Difference between revisions of "Course:Introduction to Neuropathology"
Jensflorian (talk | contribs) (→Antibodies in neurooncology: +gfap) |
Jensflorian (talk | contribs) (→Molecular neuropathology: Myopathology (Source: en. wikipedia.org + wikimedia commons)) |
||
| (8 intermediate revisions by the same user not shown) | |||
| Line 201: | Line 201: | ||
*'''GFAP''' (Ab-1) The 49kDa glial fibrillary acidic protein is an intermediate filament protein that is expressed by numerous cell types of the CNS including astrocytes and ependymal cells. It is related to otherintermediate filaments such as desmin and vimentin. Loss of GFAP through mutations results in Alexanders Disease where the white matter degenerates. Brain tumors that are derived of astrocytes ([[astroccatoma]] and [[glioblastoma]] stain for GFAP, that is absent in metastatic carcinomas and oligodendrogliomas [except for [[minigemistocyte]]s. Local and reactive astrocytes between brain tumor cells may mark for GFAP and should not confused with tumour positivity. White matter serves as ideal positive control. Cross-reactivity is seen with peripheral Schwann cells. | *'''GFAP''' (Ab-1) The 49kDa glial fibrillary acidic protein is an intermediate filament protein that is expressed by numerous cell types of the CNS including astrocytes and ependymal cells. It is related to otherintermediate filaments such as desmin and vimentin. Loss of GFAP through mutations results in Alexanders Disease where the white matter degenerates. Brain tumors that are derived of astrocytes ([[astroccatoma]] and [[glioblastoma]] stain for GFAP, that is absent in metastatic carcinomas and oligodendrogliomas [except for [[minigemistocyte]]s. Local and reactive astrocytes between brain tumor cells may mark for GFAP and should not confused with tumour positivity. White matter serves as ideal positive control. Cross-reactivity is seen with peripheral Schwann cells. | ||
*'''IDH1''' (IDH1 R132H) The isocitrate dehydrogenase is an important enzyme catalyzing the oxidative decarboxylation of isocitrate to 2-oxoglutarate. Mutations in motochondrial IDH1 and its cytoplasmic homologue IDH2 are among the most frequent mutations in diffuse gliomas, including [[astrocytoma]], [[oligodendroglioma]] and the secondary [[glioblastoma]]s that are derived therof. In contrast primary (de novo) glioblastomas usually do not carry this mutation. IDH1 mutations are heterozygous, typically involving an amino acid substitution in the active site of the enzyme in codon 132. The employed antibody is specific for the very common R132H amino acid exchange. It doesn't detect rare R132C or other IDH2 mutations. In such cases direct sequencing is necessary. Because the R132H mutation is tumor specfic, positive staining (oligodendrogliomas are ideal controls) is proves presence of a neoplasm. | |||
*'''ATRX''' - Alpha thalassemia/mental retardation syndrome X-linked is a member of the WSI/SNF chromatin remodelling family of proteins that have an important roel in sgegation of chromosomes during mitosis. It is expressed in the nuclei of all normal tissues and is lost in [[astrocytoma]]s that use alternative lengthening of telomeres (ALT) as their telomere maintenance mechanism. Since nuclear staining is lost only in IDH1 mutated astrocytomas, the antibody is a very usefula diagnostic biomarker to separate astrocytoma from [[oligodendroglioma]]. Itis however not useful to separate primary glioblastoma from other ATRX-positive tumors such as oligodendroglioma or brain metastases. | |||
====Typical staining patterns==== | |||
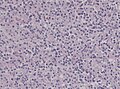
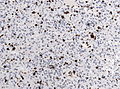
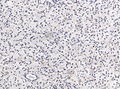
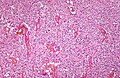
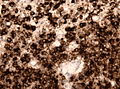
*Glioblastoma | |||
<gallery> | |||
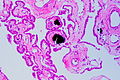
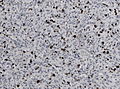
