Difference between revisions of "Salivary glands"
(→Warthin tumour: redirect) |
(→Adenoid cystic carcinoma: split out) |
||
| Line 711: | Line 711: | ||
==Adenoid cystic carcinoma== | ==Adenoid cystic carcinoma== | ||
:See: ''[[Adenoid cystic carcinoma of the breast]]'' for the [[breast]] tumour. | :See: ''[[Adenoid cystic carcinoma of the breast]]'' for the [[breast]] tumour. | ||
{{Main|Adenoid cystic carcinoma}} | |||
==Salivary duct carcinoma== | ==Salivary duct carcinoma== | ||
Revision as of 21:09, 17 July 2013
The salivary glands help digest food. ENT surgeons take 'em out and want you to diagnose 'em. Cytopathology of the salivary glands is covered in the Head and neck cytopathology article.
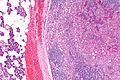
Normal salivary glands
Types of salivary glands
Types of glands:[1]
- Serrous - eosinophilic cytoplasmic granules, acinar arrangement - vaguely resembles the acinar morphology of the pancreas.
- Mucinous - light eosinophilic staining.
Identifying the glands
The three main glands:
- Parotid:
- Serous glands - lower viscosity, acini (lobules).[2]
- Most tumours in this gland are benign.
- Submandibular:
- Serous and mucinous glands.
- Serous ~90% of gland.
- Mucinous ~10% of gland.
- Serous demilunes = mucinous gland with "cap" consisting of a serous glandular component.
- Demilune = crescent.[3]
- Image: Serous demilunes (duke.edu).[4]
- Serous and mucinous glands.
- Sublingual:
- Mucinous glands.
Other:
- Adipose tissue is found between the glands.
- It increases with age.
Images:
Memory devices:
- The parotid gland vaguely resembles the pancreas.
- Submandibular = glands are mixed.
Overview
Benign tumours
Tabular form - adapted from Thompson[5]
| Entity | Architecture | Morphology | Cell borders | Cytoplasm | Nucleus | DDx | Other | Image |
|---|---|---|---|---|---|---|---|---|
| Pleomorphic adenoma | var. | mixed pop.; must include: (1) myoepithelium, (2) epithelium (ductal cells), (3) chondromyxoid stroma | var. | var. | (1) plasmacytoid | adenoid cystic carcinoma | occ. encapsulated, mixed pop. of glandular, myoepithelial and mesenchymal cells |
|
| Warthin tumour | papillary, bilayer |
cuboid (basal), columnar (apical) | clearly seen | eosinophilic, abundant | unremarkable | sebaceous lymphadenoma | AKA papillary cystadenoma lymphomatosum | |
| Basal cell adenoma | var., islands surrounded by hyaline bands, lesion encapsulated |
basaloid | subtle | scant, hyperchromatic |
granular | basal cell adenocarcinoma | - | - |
| Canalicular adenoma | chains of cells | cuboid or columnar | subtle | scant, hyperchromatic |
granular | basal cell adenoma | exclusively oral cavity, 80% in upper lip; IHC: p63- | (webpathology.com), (webpathology.com) |
| Sialoblastoma | var., islands surrounded by loose fibrous stroma |
basaloid | subtle | scant, hyperch. | granular | basal cell adenocarcinoma | - | - |
Malignant tumours
Tabular form - adapted from Thompson[6]
| Entity | Architecture | Morphology | Cell borders | Cytoplasm | Nucleus | DDx | Other | Image |
|---|---|---|---|---|---|---|---|---|
| Mucoepidermoid carcinoma | cystic & solid | epithelioid | distinct | fuffy, clear, abundant |
nuclei sm. | SCC (?) | IHC: p63+ | |
| Adenoid cystic carcinoma (AdCC) | pseudocysts, cribriform, solid, hyaline stroma |
epithelioid | subtle | scant, hyperchromatic |
small +/-"carrot-shaped" |
pleomorphic adenoma, PLGA | Stains: PAS+ (pseudocyst material), CD117+, cyclin D1+ | |
| Acinic cell carcinoma (AcCC) | sheets, acinar (islands) | epithelioid | clear | granular abundant | stippled, +/-occ. nucleoli | adenocarcinoma not otherwise specified, oncocytoma of salivary gland | Stains: PAS +ve, PAS-D +ve; IHC: S-100 -ve, p63 -ve | |
| Salivary duct carcinoma | glandular, cribriform | columnar | subtle/clear | hyperchromatic | columnar | metastatic breast carcinoma | similar to ductal breast carcinoma; male>female |
|
| Polymorphous low-grade adenocarcinoma | variable, often small nests, may be targetoid |
epithelioid | indistinct | eosinophilic | ovoid & small with small nucleoli |
AdCC | minor salivary gland tumour, often in palate, cytologically monotonous; IHC: S100+, CK+, vim.+, GFAP+/-, BCL2+/- |
|
| Epithelial-myoepithelial carcinoma | nests (myoepithelial) with tubules (epithelial) | epithelioid | not distinct | eosinophilic cytoplasm; epithelial: scant; myoepithelial: moderate | focal clearing | AdCC, pleomorphic adenoma | rare | |
| Basal cell adenocarcinoma | var., islands surrounded by hyaline bands, lesion not encapsulated |
basaloid | subtle | scant, hyperchromatic |
granular | basal cell adenoma | rare, usu. parotid gland, may arise from a basal cell adenoma |
DDx
Palate
Benign parotid tumours
Oncocytic tumours
- Benign:
- Oncocytoma.
