Difference between revisions of "Acute appendicitis"
m (tweak) |
|||
| (20 intermediate revisions by 2 users not shown) | |||
| Line 26: | Line 26: | ||
| Prognosis = good | | Prognosis = good | ||
| Other = | | Other = | ||
| ClinDDx = symptomatic [[Meckel diverticulum]], epiploic appendagitis, [[ectopic pregnancy]], ruptured ovarian cyst, ovarian torsion, pelvic inflammatory disease | | ClinDDx = symptomatic [[Meckel diverticulum]], [[epiploic appendagitis]], [[ectopic pregnancy]], ruptured ovarian cyst, [[ovarian torsion]], pelvic inflammatory disease, benign fecal impaction | ||
}} | }} | ||
'''Acute appendicitis''' is very common | '''Acute appendicitis''', abbreviated '''AA''', is an acute inflammation of the [[vermiform appendix]]. It is very common and keeps general surgeons busy. | ||
==General== | ==General== | ||
*Bread 'n butter of general surgery. | *Bread 'n butter of [[general surgery]]. | ||
*Interesting factoid: appendicitis is considered protective against [[ulcerative colitis]].<ref name=pmid19685454>{{Cite journal | last1 = Beaugerie | first1 = L. | last2 = Sokol | first2 = H. | title = Appendicitis, not appendectomy, is protective against ulcerative colitis, both in the general population and first-degree relatives of patients with IBD. | journal = Inflamm Bowel Dis | volume = | issue = | pages = | month = Aug | year = 2009 | doi = 10.1002/ibd.21064 | PMID = 19685454 }}</ref><ref name=pmid19273505>{{Cite journal | last1 = Timmer | first1 = A. | last2 = Obermeier | first2 = F. | title = Reduced risk of ulcerative colitis after appendicectomy. | journal = BMJ | volume = 338 | issue = | pages = b225 | month = | year = 2009 | doi = | PMID = 19273505 }}</ref> | *Interesting factoid: appendicitis is considered protective against [[ulcerative colitis]].<ref name=pmid19685454>{{Cite journal | last1 = Beaugerie | first1 = L. | last2 = Sokol | first2 = H. | title = Appendicitis, not appendectomy, is protective against ulcerative colitis, both in the general population and first-degree relatives of patients with IBD. | journal = Inflamm Bowel Dis | volume = | issue = | pages = | month = Aug | year = 2009 | doi = 10.1002/ibd.21064 | PMID = 19685454 }}</ref><ref name=pmid19273505>{{Cite journal | last1 = Timmer | first1 = A. | last2 = Obermeier | first2 = F. | title = Reduced risk of ulcerative colitis after appendicectomy. | journal = BMJ | volume = 338 | issue = | pages = b225 | month = | year = 2009 | doi = | PMID = 19273505 }}</ref> | ||
| Line 38: | Line 38: | ||
**Symptomatic [[Meckel diverticulum]]. | **Symptomatic [[Meckel diverticulum]]. | ||
**Epiploic appendagitis. | **Epiploic appendagitis. | ||
**Benign fecal impaction of the appendix.<ref name=pmid17875592>{{Cite journal | last1 = Park | first1 = NH. | last2 = Park | first2 = CS. | last3 = Lee | first3 = EJ. | last4 = Kim | first4 = MS. | last5 = Ryu | first5 = JA. | last6 = Bae | first6 = JM. | last7 = Song | first7 = JS. | title = Ultrasonographic findings identifying the faecal-impacted appendix: differential findings with acute appendicitis. | journal = Br J Radiol | volume = 80 | issue = 959 | pages = 872-7 | month = Nov | year = 2007 | doi = 10.1259/bjr/80553348 | PMID = 17875592 }}</ref> | |||
*Gynecologic tract: | *Gynecologic tract: | ||
