Barrett's esophagus
(Redirected from Barrett esophagus)
Jump to navigation
Jump to search
| Barrett's esophagus | |
|---|---|
| Diagnosis in short | |
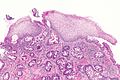
 Esophagus with intestinal metaplasia, as seen in Barrett esophagus. H&E stain. | |
|
| |
| LM | columnar epithelium with goblet cells |
| LM DDx | low-grade columnar dysplasia of the esophagus, gastroesophageal reflux disease, nonspecific inflammation at the GE junction |
| Stains | Alcian blue stain (pH 2.5) |
| Site | esophagus |
|
| |
| Associated Dx | gastroesophageal reflux disease, esophageal adenocarcinoma, columnar dysplasia of the esophagus |
| Prevalence | relatively common |
| Endoscopy | red/light brown esophageal mucosa, at gastro-esophageal junction |
| Prognosis | good |
| Treatment | on-going surveillance for columnar dysplasia |
- Intestinal metaplasia of the esophagus redirects here.
Barrett's esophagus, abbreviated BE, is a relatively common pathology of the esophagus, that is associated with an increased risk of esophageal adenocarcinoma.
General
- Diagnosis is made by clinicans not pathologists.
- A common histologic correlate is metaplastic transformation of stratified squamous epithelium to simple columnar epithelium with goblet cells.
- Associated with gastroesophageal reflux disease (GERD).
- Considered to be a consequence of chronic GERD.[4]
Significance of Barrett's esophagus:
- Increased risk of adenocarcinoma of the esophagus.
- Need on-going surveillance, i.e. long term follow-up/repeat esophagogastroduodenoscopy.
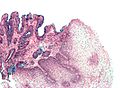
Gross
- Red/light brown esophageal mucosa.
- Normal mucosa = light pink.
Prague Classification Barrett's Esophagus
- Commonly used in by endoscopists.
- Quantifies the extent of Barrett's esophagus.
Meaning:[5]
- C = circumferential length.
- M = maximal length.
Images
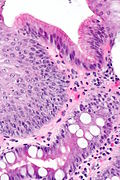
Microscopic
Features:
- Columnar epithelium with:
- Goblet cells - key feature.
- +/-Moderate chronic inflammation +/- acute inflammation -- common.[6]
- +/-Mild nuclear hyperchromasia.
- +/-Squamous epithelium with changes of gastroesophageal reflux.
DDx:
- Chronic gastritis.
- Helicobacter gastritis.
- Low-grade columnar dysplasia of the esophagus.
- Carry over from a concurrent duodenal biopsy - fragments with goblets cells have no gastric-type epithelium.
Images
Barrett's type mucosa. Alcian blue stain. (WC)
Stains
- Alcian blue (pH 2.5)[7] - goblet cells +ve.
Sign-out
Esophagus, Distal, Biopsy: - Columnar epithelium with intestinal metaplasia, see comment. - Reactive squamous epithelium. - NEGATIVE for dysplasia and NEGATIVE for malignancy. Comment: The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
Block letters
ESOPHAGUS, DISTAL, BIOPSY: - COLUMNAR EPITHELIUM WITH INTESTINAL METAPLASIA AND MILD ACUTE INFLAMMATION, SEE COMMENT. - REACTIVE SQUAMOUS EPITHELIUM. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
ESOPHAGUS, DISTAL, BIOPSY: - COLUMNAR EPITHELIUM WITH INTESTINAL METAPLASIA AND MODERATE CHRONIC INFLAMMATION, SEE COMMENT. - REACTIVE SQUAMOUS EPITHELIUM. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
ESOPHAGUS, DISTAL, BIOPSY: - COLUMNAR EPITHELIUM WITH EXTENSIVE INTESTINAL METAPLASIA, ACUTE AND CHRONIC INFLAMMATION; - SEE COMMENT. - REACTIVE SQUAMOUS EPITHELIUM. - NEGATIVE FOR DYSPLASIA AND NEGATIVE FOR MALIGNANCY. COMMENT: The columnar epithelium with intestinal metplasia is seen located deep to the squamous epithelium. The findings are consistent with Barrett's esophagus in the appropriate endoscopic setting.
See also
References
- ↑ Riddell, RH.; Odze, RD. (Oct 2009). "Definition of Barrett's esophagus: time for a rethink--is intestinal metaplasia dead?". Am J Gastroenterol 104 (10): 2588-94. doi:10.1038/ajg.2009.390. PMID 19623166.
- ↑ Odze R (August 2018). "Histology of Barrett's Metaplasia: Do Goblet Cells Matter?". Dig. Dis. Sci. 63 (8): 2042–2051. doi:10.1007/s10620-018-5151-z. PMID 29998421.
- ↑ Chandrasoma, P.; Wijetunge, S.; DeMeester, S.; Ma, Y.; Hagen, J.; Zamis, L.; DeMeester, T. (Jan 2012). "Columnar-lined esophagus without intestinal metaplasia has no proven risk of adenocarcinoma.". Am J Surg Pathol 36 (1): 1-7. doi:10.1097/PAS.0b013e31822a5a2c. PMID 21959311.
- ↑ Yantiss, RK. (Nov 2010). "Diagnostic challenges in the pathologic evaluation of Barrett esophagus.". Arch Pathol Lab Med 134 (11): 1589-600. doi:10.1043/2009-0547-RAR1.1. PMID 21043812.
- ↑ "Validation of the Prague C & M criteria for the endoscopic grading of Barrett's esophagus by gastroenterology trainees: a multicenter study". Gastrointest Endosc 75 (2): 236–41. February 2012. doi:10.1016/j.gie.2011.09.017. PMC 4547779. PMID 22248595. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4547779/.
- ↑ Voutilainen, M.; Färkkilä, M.; Mecklin, JP.; Juhola, M.; Sipponen, P. (Nov 1999). "Chronic inflammation at the gastroesophageal junction (carditis) appears to be a specific finding related to Helicobacter pylori infection and gastroesophageal reflux disease. The Central Finland Endoscopy Study Group.". Am J Gastroenterol 94 (11): 3175-80. doi:10.1111/j.1572-0241.1999.01513.x. PMID 10566710.
- ↑ Voutilainen, M.; Färkkilä, M.; Juhola, M.; Mecklin, JP.; Sipponen, P. (Nov 1999). "Complete and incomplete intestinal metaplasia at the oesophagogastric junction: prevalences and associations with endoscopic erosive oesophagitis and gastritis.". Gut 45 (5): 644-8. PMID 10517897.