Difference between revisions of "Stains"
Jensflorian (talk | contribs) (→Kluver-Barrera stain: add picture for Klüver-Barrera) |
|||
| (32 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
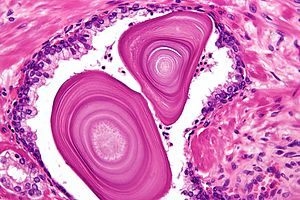
[[Image:Corpora amylacea high mag.jpg|thumb|300px|Hematoxylin and eosin stain of benign [[prostate gland]].]] | [[Image:Corpora amylacea high mag.jpg|thumb|300px|[[Hematoxylin and eosin stain]] of benign [[prostate gland]].]] | ||
This article deals with '''stains'''. H&E | This article deals with '''stains'''. The H&E stain is only one of many stains that are used in pathology. | ||
Non-H&E stains are often referred to as '''''special stains'''''. | Non-H&E stains are often referred to as '''''special stains'''''. | ||
=Where to start...= | =Where to start...= | ||
| Line 54: | Line 54: | ||
==Haematoxylin and eosin stain== | ==Haematoxylin and eosin stain== | ||
*Abbreviated ''H&E''. | *Abbreviated ''H&E''. | ||
{{Main|Hematoxylin and eosin stain}} | |||
==Haematoxylin phyloxin saffron stain== | ==Haematoxylin phyloxin saffron stain== | ||
| Line 167: | Line 156: | ||
There are several AFB stains: | There are several AFB stains: | ||
*Ziehl-Neelson stain - used to look for ''[[Mycobacterium tuberculosis]]''. | *Ziehl-Neelson stain - used to look for ''[[Mycobacterium tuberculosis]]''. | ||
*Fite stain - used to look for ''[[Mycobacterium leprae]]'' | *Fite stain - used to look for ''[[Mycobacterium leprae]]''<ref>URL: [http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/FITES.PDF http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/FITES.PDF]. Accessed on: 19 May 2011.</ref> and preferred stain for ''[[Mycobacterium avium complex]]''.<ref name=pmid21327589>{{cite journal |authors=Ilyas S, Youssef D, Chaudhary H, Al-Abbadi MA |title=Myocbacterium-avium intracellulare associated inflammatory pseudotumor of the anterior nasal cavity |journal=Head Neck Pathol |volume=5 |issue=3 |pages=296–301 |date=September 2011 |pmid=21327589 |pmc=3173547 |doi=10.1007/s12105-011-0248-0 |url=}}</ref> | ||
*Auramine-rhodamine stain. | *Auramine-rhodamine stain. | ||
| Line 285: | Line 274: | ||
<gallery> | <gallery> | ||
Image:Globus_pallidus_and_putamen_-_very_low_mag.jpg | Globus pallidus and putamen - H&E-LFB. (WC) | Image:Globus_pallidus_and_putamen_-_very_low_mag.jpg | Globus pallidus and putamen - H&E-LFB. (WC) | ||
File:LFB_CNS_cortex_supratentorial.jpg | Normal cortex - LFB only. (WC/jensflorian) | |||
File:LFB_CNS_cortex_grey-white_matter_junction.jpg | White-grey matter junction - LFB. (WC/jensflorian) | |||
</gallery> | </gallery> | ||
==Giemsa stain== | ==Giemsa stain== | ||
===Use=== | ===Use=== | ||
| Line 293: | Line 285: | ||
===Interpretation=== | ===Interpretation=== | ||
*Tissue is light blue/green. | *Tissue is light blue/green. | ||
*Goblet cells are purple.<ref>URL: [http://www.kennedy.ox.ac.uk/facilities/histology/histology-information http://www.kennedy.ox.ac.uk/facilities/histology/histology-information]. Accessed on: 17 August 2015.</ref> | |||
Image: | |||
*[http://path.upmc.edu/cases/case196/images/figure12.jpg Giemsa - colon (amser.org)].<ref>URL: [http://amser.org/index.php?P=AMSER--ResourceFrame&resourceId=6018 http://amser.org/index.php?P=AMSER--ResourceFrame&resourceId=6018]. Accessed on: 17 August 2015.</ref> | |||
==Reticulin stain== | ==Reticulin stain== | ||
| Line 378: | Line 374: | ||
===Use=== | ===Use=== | ||
*Stains adipose tissue. | *Stains adipose tissue. | ||
*Corroborate diagnosis of [[lipoid pneumonia]].<ref name=pmid25374742>{{Cite journal | last1 = Yampara Guarachi | first1 = GI. | last2 = Barbosa Moreira | first2 = V. | last3 = Santos Ferreira | first3 = A. | last4 = Sias | first4 = SM. | last5 = Rodrigues | first5 = CC. | last6 = Teixeira | first6 = GH. | title = Lipoid pneumonia in a gas station attendant. | journal = Case Rep Pulmonol | volume = 2014 | issue = | pages = 358761 | month = | year = 2014 | doi = 10.1155/2014/358761 | PMID = 25374742 }}</ref> | |||
*Screen for [[GERD]] - positive staining seen in macrophages from [[BAL]] specimens.<ref name=pmid20466562>{{Cite journal | last1 = Hopkins | first1 = PM. | last2 = Kermeen | first2 = F. | last3 = Duhig | first3 = E. | last4 = Fletcher | first4 = L. | last5 = Gradwell | first5 = J. | last6 = Whitfield | first6 = L. | last7 = Godinez | first7 = C. | last8 = Musk | first8 = M. | last9 = Chambers | first9 = D. | title = Oil red O stain of alveolar macrophages is an effective screening test for gastroesophageal reflux disease in lung transplant recipients. | journal = J Heart Lung Transplant | volume = 29 | issue = 8 | pages = 859-64 | month = Aug | year = 2010 | doi = 10.1016/j.healun.2010.03.015 | PMID = 20466562 }}</ref> | |||
*Uncommon. | *Uncommon. | ||
| Line 542: | Line 540: | ||
*Red = muscle (smooth muscle actin). | *Red = muscle (smooth muscle actin). | ||
