Heart
The heart is an important organ. It moves the blood around. For orthopods, it gets the Ancef (cefazolin) to the bones. When it stops for an extended time... people end-up in the morgue or being seen by a pathologist for an autopsy.
An introduction to cardiovascular pathology is found in the cardiovascular pathology article.
Obscure anatomy
Heart dissection
Pericardium
If adhesions are present decide whether they are:
- Fibrinous (recent) or,
- Fibrous (old).
Identifying hardware
- Defibrillator - thick wires.
- Pacer - thin wires.
General rule
- Open along the lines of flow.
Note:
- Do not open right atrium (RA) SVC to IVC.
- Why? A.: You cut through the territory of the SA node.
Coronary arteries
- These are often done first, i.e. before the heart is opened.
- They should be sectioned (axially) at ~2 mm intervals.
- Longitudinally opening the coronaries does not allow accurate assessment of luminal stenosis.[1]
- A significant stenosis (defined by diameter narrowing) is 70-75%.[2]
Notes:
- If calcified:
- Dissect off the coronary tree + decal.
Right atrium
- Open anteriorly ~ 1 cm above the tricuspid valve annulus.
- Open right auricle at the same time.
Examination of apex
- Slice apex (perpendicular to the long axis of the heart), such that both ventricles can be seen.
Right ventricle
- Make cut through the apex (transverse/biventicular section).
- Open along lateral edge (from RA cut).
Right ventricular outflow tract
- Cut along pulmonary artery.
Left atrium
- Isolate the four pulmonary veins - cut 'em so they are long on the heart.
- Join the pulmonary veins on the right with a cut.
- Join the pulmonary veins on the left with a cut.
- Open the posterior aspect of the LA by joining the two previous cuts.
- Open the left auricle (to look for thrombus).
Left ventricle
- Open on the lateral aspect with a long knife.
Left ventricular outflow tract
- Open LVOT with cut(s) from LV; stay close to intraventricular septum.[3]
- Avoid cutting the pulmonary artery.
- With luck you end-up between the left coronary cusp and right coronary cusp.
- Check whether the aortic valve and coronary ostia are normal.
Slicing
- After the heart is opened it should be sliced at 5-10 mm intervals to the semilunar valves.
Standard measures of the heart
- Mass (weight).
- Left ventricle (LV) - 2 cm below the MV.
- Right ventricle (RV) - 2 cm below the TV.
- Aortic valve (AV) circumference.
- Mitral valve (MV) circumference.
- Pulmonic valve (PV) circumference.
- Tricuspid valve (TV) circumference.
Normal measures
Younger adults (20-60 years)
Based on Ludwig:[4]
| Measure | Men | Women |
|---|---|---|
| Aortic valve | 6.7 (6.0-7.4) | 6.3 (5.7-6.9) |
| Pulmonary valve | 6.6 (6.1-7.1) | 6.2 (5.7-6.7) |
| Mitral valve | 9.6 (9.4-9.9) | 8.6 (8.2-9.1) |
| Tricuspid valve | 11.4 (11.2-11.7) | 10.6 (10.2-10.9) |
Based on Ludwig:[4]
| Feature | Measure |
|---|---|
| Left ventricle | 1.25 (1.00-1.50) |
| Right ventricle | 0.4 (0.25-0.50) |
Older adults (>60 years)
Based on Ludwig:[4]
| Measure | Men | Women |
|---|---|---|
| Aortic valve | 8.3 (8.1-8.5) | 7.6 (7.3-7.9) |
| Pulmonary valve | 7.3 (7.2-7.5) | 7.1 (6.8-7.4) |
| Mitral valve | 9.5 (9.2-9.8) | 8.6 (8.2-9.0) |
| Tricuspid valve | 11.6 (11.4-11.8) | 10.5 (10.0-11.1) |
Based on Ludwig:[4]
| Feature | Measure |
|---|---|
| Left ventricle | 1.15 (1.05-1.25) |
| Right ventricle | 0.38 (0.35-0.40) |
Standard sections
Minimalist approach (Dr. C.):
- LV and PPM (left ventricle and posterior papillary muscle).
