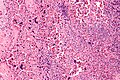
== | ===Necrosis=== | ||
* | {{Main|Necrosis}} | ||
* | Features: | ||
*Dead cells - pink (on H&E). | |||
**Anucleate cells ("Ghost cells")/outlines of cells - usu. subtle. | |||
***Fluffy appearance. | |||
*+/-Neutrophils (very common). | |||
DDx of necrosis: | |||
* | *Fibrin. | ||
= | Images (necrosis): | ||
*[http://www0.sun.ac.za/ortho/webct-ortho/tb/tb-histology.html Necrosis at the centre of a granuloma (sun.ac.za)]. | |||
* | *[http://www.biomedical-engineering-online.com/content/9/1/10/figure/F7?highres=y Necrosis (biomedical-engineering-online.com)]. | ||
*[http://www.nature.com/bmt/journal/v39/n9/fig_tab/1705646f1.html Necrosis (nature.com)]. | |||
*[http://moon.ouhsc.edu/kfung/jty1/Com08/Com08Image/Com801-1-09.gif Necrosis (ouhsc.edu)].<ref>URL: [http://moon.ouhsc.edu/kfung/jty1/Com08/Com801-1-Diss.htm http://moon.ouhsc.edu/kfung/jty1/Com08/Com801-1-Diss.htm]. Accessed on: 3 November 2010.</ref> | |||
<gallery> | |||
Image:Cat_scratch_disease_-_very_high_mag.jpg | Necrosis in [[cat scratch disease]]. (WC/Nephron) | |||
Image:Histiocytic_necrotizing_lymphadenitis_-_very_high_mag.jpg | Necrosis in [[histiocytic necrotizing lymphadenitis]]. (WC/Nephron) | |||
Image:Systemic_lupus_erythematosus_lymphadenopathy_-_high_mag.jpg | Necrosis in [[SLE lymphadenopathy]]. (WC/Nephron) | |||
</gallery> | |||
==Granulomas== | |||
{{Main|Granuloma}} | |||
==Common morphologic problems== | |||
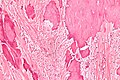
* | ===DDx of pink stuff (on H&E)=== | ||
* | The ''ABCs'' of pink: | ||
* | *'''A'''myloid. | ||
*'''B'''lood clot (organized); fibrin. | |||
*'''C'''ollagen (fibrous tissue). | |||
*'''S'''mooth muscle cells (SMCs). | |||
=====Images===== | |||
<gallery> | |||
Image:Cardiac_amyloidosis_high_mag_he.jpg | Cardiac amyloid. (WC/Nephron) | |||
Image:Laminations_in_a_thrombus_-_high_mag.jpg | Fibrin in a thrombus. (WC/Nephron) | |||
Image:Ovarian_fibroma_-_high_mag.jpg | Collagen in an ovarian fibroma. (WC/Nephron) | |||
Image:Glatte_Muskelzellen.jpg | Smooth muscle. (WC/Polarlys) | |||
</gallery> | |||
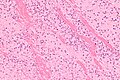
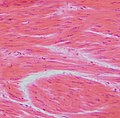
=== | ====Smooth muscle cells (SMCs) vs. fibrous tissue==== | ||
Fibroblasts (fibrous tissue): | |||
*Wavy nuclei with pointy ends. | |||
*Less nuclei. | |||
* | SMCs: | ||
* | *Elliptical nuclei. | ||
*More nuclei. | |||
* | |||
* | |||
Remembering the above: | |||
*SMCs are stretched; ergo, not wavy. | |||
* | *Fibrous tissue is fibrous... more protein... less cells; ergo, less nuclei. | ||
* | *'''F'''ibroblast = '''f'''ootball-like. | ||
*Cigar-shaped nuclei (SMCs) are affected by cigars (smoking causes vascular disease). | |||
* | |||
* | |||
Notes: | |||
*Schwann cells (found in nerve): nuclei = wavy appearance, thin. (???) | |||
===Pigmented material=== | |||
*[[AKA]] brown/black granular crap. | |||
* | |||
DDx of granular stuff/pigment: | |||
DDx of granular stuff: | |||
#Lipofuscin - especially in old people. | #Lipofuscin - especially in old people. | ||
#Hemosiderin. | #Hemosiderin. | ||
#Bile - found in hepatocytes, yellow. | #Bile - found in hepatocytes, yellow. | ||
#Foreign material (tattoo pigment, anthracotic pigment). | #Foreign material (tattoo pigment, anthracotic pigment, [[amalgam tattoo]]). | ||
#Melanin. | #Melanin. | ||
Notes: | |||
*Granular stuff should prompt consideration of ''malignant melanoma''. | *Granular stuff should prompt consideration of ''malignant melanoma''. | ||
*Memory device ''BH MILF'' = Bile, Homogentisic acid, Melanin, Iron (hemosiderin), Lipofuscin, Foreign material. | |||
*''Homogentisic acid'' found in ''alkaptonuria'',<ref name=Ref_PCPBoD8_20>{{Ref PCPBoD8|20}}</ref>can be considered the sixth (black) pigment. | |||
**Gentisic = jen-TIS-ik.<ref>URL: [http://dictionary.reference.com/browse/gentisic+acid http://dictionary.reference.com/browse/gentisic+acid]. Accessed on: 11 January 2012.</ref> | |||
Stains that can help sort it out | ====[[Stains]] that can help sort it out==== | ||
*Prussian blue for hemosiderin. | *Prussian blue (iron stain) for hemosiderin. | ||
*Melan A for melanin. | *[[Fontana-Masson stain]] (or ''Melan A'') for melanin. | ||