*Baby blue = collagen. | *Baby blue = collagen. | ||
*Blue gray = [[amyloid]].<ref name=pmid33002919>{{cite journal |authors=Kunnath-Velayudhan S, Larsen BT, Coley SM, De Michele S, Santoriello D, Colby TV, Bhagat G, Saqi A |title=Masson Trichrome and Sulfated Alcian Blue Stains Distinguish Light Chain Deposition Disease From Amyloidosis in the Lung |journal=Am J Surg Pathol |volume=45 |issue=3 |pages=405–413 |date=March 2021 |pmid=33002919 |doi=10.1097/PAS.0000000000001593 |url=}}</ref> | |||
Notes: <Ref>ULR: [http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/MASSONS.PDF http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/MASSONS.PDF]. Accessed on: 2 November 2011.</ref> | Notes: <Ref>ULR: [http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/MASSONS.PDF http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/MASSONS.PDF]. Accessed on: 2 November 2011.</ref> | ||
| Line 607: | Line 606: | ||
==Hale's colloidal iron stain== | ==Hale's colloidal iron stain== | ||
{{Main|Hale's colloidal iron stain}} | |||
== | ==von Kossa stain== | ||
===General=== | |||
*Type of silver stain.<ref name=pmid8360080>{{Cite journal | last1 = Rungby | first1 = J. | last2 = Kassem | first2 = M. | last3 = Eriksen | first3 = EF. | last4 = Danscher | first4 = G. | title = The von Kossa reaction for calcium deposits: silver lactate staining increases sensitivity and reduces background. | journal = Histochem J | volume = 25 | issue = 6 | pages = 446-51 | month = Jun | year = 1993 | doi = | PMID = 8360080 }}</ref> | |||
* | |||
===Use=== | ===Use=== | ||
*Look for calcium. | *Look for calcium. | ||
*Actually stains phosphates and carbonates as a surrogate for calcium. | |||
===Interpretation=== | ===Interpretation=== | ||
| Line 670: | Line 660: | ||
*[[Cytopathology]]. | *[[Cytopathology]]. | ||
*[[Helicobacter gastritis]] - organisms are dark blue against a light blue background.<ref>URL: [http://www.ihcworld.com/_protocols/special_stains/diff_quick_ellis.htm http://www.ihcworld.com/_protocols/special_stains/diff_quick_ellis.htm]. Accessed on: 30 August 2012.</ref> | *[[Helicobacter gastritis]] - organisms are dark blue against a light blue background.<ref>URL: [http://www.ihcworld.com/_protocols/special_stains/diff_quick_ellis.htm http://www.ihcworld.com/_protocols/special_stains/diff_quick_ellis.htm]. Accessed on: 30 August 2012.</ref> | ||
====Images==== | |||
<gallery> | |||
Image: Lung adenocarcinoma - Diff-Quik -- high mag.jpg | [[Pulmonary_cytopathology#Adenocarcinoma|Lung adenocarcinoma]] - DQ - high mag. (WC) | |||
Image: Lung adenocarcinoma - Diff-Quik -- very high mag.jpg | Lung adenocarcinoma - DQ - very high mag. (WC) | |||
Image: Lung small cell carcinoma - Diff-Quik -- very high mag.jpg | Lung SmCC - DQ - very high mag. (WC) | |||
Image: Lung small cell carcinoma - Diff-Quik -- extremely high mag.jpg | Lung SmCC - DQ - extremely high mag. (WC) | |||
</gallery> | |||
===Wright stain=== | ===Wright stain=== | ||
| Line 687: | Line 685: | ||
==Papanicolaou stain== | ==Papanicolaou stain== | ||
*Abbreviated ''Pap stain''. | *Abbreviated ''Pap stain''. | ||
{{Main|Papanicolaou stain}} | |||
==Fontana-Masson stain== | ==Fontana-Masson stain== | ||
*[[AKA]] ''Masson-Fontana stain'',<ref name=pmid16081962>{{Cite journal | last1 = Gaitanis | first1 = G. | last2 = Chasapi | first2 = V. | last3 = Velegraki | first3 = A. | title = Novel application of the masson-fontana stain for demonstrating Malassezia species melanin-like pigment production in vitro and in clinical specimens. | journal = J Clin Microbiol | volume = 43 | issue = 8 | pages = 4147-51 | month = Aug | year = 2005 | doi = 10.1128/JCM.43.8.4147-4151.2005 | PMID = 16081962 }}</ref> ''Fontana-Masson stain for melanin'', ''melanin stain''. | *[[AKA]] ''Masson-Fontana stain'',<ref name=pmid16081962>{{Cite journal | last1 = Gaitanis | first1 = G. | last2 = Chasapi | first2 = V. | last3 = Velegraki | first3 = A. | title = Novel application of the masson-fontana stain for demonstrating Malassezia species melanin-like pigment production in vitro and in clinical specimens. | journal = J Clin Microbiol | volume = 43 | issue = 8 | pages = 4147-51 | month = Aug | year = 2005 | doi = 10.1128/JCM.43.8.4147-4151.2005 | PMID = 16081962 }}</ref> ''Fontana-Masson stain for melanin'', ''melanin stain''. | ||
{{Main|Fontana-Masson stain}} | |||
==Schmorl's stain== | ==Schmorl's stain== | ||
| Line 748: | Line 711: | ||
Image: | Image: | ||
*[ | *[https://www.ole.bris.ac.uk/bbcswebdav/institution/Faculty%20of%20Health%20Sciences/Veterinary%20Science/eLearning%20resources/Pathology%20Laboratory%20Protocols/hst/msb.html MSB (bris.ac.uk)]. | ||
Ref.:<ref>URL: [http://www.bris.ac.uk/vetpath/cpl/msb.html http://www.bris.ac.uk/vetpath/cpl/msb.html]. Accessed on: 26 November 2010.</ref> | Ref.:<ref>URL: [http://www.bris.ac.uk/vetpath/cpl/msb.html http://www.bris.ac.uk/vetpath/cpl/msb.html]. Accessed on: 26 November 2010.</ref> | ||