- LV and APM (left ventricle and anterior papillary muscle).
Compromise approach:
- LV and PPM.
- LV and APM.
- LV lateral wall.
- Intraventricular septum.
- RV.
Make the lab work hard approach (Dr. B.):
- PRV (post. RV) with tricuspid valve.
- ARV (ant. RV) with pulm. valve.
- PLV (post. LV) with mitral valve.
- ALV (ant. LV) with aortic valve.
- Lat. LV.
- LV and PPM.
- Post. septum.
- Mid. septum.
- Ant. septum.
- Ant. LV wall.
- LV and APM.
- RCA.
- LAD.
- LCx.
Stock
- One slice (close to apex).
- +/-Region of SA node.
- +/-Region of AV node.
Conducting system
Indications for examining the conducting system[5]
- History of syncope.
- History of arrhythmia.
- Negative autopsy.
Sinoatrial node
- Sinoatrial (SA) node is at the lateral aspect of sulcus terminalis; lateral aspect of the superior vena cava and right atrium junction.[6]
- Cannot be identified grossly.
- Artery of the SA (branch of RCA) may be a clue to where it lies.
Submitting the SA Node:[6]
- Submit all of lateral sulcus terminalis -- serially section perpendicular to the sulcus terminalis, i.e. cuts are in the axis of the SVC (superior to inferior).
Notes: Gulino[7] has a good description and good pictures.
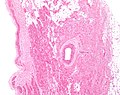
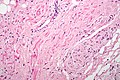
SA node histology
The SA node is best identified by it location:
- The SA Node is superficial to cardiac muscle, i.e. distant to the RA relative to the cardiac muscle.
- The SA nodal tissue abuts cardiac muscle.
- It sits around the sinoatrial node artery - which should be seen on its lumen if the sections were taken properly.
- The SA node is deep to adipose tissue that covers that epicardial aspect of the heart.
- Nerve fibres (from the vagus nerve) are typically found between that adipose tissue and SA nodal tissue.
Histologic characteristics:
- Spindle cell morphology + wavy nucleus.
- Cytoplasm stains lighter with eosin than cardiac muscle.
- +/-Vacuoles.
Images
Atrioventricular node
Approach 1 (Peter method):
- Open the LVOT - if it hasn't been opened yet.
- Cut a section of that includes the right coronary cusp (of the aortic valve) and about 1.5 cm below it (this has the membranous septum and the superior muscular septum).[8]
- This section should then be serially sectioned in the axis of the VLOT.
Approach 2 (Virmani method):
- View from right atrium: AV node is between the coronary sinus and membranous septum.
- View from LVOT: Inferior to the posterior (non-coronary) cusp of the aortic valve.
- One should cut a (coronal) section of that includes the posterior (non-coronary) cusp and about 1.5 cm below it (this has the membranous septum and the superior muscular septum) -- see: Figure 1-15 in Virmani et al.[9]
- This section should then be serially sectioned in the axis of the VLOT.
- One should cut a (coronal) section of that includes the posterior (non-coronary) cusp and about 1.5 cm below it (this has the membranous septum and the superior muscular septum) -- see: Figure 1-15 in Virmani et al.[9]
Approach 3 (Location by triangle of Koch):
- Atrioventicular (AV) node is in the triangle of Koch.
Triangle of Koch according to Virmani[10] is the floor of the RA and:
- Tendon of Todaro = "superior".
- Tricuspid valve annulus = "inferior".
- Coronary sinus = "posterior".
Images:
- Triangle of Koch (ctsnet.org).
- Triangle of Koch (ctsnet.org).
- Triangle of Koch (ipej.org) from a paper by Macedo et al.[11]
Tamponade
- Tamponade is a clinical diagnosis (classically: elevated JVP, low BP). It cannot be made at autopsy.
The pathologist (like radiologists) can say...
- Pericardial effusion.
- Hemopericardium.