- Warthin tumour.
- Malignant:
- Mucoepidermoid carcinoma, oncocytic variant.
- Salivary duct carcinoma.
- Carcinoma ex pleomorphic carcinoma with a salivary duct carcinoma component.
- Apocrine carcinoma.
- Oncocytic carcinoma.
- Acinic cell carcinoma, oncocytic variant.
Clear cell tumours
- Mucoepidermoid carcinoma, clear cell variant.
- Acinic cell carcinoma, clear cell variant.
- Hyalinizing clear cell carcinoma.
- Epithelial-myoepithelial carcinoma.
- Metastatic clear cell carcinoma.
- Metastatic clear cell renal cell carcinoma.
IHC overview
General:
- Usually has limited value.
Specifics:
- Luminal markers: CK7, CK19, CAM5.2 (LMWK).
- Basal markers: p63, HMWK, CK14.
- Myoepithelial markers: calponin, actin.
- Uncommitted: S-100.
Notes:
- p63 and S-100 are sometimes call myoepithelial.
Benign
General DDx:
- Inflammation.
- Neoplasm.
- Ductal obstrution.
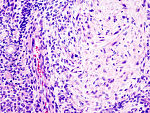
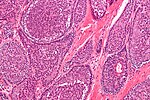
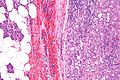
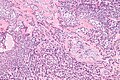
Chronic sialadenitis
General
Etiology:[7]
- Infection.
- Autoimmune (e.g. Sjögren syndrome, systemic lupus erythematosus).
- Other.
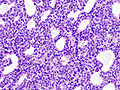
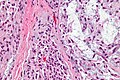
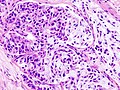
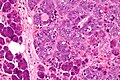
Microscopic
Features:
- +/-Fibrosis.
- Non-neoplastic mononuclear inflammatory infiltrate (lymphocytes, plasma cells).
Note:
- If the infiltrate is predominantly lymphocytes Sjögren's is a possibility, and reporting a Focus score should be considered.
DDx:
- Lymphoma - especially MALT lymphoma.[8]
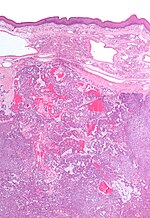
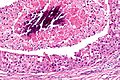
Image
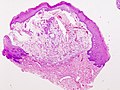
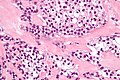
Salivary gland mucocele
General
- Benign.
- Infected mucocele = mucopyocele.
Microscopic
Features:[9]
- Granulation tissue-like and pseudocyst-like.
- Granulation tissue-like:
- Fibroblasts.
- Small caliber blood vessels.
- Histocytes.
- Neutrophils.
- Pseudocyst:
- No epithelial lining.
- Poorly circumscribed.
- Granulation tissue-like:
- Pale pink extracellular material (mucous) - key feature.
- +/-Granulomas.[10]
DDx:
- Granulation tissue.
- Signet ring cell carcinoma - muciphages may mimic signet ring cells.
Images
www:
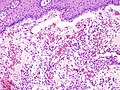
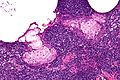
Pleomorphic adenoma
- Abbreviated PA.
General
Features:
- Very common - approx. 60% of parotid gland tumours.[11]
- May transform into a malignant tumour.
- Other benign salivary gland tumours do not do this.
- Only benign childhood salivary gland tumour of significance.
Weinreb's dictums
- Most common salivary tumour in all age groups.
- Seen in all sites (unlike other benign tumours).
- Recurrence and malignancy risk (unlike other benign salivary gland tumours).
- Any part of a tumour that looks like PA makes it a PA.
Gross
- May be cartilaginous appearing.
Image:
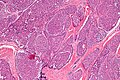
Microscopic
Features:[11]
- Proliferation of myoepithelium and epithelium (ductal cells) in mesenchymal stroma.
- Cells in ducts = epithelial.
- Cells not in ducts = myoepithelial.[12]
- Mesenchymal stroma - important feature.
Notes:
- Mesenchymal stroma not required for diagnosis -- if >5% ducts.[12]
- No chondroid stroma and <5% ductal cells = myoepithelioma.
- Complete excision is often elusive; stating "completely excised" on a surgical pathology report is unwise.
- Look for, i.e. rule-out, poorly differentiated carcinoma: carcinoma ex pleomorphic adenoma.
Memory device: MEC = myoepithelium, epithelium, chondromyxoid stroma.