| Line 777: | Line 740: | ||
*Collagen = bright red. | *Collagen = bright red. | ||
*Muscle = dull red. | *Muscle = dull red. | ||
<gallery> | |||
File:Cerebral aneurysm EVG stain.jpg |EVG stain of a cerebral aneurysm. (WC/jensflorian) | |||
</gallery> | |||
==Copper stain== | ==Copper stain== | ||
| Line 798: | Line 765: | ||
===General=== | ===General=== | ||
*Used in [[medical liver disease|medical liver]] biopsies - | *Used in [[medical liver disease|medical liver]] biopsies - stains sulfhydrl groups and identifies: | ||
**Copper-associated protein. | |||
**Elastin. | |||
**[[Hepatitis B]] surface antigen.<ref name=pmid7822848>{{Cite journal | last1 = Ghosh | first1 = AK. | last2 = Dasgupta | first2 = A. | last3 = Raha | first3 = K. | last4 = Jana | first4 = A. | last5 = Majumdar | first5 = DN. | title = Hepatic histology in chronic liver disease in hepatitis B surface antigen positive cases. | journal = J Indian Med Assoc | volume = 92 | issue = 10 | pages = 333-5 | month = Oct | year = 1994 | doi = | PMID = 7822848 }}</ref> | |||
===Interpretation=== | ===Interpretation=== | ||
Features:<ref>URL: [http://www.nottingham.ac.uk/pathology/protocols/shikata.html http://www.nottingham.ac.uk/pathology/protocols/shikata.html]. Accessed on: 24 January 2011.</ref> | Features:<ref>URL: [http://www.nottingham.ac.uk/pathology/protocols/shikata.html http://www.nottingham.ac.uk/pathology/protocols/shikata.html]. Accessed on: 24 January 2011.</ref> | ||
* | *Dark purple/brown = elastin fibres, HBsAg and copper-associated protein | ||
*Light purple = background | |||
*Light purple = background | *Red = nuclei (only if counter-stain used) | ||
* | |||
==Gömöri Trichrome stain== | ==Gömöri Trichrome stain== | ||
* | *Named after George Gömöri<ref>GOMORI, G. - A rapid one-step trichrome stain. Am. J. Clin. Path. 20: 661-664, 1950.</ref> | ||
===General=== | ===General=== | ||
*Used in [[muscle]] | *Used in [[muscle biopsies]] - used to find abnormal mitochondrial deposits. | ||
===Interpretation=== | ===Interpretation=== | ||
| Line 821: | Line 789: | ||
Images: | Images: | ||
<gallery> | <gallery> | ||
File:Ragged red fibers in MELAS.jpg | Ragged red fibers in MELAS, a mitochondrial disease (WC) | File:Ragged red fibers in MELAS.jpg | Ragged red fibers in MELAS, a mitochondrial disease. (WC) | ||
File:Dilated peri-tubular capillaries filled with sickled RBCs, original Gomori's trichrome stain.jpg | Sickle cell nephropathy (WC) | File:Dilated peri-tubular capillaries filled with sickled RBCs, original Gomori's trichrome stain.jpg | Sickle cell nephropathy. (WC) | ||
</gallery> | |||
==Miller stain== | |||
===General=== | |||
*Stains elastin. | |||
*Used to identify blood vessels and [[pleural invasion]] in [[lung cancer]]. | |||
===Interpretation=== | |||
Staining:<ref>URL: [https://www.ihcworld.com/_protocols/special_stains/miller's_elastic_ellis.htm https://www.ihcworld.com/_protocols/special_stains/miller's_elastic_ellis.htm]. Accessed on: 28 August 2015.</ref> | |||
*Black = elastin fibres, granules in mast cells. | |||
*Red = collagen. | |||
*Yellow = muscle, fibrin, [[erythrocytes]]. | |||
*Green/brown = nuclei. | |||
====Images==== | |||
<gallery> | |||
Image: Normal visceral pleura of lung - Miller -- high mag.jpg | Miller stain showing lung tissue. (WC) | |||
</gallery> | </gallery> | ||
Latest revision as of 16:05, 1 May 2024
This article deals with stains. The H&E stain is only one of many stains that are used in pathology.
Non-H&E stains are often referred to as special stains.
Where to start...
Principles
When considering additional (i.e. special) stains one should (in order) do the following:[1]
- Make sure one has exhausted the clinical history; history is considered the best special stain.
- Special stains (below).
- Immunohistochemistry (dealt with in a separate article).
- Molecular testing, electron microscopy.
Common stains
Immunohistochemistry
General
- Abbreviated IHC.
Interpretation
Simple version:
- Positive is (usually): brown.
- Negative tissue is: light blue.
Important notes:
- One has to know where the target (of the antibody) is supposed to be, i.e. cytoplasm vs. cell membrane.
- The edge of the tissue may have light staining - edge effect.
- If everything is brown... suspect that it didn't work.
- In some situations you're blessed with an internal control, e.g. in renal tumours CD10 will stain RCC and the proximal tubule, in GISTs - CD117 the mast cells are positive.
Work-up of infection
It often not possible to be definitive by staining.[2]
Basic panel:
- Gram stain - for bacteria.
- GMS stain - fungal stain.
- PAS (or PAS-D) - fungal stain.
Fungi
Fungi are a type of microorganisms. They are seen by pathologist every once in a while.
Specific stains
What follows is a big list... of stains.
