Difference between revisions of "Lung tumours"
(→Squamous cell carcinoma of the lung: split out) |
|||
| (52 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
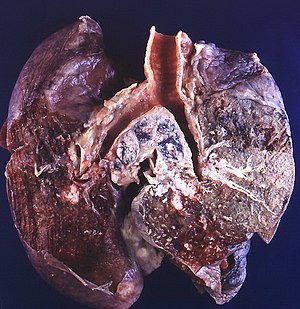
'''[[Lung]] tumours''' comes to pathology to get diagnosed. This article | [[Image:Small cell carcinoma (3931938372).jpg|right|thumb|300px|A lung tumour ([[small cell carcinoma of the lung]]) - centre of image. (WC/Rosen)]] | ||
'''[[Lung]] tumours''' comes to pathology to get diagnosed. | |||
This article deals with the surgical pathology (core biopsies, lung resections). Pulmonary cytopathology is dealt with in the ''[[pulmonary cytopathology]]'' article. | |||
An introduction to lung pathology is found in the ''[[pulmonary pathology]]'' article. | An introduction to lung pathology is found in the ''[[pulmonary pathology]]'' article. | ||
| Line 43: | Line 46: | ||
*Adenocarcinoma is the most common (primary lung cancer).<ref>{{cite journal |author=Lutschg JH |title=Lung cancer |journal=N. Engl. J. Med. |volume=360 |issue=1 |pages=87-8; author reply 88 |year=2009 |month=January |pmid=19118313 |doi=10.1056/NEJMc082208 |url=}}</ref> | *Adenocarcinoma is the most common (primary lung cancer).<ref>{{cite journal |author=Lutschg JH |title=Lung cancer |journal=N. Engl. J. Med. |volume=360 |issue=1 |pages=87-8; author reply 88 |year=2009 |month=January |pmid=19118313 |doi=10.1056/NEJMc082208 |url=}}</ref> | ||
*Adenocarcinoma is the non-smoker tumour - SCLC and squamous are more strongly associated with [[smoking]]. | *Adenocarcinoma is the non-smoker tumour - SCLC and squamous are more strongly associated with [[smoking]]. | ||
Children: | |||
*Most common lung tumour in children: metastasis (80-85% of lung tumours in children<ref name=pmid>{{Cite journal | last1 = Dishop | first1 = MK. | last2 = Kuruvilla | first2 = S. | title = Primary and metastatic lung tumors in the pediatric population: a review and 25-year experience at a large children's hospital. | journal = Arch Pathol Lab Med | volume = 132 | issue = 7 | pages = 1079-103 | month = Jul | year = 2008 | doi = 10.1043/1543-2165(2008)132[1079:PAMLTI]2.0.CO;2 | PMID = 18605764 }}</ref> | |||
**Most common primary tumours in children: [[inflammatory myofibroblastic tumour]], [[pleuropulmonary blastoma]], [[lung carcinoid]].<ref name=pmid26971789>{{Cite journal | last1 = Giuseppucci | first1 = C. | last2 = Reusmann | first2 = A. | last3 = Giubergia | first3 = V. | last4 = Barrias | first4 = C. | last5 = Krüger | first5 = A. | last6 = Siminovich | first6 = M. | last7 = Botto | first7 = H. | last8 = Cadario | first8 = M. | last9 = Boglione | first9 = M. | title = Primary lung tumors in children: 24 years of experience at a referral center. | journal = Pediatr Surg Int | volume = 32 | issue = 5 | pages = 451-7 | month = May | year = 2016 | doi = 10.1007/s00383-016-3884-3 | PMID = 26971789 }}</ref> | |||
===Distribution=== | ===Distribution=== | ||
| Line 48: | Line 55: | ||