DDx:
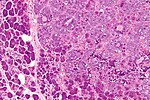
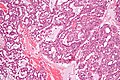
Images
www:
IHC
- S-100 +ve, SMA +ve, GFAP +ve.
Myoepithelioma
General
- Usually benign.
- May be malignant.
Location:[13]
- Parotid gland ~50%.
- Palate ~25%
- Submandibular gland ~12%.
Notes:
- First described in 1972.[14]
Microsopic
Features:[15]
- Myoepithelial cells - may be:
- Spindled.
- Plasmacytoid.
- Epithelioid.
- Clear (rare).
- Lack tubules, i.e. epithelial component.
- May be up to 10% (or 5%[16]).
DDx:
Images
IHC
Features:[15]
- S100 +ve.
- GFAP +ve.
- CK14 +ve.
Others:[17]
- SMA +ve.
- Calponin +ve.
Basal cell adenoma
General
- ~2% of salivary gland tumours.
- May be multifocal.
- Usually parotid gland, occasionally submandibular gland.
- Female:male = ~2:1.
- May be seen in association with dermal cylindromas in the context of a genetic mutation.[18]
- Malignant transformation - rarely.
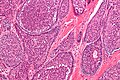
Microscopic
Features:
- Basal component.
- Basophilic cells - key feature.
- Usu. in nests.
- May be bilayered tubules or trabeculae.
- Large basophilic nucleus.
- Minimal-to-moderate eosinophilic cytoplasm.
- Stromal cells.
- Plump spindle cells without significant nuclear atypia - distinguishing feature.
- Stromal cell nuclei width ~= diameter RBC.
- Dense hyaline stroma.
- Plump spindle cells without significant nuclear atypia - distinguishing feature.
- Tubular component.
- Within basal component, may be minimal.
- Lesion is encapsulated - key feature.
Notes:
- No chondromyxoid stroma.
- Chondromyxoid stroma present -> pleomorphic adenoma.
- Neoplastic cells embedded in stroma ("stromal invasion") = basal cell adenocarcinoma.
- Basal cell adenocarcinoma may be cytologically indistinguishable from basal cell adenoma, i.e. "bad" architecture makes it a basal cell adenocarcinoma.
DDx:
- Adenoid cystic carcinoma - not encapsulated.
- Basal cell adenocarcinoma - not encapsulated.
- Canalicular adenoma - different site; canalicular adenoma is the in oral cavity, usually upper lip.
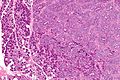
Images:
IHC
- Luminal stains +ve: CK7 +ve, CAM5.2 +ve.
- p63 +ve -- basal component.
- S100 +ve -- spindle cells in the stroma.
Canalicular adenoma
General
- Exclusively oral cavity.
- 80% of lesions on upper lip.
Microscopic
Features:
- Channels - "beading of cell".
- Mucoid/hemorrhagic stroma.
DDx:
- Basal cell adenoma.
Images:
- Canalicular adenoma - low mag. (webpathology.com).
- Canalicular adenoma - high mag. (webpathology.com).
IHC
- p63 -ve.
- Basal cell adenoma p63 +ve.
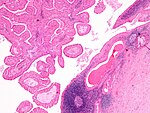
Warthin tumour
Sebaceous adenoma
- Benign counterpart of sebaceous carcinoma.
Sebaceous lymphadenoma
General
- Rare salivary gland tumour.[20]
- Benign.
Microscopic
Features:[20]
- Sebaceous glands within lymphoid tissue - key feature.
DDx:[21]
- Warthin tumour.
- Sebaceous lymphadenocarcinoma.
- Mucoepidermoid carcinoma.
- Lymphoma.
Images
www:
Oncocytoma of the salivary gland
- AKA salivary gland oncocytoma.
General
- No risk of malignant transformation.
- ~1% of all salivary gland tumours.
- Typical age: 60s-80s.
- Associated with radiation exposure.
- Major salivary glands - usually parotid gland.[22]
Gross
- Golden brown appearance.
Image
Microscopic
Features:
- Like oncocytomas elsewhere.
- Eosinophilic cytoplasm (on H&E stain).
- Due to increased number of mitochrondria.
- Fine capillaries.
- Eosinophilic cytoplasm (on H&E stain).
- Architecture: solid sheets, trabeculae or duct-like structure.[22]
Notes:
- May have clear cell change.
- Multiple small incidental lesions = oncocytosis - not oncocytoma.
DDx:
Images
www:
IHC
- p63 +ve[23] focally in nucleus.
Malignant
One approach:
- Differentiate -- luminal vs. myoepithelial vs. basal (mucoepideroid).
Mucoepidermoid carcinoma
- Abbreviated MEC.
General
- Most common malignant neoplasm of salivary gland in all age groups.[24]
- Female:male ~= 3:2.
- Site: parotid > submandibular.
Gross
- Cystic or solid, usu. a mix of both.
Microscopic
Features:
- Architecture:[25]
- Cystic (low grade).