Haematoxylin and eosin stain
- Abbreviated H&E.
Haematoxylin phyloxin saffron stain
General
- Abbreviated HPS.
- An alternative to the H&E stain - some pathol. departments use this as their standard.
Interpretation
- Haematoxylin = blue -- stains nucleus.
- Phyloxin = pink -- stains muscle and cytoplasm.
- Saffron = yellow -- stains collagen.
- An alternative to H&E stain.
- Fibrosis is easier to see on HPS than H&E... as one can see the collagen.
Images
Periodic acid Schiff stain
- Abbreviated PAS.
Primary application
- Kidney biopsies, medical.
- Liver biopsies, medical.
- Positive in alpha-1 antitrypsin deficiency.
Utility
- Stains - lipofuscin,[3] basement membranes, fungi, glycogen, (neutral) mucin.
Interpretation
- Magenta = glycogen, mucin, fungi.
- Blue = nuclei.
Ref.:[4]
Image
Periodic acid Schiff fungal stain
- Abbreviated PASF.
Primary application
- Look for fungal organisms.
Interpretation
- Light purple = fungi.
- Light green = background.
- Washed-out light purple = Gram positive bacilli.
Note:
- This is much improved over the PAS in the context of skin, as the background is similar to the fungal organisms.
Periodic acid Schiff with diastase
- Abbreviated: PAS-D and PASD.
General
Use
- Stains mucin.
- Used to identify glycogen (together with PAS stain).
- Glycogen = clear (digested) on PAS-D.
- Glycogen = magenta on PAS.
Notes: [6]
Interpretation
- Light purple = fungi.
- Light blue/pink = background. ???
Gomori methenamine-silver stain
- Abbreviated GMS.
Note:
- GMS is "Grocott's methenamine Silver" according to WMSP.[7]
Use
- Useful for fungi.
- Pneumocystis jirovecii - cause of pneumocystis pneumonia (PCP).
- Histoplasma - cause of histoplasmosis.
- Histoplasma = black, round balls.
Image
Acid-fast bacilli stains
- Abbreviated: AFB.
There are several AFB stains:
- Ziehl-Neelson stain - used to look for Mycobacterium tuberculosis.
- Fite stain - used to look for Mycobacterium leprae[8] and preferred stain for Mycobacterium avium complex.[9]
- Auramine-rhodamine stain.
Ziehl-Neelsen stain
- Most popular acid-fast bacilli stain.
- Stains other mycobacteria -- not specific for tuberculosis.
- Stains Nocardia.[10]
Image
Fite stain
Interpretation:
- Red = AFB.
- Blue = background.
Auramine-rhodamine stain
- Fluorescent stain.
Image
Kinyoun stain
- Another AFB stain[11] - useful for cryptosporidiosis and microsporidiosis.[12]
Congo red stain
Use
- Used to look for amyloid.
- Mnemonic: CRAP = congo red amyloid protein.
- An alternate stain for amyloid is Thioflavin T.
Note:
- Thick sections (~10 micrometers) are considered a requirement for the stain to work properly.[13]
- If the section is too thin... it doesn't work.
Interpretation
- Amyloid = pink/red.
- Nuclei = blue.
Ref.:[14]
Image
Congo red staining in cerebral amyloid angiopathy. (WC)
Thioflavin T stain
Use
- Used to look for amyloid.
Interpretation
- Amyloid = green.
Image: Amyloid (inano.au.dk).
Gram stain
Use
- "It is useless for finding bacteria."[15]
- If they are to be seen... they'll be visible on H&E.
Note:
- Microbiology is better at finding organisms than pathology.
- They have one significant advantage -- if a small amount of bugs are present... they grows into a large (obviously visible) colony.
DDx for common patterns
A short list of bacteria and their characteristics:[16]
| Shape\Gram stain | Positive | Negative | Variable or negative |
|---|---|---|---|
| Bacilli | Clostridium difficile, Bacillus anthracis, Nocardia spp. | Escherichia coli, Helicobacter pylori, Yersinia pestis, Hemophilus influenzae | Mycobacterium tuberulosis, Legionella pneumophila[17] |
| Cocci | Streptococcus pneumoniae, Staphylococcus aureus | Neisseria meningitidis, Moraxella catarrhalis |
Interpretation
- Purple (or blue) = Gram positive organisms.
- Red = Gram negative organisms, nuclei.[18]
- Yellow = background.
Notes:
- Many of the bacteria are quite small relative to lymphocytes; Escherichia coli is 1-2 micrometers long x 0.25 micrometers in diameter.[19]
- Epithelial cell nuclei & stromal cell nuclei may stain red.
- Memory device: purple = positive.
Images
Luxol fast blue stain
- Abbreviated LFB.
Use
- Neuropathology, myelin stain.
Intepretation
- Blue = myelinated fibers (contain lipoproteins), lipofuscin.[20]
- Lack of blue (where it ought to be) = demyelination.
- Purple = nerve cell (e.g. neuron).
- Neutrophils = pink.
Ref.:[21]
Image
Giemsa stain
Use
- Useful for finding mast cells.
- Useful for finding Donovan bodies and Leishmania.[22]
Interpretation
- Tissue is light blue/green.
- Goblet cells are purple.[23]
Image:
Reticulin stain
Use
- Liver biopsy, medical.
- Demonstrates the reticular fibers (in cirrhosis the fibers are disrupted).
- Before IHC, reticulin was used to differentiate sarcomas from carcinomas:[25]
- Sarcomas have reticulin around each cell.
- Carcinomas have reticulin around clusters of cells.
- Commonly used in neuropathology.
- In adenoma, reticulin highlights the lost acinar structure of normal pituitary gland.
- Paraganglioma (Zellballen architecture)
- Separating schwannoma (basement membrane around each cell) from meingioma in cerebellopontine angle.