* | *[[PAS stain]]<ref name=pmid5463681 >{{cite journal |author=Kovi J, Leifer C |title=Lipofuscin pigment accumulation in spontaneous mammary carcinoma of A/Jax mouse |journal=J Natl Med Assoc |volume=62 |issue=4 |pages=287–90 |year=1970 |month=July |pmid=5463681 |pmc=2611776 |doi= |url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2611776/pdf/jnma00512-0077.pdf}}</ref> ''or'' Kluver-Barrera for lipofuscin. | ||
== | |||
== | |||
==Staining== | ==Staining== | ||
| Line 311: | Line 473: | ||
==Immunohistochemistry== | ==Immunohistochemistry== | ||
{{main|Immunohistochemistry}} | {{main|Immunohistochemistry}} | ||
If the special stains don't help... there is immunohistochemistry. | |||
==Food and pathology== | ==Food and pathology== | ||
{{main|Pathology and food}} | {{main|Pathology and food}} | ||
Generally, positive margins suck | ==Tumour remaining== | ||
{{Main|Surgical margins}} | |||
''R classification'':<ref>URL: [http://www.informedicalcme.com/colon-cancer/tnm-stage-groupings/ http://www.informedicalcme.com/colon-cancer/tnm-stage-groupings/]. Accessed on: 27 March 2012.</ref> | |||
*"RX resection" = residual tumour cannot be assessed. | |||
*"R0 resection" = clean margin macroscopically & microscopically. | |||
*"R1 resection" = microscopic tumour left. | |||
*"R2 resection" = macroscopic tumour left. | |||
Surgeons use this terminology. Essentially, it is the margin status. It is nice when the surgeon's assessment and the pathologist's are in agreement. | |||
Note: | |||
*Generally, positive margins suck. For example, in locally advanced rectal cancer, in one study,<ref name=pmid17614249>{{cite journal |author=Larsen SG, Wiig JN, Dueland S, Giercksky KE |title=Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer |journal=Eur J Surg Oncol |volume=34 |issue=4 |pages=410–7 |year=2008 |month=April |pmid=17614249 |doi=10.1016/j.ejso.2007.05.012 |url=}}</ref> five year survival was found to be 60%, 31% and 0% for R0, R1, and R2 resections respectively. | |||
== | ==Clinician talk== | ||
===Performance status=== | |||
*ECOG - score from 1-5 for performance status.<ref name=pmid7165009>{{cite journal |author=Oken MM, Creech RH, Tormey DC, ''et al.'' |title=Toxicity and response criteria of the Eastern Cooperative Oncology Group |journal=Am. J. Clin. Oncol. |volume=5 |issue=6 |pages=649–55 |year=1982 |month=December |pmid=7165009 |doi= |url=}}</ref> | *ECOG - score from 1-5 for performance status.<ref name=pmid7165009>{{cite journal |author=Oken MM, Creech RH, Tormey DC, ''et al.'' |title=Toxicity and response criteria of the Eastern Cooperative Oncology Group |journal=Am. J. Clin. Oncol. |volume=5 |issue=6 |pages=649–55 |year=1982 |month=December |pmid=7165009 |doi= |url=}}</ref> | ||
**ECOG = Eastern Cooperative Oncology Group. | **ECOG = Eastern Cooperative Oncology Group. | ||
| Line 334: | Line 505: | ||
*ECOG 5: dead. | *ECOG 5: dead. | ||
==Fixation & lifestyle== | ==Pathology & pathologists== | ||
===[[Fixation]] & lifestyle=== | |||
Pathologist have a great lifestyle 'cause tissue takes long to fix; the penetration of tissue by formalin is 1 mm/hour.<ref>Gross rounds. 14 August 2009.</ref> | Pathologist have a great lifestyle 'cause tissue takes long to fix; the penetration of tissue by formalin is 1 mm/hour.<ref>Gross rounds. 14 August 2009.</ref> | ||
===Malignancy & inflammation=== | |||
If there is lots of inflammation... and you're thinking cancer you should probably back-off, i.e. tend toward benign. Inflammation can make cells look more malignant than they might be if left alone. | |||
==Miscellaneous== | |||
===Infectious stuffs=== | |||
{{main|Microorganisms}} | |||
Images: [http://www.uphs.upenn.edu/bugdrug/antibiotic_manual/Gram3.htm http://www.uphs.upenn.edu/bugdrug/antibiotic_manual/Gram3.htm] | |||
*Staphylococcus - in clusters. | |||
*Streptococcus - in chains. | |||
==Microscopes== | ==Microscopes== | ||
{{main|HPFitis}} | |||
*Pathologists throw around the term ''high power field'' (''HPF''). | *Pathologists throw around the term ''high power field'' (''HPF''). | ||