Image: Pericardial effusion - CT scan (wikipedia.org).
Fibrinous pericarditis
- AKA bread and butter pericarditis.
- Post-myocardial infarction this is known as Dressler's syndrome.[12]
General
Etiology:
- Radiation.[13]
- Uremia.
- Myocardial infarction (MI).
- Classically occurs at 2-3 days following a MI.[12]
Note:
- Roberts suggests that pericardial heart disease may be a better term for this, as this isn't really an inflammatory process.[14]
Gross
- Pericardium with a shaggy rough appearance.
- Described as "buttered bread dropped-on-the-floor look".[15]
Image:
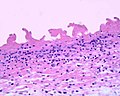
Microscopic
Features:
- Fibrin - pink amorphous material.
Note:
- Inflammation is not a strict requirement for the diagnosis.[14]
Images:
Sign out
Pericardium, Excision: - Fibrinous pericardial heart disease.
Myocardial infarction
- Abbreviated MI.
- AKA myocardial infarct.
Coronary artery atherosclerosis
- AKA coronary artery disease, abbreviated CAD.
- AKA atherosclerotic heart disease, abbreviated ASHD.
- AKA atherosclerotic coronary artery disease.
General
- Greater than 75% (diameter) stenosis - considered significant.[17]
- Leading cause of morbidity and mortality, esp. in the elderly.
- Left main coronary artery (LMCA) disease is particularly fatal.[18]
Clinical presentations:
- Stable angina.
- Unstable angina.
- Myocardial infarction.
- Sudden cardiac death.
Note:
- Coronary artery atherosclerosis is not the only type of coronary artery disease... but it is by far the most common; thus, CAD is generally considered synonymous with coronary artery atherosclerosis.
Treatment:
- Medical management (blood pressure control (antihypertensives), cholesterol control (e.g. statins, exercise), diabetes control, smoking cessation).
- Coronary artery bypass surgery (CABG).
- Percutaneous coronary intervention (PCI).
Stenosis definition
Definition (as per NASCET):[19]
With a bit of algebra one can show:
Where:
- x = 1 - (percent diameter reduction/100).
- Ao = the initial area.
- Ax = the area with diameter x.
If one applies the above equation:
- A 50% diameter reduction results in a 75% area reduction.
- A 75% diameter reduction results in a 93.75% area reduction.
- A 90% diameter reduction results in a 99% area reduction.
Microscopic
- See Atherosclerosis.
Abnormal hearts
Cardiac hypertrophy
Can be by:
- Mass criteria described in a couple of articles from the Mayo Clinic Proceedings.[20][21]
- Thickness criteria.
Rules of thumb:[22]
- >400 g is often abnormal.
- >500 g is abnormal.
- >1.5 cm left ventricle thickness.
- >0.5 cm right ventricle thickness.
Common patterns
Dilated hearts
Dilated pattern DDx:[23]
- Hypertensive heart disease.
- Hypertrophic cardiomyopathy.
- Amyloidosis.
Concentric left ventricular hypertrophy
Concentric left ventricular hypertrophy is a common gross pathologic finding.
The main DDx is:
Other considerations:
- Hypertrophic cardiomyopathy (usually eccentric).
Eccentric left ventricular hypertrophy
- Hypertrophic cardiomyopathy, includes hypertrophic obstructive cardiomyopathy (HOCM).
Detail articles
Cardiomyopathy
In the land of cardiology... there is a thing called cardiomyopathy. This article deals with it.
It includes discussion of dilated cardiomyopathy, hypertrophic cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy.
Congenital heart disease
Congenital heart disease... a domain of pediatric cardiac surgery and occasionally adult cardiac surgery.
The article covers shunts, both left-to-right and right-to-left.
Tumours
These are rare buggers.
Valvular disease
This is the domain of cardiac surgery... only seen in hospitals with cardiac surgery.