File:Neuropathology_case_IX_02.jpg | [[H&E]] | |||
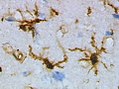
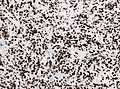
File:Neuropathology_case_IX_04.jpg | [[GFAP]] | |||
File:Neuropathology_case_IX_06.jpg | MIB-1 | |||
File:Neuroparthology case IX 0125.jpg | [[ATRX]] | |||
File:Neuropathology case IX.jpg | [[IDH-1]] | |||
File:Neuropathology case IX.jpg | panCK | |||
</gallery> | |||
[[Glioblastoma]] is a pleomorphic astroglial tumor with endothelial proliferations and necrosis. As expected by a malignant tumor, the number of proliferating cells (MIB-1) is high. The tumour cells often stain for [[GFAP]]. There is no [[ATRX]] loss and the [[IDH-1]] R132H mutation is absent (negative staining). | |||
{{hidden|Other language: German| Glioblastome sind pleomorphe astrogliale Tumore mit Gefäßproliferaten und Nekrosen. Entsprechend einem malignen Tumor ist die Anzahl der proliferierenden Zellen (MIB-1) hoch. Die Tumorzellen markieren sich für GFAP. Es besteht kein Verlust von ATRX und die IDH1 R132H Mutationsfärbung ist negativ. | |||
}} | |||
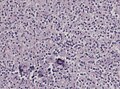
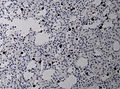
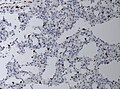
*Oligodendroglioma | |||
<gallery> | |||
File:Oligodendroglioma1 low mag.jpg | [[H&E]] | |||
File:Oligodendorglioma GFAP.jpg| [[GFAP]] | |||
File:Neuropathology case II 04.jpg | MIB-1 | |||
File:Neuroparthology case IX 0125.jpg | [[ATRX]] | |||
File:IDH1 R132H in anaplastic ologodendroglioma.jpg | [[IDH-1]] | |||
File:Neuropathology case IX.jpg | panCK | |||
</gallery> | |||
[[Oligodendroglioma]] is a diffuse geowing glial tumour with clear cell morphology. In WHO grade II the MIB-1 proliferation index is rather low. GFAP stains the neuropil background and minigemistocytes (if present). There is no [[ATRX]] loss. The vast majority of oligodendrogliomas stain positively for [[IDH-1]] R132H mutation.There is no expression of epithelial markers (panCK). | |||
{{hidden|Other language: German|Oligodendrogliome sind diffus wachsende gliale Tumore mit klarzelligem Aspekt in der Morphologie. In WHO Grad II Tumoren ist der MIB-1 Proliferationsindex gering. GFAP färbt vor allem das Neuropil im Hintergrund sowie Minigemistozyten, wenn diese im Tumor vorkommen. Es findet sich kein ATRX Verlust. Der Großteil der Oligodendrogliome ist positiv für die IDH1 R132H Mutation. Epitheliale Marker wie panCK werden nicht exprimiert.}} | |||
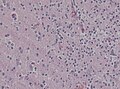
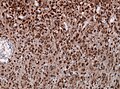
*Astrocytoma | |||
<gallery> | |||
File:Astrocytoma whoII HE.jpg | [[H&E]] | |||
File:GFAP astrocytoma.jpg | [[GFAP]] | |||
File:Neuropathology case II 04.jpg | MIB-1 | |||
File:Neuropathology case II ATRX immunohistochemistry.jpg | [[ATRX]] | |||
File:IDH1R132H oligoastrocytoma.jpg | | [[IDH-1]] | |||
File:Neuropathology case IX.jpg | panCK | |||
</gallery> | |||
[[Astrocytoma]] is a diffusely growing tumor with low cell density, neoplastic astrocytes resting in a fibrillary backrgound and low MIB1 index. [[GFAP]] is strong and also stains the cell processes. [[IDH-1]] R132H postive astrocytomas usually exhibit nuclear [[ATRX]] loss. There is no expression of epithelial markers (panCK). | |||
{{hidden|Other language: German|Astrozytome sind diffus wachsende gliale Tumore mit sternförmigen Astrozyten auf einem fibrillärem Untergrund. In WHO Grad II Tumoren ist der MIB-1 Proliferationsindex gering. GFAP färbt die Tumorzellen und den Hintergrund stark an Es findet sich in IDH1 R132H mutierten Tumoren häufig ein ATRX Verlust. Epitheliale Marker wie panCK werden nicht exprimiert.}} | |||
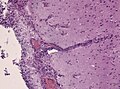
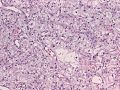
*Carcinoma metastasis | |||
<gallery> | |||
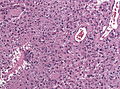
File:Neuropathology_case_XIII_01.jpg | HE | |||
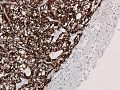
File:Neuropathology_case_XIII_03.jpg | [[GFAP]] | |||