- Solid (high grade).
- Mucous cells with abundant fluffy cytoplasm and large mucin vacuoles - key feature.
- Nucleus distorted by mucin vacuole.
- Mucous cell may be scarce - more difficult to diagnose.
- Epidermoid cells:
Notes:
- The classic description - composed of 3 cell types: epidermoid, intermediate, and mucin producing.[26]
- "Intermediate cells" are described in textbooks. Weinreb thinks they are a pretty much a myth.[12]
- Mucin vacuoles may be rare; in a superficial glance -- it may mimic squamous cell carcinoma.
- The thought of high-grade MEC should prompt consideration of squamous cell carcinoma.
Images
www:
Subtypes
- Conventional.
- Oncocytic.
- Definition: composed of 50% oncocytes.
- Good outcome.[27]
- Clear cell.
- Unicystic (cystadenocarcinoma).
- Based on the gross. (???)
- Sclerosing MEC +/- eosinophilia.
- Rare.
Grading
General:
Notes:
- Both systems have their pros and cons.
- Weinreb uses the AFIP system with a slight modification.
AFIP
- Low cystic content (<20%) - 2 points.
- Perineural invasion - 2 points.
- Necrosis - 3 points.
- Mitoses > 4 per 10 HPFs (HPF not defined in paper - see HPFitis) - 3 points.
- Anaplasia - 4 points.
Scoring:
- Low grade = 0-4 points.
- Intermediate grade = 5-6 points.
- High grade = 7+ points.
Weinreb modification
Weinreb looks for the following:
- Tumour invades in small nests/islands - 2 points.
- If applicable, the two points are added to the AFIP score.
- The tumour is graded using the AFIP (scoring) cut points -- see above.
Notes:
- It seems pointless to memorize this but it is occasionally asked on exams.
- How to remember: think of the Nottingham grading system (architecture, mitoses, nuclear grade) + necrosis + LVI.
Stains
Mucous cells:
- Alcian blue +ve.
- Mucicarcmine +ve.
Molecular
- t(11;19)(q21;p13) -- MECT1-MAML2 fusion.[30][31]
- Present in ~65% of MECs.
- Presence assoc. with low-grade MEC (vs. high-grade MEC) & favourable prognosis.
- Not seen in tumours that are in the DDx of MEC.
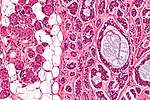
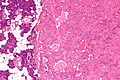
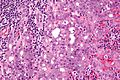
Acinic cell carcinoma
- Not to be confused with pancreatic acinar cell carcinoma.
- Abbreviated AcCC.
- AKA acinic cell adenocarcinoma.
General
- Malignant neoplasm of salivary gland arising from acinic cells.
- The relative prevalence of the neoplasm in the various salivary gland reflects the abundance of acinic cells: parotid gland (~80%) > minor salivary glands (~17%) > submandibular glands (~3%).
- Affects wide age range -- including children.
- Site affect prognosis (most aggressive to least aggressive): submandibular > parotid > minor salivary.
Gross
- Tan or reddish.
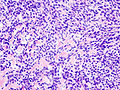
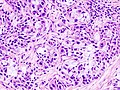
Microscopic
Features:
- Sheets of acinic cells with:
- Abundant finely vacuolated cytoplasm with basophilic granules - key feature.
- Granules may be focal.
- Small nuclei stippled chromatin.
- Abundant finely vacuolated cytoplasm with basophilic granules - key feature.
- Scattered intercalcated duct type cells with:
- Eosinophilic cytoplasm with moderate amount of cytoplasm.
- Bland nuclei with slightly larger than seen in acinic cells.
- +/-Peri-tumoural lymphocytes.
- +/-Glassy extracellular bluish/purple blobs.
Notes:
- Adipose tissue -- present in the salivary glands -- is absent in AcCC.
- May focally resemble thyroid tissue.
- Smaller (characteristic) microvacuoles (unreported in the literature) may be present that have a bubbly appearance and glassy basophilic inclusions.[12]
Memory device:
- AcCC - lots of "C"s - chromatin stipled, cytoplasm generous.
DDx:
- Oncocytoma of the salivary gland.
- Adenocarcinoma not otherwise specified.[32]
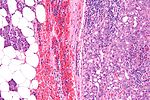
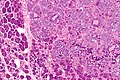
Images
www:
- AcCC (surgicalpathologyatlas.com).
- AcCC (brown.edu).
- AcCC (aciniccell.org) - image collection.
Grading
General:
- Not prognostic.
- Done to avoid phone calls from clinician.
Factors Weinreb uses:[12]
- Necrosis.
- Nuclear atypia.
- Perineural invasion.
- Mitoses.
- Infiltrative margin.
- Tumour sclerosis.
Subtypes
- Oncocytic variant - rare.
- Clear cell variant - rare.
- Papillary cystic variant.
Stains
- PAS +ve.
- PAS-D +ve.
IHC
- S-100 -ve.
- p63 -ve.
- p63 +ve in mucoepidermoid carcinoma.