Endocarditis
Cardiac sarcoidosis
General
- Can be in isolation or part of systemic sarcoidosis.[24]
- May mimic hypertrophic cardiomyopathy clinically.[25]
- Clinical: associated with heart block.[24]
Gross
- Ventricular septum base - most common site of involvement.[24]
Distribution by autopsy findings:[26]
- Septum - 31.5%.
- Posterior LV - 24.6%.
- Anterior LV - 18.0%.
- RV - 17.9%.
- RV involvement may lead to confusion with arrhythmogenic right ventricular cardiomyopathy (ARVC).
- Lateral LV - 14.1%.
Notes:
- Advanced lesions are fibrotic and may mimic old infarcts (grossly) due to coronary artery atherosclerosis.
Microscopic
Features:[26]
- Non-caseating granulomas.
- Subepicardial predominance.
- +/-Fibrosis - old lesions are fibrotic.
Negatives:
- Significant number of eosinophils.
- Myocyte necrosis.
Notes:
- Myocyte necrosis and eosinophils are features of granulomatous myocarditis.[26]
Myocarditis
Idiopathic granulomatous myocarditis
General
- Unknown etiology.[28]
Microscopic
Features:[26]
- Granulomas.
- Myocyte necrosis.
- Eosinophils.
Note:
- Eosinophils and myocyte necrosis differentiate this entity from cardiac sarcoidosis.
- Granulomas in sarcoidosis are well formed and also involve the fat.[28]
DDx:
- Infectious granulomatous myocarditis, e.g. tuberculosis.
- Rheumatic myocarditis.
- Lymphocytic myocarditis.
Images:
Stains
- Ziehl-Neelsen stain -ve.
- GMS stain -ve.
Chagas disease
- AKA American trypanosomiasis.
Cardiac amyloidosis
General
- Amyloid in the heart.
- Common in the elderly - see senile systemic amyloidosis.
Microscopic
Features (H&E stain):
- Acellular fluffy pink material.
Special stains:
Images (amyloidosis cardiac):
Images (amyloidosis - non-cardiac):
Notes:
- ABCs of pink on H&E = amyloid, blood (fibrin), collagen, smooth muscle.
Mesothelial/monocytic incidental cardiac excrescence
- AKA Cardiac MICE.
General
- Very rare.
- Benign.
- May be confused with a tumour.[31]
Microscopic
Features:[31]
- Mesothelial cells.
Cocaine toxicity
No distinctive pathologic findings. May appear older than one would expect, e.g. advanced atherosclerosis in a young man.
Heart transplant pathology
Comes in different flavours... cellular, acute vascular chronic.
See also
References
- ↑ URL: http://www.histopathology-india.net/CAEx.htm. Accessed on: 7 July 2011.
- ↑ Burton, Julian L.; Rutty, Guy N. (2010). The Hospital Autopsy A Manual of Fundamental Autopsy Practice (3rd ed.). Oxford University Press. pp. 147. ISBN 978-0340965146.
- ↑ {{Ref HospAuto|
- ↑ 4.0 4.1 4.2 4.3 Ludwig, Jurgen (2002). Handbook of Autopsy Practice (3rd ed.). Humana Press. pp. 569. ISBN 978-1588291691.
- ↑ KC. 1 October 2010.
- ↑ 6.0 6.1 Virmani et al. Cardiovascular Pathology. 2nd Ed. 2001. P.16.
- ↑ Gulino SP (September 2003). "Examination of the cardiac conduction system: forensic application in cases of sudden cardiac death". Am J Forensic Med Pathol 24 (3): 227–38. doi:10.1097/01.paf.0000083453.43318.74. PMID 12960658.
- ↑ PF. August 21, 2009.
- ↑ Virmani et al. Cardiovascular Pathology. 2nd Ed. 2001. P.18.
- ↑ Virmani et al. Cardiovascular Pathology. 2nd Ed. 2001. P.17.
- ↑ Macedo, PG.; Patel, SM.; Bisco, SE.; Asirvatham, SJ. (2010). "Septal accessory pathway: anatomy, causes for difficulty, and an approach to ablation.". Indian Pacing Electrophysiol J 10 (7): 292-309. PMID 20680108.