**Adenocarcinoma is usually periperal, i.e. smaller airways. | **Adenocarcinoma is usually periperal, i.e. smaller airways. | ||
**Squamous cell carcinoma and small cell carcinoma are typically central. | **Squamous cell carcinoma and small cell carcinoma are typically central. | ||
===Margins in lung=== | |||
Margin in pneumonectomy specimens include: | |||
*Vessels (artery, vein). | |||
*Airway (bronchus). | |||
*Soft tissue (lymphatics, fibrous tissue and lymph nodes).<ref name=pmid21129810>{{Cite journal | last1 = Sakai | first1 = Y. | last2 = Ohbayashi | first2 = C. | last3 = Kanomata | first3 = N. | last4 = Kajimoto | first4 = K. | last5 = Sakuma | first5 = T. | last6 = Maniwa | first6 = Y. | last7 = Nishio | first7 = W. | last8 = Tauchi | first8 = S. | last9 = Uchino | first9 = K. | title = Significance of microscopic invasion into hilar peribronchovascular soft tissue in resection specimens of primary non-small cell lung cancer. | journal = Lung Cancer | volume = 73 | issue = 1 | pages = 89-95 | month = Jul | year = 2011 | doi = 10.1016/j.lungcan.2010.11.002 | PMID = 21129810 }}</ref> | |||
Notes: | |||
*The traditional teaching is there are only hollow structure margins (artery, vein, airway) - yet the bronchial margin has been divided into mucosal and extramucosal.<ref>{{Cite journal | last1 = Kaiser | first1 = LR. | last2 = Fleshner | first2 = P. | last3 = Keller | first3 = S. | last4 = Martini | first4 = N. | title = Significance of extramucosal residual tumor at the bronchial resection margin. | journal = Ann Thorac Surg | volume = 47 | issue = 2 | pages = 265-9 | month = Feb | year = 1989 | doi = | PMID = 2537610 }}</ref> | |||
*Peribronchovascular soft tissue involvement is a poor prognosticator but not an independent predictor if considered within the [[TNM staging]].<ref name=pmid21129810/> | |||
===Management of primary lung cancer=== | ===Management of primary lung cancer=== | ||
Management | Management in the past was determined by categorization into: | ||
*Small cell cancer. | *Small cell cancer. | ||
*Non-small cell cancer (includes adenocarcinoma, squamous cell carcinoma, large cell carcinoma). | *Non-small cell cancer (includes adenocarcinoma, squamous cell carcinoma, large cell carcinoma). | ||
| Line 74: | Line 91: | ||
===Small cell carcinoma=== | ===Small cell carcinoma=== | ||
*CD56 +ve - sensitive.<ref name=pmid16862075>{{cite journal |author=Hiroshima K, Iyoda A, Shida T, ''et al'' |title=Distinction of pulmonary large cell neuroendocrine carcinoma from small cell lung carcinoma: a morphological, immunohistochemical, and molecular analysis |journal=Mod. Pathol. |volume=19 |issue=10 |pages=1358-68 |year=2006 |month=October |pmid=16862075 |doi=10.1038/modpathol.3800659 |url=}}</ref> | *[[TTF-1]] +ve. | ||
*CK7 -ve, CK20 -ve. | *[[CD56]] +ve - sensitive.<ref name=pmid16862075>{{cite journal |author=Hiroshima K, Iyoda A, Shida T, ''et al'' |title=Distinction of pulmonary large cell neuroendocrine carcinoma from small cell lung carcinoma: a morphological, immunohistochemical, and molecular analysis |journal=Mod. Pathol. |volume=19 |issue=10 |pages=1358-68 |year=2006 |month=October |pmid=16862075 |doi=10.1038/modpathol.3800659 |url=}}</ref> | ||
*[[CK7]] -ve, [[CK20]] -ve. | |||