There are a bunch of other stains that are touted to be useful (amylase, anti-chymotrypsin, lactoferrin). Weinreb thinks these are not helpful.[12]
EM
Adenoid cystic carcinoma
- See: Adenoid cystic carcinoma of the breast for the breast tumour.
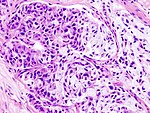
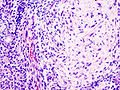
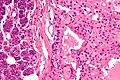
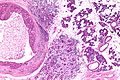
Salivary duct carcinoma
General
- Malignant counterpart of salivary duct adenoma.
- Male:female ~= 4:1.
- Dismal prognosis.[34]
- Typically >50 years old.
- Mostly in the parotid.
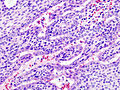
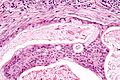
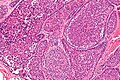
Microscopic
Features - resembles ductal breast carcinoma:[34]
- Architecture: sheets, nests, cords, cribriform, micropapillary.
- Neoplastic cells line-up around cystic spaces "Roman bridges".
- Nuclear atypia (variation in size, shape, staining).
- Apocrine snouts - pseudopod-like/lollipop-like undulations of the cell membrane.
- Decapitation secretions - apocrine snouts (membrane bound blobs of cytoplasm) that have separated from its mother cell.
Notes:
- Similar to ductal breast carcinoma - key to remember.
DDx:
- Carcinoma ex pleomorphic adenoma with SDC component.
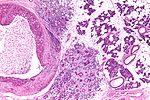
Images
www:
Subtypes
- Conventional.
- Mucinous - worse prognosis; opposite of what would one expect from the outcomes in breast cancer.
- Micropapillary - assoc. with a poor prognosis.
- Sarcomatoid/spindle cell.
IHC
- LMWK, EMA, CK7, CK19 +ve.
- p63 -ve.
- Androgen receptor +ve.
- BRST2 (GCDFP-15) +ve.
- HER2 +ve ~21%; use of trastuzumab (Herceptin) not systematically studied.
Curiosity:
- PSA +/-.
- PSAP +/-.
- ER-beta +ve.[35]
- ER-alpha -ve (the common ER stain).
Polymorphous low-grade adenocarcinoma
- Abbreviated PLGA.
General
- Almost exclusively in the oral cavity.
- Classically found in the palate -- 60% of PLGAs in palate.
- Tumour of the minor salivary glands.
- Always a low-grade tumour - by definition.
- Female:male ~= 2:1.
- Older people ~50-70 years old.
Microscopic
Features:[36]
- Architecture: often small nests, may be targetoid.
- Classically has whorling with eye-of-storm & single file.
- Cytologically monotonous (uniform) with variable architecture - key feature.
- Nucleus: ovoid & small, small nucleoli, powdery chromatin.
- Papillary thyroid carcinoma-like appearance.
- Cytoplasm: eosinophilic.
- Nucleus: ovoid & small, small nucleoli, powdery chromatin.
- Indistinct cell borders.
DDx:
- Adenoid cystic carcinoma.
- Pleomorphic adenoma.
- Cribriform adenocarcinoma of the minor salivary gland.[37]
Images
IHC
- S100 +ve, CK +ve, vimentin +ve.
- GFAP +ve/-ve.
- BCL2 +ve/-ve.
- Generally negative for myoepithelial markers (calponin, actin) - useful if negative.
Carcinoma ex pleomorphic adenoma
- Abbreviated Ca ex PA.
General
Definition:
- Malignant transformation of a pleomorphic adenoma.
Diagnosis (either 1 or 2):
- History of a pleomorphic adenoma at the same site.
- Features of a pleomorphic adenoma and a carcinoma.
Epidemiology:
- Rare.
Microscopic
Features:
- Cells with cytologic features of malignancy.
- Architecture (any of the following):
- Glands.
- Nests.
- Single cells (may be subtle).
Architectural patterns:
- Ductal carcinoma NOS (arising from ductal cells) - most common pattern for Ca ex PA.
- Myoepithelial cacinoma NOS (arising from myoepithelial cells).
- "Named carcinoma":
- Salivary duct carcinoma - second most common pattern for Ca ex PA.
- Mucoepidermoid carcinoma.
- Adenoid cystic carcinoma.
Note:
- Often adenocarcinoma-like.
- Myoepithelial cells may be clear cells. (???)
Subclassification
Extent of invasion:[38]
- Non-invasive AKA intracapsular AKA in situ.
- Minimally invasive <=1.5 mm beyond the capsule.
- Widely invasive >1.5 mm beyond the capsule.
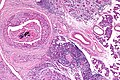
Epithelial-myoepithelial carcinoma
- Abbreviated EMCa.
General
- Rare ~1% of salivary gland tumours.[39]
- Female:male = 1.5:1.[40]
- Usu. older people - 50s or 60s.