**"HPF" has no agreed upon definition and, IMHO, should '''''never''''' be used without definition. | **"HPF" has no agreed upon definition and, IMHO, should '''''never''''' be used without a non-ambiguous definition. | ||
''HPF'' generally refers to the area seen with the largest magnification objective (40x), i.e. the field at 400x (as the eye piece magnification is usually 10x). The field size varies significantly from microscope to microscope. | ''HPF'' generally refers to the area seen with the largest magnification objective (40x), i.e. the field at 400x (as the eye piece magnification is usually 10x). The field size varies significantly from microscope to microscope. | ||
| Line 358: | Line 544: | ||
*FOV = 22 mm / 40 | *FOV = 22 mm / 40 | ||
*FOV = 0.55 mm | *FOV = 0.55 mm | ||
Note: | |||
*Most modern [[microscope]]s, have an eye piece diameter of 22 mm. Therefore, the field diameter at 40 X is approximately 22 mm / 40 X ~= 0.55 mm and the field of view is pi/4*(0.55 mm)^2 = 0.2376 mm^2. | |||
==Pathology reports== | ==Pathology reports== | ||
{{Main|Pathology reports}} | |||
The key point in report writing is that the report should be precise, complete and easy-to-understand. | |||
The | |||
===Standards=== | ===Standards=== | ||
There is no universal standard; however, there is a push to standardize by the ''Association of Directors of Anatomic and Surgical Pathology'',<ref>URL: [http://www.adasp.org/papers/position/Standardization.htm http://www.adasp.org/papers/position/Standardization.htm]</ref> among others. | |||
====Checklists==== | ====Checklists==== | ||
{{Main|CAP checklists}} | |||
The College of American Pathologists (CAP) has checklists for cancer - [http://www.cap.org/apps/cap.portal?_nfpb=true&cntvwrPtlt_actionOverride=%2Fportlets%2FcontentViewer%2Fshow&_windowLabel=cntvwrPtlt&cntvwrPtlt%7BactionForm.contentReference%7D=committees%2Fcancer%2Fcancer_protocols%2Fprotocols_index.html&_state=maximized&_pageLabel=cntvwr CAP protocols]. | The College of American Pathologists (CAP) has checklists for cancer - [http://www.cap.org/apps/cap.portal?_nfpb=true&cntvwrPtlt_actionOverride=%2Fportlets%2FcontentViewer%2Fshow&_windowLabel=cntvwrPtlt&cntvwrPtlt%7BactionForm.contentReference%7D=committees%2Fcancer%2Fcancer_protocols%2Fprotocols_index.html&_state=maximized&_pageLabel=cntvwr CAP protocols]. | ||
Pathologists will probably use more checklists in the future... they are deemed effective in a number of places inside and outside of medicine. | |||
Surgeons know that checklists work and that they save lives.<ref name=pmid19158173>{{cite journal |author=Soar J, Peyton J, Leonard M, Pullyblank AM |title=Surgical safety checklists |journal=BMJ |volume=338 |issue= |pages=b220 |year=2009 |pmid=19158173 |doi= |url=http://bmj.com/cgi/pmidlookup?view=long&pmid=19158173}}</ref> | Surgeons know that checklists work and that they save lives.<ref name=pmid19158173>{{cite journal |author=Soar J, Peyton J, Leonard M, Pullyblank AM |title=Surgical safety checklists |journal=BMJ |volume=338 |issue= |pages=b220 |year=2009 |pmid=19158173 |doi= |url=http://bmj.com/cgi/pmidlookup?view=long&pmid=19158173}}</ref> | ||
Pilots have been using checklists since the 1930s. | |||
===Standard diagnostic notation=== | ===Standard diagnostic notation=== | ||
| Line 388: | Line 573: | ||
Gallbladder, cholecystectomy:<br> | Gallbladder, cholecystectomy:<br> | ||
- Acute cholecystitis. | - Acute cholecystitis. | ||
==Lab talk== | |||
{{Main|Cutting}} | |||
Tissue cutting terms - these often vary from lab-to-lab:<ref>URL: [http://www.mailman.srv.ualberta.ca/pipermail/patho-l/2002-July/016955.html http://www.mailman.srv.ualberta.ca/pipermail/patho-l/2002-July/016955.html]. Accessed on: 18 October 2011.</ref> | |||
*Recut = cut off the top of the block. | |||
*Serial sections = make several cuts off the top of the block and look at all of 'em. | |||
*Level = trim the block ~30 micrometres --throw away trimmed tissue-- and then cut a section to look at. | |||
*Deeper = trim the block ~100 micrometres --throw away trimmed tissue-- and then cut a section to look at. | |||
==See also== | |||
*[[Granulation tissue]]. | |||
*[[No truth in names]]. | |||
*[[Blood work]]. | |||
*[[Quality]]. | |||
==References== | ==References== | ||
Latest revision as of 03:29, 14 July 2016
This article serves as an introduction to anatomical pathology and discusses the basics.