Note: | Note: | ||
*CD56 - cytoplasmic.<ref>URL: [http://jcp.bmjjournals.com/content/58/9/978.full http://jcp.bmjjournals.com/content/58/9/978.full]. Accessed: 11 February 2010.</ref> | *CD56 - cytoplasmic.<ref>URL: [http://jcp.bmjjournals.com/content/58/9/978.full http://jcp.bmjjournals.com/content/58/9/978.full]. Accessed: 11 February 2010.</ref> | ||
===Adenocarcinoma=== | |||
*[[TTF-1]] +ve. | |||
*[[Napsin]] +ve - sensitive.<ref name=pmid22288963>{{cite journal |author=Turner BM, Cagle PT,Fukuoka J, ''et al'' |title=Napsin A, a New Marker for Lung Adenocarcinoma, Is Complementary and More Sensitive and Specific Than Thyroid Transcription Factor 1 in the Differential Diagnosis of Primary Pulmonary Carcinoma: Evaluation of 1674 Cases by Tissue Microarray |journal=Arch Pathol Lab Med. |volume=136 |issue=10 |pages=163-71 |year=2012 |month=February|pmid=22288963 |doi: 10.5858/arpa.2011-0320-OA|url=}}</ref> | |||
*[[CK7]] +ve, [[CK20]] -ve. | |||
===Squamous cell carcinoma=== | ===Squamous cell carcinoma=== | ||
*CK7 -ve, CK20 -ve. | *[[CK7]] -ve, CK20 -ve. | ||
*HMWK +ve. | *HMWK +ve. | ||
*Usually TTF-1 -ve.<ref>{{cite journal |author=Al-Zahrani IH |title=The value of immunohistochemical expression of TTF-1, CK7 and CK20 in the diagnosis of primary and secondary lung carcinomas |journal=Saudi Med J |volume=29 |issue=7 |pages=957-61 |year=2008 |month=July |pmid=18626520 |doi= |url=}}</ref> | *Usually TTF-1 -ve.<ref>{{cite journal |author=Al-Zahrani IH |title=The value of immunohistochemical expression of TTF-1, CK7 and CK20 in the diagnosis of primary and secondary lung carcinomas |journal=Saudi Med J |volume=29 |issue=7 |pages=957-61 |year=2008 |month=July |pmid=18626520 |doi= |url=}}</ref> | ||
*p40 +ve. | *[[p40]] +ve. | ||
===Primary vs. secondary=== | ===Primary vs. secondary=== | ||
| Line 95: | Line 119: | ||
Note: | Note: | ||
*TTF-1 - should be nuclear staining; cytoplasmic staining is non-specific.<ref name=pmid15861215>{{cite journal |author=Compérat E, Zhang F, Perrotin C, ''et al.'' |title=Variable sensitivity and specificity of TTF-1 antibodies in lung metastatic adenocarcinoma of colorectal origin |journal=Mod. Pathol. |volume=18 |issue=10 |pages=1371–6 |year=2005 |month=October |pmid=15861215 |doi=10.1038/modpathol.3800422 |url=http://www.nature.com/modpathol/journal/v18/n10/full/3800422a.html}}</ref> | *TTF-1 - should be nuclear staining; cytoplasmic staining is non-specific.<ref name=pmid15861215>{{cite journal |author=Compérat E, Zhang F, Perrotin C, ''et al.'' |title=Variable sensitivity and specificity of TTF-1 antibodies in lung metastatic adenocarcinoma of colorectal origin |journal=Mod. Pathol. |volume=18 |issue=10 |pages=1371–6 |year=2005 |month=October |pmid=15861215 |doi=10.1038/modpathol.3800422 |url=http://www.nature.com/modpathol/journal/v18/n10/full/3800422a.html}}</ref> | ||
**Image: [http://commons.wikimedia.org/w/index.php?title=File:Lung_adenocarcinoma_-_TTF-1_-_high_mag.jpg Nuclear staining with TTF-1 in a | **Image: [http://commons.wikimedia.org/w/index.php?title=File:Lung_adenocarcinoma_-_TTF-1_-_high_mag.jpg Nuclear staining with TTF-1 in a primary lung adenocarcinoma (WC)]. | ||
==Neuroendocrine tumours== | ==Neuroendocrine tumours== | ||