**[[Ectopic pregnancy]]. | **[[Ectopic pregnancy]]. | ||
**Ruptured ovarian cyst. | **Ruptured ovarian cyst. | ||
**Ovarian torsion. | **Ovarian torsion +/-[[ovarian tumour]]. | ||
**Pelvic inflammatory disease. | |||
==Gross== | ==Gross== | ||
| Line 68: | Line 69: | ||
Note: | Note: | ||
* | *[[Eosinophil]]s are very common.<ref name=pmid9444860>{{Cite journal | last1 = Aravindan | first1 = KP. | title = Eosinophils in acute appendicitis: possible significance. | journal = Indian J Pathol Microbiol | volume = 40 | issue = 4 | pages = 491-8 | month = Oct | year = 1997 | doi = | PMID = 9444860 }}</ref> | ||
**Appendices with eosinophils but no apparent [[neutrophil]]s probably represent the same process.<ref name=pmid20551528>{{Cite journal | last1 = Aravindan | first1 = KP. | last2 = Vijayaraghavan | first2 = D. | last3 = Manipadam | first3 = MT. | title = Acute eosinophilic appendicitis and the significance of eosinophil - Edema lesion. | journal = Indian J Pathol Microbiol | volume = 53 | issue = 2 | pages = 258-61 | month = | year = | doi = 10.4103/0377-4929.64343 | PMID = 20551528 }}</ref> | **Appendices with eosinophils but no apparent [[neutrophil]]s probably represent the same process.<ref name=pmid20551528>{{Cite journal | last1 = Aravindan | first1 = KP. | last2 = Vijayaraghavan | first2 = D. | last3 = Manipadam | first3 = MT. | title = Acute eosinophilic appendicitis and the significance of eosinophil - Edema lesion. | journal = Indian J Pathol Microbiol | volume = 53 | issue = 2 | pages = 258-61 | month = | year = | doi = 10.4103/0377-4929.64343 | PMID = 20551528 }}</ref> | ||
| Line 75: | Line 76: | ||
*[[Adenovirus appendicitis]] - lymphoid hyperplasia. | *[[Adenovirus appendicitis]] - lymphoid hyperplasia. | ||
*[[Mucinous_tumours_of_the_appendix|Mucinous tumour]] - usu. apparent on gross. | *[[Mucinous_tumours_of_the_appendix|Mucinous tumour]] - usu. apparent on gross. | ||
*[[ | *[[Appendiceal neuroendocrine tumour]]. | ||
*[[Granulomatous appendicitis]]. | *[[Granulomatous appendicitis]]. | ||
*[[Crohn's disease]] of the appendix. | *[[Crohn's disease]] of the appendix. | ||
**Approximately of 40% colectomies for CD (that include an appendix) have involvement of the appendix.<ref name=pmid11956821>{{Cite journal | last1 = Stangl | first1 = PC. | last2 = Herbst | first2 = F. | last3 = Birner | first3 = P. | last4 = Oberhuber | first4 = G. | title = Crohn's disease of the appendix. | journal = Virchows Arch | volume = 440 | issue = 4 | pages = 397-403 | month = Apr | year = 2002 | doi = 10.1007/s004280100532 | PMID = 11956821 }}</ref> | **Approximately of 40% colectomies for CD (that include an appendix) have involvement of the appendix.<ref name=pmid11956821>{{Cite journal | last1 = Stangl | first1 = PC. | last2 = Herbst | first2 = F. | last3 = Birner | first3 = P. | last4 = Oberhuber | first4 = G. | title = Crohn's disease of the appendix. | journal = Virchows Arch | volume = 440 | issue = 4 | pages = 397-403 | month = Apr | year = 2002 | doi = 10.1007/s004280100532 | PMID = 11956821 }}</ref> | ||
*[[Crypt cell carcinoma]] (goblet cell carcinoid) - may be subtle. | |||