Pathology simplified
Blue & pink
H&E is the standard...
- Too much PINK = DEAD (necrosis).
- Too much BLUE = BAD.
In words:
- Blue is bad and pink is dead![1]
Note:
- There is a lengthy list of things that are blue and not "bad"... that why a pathology residency is years.
- Lymph nodes are very blue... they aren't necessarily bad.
- Reactive processes can be very blue... they aren't bad.
Three questions
Pathology can be boiled down to:
- What is it?
- Biopsies.
- Did I get it all?
- Resections.
- Did I get the right thing?
- Most other things.
Terms
Staining
- Eosinophilic - pink.
- Hyperchromatic - blue.
- Amphophilic - bluish-red colour when referring to H&E stained section.[2]
- Amphophilic means stains with both acidic & basic dyes.
- Images: amphophilic material - arrow (pancreaticcancer2000.com), amphophilic cytoplasm in prostate carcinoma (webpathology.com).
- Argyrophilic means has an affinity for silver[3][4]/loves silver/stains with silver.
Morphologic patterns
This covers things like cribriform, hobnail, herring bone and many others.
Nuclear destruction words
There are several fancy terms:[5]
- Karyolysis = nuclear fading/dissolution.
- Pyknosis = nuclear shrinkage.
- Karyorrhexis = nuclear fragmentation.
Image:
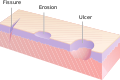
Erosions and ulcers
- Ulcer = lesion through skin or mucous membrane.
- Erosion = limited to the mucosa - superficial ulceration.
- In dermatopathology - through the epidermis.
Image:
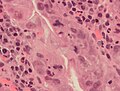
Microscopic - erosion
Features - require 1 and 2:
- Loss of epithelium.
- Vital response at site of lost epithelium.
- Neutrophilic infiltrate.
- +/-Fibrin.
- +/-Cellular debris.
Image:
The general differential diagnosis
Mnemonic CINE-TV-DATE:
- Congenital.
- Inflammatory.
- Neoplastic.
- Endocrine.
- Trauma.
- Vascular.
- Degenerative.
- Autoimmune.
- Toxic.
- Everything else (iatrogenic, idiopathic, psychiatric).
In diagnostic pathology, most stuff falls into the neoplastic category.
Features of malignancy
Cytologic features of malignancy
It is said that:[7]
- It is the nuclear abnormalities that make a cell malignant.
- The cytoplasm that gives one clues as to the cell of origin.
Nuclear features and malignancy:[7]
| Feature | Strength in predicting malignancy? |
|---|---|
| Large nuclear size | weak |
| Nuclear-to-cytoplasmic ratio | strong |
| Nuclear pleomorphism | weak |
| Nucleoli shape (angulated, spiked, complex) | strong |
| Nucleoli size | weak - generally; strong if like in a RS cell |
| High nucleoli number | weak negative; finding favours benign |
| Chromatin hyperchromasia | weak |
| Chromatin granularity | strong |
| Nuclear membrane irregularities | strong (clefting, flat edges, sharp angles), scalloped (suggests benign) |
| Mitoses | weak § |
| Atypical mitoses | strong |
§ mitoses are seen in poorly differentiated tumour and regeneration. High mitotic rate in the context of unremarkable nuclear morphology is usually not malignant.
Other features
In the context of soft tissue lesions, it is said that the two most important features of malignancy are:
- Necrosis.
- High vascularity.
Notes:
- Benign soft tissue lesions may have marked nuclear atypia and abundant mitotic activity.
General differential diagnosis of malignant lesion
This should always be considered:
| Malignancy | |||||||||||||||||||
| Primary | Metastatic | ||||||||||||||||||
Q. Why?
A. (1) The site of the tumour can considerably change the differential diagnosis. (2) The management is usually totally different.