| Line 101: | Line 125: | ||
===Overview=== | ===Overview=== | ||
*This is a group of tumours that has benign (e.g. [[carcinoid]] tumour of the lung) to malignant (e.g. small cell lung carcinoma) behaviour.<ref>URL: [http://emedicine.medscape.com/article/426400-overview http://emedicine.medscape.com/article/426400-overview]. Accessed on: 20 January 2010.</ref> | *This is a group of tumours that has benign (e.g. [[carcinoid]] tumour of the lung) to malignant (e.g. small cell lung carcinoma) behaviour.<ref>URL: [http://emedicine.medscape.com/article/426400-overview http://emedicine.medscape.com/article/426400-overview]. Accessed on: 20 January 2010.</ref> | ||
*They are thought to arise from | *They are thought to arise from ''pulmonary neuroendocrine cells''.<ref>{{cite journal |author=Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS |title=Neuroendocrine tumors of the lung: clinical, pathologic, and imaging findings |journal=Radiographics |volume=26 |issue=1 |pages=41–57; discussion 57–8 |year=2006 |pmid=16418242 |doi=10.1148/rg.261055057 |url=}}</ref> | ||
===Classification=== | ===Classification=== | ||
| Line 109: | Line 133: | ||
*Typical carcinoid. | *Typical carcinoid. | ||
*Atypical carcinoid. | *Atypical carcinoid. | ||
Notes: | |||
*[[Typical carcinoid]]-like lesions <5 mm are called [[carcinoid tumourlet]]s. | |||
===Cytologic features=== | ===Cytologic features=== | ||
| Line 123: | Line 150: | ||
=Malignant tumours= | =Malignant tumours= | ||
==Adenocarcinoma of the lung== | ==Adenocarcinoma of the lung== | ||
* | *[[AKA]] ''lung adenocarcinoma''. | ||
{{Main|Adenocarcinoma of the lung}} | |||
==Bronchioloalveolar carcinoma== | ==Bronchioloalveolar carcinoma== | ||
| Line 288: | Line 162: | ||
==Small cell carcinoma of the lung== | ==Small cell carcinoma of the lung== | ||
*[[AKA]] ''small cell lung carcinoma'', abbreviated ''SCLC''.<ref name=pmid20943645/> | *[[AKA]] ''small cell lung carcinoma'', abbreviated ''SCLC''.<ref name=pmid20943645>{{Cite journal | last1 = Travis | first1 = WD. | title = Advances in neuroendocrine lung tumors. | journal = Ann Oncol | volume = 21 Suppl 7 | issue = | pages = vii65-71 | month = Oct | year = 2010 | doi = 10.1093/annonc/mdq380 | PMID = 20943645 }}</ref> | ||
{{Main|Small cell carcinoma of the lung}} | {{Main|Small cell carcinoma of the lung}} | ||
| Line 294: | Line 168: | ||
:Should '''not''' be confused with ''[[benign multicystic mesothelioma]]'' and ''[[benign papillary mesothelioma]]''. | :Should '''not''' be confused with ''[[benign multicystic mesothelioma]]'' and ''[[benign papillary mesothelioma]]''. | ||
{{Main|Malignant mesothelioma}} | {{Main|Malignant mesothelioma}} | ||
==Non-small cell lung carcinoma== | |||
*[[AKA]] ''poorly differentiated carcinoma of the lung''. | |||
{{Main|Non-small cell lung carcinoma}} | |||
==Adenosquamous carcinoma of the lung== | |||
{{Main|Adenosquamous carcinoma of the lung}} | |||
==Lung metastasis== | |||