File:Neuropathology_case_XII_05.jpg | MIB-1 | |||
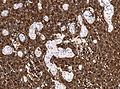
File:Neuropathology_case_XIII_04.jpg | [[ATRX]] | |||
File:Neuropathology_case_XIII_06.jpg | [[IDH-1]] | |||
File:Neuropathology_case_XIII_02.jpg | panCK | |||
</gallery> | |||
[[Brain_metastasis|Brain metastases]] are usually circumscribed lesions that infiltrate the brain parenchyma. Most metastases are carcinomas as in this case of a renal clear cell carcinoma. At the first glance, it's morphology is similiar to [[oligodendroglioma]], but absence of [[GFAP]] and postive cytokeratin staining confirms epithelial origin. As expected from a malignant tumor, MIB-1 proliferation is elevated. There is no [[ATRX]] loss and no [[IDH-1]] mutation present. | |||
{{hidden|Other language: German|Hirnmetastasen sind in der Regel umschriebene Läsionen, die das Hirnparenchym infiltrieren. Die meisten Metastasen sind Karzinome, wie in diesem Fall eines klarzelligen Nierenzellkarzinom. Auf den ersten Blick ist die Morphologie zum Oligodendrogliom sehr ähnlich, aber das Fehlen von GFAP und die Immunreaktivität für pan-Zytokeratin bestätigen die epitheliale Herkunft. Wie bei malignen Tumoren zu erwarten, ist die MIB-1 Proliferationsrate erhöht. Es existiert kein ATRX-Verlust und keine IDH1-Mutation.}} | |||
A descriptive overview of various brain tumours is found [[Neuropathology tumours|here]]. | A descriptive overview of various brain tumours is found [[Neuropathology tumours|here]]. | ||
====Molecular neurooncology==== | |||
Because [[IDH-1]] and IDH-2 mutations are found in up to 80% of [[astrocytoma]]s and [[oligodendroglioma]], IDH-1 R132H (which detects only the R132H substitution <ref name=pmid19798509>{{Cite journal | last1 = Capper | first1 = D. | last2 = Zentgraf | first2 = H. | last3 = Balss | first3 = J. | last4 = Hartmann | first4 = C. | last5 = von Deimling | first5 = A. | title = Monoclonal antibody specific for IDH1 R132H mutation. | journal = Acta Neuropathol | volume = 118 | issue = 5 | pages = 599-601 | month = Nov | year = 2009 | doi = 10.1007/s00401-009-0595-z | PMID = 19798509 }}</ref>) stained negative cases are sequenced for other rare mutations that include IDH1 R132C or IDH2 R172K among others. These mutations are not only useful in differential diagnosis of brain tumours but also prognostic, because tumours carrying a IDH-1 or IDH-2 mutation usually show a more favourable course than their wild-type counterparts <ref name=pmid21088844>{{Cite journal | last1 = Hartmann | first1 = C. | last2 = Hentschel | first2 = B. | last3 = Wick | first3 = W. | last4 = Capper | first4 = D. | last5 = Felsberg | first5 = J. | last6 = Simon | first6 = M. | last7 = Westphal | first7 = M. | last8 = Schackert | first8 = G. | last9 = Meyermann | first9 = R. | title = Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas, and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas. | journal = Acta Neuropathol | volume = 120 | issue = 6 | pages = 707-18 | month = Dec | year = 2010 | doi = 10.1007/s00401-010-0781-z | PMID = 21088844 }}</ref>. | |||
[[Oligodendroglioma]]s show a more favourable course and therfore are treated differently than [[astrocytoma]]s. A clear separation of these two entities is important, because [[H&E]] morphology is not always convincing. Succesful treatment depends on allelic losses on chromosomal arms 1p and 19q in oligodendroglioma that can be obtained by copy-number analysis or microsatellite PCR. By combining LOH (loss of heterozygosity) 1p/19q and [[ATRX]] status it is also possible to place the mixed [[oligoastrocytoma]]s into the astrocytoma or oligodendroglioma group. | |||
===Day 1=== | |||
====Immunofluorescence==== | |||
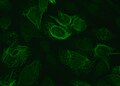
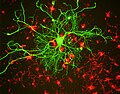