*[[Interval appendectomy]] - may have active inflammation - [[clinical history]] is essential to differentiate.<ref>{{cite journal |authors=Malvar G, Peric M, Gonzalez RS |title=Interval appendicitis shows histological differences from acute appendicitis and may mimic Crohn disease and other forms of granulomatous appendicitis |journal=Histopathology |volume=80 |issue=6 |pages=965–973 |date=May 2022 |pmid=35076982 |doi=10.1111/his.14621 |url=}}</ref> | |||
===Images=== | ===Images=== | ||
| Line 84: | Line 87: | ||
Image:Appendicitis_-_low_mag.jpg | Appendicitis - low mag. (WC/Nephron) | Image:Appendicitis_-_low_mag.jpg | Appendicitis - low mag. (WC/Nephron) | ||
Image:Appendicitis_-_very_high_mag.jpg | Appendicitis - very high mag. (WC/Nephron) | Image:Appendicitis_-_very_high_mag.jpg | Appendicitis - very high mag. (WC/Nephron) | ||
Image:Appendix Appendicitis PA.JPG|Acute Appendicitis(SKB) | |||
</gallery> | </gallery> | ||
==Sign out== | ==Sign out== | ||
<pre> | |||
Vermiform Appendix, Appendectomy: | |||
- Acute appendicitis with acute periappendicitis. | |||
</pre> | |||
===Block letters=== | |||
<pre> | <pre> | ||
VERMIFORM APPENDIX, APPENDECTOMY: | VERMIFORM APPENDIX, APPENDECTOMY: | ||
| Line 93: | Line 103: | ||
</pre> | </pre> | ||
<pre> | |||
VERMIFORM APPENDIX, APPENDECTOMY: | |||
- ACUTE APPENDICITIS WITH FOCAL NECROSIS OF THE APPENDICEAL WALL. | |||
- ACUTE PERIAPPENDICITIS. | |||
</pre> | |||
===Gangrenous=== | |||
<pre> | <pre> | ||
VERMIFORM APPENDIX, APPENDECTOMY: | VERMIFORM APPENDIX, APPENDECTOMY: | ||
- GANGRENOUS APPENDICITIS. | - GANGRENOUS APPENDICITIS. | ||
- ACUTE PERIAPPENDICITIS. | - ACUTE PERIAPPENDICITIS. | ||
</pre> | |||
<pre> | |||
VERMIFORM APPENDIX, APPENDECTOMY: | |||
- GANGRENOUS APPENDICITIS WITH PERFORATION. | |||
- ACUTE PERIAPPENDICITIS. | |||
</pre> | |||
<pre> | |||
VERMIFORM APPENDIX, APPENDECTOMY: | |||
- ACUTE APPENDICITIS WITH GANGRENOUS CHANGES. | |||
- ACUTE PERIAPPENDICITIS. | |||
</pre> | </pre> | ||
| Line 103: | Line 132: | ||
VERMIFORM APPENDIX, APPENDECTOMY: | VERMIFORM APPENDIX, APPENDECTOMY: | ||
- ACUTE APPENDICITIS WITH PERFORATION AND ACUTE PERIAPPENDICITIS. | - ACUTE APPENDICITIS WITH PERFORATION AND ACUTE PERIAPPENDICITIS. | ||
</pre> | |||
<pre> | |||
VERMIFORM APPENDIX, APPENDECTOMY: | |||
- PERFORATED ACUTE APPENDICITIS WITH ACUTE PERIAPPENDICITIS. | |||
</pre> | </pre> | ||
This is uncommon to see definitively on histology. | This is uncommon to see definitively on histology. | ||
===Micro=== | ===Micro=== | ||
====Gangrenous appendicitis==== | ====Gangrenous appendicitis==== | ||
The sections | The sections show appendiceal wall with marked acute transmural inflammation and necrotic appendiceal wall with large collections of neutrophils. Several medium-sized blood vessels are thrombosed. A thick layer of neutrophils cover the serosal aspect. | ||
=====Alternate - less developed===== | |||
The sections show appendiceal wall with marked acute inflammation and a focally | |||
necrotic appendiceal wall with large collections of neutrophils. Intravascular fibrin | |||
is seen in medium-sized blood vessels. Clusters of neutrophils are seen on the serosal | |||
aspect. | |||
==See also== | ==See also== | ||
Latest revision as of 16:09, 30 November 2023
Acute appendicitis, abbreviated AA, is an acute inflammation of the vermiform appendix. It is very common and keeps general surgeons busy.