*[[AKA]] ''pulmonary metastasis''. | |||
{{Main|Lung metastasis}} | |||
=Malignant potential= | =Malignant potential= | ||
| Line 299: | Line 184: | ||
*Abbreviated ''AAH''. | *Abbreviated ''AAH''. | ||
*[[AKA]] ''atypical adenomatous hyperplasia of the lung''.<ref name=pmid11235908>{{Cite journal | last1 = Mori | first1 = M. | last2 = Rao | first2 = SK. | last3 = Popper | first3 = HH. | last4 = Cagle | first4 = PT. | last5 = Fraire | first5 = AE. | title = Atypical adenomatous hyperplasia of the lung: a probable forerunner in the development of adenocarcinoma of the lung. | journal = Mod Pathol | volume = 14 | issue = 2 | pages = 72-84 | month = Feb | year = 2001 | doi = 10.1038/modpathol.3880259 | PMID = 11235908 }}</ref> | *[[AKA]] ''atypical adenomatous hyperplasia of the lung''.<ref name=pmid11235908>{{Cite journal | last1 = Mori | first1 = M. | last2 = Rao | first2 = SK. | last3 = Popper | first3 = HH. | last4 = Cagle | first4 = PT. | last5 = Fraire | first5 = AE. | title = Atypical adenomatous hyperplasia of the lung: a probable forerunner in the development of adenocarcinoma of the lung. | journal = Mod Pathol | volume = 14 | issue = 2 | pages = 72-84 | month = Feb | year = 2001 | doi = 10.1038/modpathol.3880259 | PMID = 11235908 }}</ref> | ||
{{Main|Atypical adenomatous hyperplasia of the lung}} | |||
==Atypical carcinoid lung tumour== | ==Atypical carcinoid lung tumour== | ||
*[[AKA]] ''atypical carcinoid tumour of the lung''. | *[[AKA]] ''atypical carcinoid tumour of the lung''. | ||
{{Main|Atypical lung carcinoid tumour}} | |||
==Solitary fibrous tumour of the pleura== | ==Solitary fibrous tumour of the pleura== | ||
{{Main|Solitary fibrous tumour of the pleura}} | |||
=== | =Benign tumours= | ||
==Pulmonary apical cap== | |||
{{Main|Pulmonary apical cap}} | |||
A lesion that can mimic a lung neoplasm. | |||
==Pulmonary carcinoid tumourlet== | ==Pulmonary carcinoid tumourlet== | ||
*[[AKA]] ''carcinoid tumourlet''. | *[[AKA]] ''carcinoid tumourlet''. | ||
{{Main|Pulmonary carcinoid tumourlet}} | |||
==Typical carcinoid lung tumour== | ==Typical carcinoid lung tumour== | ||
*[[AKA]] ''carcinoid tumour of the lung''. | *[[AKA]] ''carcinoid tumour of the lung''. | ||
*[[AKA]] ''lung carcinoid''. | *[[AKA]] ''lung carcinoid''. | ||
{{Main|Typical carcinoid lung tumour}} | |||
==Clear cell sugar tumour of the lung== | ==Clear cell sugar tumour of the lung== | ||
*[[AKA]] ''clear cell sugar tumour''. | *[[AKA]] ''clear cell sugar tumour''. | ||
**Abbreviated ''CCST''. | **Abbreviated ''CCST''. | ||
{{Main|Clear cell sugar tumour of the lung}} | |||
=See also= | =See also= | ||
| Line 444: | Line 218: | ||
*[[Basics]]. | *[[Basics]]. | ||
*[[Heart]]. | *[[Heart]]. | ||
*[[Missed endobronchial biopsy]]. | |||
=References= | =References= | ||
Latest revision as of 23:44, 17 March 2019
Lung tumours comes to pathology to get diagnosed.
This article deals with the surgical pathology (core biopsies, lung resections). Pulmonary cytopathology is dealt with in the pulmonary cytopathology article.
An introduction to lung pathology is found in the pulmonary pathology article.