Immunofluorescence is a technique used for light microscopy with a fluorescence microscope (usually a confocal microscope). This technique uses the specificity of antibodies to their antigen to target fluorescent dyes to specific biomolecule targets within a cell, and therefore allows visualisation of the distribution of the target molecule through the sample. The typical approach uses a unlabeled first (primary) antibody that specifically binds the target molecule, and the secondary antibody, which carries the fluorophore, recognises the primary antibody and binds to it. Advantages of immunofluorescence are the usually better resolution of the signals compared with standard light-microscope stains and the possibility to combine antibodies of different species to target two or more epitopes with different fluorophores. These different signals can be merged into a single image. | |||
<gallery> | |||
File:VIMENTIN.jpg | Immunofluorescence staining for vimentin in human epithelial cells (green). | |||
File:Neuron in tissue culture.jpg | Combined immunofluoerescence to visualize Neurofilament (green) and alpha-internexin (red). | |||
</gallery> | |||
====Myopathology==== | |||
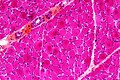
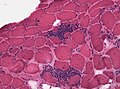
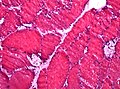
The skeletal muscle is anchored by tendons (or by aponeuroses at a few places) to bone and is used to effect skeletal movement such as locomotion and to maintain posture. Striated or skeletal muscle only contracts voluntarily, upon influence of the central nervous system.Skeletal muscle is further divided into several subtypes: | |||
* Type I, slow oxidative, slow twitch, or "red" muscle is dense with capillaries and is rich in mitochondria and myoglobin, giving the muscle tissue its characteristic red color. It can carry more oxygen and sustain aerobic activity. | |||
* Type II, fast twitch muscle, has three major kinds that are, in order of increasing contractile speed. | |||
Muscle biopsies are performed to obtain a specific diagnosis in persisting weakness or muscle pain. | |||
<gallery> | |||
File:1007 Muscle Fibes (large).jpg | Structure of myofibers. | |||
File:Denervation atrophy - high mag.jpg | Cross section of skeletal muscle (HE stain). The variation in size is due to loss of innervation (neurogenic atrophy). | |||
File:DM2 Histopathology.jpg | Slow myosin staining in muscle cross section highlighting type 1 fibers (brown). | |||
File:Polymyositis HE.jpg | Inflammatory cells in muscle fibers allow the diagnosis of myositis. | |||
File:Pompe vacuoles.jpg | Defects in muscle enzymes result in abnormal storage - here vacuoles in acid maltase deficiency. | |||
File:LGMD2D alpha sarcoglycan.jpg | Inherited diseases often affect elementar structural proteins, as seen here with alpha-sarcoglycan deficiency in limb-girdle musculary dystrophy (B). | |||
</gallery> | |||
==References== | ==References== | ||
Latest revision as of 09:00, 8 October 2015
Course Neuropathology is a online collection of images and descriptions of specimens used for teaching medical students and residents.
This page is divided into following courses:
- Basic neuropathology - preclinical medical education
- Molecular neuropathology - ideal for bachelor of molecular medicine or oncology
- Advanced neuropathology - clinical medical education
Basic neuropathology
Day one
Meningioma
This H&E stain displays parts of a moderately cellular tumor growing with ovoid elongated nuclei (Pictures 1+2). There are no clear-cut cell borders discernible in light microscopy. This interveawing is called a syncytium. WHO Grading of the tumour is dependent of the mitotic activity (Picture 3) or histological hallmarks such as prominent nucleoli, high nuclear to cytoplasmic ratio, CNS infiltation etc.. Focal nuclear clearing (Nuclear pseudoinclusions, Picture 4+5) are typical cut phenomenon. The round calcified inclusions (Psammoma bodies) are characteristic for a meningioma.