A general clinico-histomorphologically motivated differential diagnosis of malignancy
| Malignancy | |||||||||||||||||||||||||||||||||||||||||||||||
| Epithelial (Carcinoma) | Mesenchymal (Sarcoma) | Germ cell tumour | Neuroendocrine carcinoma | Hematologic | Malignant melanoma | ||||||||||||||||||||||||||||||||||||||||||
Notes:
- Malignant melanoma, also melanoma, is a separate category as it can look like almost anything under the microscope.
- Hematologic includes lymphoma, leukemia, plasma cell neoplasms and others.
- The above is a useful clinical classification. The problem is it isn't that useful for difficult cases as:
- Germ cell tumours are often not distinctive.
- Numerous epithelioid sarcomas can mimic carcinomas.
- Spindle cell carcinomas can mimic sarcomas very well.
- Neuroendocrine differentiation is not always readily apparent.
- The modified general morphologic DDx of malignancy is better for approaching difficult tumours.
Memory device HMN GEM: hematologic, melanoma, neuroendocrine carcinoma, germ cell, epithelial, mesenchymal.
Morphologic categorization
Factors to consider
Factors to consider when attempting to group by morphology:
- Cell shape (spindle cell, epithelioid, plasmacytoid, mixed).
- Cell size (small or large) - size in relation to a neutrophil or red blood cell.
- Cell cohesion - dyscohesive vs. cohesive.
- If one sees several groups of 5+ cells... probably cohesive.
- Presence of cell cohesion strongly disfavours lymphoma.
- Cytoplasm - abundance (scant, moderate, abundant).
- Eosinophilic cytoplasm disfavours lymphoma.
- Oncocytic - possessing copious eosinophilic granular cytoplasm.
- Benign lesions composed of oncocytes - oncocytoma
- Oncocytic metaplasia (alteration of cytoplasm) can effect all or a part of a lesion.
- Oncocytic neoplasms are common in the kidneys, thyroid and salivary glands.
- Oncocytic change increases with age
- May represent senescent accumulation of mitochondria in secretory epithelial.
- Chromatin - coarseness (fine, granular).
- Nucleoli - number (absent, present, multiple).
- Large nucleoli (nucleoli seen with the 10x objective) pretty much exclude neuroendocrine.
Types of cells
| Type | Morphology | Significance |
|---|---|---|
| Spindle cell | tapered at both ends[8] | suggestive of sarcoma - compatible with melanoma and some carcinomas |
| Epithelioid cell | cell shape round/oval, nucleus round/oval, looks like epithelium (cell borders touch neighbouring cells - collectively form a barrier) | suggests epithelial lesion (carcinoma) - compatible with others |
| Small round blue cell tumour/lymphoid: | small cells with scant cytoplasm - usually round; "small" is classically 2x a "resting lymphocyte" diameter † | common in children; in adults often lymphoma |
| Small lymphoid (small cell lymphoma). | "small" in the context of lymphoid is classically ~1x a "resting lymphocyte" diameter; often not malignant by cytology | suggests small cell lymphoma, reactive changes or infection |
| Plasmacytoid cell | resemble a plasma cell: eccentric nucleus, moderate basophilic cytoplasm, +/-"clockface" chromatin pattern (clumping of chromatin at the periphery of the nucleus), +/-perinuclear hof (crescentic cytoplasmic clearing adjacent to the nucleus; represents abundant Golgi apparatus | suggests plasma cell neoplasm or infection |
Note:
- † Diameter of a "resting lymphocyte" ~ diameter of a red blood cell (RBC) ~ 8 micrometres.
- Most carcinoma cells are 3-4x the size of a RBC.
Dyscohesive versus cohesive
Deciding cells are dyscohesive vs. cohesive is important, as it is a strong determinant of whether one is dealing with a lymphoid lesion or not.
| Cell spacing | Cell membrane | Cytoplasm, abundance | Cytoplasm, staining | |
|---|---|---|---|---|
| Cohesive | equal spacing or 3-D clusters or intracellular bridges | visible & opposed (in >50% of cells) | scant to abundant | any |
| Dyscohesive | unequal spacing, thin space surrounds cell | not apparent | usually scant | usually basophilic |
| Value/utility | equal or 3-D clusters suggests cohesive, pericellular space/rim suggests dyscohesive | visible opposed membrane r/i cohesive | abundant usu. cohesive | eosinophilic usu. cohesive |
Strong predictors of cohesive:
- Intracellular bridges.
- 3-D clusters.
- Nuclear moulding.
Weak predictors of cohesive:
- Eosinophilic cytoplasm.
- Abundant cytoplasm.