- Usu. parotid gland ~ 60% of cases.[40]
- Prognosis: usually good; 5-year and 10-year survival over 90% and 80% respectively.[40]
Notes:
- Most common malignant component in carcinoma ex pleomorphic adenoma.
- May be the same tumour as adenomyoepithelioma of the breast.[41]
Microscopic
Features:
- Biphasic tumour:[40]
- Epithelial layer.
- Myoepithelial layer - key feature.
- Architecture: variable (solid, cystic, tubular, papillary).
- +/-Spindle cells.
- Basement membrane-like material; may mimic adenoid cystic carcinoma.
Notes:
- Usually few mitoses.
DDx:
- Adenoid cystic carcinoma (tubular variant).
- Pleomorphic adenoma, tubular variant.
- Has focal epithelial-myoepithelial carcinoma-like areas.
Images
www:
IHC
- CAM5.2 +ve -- epithelial component.
- p63 +ve -- myoepithelial component.
Basal cell adenocarcinoma
- Abbreviated BCAC.
General
- Very rare.
- Malignant.
- Good prognosis.
- May arise from a basal cell adenoma.[43]
Gross
- Usually in the parotid gland ~90% of cases.[43]
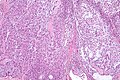
Microscopic
Features:
- Lesion is not encapsulated - key feature.
- Basal-like cells:
- Basophilic cells - key feature.
- Usually in nests.
- May be bilayered tubules or trabeculae.
- Large basophilic nucleus.
- Minimal-to-moderate eosinophilic cytoplasm.
- Stromal cells.
- Plump spindle cells without significant nuclear atypia.
- Stromal cell nuclei width ~= diameter RBC.
- Dense hyaline stroma.
- Plump spindle cells without significant nuclear atypia.
- Tubular component.
- Within basal component, may be minimal.
DDx:
- Adenoid cystic carcinoma.
- Basal cell adenoma - encapsulated.
- Basaloid squamous cell carcinoma.
Images
www:
- Basal cell adenocarcinoma - intermed. mag. (webpathology.com).
- Basal cell adenocarcinoma - high mag. (webpathology.com).
IHC
Features:[44]
- CK7 +ve (strong).
- S100 +ve/-ve.
Sebaceous carcinoma
It is similar to the tumour found in the skin.
Hyalinizing clear cell carcinoma
- Abbreviated HCCC.
General
Microscopic
Features:[47]
- Groups of cells with abundant clear cytoplasm.
- Arranged in cords, trabeculae or clusters.
- Minimal nuclear pleomorphism.[48]
- Hyalinized stroma.
Notes:
- Clear cytoplasm due to glycogen.[48]
- Low mitotic rate.
DDx:
- Mucoepidermoid carcinoma, clear cell variant.
- Acinic cell carcinoma, clear cell variant.
- Metastatic clear cell renal cell carcinoma.
- Classically have hemorrhage & necrosis.
- Epithelial-myoepithelial carcinoma.
Images
www:
Stains/IHC
- PAS +ve.
- AE1/AE3 +ve.
- EMA +ve.[48]
Others:
Molecular
Recurrent translocation:[49]
- t(12;22) -- EWSR1/ATF1.
- Same translocation as in clear cell sarcoma.
See also
References
- ↑ http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Oral/oral.htm#LABSALIVA
- ↑ http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Epithelia/Epithel.htm
- ↑ URL: http://dictionary.reference.com/browse/demilune. Accessed on: 19 August 2011.
- ↑ URL: http://pathology.mc.duke.edu/research/pth225.html. Accessed on: 19 August 2011.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 295-319. ISBN 978-0443069604.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 325-357. ISBN 978-0443069604.
- ↑ URL: http://emedicine.medscape.com/article/882358-overviewhttp://emedicine.medscape.com/article/882358-overview. Accessed on: 10 January 2011.
- ↑ Beasley, MJ. (Apr 2012). "Lymphoma of the Thyroid and Head and Neck.". Clin Oncol (R Coll Radiol). doi:10.1016/j.clon.2012.02.010. PMID 22475637.
- ↑ URL: http://emedicine.medscape.com/article/1076717-workup. Accessed on: 6 March 2012.
- ↑ Seifert, G.; Donath, K.; von Gumberz, C. (Jun 1981). "[Mucoceles of the minor salivary glands. Extravasation mucoceles (mucus granulomas) and retention mucoceles (mucus retention cysts) (author's transl)].". HNO 29 (6): 179-91. PMID 7251405.
- ↑ 11.0 11.1 Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 295. ISBN 978-0443069604.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 IW. 10 January 2011. Cite error: Invalid
<ref>tag; name "IW_10jan2011" defined multiple times with different content Cite error: Invalid<ref>tag; name "IW_10jan2011" defined multiple times with different content Cite error: Invalid<ref>tag; name "IW_10jan2011" defined multiple times with different content - ↑ Barnes, L.; Appel, BN.; Perez, H.; El-Attar, AM. (Jan 1985). "Myoepithelioma of the head and neck: case report and review.". J Surg Oncol 28 (1): 21-8. PMID 2982059.