Lung tumours overview
Schematic overview of lung cancer (clinical)
| Lung cancer | |||||||||||||||||||||||||||||||||||||||||
| Primary | Metastatic | ||||||||||||||||||||||||||||||||||||||||
| NSCLC | SCLC | ||||||||||||||||||||||||||||||||||||||||
- NSCLC = non-small cell lung cancer.
- SCLS = small cell lung cancer.
Basic pathologic approach to lung cancer
| Lung cancer | |||||||||||||||||||||||||||||||
| Adenocarcinoma | Squamous cell carcinoma | SCLC | LCLC | ||||||||||||||||||||||||||||
- LCLC = large cell lung cancer.
- SCLS = small cell lung cancer.
Notes:
- Most lung cancer fits into one of the above categories.
- All types may be metastatic. Pathologists usually don't have to sort this out, as the clinican often knows whether a given lesion is metastatic (when correlated with radiology).
- Lung cancers may have a mixed morphology, e.g. SCLS may have squamous component.[1]
- Categorization as non-small cell lung cancer (NSCLC) should be avoided, as treatment is now somewhat dependent on subcategorization.[2]
Major types (primary)
Mnemonic ASSL:
- Adenocarcinoma.
- Squamous cell carcinoma.
- Small cell carcinoma (SCLC).
- Large cell carcinoma (LCLC).
Epidemiology
- Adenocarcinoma is the most common (primary lung cancer).[3]
- Adenocarcinoma is the non-smoker tumour - SCLC and squamous are more strongly associated with smoking.
Children:
- Most common lung tumour in children: metastasis (80-85% of lung tumours in children[4]
- Most common primary tumours in children: inflammatory myofibroblastic tumour, pleuropulmonary blastoma, lung carcinoid.[5]
Distribution
- Distribution - think about the location of letters in mnemonic ASSL.
- Adenocarcinoma is usually periperal, i.e. smaller airways.
- Squamous cell carcinoma and small cell carcinoma are typically central.
Margins in lung
Margin in pneumonectomy specimens include:
- Vessels (artery, vein).
- Airway (bronchus).
- Soft tissue (lymphatics, fibrous tissue and lymph nodes).[6]
Notes:
- The traditional teaching is there are only hollow structure margins (artery, vein, airway) - yet the bronchial margin has been divided into mucosal and extramucosal.[7]
- Peribronchovascular soft tissue involvement is a poor prognosticator but not an independent predictor if considered within the TNM staging.[6]
Management of primary lung cancer
Management in the past was determined by categorization into:
- Small cell cancer.
- Non-small cell cancer (includes adenocarcinoma, squamous cell carcinoma, large cell carcinoma).
Microscopic features overview
Adenocarcinoma
- Glands or cytoplasm with mucin.
Squamous cell carcinoma
- Distinct cell borders with intercellular bridges.
- Eosinophilic cytoplasm.
Small cell carcinoma
- Very cellular.
- Large NC ratio - very small amount of cytoplasm.
- Cells fragile - they tend to look "smudged" (Azzopardi phenomenon).
IHC
There is a great review paper by Jagirdar.[8]
Small cell carcinoma
Note:
- CD56 - cytoplasmic.[10]
Adenocarcinoma
Squamous cell carcinoma
Primary vs. secondary
- TTF-1 is considered useful.[8]
- 75% +ve adenocarcinoma
- 11% +ve SSC
- 50% +ve large cell carcinoma
- 0% +ve mesothelioma
- significant rates of +ve in some metastatic tumours -- see article by Jagirdar.
Note:
- TTF-1 - should be nuclear staining; cytoplasmic staining is non-specific.[13]
Neuroendocrine tumours
Overview
- This is a group of tumours that has benign (e.g. carcinoid tumour of the lung) to malignant (e.g. small cell lung carcinoma) behaviour.[14]
- They are thought to arise from pulmonary neuroendocrine cells.[15]
Classification
The grouping can be divided into four types:[16]
- Small cell carcinoma.
- Large cell neuroendocrine carcinoma.
- Typical carcinoid.