- Separating desmoplastic medulloblastoma from classic/anaplastic forms.
Interpretation
- Black = reticular fibers.
- Red = nuclei.
Notes:[26]
Images
Liver. Reticulin stain. (WC)
Hepatic adenoma. Reticulin stain. (WC)
Cresyl violet stain
Use
- Used at some places (e.g. SMH) to look for Helicobacter organisms.
Interpretation
- Everything is shades of blue.
- Helicobacter stains blue.
Prussian blue stain
- AKA Perl's iron stain.
Use
- Useful for iron and hemosiderin; useful for differentiating brown pigments (melanin, lipofuscin, tattoo pigment, hemosiderin).
Interpretation
- Blue = iron.
Image:
Notes:
- Described well by vetmed.vt.edu.[27]
- DDx of brown pigment: Fontana-Masson (melanin), Kluver-Barrera stain (lipofuscin).
Images
Liver hemosiderosis. Prussian blue stain. (WC/Nephron)
Kluver-Barrera stain
Combination of:
- Luxol Fast Blue,
- Cresyl Violet,
- Special component for lipofuscin.
Use
- Useful for differentiating brown pigments (melanin, lipofuscin, tattoo pigment, hemosiderin).
- Stains lipofuscin.
- Useful to detect demyelinating lesions in the CNS.
Notes:
- PAS also stains lipofuscin and is more commonly available.
Interpretation
- Blue pigmented granules = lipofuscin.
Notes:
- Described well by vetmed.vt.edu.[28]
- DDx of brown pigment: Fontana-Masson (melanin), Prussian blue stain (hemosiderin).
Oil red O stain
Use
- Stains adipose tissue.
- Corroborate diagnosis of lipoid pneumonia.[29]
- Screen for GERD - positive staining seen in macrophages from BAL specimens.[30]
- Uncommon.
Notes:
- Must be done on fresh tissue, i.e. it cannot be fixed in formalin.
Interpretation
- Red = fat.
Images
Warthin-Starry stain
Background:
- Developed by a bunch of pathologists in Michigan to look for spirochetes.[31]
Use
- Find spirochetes, e.g. syphilis (Treponema pallidum),[32] cat-scratch disease (Bartonella henselae).
- Find Helicobacter spp., e.g. Helicobacter pylori -- Mount Sinai Hospital.[33]
Interpretation:[34]
- Spirochetes - black.
- Background - yellow.
Image
Notes:
- Considered a "dirty" stain - picks-up junk in the background.[35]
Dieterle stain
Considered a variant of the Steiner stain.[36]
Use
- Find spirochetes, e.g. syphilis (Treponema pallidum),[37] donovan bodies (leishmaniasis),[38] Helicobacter pylori and Bartonella henselae (Cat-scratch disease).[39]
Interpretation
- Spirochetes - black.
- Background - yellow.
Images
www:
Bielschowsky stain
Abbreviated: Biel stain.
Use
- Stains glial tissue, i.e. brain.
- Demonstrates neurofibrillary tangles, senile plaques (as in Alzheimer's disease).
Interpretation
- Black = axons, tangles, plaques.
- Brown/dark brown = plaque, vascular amyloid.
- Yellow/brown = other.
Ref.: [40]
Image
Mucicarmine stain
- Stains some mucins... uses the dye carmine.
Use
- Identify mucin.
- Malignant cells that produce mucin... carcinomas.[41]
Interpretation
- Carmine with metanil yellow and Weigert's Hematoxylin:[42]
- Blue/black = nucleus.
- Yellow = background.
- Red = mucin.[43]
Images
Cryptococcosis. Mucicarmine stain. (WC/CDC)
www:
- Mucicarmine stained bowel (medschool.lsuhsc.edu).
- Mucicarmine stained pancreatic adenosquamous carcinoma (nature.com).
Alcian blue stain
General
- Stains acidic mucin (pH=2.5); Alcian blue = Acidic.
- A variant uses pH=1.0.[7]
Note:
- Alcian blue (not otherwise specified) usu. refers to the pH=2.5.[44]
Use
- Identify intestinal metaplasia in the stomach and esophagus -- goblets = blue.
Note:
- Esophageal submucosal glands - alcian blue positive.
Interpretation
- Blue = acidic mucins.[45]
Notes:
- Mucin stains:
Image
Barrett's type mucosa. Alcian blue stain. (WC/AFIP)
Barrett's type mucosa. Alcian blue stain. (WC/AFIP)
Sodium sulphate-alcian blue stain
- Sulfated alcian blue (abbreviated 'SAB) redirects here.
Use
- Identify amyloid.[46][47]
- Less specific than congo red but equally sensitive.
- Does not require polarized light.
Interpretation
- Green = amyloid.[46]
- Other things that are green: mast cells, mucoid degeneration, basophilic myofibre degeneration, califications.
- Yellow = background.
Image:
Movat's stain
Use
- Myxomatous degeneration of cardiac valves.
Components
Interpretation of Movat stain
- Black = nuclei and elastic fibers.
- Yellow = collagen and reticular fibers.
- Blue = mucin, ground substance.
- Red (intense) = fibrin.
- Red = muscle.
Reference: [49]
How to remember? A.: Primary colours (red, blue, yellow) + black.
Images
Cardiac amyloidosis - Movat stain. (WC/Nephron)
Cystic medial degeneration - Movat stain - low mag. (WC/Nephron)
Masson's trichrome stain
- Should not be confused with the Mallory trichrome stain.
- May be referred to as trichrome stain.
General
- Collagen vs. muscle.
Interpretation
Notes: [51]
Elastic trichrome stain
General:
- "Elastic trichrome" is one important variant of Masson's trichrome.
Interpretation - as above in Masson's trichrome - plus:
- Black = nuclei and elastin.
Mallory trichome stain
- Should not be confused with Masson trichrome stain.