| Acute appendicitis | |
|---|---|
| Diagnosis in short | |
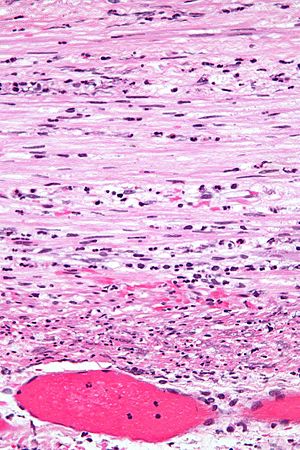 Acute appendicitis. H&E stain. | |
|
| |
| LM | neutrophils in the muscularis propria |
| LM DDx | adenovirus appendicitis, negative appendectomy, Granulomatous appendicitis, Crohn's disease of the appendix, appendiceal neuroendocrine tumour, mucinous tumour of the appendix |
| Gross | serosal surface dull, +/-fibrinous exudate, +/-perforation |
| Site | vermiform appendix |
|
| |
| Clinical history | classically periumbilical pain then right lower quadrant pain, usu. younger patients |
| Signs | rebound tenderness, tenderness at McBurney's point, Rovsing sign, psoas sign, obturator sign |
| Prevalence | common |
| Blood work | leukocytosis |
| Radiology | periappendiceal fat stranding, increased appendiceal diameter |
| Prognosis | good |
| Clin. DDx | symptomatic Meckel diverticulum, epiploic appendagitis, ectopic pregnancy, ruptured ovarian cyst, ovarian torsion, pelvic inflammatory disease, benign fecal impaction |
General
- Bread 'n butter of general surgery.
- Interesting factoid: appendicitis is considered protective against ulcerative colitis.[1][2]
Short clinical DDx:
- GI tract:
- Symptomatic Meckel diverticulum.
- Epiploic appendagitis.
- Benign fecal impaction of the appendix.[3]
- Gynecologic tract:
- Ectopic pregnancy.
- Ruptured ovarian cyst.
- Ovarian torsion +/-ovarian tumour.
- Pelvic inflammatory disease.
Gross
Features:
- Serosal surface dull.
- May be perforated (best determined on gross).
- +/-Fibrinous exudate.
Note:
- Normal diameter of appendix (based on CT): 6.6 +/- 1.5 mm.[4]
- Similar numbers are found in another study.[5]
Image:
Microscopic
Features:
- Neutrophils in the muscularis propria - key feature.
- +/- Vascular thrombosis (and necrosis) - known as gangrenous appendicitis.[6]
- +/- Findings suggestive of etiology - usu. absent:
- +/- Fecalith.
- +/- Viral inclusions (extremely rare)
Note:
- Eosinophils are very common.[7]
- Appendices with eosinophils but no apparent neutrophils probably represent the same process.[8]
DDx:
- Negative appendectomy - specimen should be submitted in toto, no lymphoid hyperplasia.
- Adenovirus appendicitis - lymphoid hyperplasia.
- Mucinous tumour - usu. apparent on gross.
- Appendiceal neuroendocrine tumour.
- Granulomatous appendicitis.
- Crohn's disease of the appendix.
- Approximately of 40% colectomies for CD (that include an appendix) have involvement of the appendix.[9]
- Crypt cell carcinoma (goblet cell carcinoid) - may be subtle.
- Interval appendectomy - may have active inflammation - clinical history is essential to differentiate.[10]
Images
Sign out
Vermiform Appendix, Appendectomy: - Acute appendicitis with acute periappendicitis.
Block letters
VERMIFORM APPENDIX, APPENDECTOMY: - ACUTE APPENDICITIS. - ACUTE PERIAPPENDICITIS.
VERMIFORM APPENDIX, APPENDECTOMY: - ACUTE APPENDICITIS WITH FOCAL NECROSIS OF THE APPENDICEAL WALL. - ACUTE PERIAPPENDICITIS.