- Atypical carcinoid.
Notes:
- Typical carcinoid-like lesions <5 mm are called carcinoid tumourlets.
Cytologic features
Cytologic features useful for differentiation:
- Small cell carcinoma: necrosis, scant cytoplasm, mitoses.
- Typical carcinoid: often more cytoplasm, no necrosis, low mitotic rate (MIB1: scant staining).
- Atypical carcinoid: higher mitotic rate/MIB1 than typical carcinoid,[17] no necrosis.
Notes:[16]
- Large cell and small cell tumours behave in a similar fashion; large cell can be considered a morphological variant of small cell.
- 9/10 of carcinoids are typical and usually have a good prognosis, i.e. do not metastasize.
- Central location (vis-a-vis peripheral location) tends favours typical carcinoid over atypical carcinoid.
Malignant tumours
Adenocarcinoma of the lung
- AKA lung adenocarcinoma.
Bronchioloalveolar carcinoma
- Abbreviated BAC.
The term is no longer used in the new classification;[18] it is now "adenocarcinoma in situ" - see lung adenocarcinoma.
Squamous cell carcinoma of the lung
Small cell carcinoma of the lung
Malignant mesothelioma
- Should not be confused with benign multicystic mesothelioma and benign papillary mesothelioma.
Non-small cell lung carcinoma
- AKA poorly differentiated carcinoma of the lung.
Adenosquamous carcinoma of the lung
Lung metastasis
- AKA pulmonary metastasis.
Malignant potential
Atypical alveolar hyperplasia
Atypical carcinoid lung tumour
- AKA atypical carcinoid tumour of the lung.
Solitary fibrous tumour of the pleura
Benign tumours
Pulmonary apical cap
A lesion that can mimic a lung neoplasm.
Pulmonary carcinoid tumourlet
- AKA carcinoid tumourlet.
Typical carcinoid lung tumour
Clear cell sugar tumour of the lung
- AKA clear cell sugar tumour.
- Abbreviated CCST.
See also
- Lung - introduction to the lung, includes a basic approach.
- Medical lung disease.
- Thyroid.
- Basics.
- Heart.
- Missed endobronchial biopsy.
References
- ↑ Righi L, Volante M, Rapa I, Scagliotti GV, Papotti M (August 2007). "Neuro-endocrine tumours of the lung. A review of relevant pathological and molecular data". Virchows Arch. 451 Suppl 1: S51–9. doi:10.1007/s00428-007-0445-0. PMID 17684766.
- ↑ URL: http://www.nature.com/modpathol/journal/v21/n2s/full/3801018a.html. Accessed on: 8 September 2010.
- ↑ Lutschg JH (January 2009). "Lung cancer". N. Engl. J. Med. 360 (1): 87-8; author reply 88. doi:10.1056/NEJMc082208. PMID 19118313.
- ↑ Dishop, MK.; Kuruvilla, S. (Jul 2008). "Primary and metastatic lung tumors in the pediatric population: a review and 25-year experience at a large children's hospital.". Arch Pathol Lab Med 132 (7): 1079-103. doi:10.1043/1543-2165(2008)132[1079:PAMLTI]2.0.CO;2. PMID 18605764.
- ↑ Giuseppucci, C.; Reusmann, A.; Giubergia, V.; Barrias, C.; Krüger, A.; Siminovich, M.; Botto, H.; Cadario, M. et al. (May 2016). "Primary lung tumors in children: 24 years of experience at a referral center.". Pediatr Surg Int 32 (5): 451-7. doi:10.1007/s00383-016-3884-3. PMID 26971789.
- ↑ 6.0 6.1 Sakai, Y.; Ohbayashi, C.; Kanomata, N.; Kajimoto, K.; Sakuma, T.; Maniwa, Y.; Nishio, W.; Tauchi, S. et al. (Jul 2011). "Significance of microscopic invasion into hilar peribronchovascular soft tissue in resection specimens of primary non-small cell lung cancer.". Lung Cancer 73 (1): 89-95. doi:10.1016/j.lungcan.2010.11.002. PMID 21129810.