- May be referred to as trichrome stain.
General
- Collagen vs. muscle.
- May be done with elastin.
Site
- Kidney Bx (to assess for fibrosis).
- Considered better than the Masson trichrome stain.
- Liver Bx (to assess for cirrhosis).
- Cardiovascular/lung (to see differentiate the layers of the arteries, and arteries from veins).
Interpretation
- Black = nuclei.
- Red = muscle (smooth muscle actin).
- Green = collagen.
Image
Cirrhosis. Mallory trichrome. (WC/Nephron)
Haematoxylin orcein phyloxin saffron stain
Interpretation
- Blue (haematoxylin) = nuclei.
- Black (orcein) = elastin.
- Red (phyloxin) = muscle.
- Yellow (saffron) = collagen.
Jones stain
Use
- Visualize basement membrane in kidney biopsies.
- Especially useful for the diagnosis of membranous nephropathy (MN).
Interpretation
- Black = basement membrane.
- Blue = nuclei.
- Pink = other structures/background.
Notes:[54]
Images
MN demonstrated with a MPAS - very high mag. (WC/Nephron)
Hale's colloidal iron stain
von Kossa stain
General
- Type of silver stain.[55]
Use
- Look for calcium.
- Actually stains phosphates and carbonates as a surrogate for calcium.
Interpretation
- Black = calcium.[7]
Toluidine blue stain
Use
- May be useful in kidney biopsies.[56][57]
- Stains mast cells, pneumocystis jirovecii.
Interpretation
- Dark blue - nuclei, mast cell granules (darker than nuclei).
- Light blue - cytoplasm.
- Red/magneta - cartilage. (???)
Refs: looks a bit sketchy[58], [59]
Image
PCP stained with toluidine blue. (WC)
www:
Romanowsky stain
- Occasionally spelled Romanowski.
- Many variants of this stain exist.
- Specimens are air-dried.
Interpretation:[60]
- Red - RBCs, eosinophil granules.
- Blue (basophilic) - lymphocyte cytoplasm.
- Purple - nuclear chromatin, neutrophil granules, platelets.
Field stain
- Variant of the Romanowsky stain for rapid processing.
- Tends to "blow-up" cell, i.e. cells are larger vis-a-vis Pap stain.
Diff-Quik
- Pronounced Diff-Quick.
- Proprietary variant of Romanowsky stain.[61]
Uses:
- Cytopathology.
- Helicobacter gastritis - organisms are dark blue against a light blue background.[62]
Images
Lung adenocarcinoma - DQ - high mag. (WC)
Wright stain
- A variant of the Romanowsky stain; popular in North American.
Use:
- Blood films.
May-Grünwald-Giemsa stain
- A variant of the Romanowsky stain; popular in Europe.
- Abbreviated MGG.
Use:
- Blood films.
- Cytopathology.
Papanicolaou stain
- Abbreviated Pap stain.
Fontana-Masson stain
Schmorl's stain
- Stains melanin.
- Similar to Fontana-Masson stain.
Notes:[64]
Martius scarlet blue stain
General
- Stains connective tissue and fibrin.[65]
- Abbreviated MSB.
Use:
- Look for fibrinoid necrosis in vasculitis.
Interpretation
- Muscle and fibrin - red.
- Nuclei = brown/black.
- Collagen - blue.
- Red blood cells - yellow.
Image:
Ref.:[66]
Picro-Mallory stain
General
- Find fibrin.
Interpretation[67]
- Fibrin = red.
- Erythrocytes = yellow.
- Connective tissue = blue.
Image:
Verhoeff-van Gieson stain
- Verhoeff stain redirects here.
- AKA Elastic van Gieson stain, abbreviated EVG.
General
- Similar to Masson Trichrome & Verhoeff stain.[68]
Use:
- Examine large blood vessels.[69]
Interpretation
- Elastin = black.
- Collagen = bright red.
- Muscle = dull red.
Copper stain
General
- Used in liver biopsies.
- May be seen in Wilson's disease.
Note:
- Copper staining is a non-specific finding seen in many liver diseases; it is associated with impaired bile secretion.[70]
Interpretation
- Copper = red granules.
Images:
Shikata stain
General
- Used in medical liver biopsies - stains sulfhydrl groups and identifies:
- Copper-associated protein.
- Elastin.
- Hepatitis B surface antigen.[74]
Interpretation
Features:[75]
- Dark purple/brown = elastin fibres, HBsAg and copper-associated protein
- Light purple = background
- Red = nuclei (only if counter-stain used)
Gömöri Trichrome stain
- Named after George Gömöri[76]
General
- Used in muscle biopsies - used to find abnormal mitochondrial deposits.
Interpretation
- Dark green = muscle fibers.
- Red = nuclei.
- Bright red = mitochondria, red blood cells.
Images:
Miller stain
General
- Stains elastin.
- Used to identify blood vessels and pleural invasion in lung cancer.
Interpretation
Staining:[77]
- Black = elastin fibres, granules in mast cells.
- Red = collagen.
- Yellow = muscle, fibrin, erythrocytes.
- Green/brown = nuclei.
Images
See also
References
- ↑ LAE. 13 July 2010.
- ↑ Woods GL, Walker DH (July 1996). "Detection of infection or infectious agents by use of cytologic and histologic stains". Clin. Microbiol. Rev. 9 (3): 382-404. PMC 172900. PMID 8809467. http://cmr.asm.org/cgi/pmidlookup?view=long&pmid=8809467.
- ↑ Kovi J, Leifer C (July 1970). "Lipofuscin pigment accumulation in spontaneous mammary carcinoma of A/Jax mouse". J Natl Med Assoc 62 (4): 287–90. PMC 2611776. PMID 5463681. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2611776/pdf/jnma00512-0077.pdf.