- >2 X RBC diameter (most lymphoma smaller).
Weak predictors of dyscohesive:
- Pericellular space/rim.
- Scant cytoplasm.
- Basophilic cytoplasm.
Probable category by morphology
- Carcinoma = cohesive, relatively large (>~2X neutrophil), +/-nucleolus, +/-gland formation (circular structures), often moderate to abundant cytoplasm.
- Sarcoma = cohesive, composed of spindle cells (cells taper at both ends, nucleus oval/cigar-shaped).
- Germ cell tumour = appearance often similar to carcinoma, site (location) very useful - esp. gonadal, midline, retroperitoneal.
- Neuroendocrine carcinoma = cohesive, fine granular chromatin and no nucleolus.
- Lymphoma = dyscohesive, relatively small (usually <=2X neutrophil diameter), usu. scant basophilic (blue) cytoplasm.
- Melanoma = classically pigmented, often a prominent red nucleolus, a mix of spindle cells and epithelioid cells, mix of cohesive and dyscohesive cells.
A practical histomorphologic differential diagnosis of malignancy
General morphologic DDx of malignancy
| Malignancy | |||||||||||||||||||||||||||||||||
| Large epithelioid tumours | Spindle cell tumours | Small blue cell tumours | Pleomorphic tumours | ||||||||||||||||||||||||||||||
Modified general morphologic DDx of malignancy
| Malignancy | |||||||||||||||||||||||||||||||||||||||||||||||
| Large epithelioid tumours | Spindle cell tumours | Small blue cell tumours | Pleomorphic tumours | Clear cell tumours | Myxoid tumours | ||||||||||||||||||||||||||||||||||||||||||
The above is more useful than the general clinico-histomorphologically motivated differential diagnosis of malignancy.
Differential diagnosis by site
It is essential to have a concept of what is common. The short power list gives a short differential diagnosis for the common sites.
The long power list is a longer list for the common sites.
Finding the elements
Mitoses
- Nucleus darker (hyperchromatic) - key feature.
- No nuclear membrane - key feature.
- In prophase chromatin may have a scalloped border/beaded border.[9]
DDx:
- Apoptotic cell -- has nuclear condensation (pyknosis), eosinophilic cytoplasm.
Images
www:
Phases of mitosis
- Prophase - chromatin condenses to chromosomes.
- Metaphase - chromosome aligned.
- Anaphase - spindles separated.
- Telophase - reversal of prophase.
Neutrophils
- Little dots = the multilobular nucleus - key feature.
- Neutrophils are often found with friends, i.e. lymphocytes, plasma cells.
DDx of little specs:
- Nuclear debris - apoptotic cell.
- Apoptotic cell -- has nuclear condensation (pyknosis), eosinophilic cytoplasm.
Notes:
- AKA PMNs - polymorphonuclearcyte, polymorphonuclear cell.
- You find PMNs by their nucleus; on a histologic section don't bother looking for the cell membrane (they are usually impossible to see).
- A collection of PMNs... think about necrosis and abscess.
Lymph node metastasis
- Take a good to look at the tumour first.
- Tumour in a node is often better differentiated than the most poorly differentiated part in the primary site.
- Subcapsular space - the first place to look for mets.
- Lymph node metastasis are usually obvious.
- There are of course exceptions, e.g. small cell carcinoma, invasive lobular carcinoma.
- Histiocytes may be difficult to separate from tumour - especially for the novice.
- Histiocytes may be found in the germinal centres, i.e. the node architecture helps.
- Malignant cells, generally, have to have malignant features, i.e. the NC ratio is abnormal, there is nuclear pleomorphism.
- Several things can mimic metastases - see Lymph node metastasis.
See: Lymph node article for a detailed description of cell types in a lymph node.
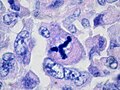
Signet ring cell carcinoma
- It has been said that there are two types of pathologists... those that have missed SRCs and those that will miss SRCs.
Microscopic:
- Cells resemble signet rings:
- They contain a large amount of mucin, which pushes the nucleus to the cell periphery.
- The pool of mucin in a signet ring cell mimics the appearance of a finger hole.
- The nucleus mimics the appearance of the face of the ring in profile.
- Cells typically 2-3x the size of a lymphocyte.
- Smaller than the typical adipocyte.
- Often have a crescent-shaped or ovoid nucleus.
- Capillaries sectioned on their lumen have endothelial cells -- the nuclei of these are more spindled.
- SRCs are usually close to friend -- another SRC.
- This helps differentiate SRCs from capillaries sectioned on their lumen.
- The mucin is often clear on H&E... but maybe eosinophilic.
DDx:
Stains:
- PAS stain.
- Alican blue-PAS stain.