- ↑ Kaiser, LR.; Fleshner, P.; Keller, S.; Martini, N. (Feb 1989). "Significance of extramucosal residual tumor at the bronchial resection margin.". Ann Thorac Surg 47 (2): 265-9. PMID 2537610.
- ↑ 8.0 8.1 Jagirdar J (March 2008). "Application of immunohistochemistry to the diagnosis of primary and metastatic carcinoma to the lung". Arch. Pathol. Lab. Med. 132 (3): 384-96. PMID 18318581. http://journals.allenpress.com/jrnlserv/?request=get-abstract&issn=0003-9985&volume=132&page=384.
- ↑ Hiroshima K, Iyoda A, Shida T, et al (October 2006). "Distinction of pulmonary large cell neuroendocrine carcinoma from small cell lung carcinoma: a morphological, immunohistochemical, and molecular analysis". Mod. Pathol. 19 (10): 1358-68. doi:10.1038/modpathol.3800659. PMID 16862075.
- ↑ URL: http://jcp.bmjjournals.com/content/58/9/978.full. Accessed: 11 February 2010.
- ↑ Turner BM, Cagle PT,Fukuoka J, et al (February 2012). "Napsin A, a New Marker for Lung Adenocarcinoma, Is Complementary and More Sensitive and Specific Than Thyroid Transcription Factor 1 in the Differential Diagnosis of Primary Pulmonary Carcinoma: Evaluation of 1674 Cases by Tissue Microarray". Arch Pathol Lab Med. 136 (10): 163-71. PMID 22288963.
- ↑ Al-Zahrani IH (July 2008). "The value of immunohistochemical expression of TTF-1, CK7 and CK20 in the diagnosis of primary and secondary lung carcinomas". Saudi Med J 29 (7): 957-61. PMID 18626520.
- ↑ Compérat E, Zhang F, Perrotin C, et al. (October 2005). "Variable sensitivity and specificity of TTF-1 antibodies in lung metastatic adenocarcinoma of colorectal origin". Mod. Pathol. 18 (10): 1371–6. doi:10.1038/modpathol.3800422. PMID 15861215. http://www.nature.com/modpathol/journal/v18/n10/full/3800422a.html.
- ↑ URL: http://emedicine.medscape.com/article/426400-overview. Accessed on: 20 January 2010.
- ↑ Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS (2006). "Neuroendocrine tumors of the lung: clinical, pathologic, and imaging findings". Radiographics 26 (1): 41–57; discussion 57–8. doi:10.1148/rg.261055057. PMID 16418242.
- ↑ 16.0 16.1 URL: http://www.cancer.org/docroot/CRI/content/CRI_2_4_1X_What_is_lung_carcinoid_tumor_56.asp. Accessed on: 16 February 2011.
- ↑ Geddie, W. February 2010.
- ↑ Travis, WD.; Brambilla, E.; Noguchi, M.; Nicholson, AG.; Geisinger, K.; Yatabe, Y.; Powell, CA.; Beer, D. et al. (Sep 2011). "International association for the study of lung cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary.". Proc Am Thorac Soc 8 (5): 381-5. doi:10.1513/pats.201107-042ST. PMID 21926387.
- ↑ Travis, WD. (Oct 2010). "Advances in neuroendocrine lung tumors.". Ann Oncol 21 Suppl 7: vii65-71. doi:10.1093/annonc/mdq380. PMID 20943645.
- ↑ Mori, M.; Rao, SK.; Popper, HH.; Cagle, PT.; Fraire, AE. (Feb 2001). "Atypical adenomatous hyperplasia of the lung: a probable forerunner in the development of adenocarcinoma of the lung.". Mod Pathol 14 (2): 72-84. doi:10.1038/modpathol.3880259. PMID 11235908.