- ↑ Saksela, E.; Tarkkanen, J.; Wartiovaara, J. (Sep 1972). "Parotid clear-cell adenoma of possible myoepithelial origin.". Cancer 30 (3): 742-8. PMID 5075358.
- ↑ 15.0 15.1 Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 130. ISBN 978-0470519035.
- ↑ I. Weinreb. 24 October 2011.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 18. ISBN 978-0470519035.
- ↑ Choi, HR.; Batsakis, JG.; Callender, DL.; Prieto, VG.; Luna, MA.; El-Naggar, AK. (Jun 2002). "Molecular analysis of chromosome 16q regions in dermal analogue tumors of salivary glands: a genetic link to dermal cylindroma?". Am J Surg Pathol 26 (6): 778-83. PMID 12023583.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/Com/Com304-3-Diss.htm. Accessed on: 25 October 2011.
- ↑ 20.0 20.1 Mishra, A.; Tripathi, K.; Mohanty, L.; Nayak, M.. "Sebaceous lymphadenoma of the parotid gland.". Indian J Pathol Microbiol 54 (1): 131-2. doi:10.4103/0377-4929.77364. PMID 21393895. http://www.ijpmonline.org/article.asp?issn=0377-4929;year=2011;volume=54;issue=1;spage=131;epage=132;aulast=Mishra.
- ↑ While, B.; Whiteside, OJ.; Desai, V.; Gurr, P. (Aug 2010). "Sebaceous lymphadenoma: a case report and review of the literature.". Ear Nose Throat J 89 (8): E22-3. PMID 20737364.
- ↑ 22.0 22.1 Zhou, CX.; Gao, Y. (Dec 2009). "Oncocytoma of the salivary glands: a clinicopathologic and immunohistochemical study.". Oral Oncol 45 (12): e232-8. doi:10.1016/j.oraloncology.2009.08.004. PMID 19796983.
- ↑ 23.0 23.1 McHugh, JB.; Hoschar, AP.; Dvorakova, M.; Parwani, AV.; Barnes, EL.; Seethala, RR. (Dec 2007). "p63 immunohistochemistry differentiates salivary gland oncocytoma and oncocytic carcinoma from metastatic renal cell carcinoma.". Head Neck Pathol 1 (2): 123-31. doi:10.1007/s12105-007-0031-4. PMC 2807526. PMID 20614263. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2807526/.
- ↑ URL: http://path.upmc.edu/cases/case715/dx.html. Accessed on: 2 February 2012.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/D2A001-PQ01-M.htm. Accessed on: 19 October 2010.
- ↑ Lennerz, JK.; Perry, A.; Mills, JC.; Huettner, PC.; Pfeifer, JD. (Jun 2009). "Mucoepidermoid carcinoma of the cervix: another tumor with the t(11;19)-associated CRTC1-MAML2 gene fusion.". Am J Surg Pathol 33 (6): 835-43. doi:10.1097/PAS.0b013e318190cf5b. PMID 19092631.
- ↑ Weinreb I, Seethala RR, Perez-Ordoñez B, Chetty R, Hoschar AP, Hunt JL (March 2009). "Oncocytic mucoepidermoid carcinoma: clinicopathologic description in a series of 12 cases". Am. J. Surg. Pathol. 33 (3): 409–16. doi:10.1097/PAS.0b013e318184b36d. PMID 18971778.
- ↑ Goode RK, Auclair PL, Ellis GL (April 1998). "Mucoepidermoid carcinoma of the major salivary glands: clinical and histopathologic analysis of 234 cases with evaluation of grading criteria". Cancer 82 (7): 1217–24. PMID 9529011.
- ↑ Brandwein MS, Ivanov K, Wallace DI, et al. (July 2001). "Mucoepidermoid carcinoma: a clinicopathologic study of 80 patients with special reference to histological grading". Am. J. Surg. Pathol. 25 (7): 835–45. PMID 11420454.
- ↑ Tonon G, Modi S, Wu L, et al. (February 2003). "t(11;19)(q21;p13) translocation in mucoepidermoid carcinoma creates a novel fusion product that disrupts a Notch signaling pathway". Nat. Genet. 33 (2): 208–13. doi:10.1038/ng1083. PMID 12539049.
- ↑ Seethala RR, Dacic S, Cieply K, Kelly LM, Nikiforova MN (August 2010). "A reappraisal of the MECT1/MAML2 translocation in salivary mucoepidermoid carcinomas". Am. J. Surg. Pathol. 34 (8): 1106–21. doi:10.1097/PAS.0b013e3181de3021. PMID 20588178.
- ↑ Ihrler, S.; Blasenbreu-Vogt, S.; Sendelhofert, A.; Lang, S.; Zietz, C.; Löhrs, U. (2002). "Differential diagnosis of salivary acinic cell carcinoma and adenocarcinoma (NOS). A comparison of (immuno-)histochemical markers.". Pathol Res Pract 198 (12): 777-83. PMID 12608654.