- See also: Virtual slide (Meningioma I, HE, usz.ch)
Other language: German
|
|---|
|
Das H&E-Präparat zeigt Anteile eines mäßig zelldichten in Zügen und Wirbeln orientierten Tumors mit ovoid elongierten Tumorzellkernen (Bilder 1+2). Eindeutige Zellgrenzen lassen sich lichtmikroskopisch nicht definieren, was als pseudosynzytialer Aspekt bezeichnet wird. Die Wertung des Tumors nach WHO ist abhängig von der mitotischen Aktivität (Bild 3), oder durch histologische Kriterien wie z.B. prominente Nukleolen, Kern-Plasma-Relation, ZNS-Infiltration etc.. Lochkernzellen (Bild 4+5) sind hingegen ein typisches Anschnittphänomen. Auch rundliche Verkalkungen (Bild 5), sogenannte Psammomkörper sind charakteristisch für Meningeome. |
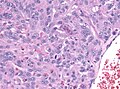
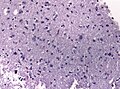
Astrocytoma
This specimen contains fragments of a diffusely growing tumor with only slight inclreased cell density and focally microcysts withing the neuropil background (Picture 1). Although many of the astrocytic tumour cells look quite similiar there is increased pleomorphism, mostly larger and a more dense chromatin. There are no mitoses seen in this tumour (Picture 2). The tumour borders are not clear, there is just a decrease of cell density a the tumor infiltration zone. In this area one is not always sure which cells are still neoplastic and which cells are normal or reactive astrocytes of the normal brain (Picture 3).
Other language: German
|
|---|
|
Das Präparat besteht aus Fragmenten eines diffus wachsenden, gering zelldichten Tumors, welcher fokal mikrozystische Auflockerungen aufweist (Bild 1). Trotz hoher Ähnlichkeit der astrozytären Tumorzellen finden sich fokal vermehrte Pleomorphie der Kerne, diese meist etwas größer und chromatindichter. Mitosen finden sich in diesem Tumor nicht. (Bild 2). Die Tumorgrenzen sind unscharf, man beobachtet lediglich eine diffus abnehmende Zelldichte im Bereich der Infiltrationszone, in der man nicht genau sagen kann, welches noch Tumorzellen sind und welche bereits normale bzw. reaktiv veränderte Astrozyten darstellen (Bild 3). |
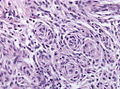
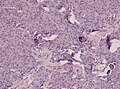
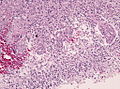
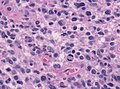
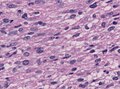
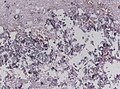
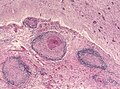
Glioblastoma
Already at low magnification extraordinary pleomorphism is evident in the cellular tumour (Picture 1). Major hallmark are extensive line-shaped necroses. Tumour cells bordering these necrotic centers are arranged in a pseudopalisading fashion (Picture 2). In addition the glioblastoma harbors neoagniogenesis with vascular proliferations of enlarged endothelial in several layers (Picture 3). The tumour cells are quite pleomorphic, somitimes round, sometimes polygonal. Plenty of mitoses are seen (Picture 4). The tumour cells show slender, elongated cytoplasmic processes, in part still resting on a neuropil-like (fibrillary) background that resembles normal CNS tissue (Picture 5).
Other language: German
|
|---|
|
Schon bei niedriger Vergrößerung erkennt man einen ausserordentlich pleomophen, zelldichten Tumor (Bild 1), dessen herausragendes Merkmal ausgeprägte strichförmige Nekroseareale sind. Die angrenzenden Tumorzellen sind entlang dieser Nekrosebezirke in Pseudopalisadenstellung aufgereiht (Bild 2). Zusätzlich finden sich innerhalb des Tumors Zeichen einer Gefäßneubildung, bei der die Gefäßwände deutlich verbreiter sind und Endothelzellen in mehreren Reihen aufweisen (Bild 3). Die Tumorzellen sind recht pleomorph , teils rundlich teils polygonal bei heterogenem Kernchromatin. Es finden sich reichlich Kernteilungsfiguren (Mitosen, Bild 4). Die Tumorzellen zeigen schmale, jedoch längere Zytoplasmaausläufer, die nur noch abschnittsweise auf einem typischen Neuropil-artigen (fibrillären) Untergrund zu liegen kommen, wie man ihn noch vom normalen ZNS kennt (Bild 5). |
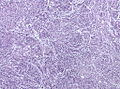
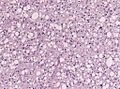
Oligodendroglioma
The sample consists mainly of tumour particles that show extensive calcifications which are already visible at low magnification (Picture 1). The tumour cells show perinuclear halos - a fixation artefact seen typically in oligodendrogliomas (Picture 2). This "fried-egg" appearance at higher cell density results in the so called "honeycomb" appearance. Oligodendrogliomas usually have monomprhic round nuclei with scant chromatin. Between the tumour cells delicate capillaries are present. In contrast to astrocytomas the tumor border is more pronounced, the infiltrative pattern is less evident (Picture 4). In absence of necrosis and almost no mitotic activity this tumour corresponds to WHO Grade II.