Images
www:
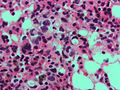
Necrosis
Features:
- Dead cells - pink (on H&E).
- Anucleate cells ("Ghost cells")/outlines of cells - usu. subtle.
- Fluffy appearance.
- Anucleate cells ("Ghost cells")/outlines of cells - usu. subtle.
- +/-Neutrophils (very common).
DDx of necrosis:
- Fibrin.
Images (necrosis):
- Necrosis at the centre of a granuloma (sun.ac.za).
- Necrosis (biomedical-engineering-online.com).
- Necrosis (nature.com).
- Necrosis (ouhsc.edu).[10]
Necrosis in cat scratch disease. (WC/Nephron)
Necrosis in histiocytic necrotizing lymphadenitis. (WC/Nephron)
Necrosis in SLE lymphadenopathy. (WC/Nephron)
Granulomas
Common morphologic problems
DDx of pink stuff (on H&E)
The ABCs of pink:
- Amyloid.
- Blood clot (organized); fibrin.
- Collagen (fibrous tissue).
- Smooth muscle cells (SMCs).
Images
Smooth muscle cells (SMCs) vs. fibrous tissue
Fibroblasts (fibrous tissue):
- Wavy nuclei with pointy ends.
- Less nuclei.
SMCs:
- Elliptical nuclei.
- More nuclei.
Remembering the above:
- SMCs are stretched; ergo, not wavy.
- Fibrous tissue is fibrous... more protein... less cells; ergo, less nuclei.
- Fibroblast = football-like.
- Cigar-shaped nuclei (SMCs) are affected by cigars (smoking causes vascular disease).
Notes:
- Schwann cells (found in nerve): nuclei = wavy appearance, thin. (???)
Pigmented material
- AKA brown/black granular crap.
DDx of granular stuff/pigment:
- Lipofuscin - especially in old people.
- Hemosiderin.
- Bile - found in hepatocytes, yellow.
- Foreign material (tattoo pigment, anthracotic pigment, amalgam tattoo).
- Melanin.
Notes:
- Granular stuff should prompt consideration of malignant melanoma.
- Memory device BH MILF = Bile, Homogentisic acid, Melanin, Iron (hemosiderin), Lipofuscin, Foreign material.
- Homogentisic acid found in alkaptonuria,[11]can be considered the sixth (black) pigment.
- Gentisic = jen-TIS-ik.[12]
Stains that can help sort it out
- Prussian blue (iron stain) for hemosiderin.
- Fontana-Masson stain (or Melan A) for melanin.
- PAS stain[13] or Kluver-Barrera for lipofuscin.
Staining
Basic knowledge of stain is important. The above article starts with H&E and goes from there.
Immunohistochemistry
If the special stains don't help... there is immunohistochemistry.
Food and pathology
Tumour remaining
R classification:[14]
- "RX resection" = residual tumour cannot be assessed.
- "R0 resection" = clean margin macroscopically & microscopically.
- "R1 resection" = microscopic tumour left.
- "R2 resection" = macroscopic tumour left.
Surgeons use this terminology. Essentially, it is the margin status. It is nice when the surgeon's assessment and the pathologist's are in agreement.
Note:
- Generally, positive margins suck. For example, in locally advanced rectal cancer, in one study,[15] five year survival was found to be 60%, 31% and 0% for R0, R1, and R2 resections respectively.
Clinician talk
Performance status
- ECOG - score from 1-5 for performance status.[16]
- ECOG = Eastern Cooperative Oncology Group.
ECOG score:
- ECOG 0: healthy.
- ECOG 1: ambulatory, no strenuous activity.
- ECOG 2: limited to self-care in bed <50% of time.
- ECOG 3: difficult to care for self in bed >50% of time.
- ECOG 4: bed bound.
- ECOG 5: dead.
Pathology & pathologists
Fixation & lifestyle
Pathologist have a great lifestyle 'cause tissue takes long to fix; the penetration of tissue by formalin is 1 mm/hour.[17]
Malignancy & inflammation
If there is lots of inflammation... and you're thinking cancer you should probably back-off, i.e. tend toward benign. Inflammation can make cells look more malignant than they might be if left alone.
Miscellaneous
Infectious stuffs
Images: http://www.uphs.upenn.edu/bugdrug/antibiotic_manual/Gram3.htm
- Staphylococcus - in clusters.
- Streptococcus - in chains.
Microscopes
- Pathologists throw around the term high power field (HPF).
- "HPF" has no agreed upon definition and, IMHO, should never be used without a non-ambiguous definition.
HPF generally refers to the area seen with the largest magnification objective (40x), i.e. the field at 400x (as the eye piece magnification is usually 10x). The field size varies significantly from microscope to microscope.
Estimating field of view
FOV = Deye piece x 1/Mobj.