- ↑ Sun, Y.; Wasserman, PG. (Feb 2004). "Acinar cell carcinoma arising in the stomach: a case report with literature review.". Hum Pathol 35 (2): 263-5. PMID 14991547.
- ↑ 34.0 34.1 Rajesh, NG.; Prayaga, AK.; Sundaram, C.. "Salivary duct carcinoma: correlation of morphologic features by fine needle aspiration cytology and histopathology.". Indian J Pathol Microbiol 54 (1): 37-41. doi:10.4103/0377-4929.77321. PMID 21393874. http://www.ijpmonline.org/text.asp?2011/54/1/37/77321.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/MajorSalGlands_11protocol.pdf. Accessed on: 3 April 2012.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 74. ISBN 978-0781765275.
- ↑ Skalova, A.; Sima, R.; Kaspirkova-Nemcova, J.; Simpson, RH.; Elmberger, G.; Leivo, I.; Di Palma, S.; Jirasek, T. et al. (Aug 2011). "Cribriform adenocarcinoma of minor salivary gland origin principally affecting the tongue: characterization of new entity.". Am J Surg Pathol 35 (8): 1168-76. doi:10.1097/PAS.0b013e31821e1f54. PMID 21716087.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/MajorSalGlands_11protocol.pdf. Accessed on: 2 April 2012.
- ↑ Tralongo, V.; Daniele, E.. "Epithelial-myoepithelial carcinoma of the salivary glands: a review of literature.". Anticancer Res 18 (1B): 603-8. PMID 9568184.
- ↑ 40.0 40.1 40.2 40.3 Seethala, RR.; Barnes, EL.; Hunt, JL. (Jan 2007). "Epithelial-myoepithelial carcinoma: a review of the clinicopathologic spectrum and immunophenotypic characteristics in 61 tumors of the salivary glands and upper aerodigestive tract.". Am J Surg Pathol 31 (1): 44-57. doi:10.1097/01.pas.0000213314.74423.d8. PMID 17197918.
- ↑ Seifert, G. (Sep 1998). "Are adenomyoepithelioma of the breast and epithelial-myoepithelial carcinoma of the salivary glands identical tumours?". Virchows Arch 433 (3): 285-8. PMID 9769134.
- ↑ [http://www.pathologyimagesinc.com/sgt-cytopath/epith-myoepith-ca/cytopathology/fs-emc-cytopath-feat.html "Cytopathologic Features of Epithelial-myoepithelial Carcinoma"]. http://www.pathologyimagesinc.com/sgt-cytopath/epith-myoepith-ca/cytopathology/fs-emc-cytopath-feat.html. Retrieved January 18, 2011.
- ↑ 43.0 43.1 Muller, S.; Barnes, L. (Dec 1996). "Basal cell adenocarcinoma of the salivary glands. Report of seven cases and review of the literature.". Cancer 78 (12): 2471-7. PMID 8952553.
- ↑ Farrell, T.; Chang, YL. (Oct 2007). "Basal cell adenocarcinoma of minor salivary glands.". Arch Pathol Lab Med 131 (10): 1602-4. doi:10.1043/1543-2165(2007)131[1602:BCAOMS]2.0.CO;2. PMID 17922602.
- ↑ Masilamani, S.; Rao, S.; Chirakkal, P.; Kumar, AR.. "Hyalinizing clear cell carcinoma of the base of tongue: a distinct and rare entity.". Indian J Pathol Microbiol 54 (1): 167-9. doi:10.4103/0377-4929.77393. PMID 21393908.
- ↑ Kauzman, A.; Tabet, JC.; Stiharu, TI. (Jul 2011). "Hyalinizing clear cell carcinoma: a case report and review of the literature.". Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112 (1): e26-34. doi:10.1016/j.tripleo.2011.02.041. PMID 21669357.
- ↑ 47.0 47.1 O'Sullivan-Mejia, ED.; Massey, HD.; Faquin, WC.; Powers, CN. (Sep 2009). "Hyalinizing clear cell carcinoma: report of eight cases and a review of literature.". Head Neck Pathol 3 (3): 179-85. doi:10.1007/s12105-009-0124-3. PMID 20596970.
- ↑ 48.0 48.1 48.2 48.3 48.4 Milchgrub, S.; Gnepp, DR.; Vuitch, F.; Delgado, R.; Albores-Saavedra, J. (Jan 1994). "Hyalinizing clear cell carcinoma of salivary gland.". Am J Surg Pathol 18 (1): 74-82. PMID 7506496.
- ↑ Antonescu, CR.; Katabi, N.; Zhang, L.; Sung, YS.; Seethala, RR.; Jordan, RC.; Perez-Ordoñez, B.; Have, C. et al. (Jul 2011). "EWSR1-ATF1 fusion is a novel and consistent finding in hyalinizing clear-cell carcinoma of salivary gland.". Genes Chromosomes Cancer 50 (7): 559-70. doi:10.1002/gcc.20881. PMID 21484932.