- ↑ http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/PAS.PDF
- ↑ Qizilbash, A.; Young-Pong, O. (Jun 1983). "Alpha 1 antitrypsin liver disease differential diagnosis of PAS-positive, diastase-resistant globules in liver cells.". Am J Clin Pathol 79 (6): 697-702. PMID 6189389.
- ↑ http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/PASD.PDF
- ↑ 7.0 7.1 7.2 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 682. ISBN 978-0781765275.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/FITES.PDF. Accessed on: 19 May 2011.
- ↑ Ilyas S, Youssef D, Chaudhary H, Al-Abbadi MA (September 2011). "Myocbacterium-avium intracellulare associated inflammatory pseudotumor of the anterior nasal cavity". Head Neck Pathol 5 (3): 296–301. doi:10.1007/s12105-011-0248-0. PMC 3173547. PMID 21327589. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3173547/.
- ↑ URL: http://library.med.utah.edu/WebPath/LUNGHTML/LUNG024.html. Accessed on: 19 May 2011.
- ↑ Kehl, KS.; Cicirello, H.; Havens, PL. (Feb 1995). "Comparison of four different methods for detection of Cryptosporidium species.". J Clin Microbiol 33 (2): 416-8. PMID 7536216.
- ↑ Ignatius, R.; Lehmann, M.; Miksits, K.; Regnath, T.; Arvand, M.; Engelmann, E.; Futh, U.; Hahn, H. et al. (Feb 1997). "A new acid-fast trichrome stain for simultaneous detection of Cryptosporidium parvum and microsporidial species in stool specimens.". J Clin Microbiol 35 (2): 446-9. PMID 9003613.
- ↑ URL: http://www.ihcworld.com/_protocols/special_stains/congo_red_bennhold.htm. Accessed on: 26 January 2012.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/CONGORED.PDF. Accessed on: 4 December 2010.
- ↑ St. Michael's Hospital - Stains Handout.
- ↑ URL: http://www.atsu.edu/faculty/chamberlain/Website/pnebact.htm. Accessed on: 7 May 2013.
- ↑ URL: http://meded.ucsd.edu/isp/1999/CAP/legion.html. Accessed on: 7 May 2013.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/GRAM.PDF. Accessed on: 7 May 2013.
- ↑ URL: http://www.lpi.usra.edu/publications/slidesets/marslife/slide_27.html.
- ↑ MUN. 26 November 2010.
- ↑ http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/LFB.PDF
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/STAINS/STAINS.html. Accessed on: April 6, 2009.
- ↑ URL: http://www.kennedy.ox.ac.uk/facilities/histology/histology-information. Accessed on: 17 August 2015.
- ↑ URL: http://amser.org/index.php?P=AMSER--ResourceFrame&resourceId=6018. Accessed on: 17 August 2015.
- ↑ MACKENZIE DH (March 1958). "Reticulin patterns in the diagnosis of carcinomas and sarcomas". Br. J. Cancer 12 (1): 14–9. PMC 2074006. PMID 13536209. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2074006/.
- ↑ http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/RETIC.PDF
- ↑ Prussian blue stain. URL:[http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exprussb.htm. Accessed on: 5 May 2010.
- ↑ Kluver-Barrera stain. URL:http://education.vetmed.vt.edu/curriculum/VM8054/labs/Lab2/Examples/exkluvbarr.htm. Accessed on: 5 May 2010.
- ↑ Yampara Guarachi, GI.; Barbosa Moreira, V.; Santos Ferreira, A.; Sias, SM.; Rodrigues, CC.; Teixeira, GH. (2014). "Lipoid pneumonia in a gas station attendant.". Case Rep Pulmonol 2014: 358761. doi:10.1155/2014/358761. PMID 25374742.
- ↑ Hopkins, PM.; Kermeen, F.; Duhig, E.; Fletcher, L.; Gradwell, J.; Whitfield, L.; Godinez, C.; Musk, M. et al. (Aug 2010). "Oil red O stain of alveolar macrophages is an effective screening test for gastroesophageal reflux disease in lung transplant recipients.". J Heart Lung Transplant 29 (8): 859-64. doi:10.1016/j.healun.2010.03.015. PMID 20466562.
- ↑ URL: http://www.merriam-webster.com/medical/warthin. Accessed on: 17 August 2010.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/STAINS/STAINS.html. Accessed on: April 6, 2009.
- ↑ http://www.dako.co.uk/index/prod_search/prod_products.htm?productareaid=41&baseprodidver=A224462007
- ↑ http://library.med.utah.edu/WebPath/HISTHTML/STAINS/STAIN029.html
- ↑ DB. 4 August 2010.
- ↑ URL: http://www.mayomedicallaboratories.com/test-catalog/Overview/80327. Accessed on: 8 August 2010.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 455. ISBN 978-0781765275.
- ↑ URL: http://www.mondofacto.com/facts/dictionary?Dieterle%27s+stain. Accessed on: 4 August 2010.
- ↑ URL: http://www.mayomedicallaboratories.com/test-catalog/Overview/80327. Accessed on: 8 August 2010.
- ↑ http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/BIELSCH.PDF
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 681 (Q25). ISBN 978-1416025887.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 678. ISBN 978-0781765275.
- ↑ http://www.medschool.lsuhsc.edu/pathology/pathist/SURGPATH/special%20stains/assets/mucicarmine3.jpg
- ↑ URL: http://www.pathologyoutlines.com/topic/stainsalcianblue.html. Accessed on: 11 October 2012.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/ALCIAN.PDF. Accessed on: 20 December 2011.
- ↑ 46.0 46.1 Pomerance, A.; Slavin, G.; McWatt, J. (Jan 1976). "Experience with the sodium sulphate-Alcian Blue stain for amyloid in cardiac pathology.". J Clin Pathol 29 (1): 22-6. PMID 55419.