Where:
- FOV = field of view.
- Deye piece = diameter of eye piece (this is usually inscribed on the side of the eye piece).
- Mobj = magnification of the objective.
Example:
- Deye piece = 22 mm
- Mobj = 40x (largest magnification objective)
Applying the formula:
- FOV = 22 mm / 40
- FOV = 0.55 mm
Note:
- Most modern microscopes, have an eye piece diameter of 22 mm. Therefore, the field diameter at 40 X is approximately 22 mm / 40 X ~= 0.55 mm and the field of view is pi/4*(0.55 mm)^2 = 0.2376 mm^2.
Pathology reports
The key point in report writing is that the report should be precise, complete and easy-to-understand.
Standards
There is no universal standard; however, there is a push to standardize by the Association of Directors of Anatomic and Surgical Pathology,[18] among others.
Checklists
The College of American Pathologists (CAP) has checklists for cancer - CAP protocols.
Pathologists will probably use more checklists in the future... they are deemed effective in a number of places inside and outside of medicine. Surgeons know that checklists work and that they save lives.[19] Pilots have been using checklists since the 1930s.
Standard diagnostic notation
Site, operation/procedure:
- Tissue type diagnosis.
Example:
Gallbladder, cholecystectomy:
- Acute cholecystitis.
Lab talk
Tissue cutting terms - these often vary from lab-to-lab:[20]
- Recut = cut off the top of the block.
- Serial sections = make several cuts off the top of the block and look at all of 'em.
- Level = trim the block ~30 micrometres --throw away trimmed tissue-- and then cut a section to look at.
- Deeper = trim the block ~100 micrometres --throw away trimmed tissue-- and then cut a section to look at.
See also
References
- ↑ Streutker, C. 8 June 2013.
- ↑ URL:http://pancreaticcancer2000.com/page1.htm. Accessed on: 3 June 2010.
- ↑ URL: http://www.merriam-webster.com/medical/argyrophilic. Accessed on: 29 August 2011.
- ↑ URL: http://en.wiktionary.org/wiki/argyrophilic. Accessed on: 29 August 2011.
- ↑ http://upload.wikimedia.org/wikipedia/en/5/51/Nuclear_changes.jpg
- ↑ Arashiro, RT.; Teixeira, MG.; Rawet, V.; Quintanilha, AG.; Paula, HM.; Silva, AZ.; Nahas, SC.; Cecconello, I. (Jul 2012). "Histopathological evaluation and risk factors related to the development of pouchitis in patients with ileal pouches for ulcerative colitis.". Clinics (Sao Paulo) 67 (7): 705-10. PMC 3400158. PMID 22892912. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400158/.
- ↑ 7.0 7.1 S. Boerner. 12 September 2011.
- ↑ URL: http://www.medterms.com/script/main/art.asp?articlekey=25657. Accessed on: 18 January 2010.
- ↑ URL: http://www.microbehunter.com/wp/wp-content/uploads/2009/lily_prophase.jpg and http://www.microbehunter.com/2009/12/06/mitosis-stages-of-the-lily/. Accessed on: 3 November 2010.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com08/Com801-1-Diss.htm. Accessed on: 3 November 2010.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 20. ISBN 978-1416054542.
- ↑ URL: http://dictionary.reference.com/browse/gentisic+acid. Accessed on: 11 January 2012.
- ↑ Kovi J, Leifer C (July 1970). "Lipofuscin pigment accumulation in spontaneous mammary carcinoma of A/Jax mouse". J Natl Med Assoc 62 (4): 287–90. PMC 2611776. PMID 5463681. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2611776/pdf/jnma00512-0077.pdf.
- ↑ URL: http://www.informedicalcme.com/colon-cancer/tnm-stage-groupings/. Accessed on: 27 March 2012.
- ↑ Larsen SG, Wiig JN, Dueland S, Giercksky KE (April 2008). "Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer". Eur J Surg Oncol 34 (4): 410–7. doi:10.1016/j.ejso.2007.05.012. PMID 17614249.
- ↑ Oken MM, Creech RH, Tormey DC, et al. (December 1982). "Toxicity and response criteria of the Eastern Cooperative Oncology Group". Am. J. Clin. Oncol. 5 (6): 649–55. PMID 7165009.
- ↑ Gross rounds. 14 August 2009.
- ↑ URL: http://www.adasp.org/papers/position/Standardization.htm
- ↑ Soar J, Peyton J, Leonard M, Pullyblank AM (2009). "Surgical safety checklists". BMJ 338: b220. PMID 19158173. http://bmj.com/cgi/pmidlookup?view=long&pmid=19158173.
- ↑ URL: http://www.mailman.srv.ualberta.ca/pipermail/patho-l/2002-July/016955.html. Accessed on: 18 October 2011.