Gangrenous
VERMIFORM APPENDIX, APPENDECTOMY: - GANGRENOUS APPENDICITIS. - ACUTE PERIAPPENDICITIS.
VERMIFORM APPENDIX, APPENDECTOMY: - GANGRENOUS APPENDICITIS WITH PERFORATION. - ACUTE PERIAPPENDICITIS.
VERMIFORM APPENDIX, APPENDECTOMY: - ACUTE APPENDICITIS WITH GANGRENOUS CHANGES. - ACUTE PERIAPPENDICITIS.
Perforated appendicitis
VERMIFORM APPENDIX, APPENDECTOMY: - ACUTE APPENDICITIS WITH PERFORATION AND ACUTE PERIAPPENDICITIS.
VERMIFORM APPENDIX, APPENDECTOMY: - PERFORATED ACUTE APPENDICITIS WITH ACUTE PERIAPPENDICITIS.
This is uncommon to see definitively on histology.
Micro
Gangrenous appendicitis
The sections show appendiceal wall with marked acute transmural inflammation and necrotic appendiceal wall with large collections of neutrophils. Several medium-sized blood vessels are thrombosed. A thick layer of neutrophils cover the serosal aspect.
Alternate - less developed
The sections show appendiceal wall with marked acute inflammation and a focally necrotic appendiceal wall with large collections of neutrophils. Intravascular fibrin is seen in medium-sized blood vessels. Clusters of neutrophils are seen on the serosal aspect.
See also
References
- ↑ Beaugerie, L.; Sokol, H. (Aug 2009). "Appendicitis, not appendectomy, is protective against ulcerative colitis, both in the general population and first-degree relatives of patients with IBD.". Inflamm Bowel Dis. doi:10.1002/ibd.21064. PMID 19685454.
- ↑ Timmer, A.; Obermeier, F. (2009). "Reduced risk of ulcerative colitis after appendicectomy.". BMJ 338: b225. PMID 19273505.
- ↑ Park, NH.; Park, CS.; Lee, EJ.; Kim, MS.; Ryu, JA.; Bae, JM.; Song, JS. (Nov 2007). "Ultrasonographic findings identifying the faecal-impacted appendix: differential findings with acute appendicitis.". Br J Radiol 80 (959): 872-7. doi:10.1259/bjr/80553348. PMID 17875592.
- ↑ Charoensak, A.; Pongpornsup, S.; Suthikeeree, W. (Dec 2010). "Wall thickness and outer diameter of the normal appendix in adults using 64 slices multidetector CT.". J Med Assoc Thai 93 (12): 1437-42. PMID 21344807.
- ↑ Huwart, L.; El Khoury, M.; Lesavre, A.; Phan, C.; Rangheard, AS.; Bessoud, B.; Menu, Y. (Mar 2007). "[What is the thickness of the normal appendix on MDCT?].". J Radiol 88 (3 Pt 1): 385-9. PMID 17457270.
- ↑ URL: http://emedicine.medscape.com/article/363818-overview. Accessed on: 21 June 2010.
- ↑ Aravindan, KP. (Oct 1997). "Eosinophils in acute appendicitis: possible significance.". Indian J Pathol Microbiol 40 (4): 491-8. PMID 9444860.
- ↑ Aravindan, KP.; Vijayaraghavan, D.; Manipadam, MT.. "Acute eosinophilic appendicitis and the significance of eosinophil - Edema lesion.". Indian J Pathol Microbiol 53 (2): 258-61. doi:10.4103/0377-4929.64343. PMID 20551528.
- ↑ Stangl, PC.; Herbst, F.; Birner, P.; Oberhuber, G. (Apr 2002). "Crohn's disease of the appendix.". Virchows Arch 440 (4): 397-403. doi:10.1007/s004280100532. PMID 11956821.
- ↑ Malvar G, Peric M, Gonzalez RS (May 2022). "Interval appendicitis shows histological differences from acute appendicitis and may mimic Crohn disease and other forms of granulomatous appendicitis". Histopathology 80 (6): 965–973. doi:10.1111/his.14621. PMID 35076982.