- ↑ URL: http://www.polyrnd.com/products/reagent-assembly-kits/conventional/amyloid-stain---sulfated-alcian-blue-(sab).aspx. Accessed on: October 15, 2014.
- ↑ [1]
- ↑ 49.0 49.1 Modified Movat's Pentachrome Stain. University Penn Medicine. URL: http://www.med.upenn.edu/mcrc/histology_core/movat.shtml. Accessed on: January 29, 2009.
- ↑ Kunnath-Velayudhan S, Larsen BT, Coley SM, De Michele S, Santoriello D, Colby TV, Bhagat G, Saqi A (March 2021). "Masson Trichrome and Sulfated Alcian Blue Stains Distinguish Light Chain Deposition Disease From Amyloidosis in the Lung". Am J Surg Pathol 45 (3): 405–413. doi:10.1097/PAS.0000000000001593. PMID 33002919.
- ↑ ULR: http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/MASSONS.PDF. Accessed on: 2 November 2011.
- ↑ Perry JR, Bilbao JM, Gray T (1992). "Fatal basilar vasculopathy complicating bacterial meningitis". Stroke 23 (8): 1175–8. PMID 1636194. Free Full Text.
- ↑ Jones, DB.. "Nephrotic glomerulonephritis.". Am J Pathol 33 (2): 313-29. PMC 1934622. PMID 13402889. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1934622/.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/MANUALS/JONES.PDF. Accessed on: 19 May 2011.
- ↑ Rungby, J.; Kassem, M.; Eriksen, EF.; Danscher, G. (Jun 1993). "The von Kossa reaction for calcium deposits: silver lactate staining increases sensitivity and reduces background.". Histochem J 25 (6): 446-51. PMID 8360080.
- ↑ Fischer EG, Moore MJ, Lager DJ (October 2006). "Fabry disease: a morphologic study of 11 cases". Mod. Pathol. 19 (10): 1295–301. doi:10.1038/modpathol.3800634. PMID 16799480. http://www.nature.com/modpathol/journal/v19/n10/abs/3800634a.html.
- ↑ Nicholas, SB.; Basgen, JM.; Sinha, S. (2011). "Using stereologic techniques for podocyte counting in the mouse: shifting the paradigm.". Am J Nephrol 33 Suppl 1: 1-7. doi:10.1159/000327564. PMID 21659728.
- ↑ URL: http://www.molecularstation.com/protocol-links/articles/Toluidine-Blue-Stain-32.html. Accessed on: 17 March 2011.
- ↑ URL: http://www.dermnetnz.org/doctors/dermatopathology/stains.html. Accessed on: 17 March 2011.
- ↑ Horobin RW, Walter KJ (1987). "Understanding Romanowsky staining. I: The Romanowsky-Giemsa effect in blood smears". Histochemistry 86 (3): 331–6. PMID 2437082. http://www.springerlink.com/content/r81x25451m841866/.
- ↑ URL: http://www.ihcworld.com/_protocols/special_stains/diff_quick_ellis.htm. Accessed on: 4 January 2010.
- ↑ URL: http://www.ihcworld.com/_protocols/special_stains/diff_quick_ellis.htm. Accessed on: 30 August 2012.
- ↑ Gaitanis, G.; Chasapi, V.; Velegraki, A. (Aug 2005). "Novel application of the masson-fontana stain for demonstrating Malassezia species melanin-like pigment production in vitro and in clinical specimens.". J Clin Microbiol 43 (8): 4147-51. doi:10.1128/JCM.43.8.4147-4151.2005. PMID 16081962.
- ↑ URL: http://library.med.utah.edu/WebPath/HISTHTML/STAINS/STAINS.html. Accessed on: 5 May 2010.
- ↑ URL: http://www.bris.ac.uk/vetpath/cpl/msb.html. Accessed on: 26 November 2010.
- ↑ URL: http://www.bris.ac.uk/vetpath/cpl/msb.html. Accessed on: 26 November 2010.
- ↑ "Picro-Mallory for Fibrin – Long Version". http://stainsfile.info/StainsFile/stain/fibrin/picro-mallory-1.htm. Retrieved 17 January 2011.
- ↑ URL: http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/Lab2/Examples/exvrmass.htm. Accessed on: 3 January 2011.
- ↑ URL: http://education.vetmed.vt.edu/Curriculum/VM8054/Labs/Lab2/Examples/exvvg.htm. Accessed on: 3 January 2011.
- ↑ Miyamura H, Nakanuma Y, Kono N (December 1988). "Survey of copper granules in liver biopsy specimens from various liver abnormalities other than Wilson's disease and biliary diseases". Gastroenterol. Jpn. 23 (6): 633–8. PMID 2464523.
- ↑ URL: http://www.naika.or.jp/im2/42/10/14c.aspx. Accessed on: 24 January 2011.
- ↑ http://www.mayomedicallaboratories.com/test-catalog/Overview/9836. Accessed on: 24 January 2011.
- ↑ URL: http://informahealthcare.com/doi/abs/10.3109/00313027709085239?journalCode=pat. Accessed on: 24 January 2011.
- ↑ Ghosh, AK.; Dasgupta, A.; Raha, K.; Jana, A.; Majumdar, DN. (Oct 1994). "Hepatic histology in chronic liver disease in hepatitis B surface antigen positive cases.". J Indian Med Assoc 92 (10): 333-5. PMID 7822848.
- ↑ URL: http://www.nottingham.ac.uk/pathology/protocols/shikata.html. Accessed on: 24 January 2011.
- ↑ GOMORI, G. - A rapid one-step trichrome stain. Am. J. Clin. Path. 20: 661-664, 1950.
- ↑ URL: https://www.ihcworld.com/_protocols/special_stains/miller's_elastic_ellis.htm. Accessed on: 28 August 2015.
External links
- Procedure manuals - med.utah.edu.
- Special stains (introduction) - med.utah.edu.
- Stains - histology-world.com.