- ↑ 12.0 12.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 293. ISBN 978-1416054542.
- ↑ Schneider, JS.; Edwards, JE. (May 1979). "Irradiation-induced pericarditis.". Chest 75 (5): 560-4. PMID 436483.
- ↑ 14.0 14.1 Roberts, WC. (Jan 2005). "Pericardial heart disease: its morphologic features and its causes.". Proc (Bayl Univ Med Cent) 18 (1): 38-55. PMID 16200146.
- ↑ Cohen, MB.; Laennec, RT. (Feb 2004). "Cross your heart: Some historical comments about fibrinous pericarditis.". Hum Pathol 35 (2): 147-9. PMID 14991530.
- ↑ URL: http://autopsy.stanford.edu/fellowships.html. Accessed on: 21 January 2012.
- ↑ Chamberlain, D. March 7, 2008.
- ↑ Kanjwal, MY.; Carlson, DE.; Schwartz, JS. (Nov 1999). "Chronic/subacute total occlusion of the left main coronary artery--a case report and review of literature.". Angiology 50 (11): 937-45. PMID 10580359.
- ↑ Barnett HJ, Taylor DW, Eliasziw M, et al. (November 1998). "Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators". The New England Journal of Medicine 339 (20): 1415–25. PMID 9811916. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=9811916&promo=ONFLNS19.
- ↑ Scholz DG, Kitzman DW, Hagen PT, Ilstrup DM, Edwards WD (February 1988). "Age-related changes in normal human hearts during the first 10 decades of life. Part I (Growth): A quantitative anatomic study of 200 specimens from subjects from birth to 19 years old". Mayo Clin. Proc. 63 (2): 126–36. PMID 3276973.
- ↑ Kitzman DW, Scholz DG, Hagen PT, Ilstrup DM, Edwards WD (February 1988). "Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): A quantitative anatomic study of 765 specimens from subjects 20 to 99 years old". Mayo Clin. Proc. 63 (2): 137–46. PMID 3276974.
- ↑ KC. 14 October 2010.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 602. ISBN 0-7216-0187-1.
- ↑ 24.0 24.1 24.2 Veinot JP, Johnston B (May 1998). "Cardiac sarcoidosis--an occult cause of sudden death: a case report and literature review". J. Forensic Sci. 43 (3): 715–7. PMID 9608713.
- ↑ Matsumori A, Hara M, Nagai S, et al. (September 2000). "Hypertrophic cardiomyopathy as a manifestation of cardiac sarcoidosis". Jpn. Circ. J. 64 (9): 679–83. PMID 10981852.
- ↑ 26.0 26.1 26.2 26.3 Tavora F, Cresswell N, Li L, Ripple M, Solomon C, Burke A (August 2009). "Comparison of necropsy findings in patients with sarcoidosis dying suddenly from cardiac sarcoidosis versus dying suddenly from other causes". Am. J. Cardiol. 104 (4): 571–7. doi:10.1016/j.amjcard.2009.03.068. PMID 19660614.
- ↑ http://emedicine.medscape.com/article/1612533-overview
- ↑ 28.0 28.1 URL: http://path.upmc.edu/cases/case175/dx.html. Accessed on: 8 January 2012.
- ↑ Ebert EC, Nagar M (March 2008). "Gastrointestinal manifestations of amyloidosis". Am. J. Gastroenterol. 103 (3): 776-87. doi:10.1111/j.1572-0241.2007.01669.x. PMID 18076735.
- ↑ Nishi S, Alchi B, Imai N, Gejyo F (April 2008). "New advances in renal amyloidosis". Clin. Exp. Nephrol. 12 (2): 93-101. doi:10.1007/s10157-007-0008-3. PMID 18175051.
- ↑ 31.0 31.1 de Gouveia, RH.; Ramos, S.; Ribeiro, MA.; Ferreira, M.; Martins, AP. (Apr 2003). "Cardiac MICE--tumor or thrombus?". Rev Port Cardiol 22 (4): 523-9. PMID 12879644.