Other language: German
|
|---|
|
Das Präparat besteht hauptsächlich aus Tumorpartikeln, welche an mehreren Stellen deutliche Verkalkungen aufweisen. Diese lassen sich schon bei niedriger Vergrößerung beobachten (Bild 1). Die Tumorzellen zeigen ein für Oligodendrogliome typisches Präparationsartefakt bei der durch die Paraffineinbettung ein optisch leeres Zytoplasma entsteht (Bild 2). Dieser sogenannte "Spiegeleieffekt" lässt bei hoher Zelldichte auch an ein Honigwabenmuster denken. Oligodendrogliome besitzen in der Regel relativ monomorphe rundliche Kerne mit mäßigem Chromatingehalt. Zwischen den Tumorzellen verlaufen sehr feine Kapillaren. Im Gegensatz zu Astrozytomen nimmt im Randbereich die Zelldichte abrupter ab, sodaß der Tumor ein weniger diffuses Wachstum aufzeigt (Bild 4). Bei Fehlen von Nekrosen und nahezu nicht vorhandenen Mitosefiguren entspricht der Tumor einem WHO Grad II. |
Day two
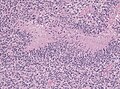
Purulent meningitis
This autopsy specimen from cerebral hemisphere shows diffuse clouding of the arachnoidea and pia mater by a dense cellular infiltrate as seen in this low magnification (Picture 1). In higher magnification the infiltrate consists mainly of neutrophil granulocytes (Picture 2). Because the granulocytes are also seen along capillaries in the Virchow-Robin space, we consider this a meningoencephalitis (Picture 3).
Other language: German
|
|---|
|
Der Gewebeschnitt zeigt Anteile des cerebralen Cortex, dessen Subrarachnoidalraum durch ein zellreiches Infiltrat verlegt ist, welches schon bei niedriger Vergrösserung gut zu erkennen ist (Bild 1). Dieses stellt sich in höherer Vergrößerung als überwiegend aus segmentkernigen neutrophilen Granulozyten bestehend dar (Bild 2). Da die Granulozyten auch entlang der Kapillaren in dem sogenannten Virchow-Robinschen Raum eindringen, spricht man genauer von einer Meningoenzephalitis (Bild 3). |
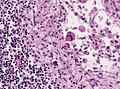
Tuberculous meningitis
This autopsy specimen was sampled in coronar section from the optic chiasm and displays numerous granulomas (Picture 1). In the brain parenchyma mutlifocal smaller infiltrates consisting of lymphocytes and monocytes. The adjacent astrocytes show reactive changes with broadly swollen, pink cytoplasm ("gemistocytes", Picture 2). The granulomas are surronded by lymphocytes and in between so called epitheloid cells with chromatin-dense, elongated, sole-like nuclei and occassionally Langhans giant cells (Picture 3). The center of the granuloma is often necrotic, such "caeseating necroses" are typical for tuberculous meningitis (Picture 4).
- Further reading: neuropathology-web.org
Other language: German
|
|---|
|
Der Gewebeschnitt in der Frontalebene auf Höhe des Chiasmas, zeigt basal zahlreiche Granulome (Bild 1). Im ZNS-Parenchym finden sich multifokal kleinere rundzellige Infiltrate aus überwiegend lympho-monozytären Zellen, die angrenzenden Astrozyten sind reaktiv verändert mit pinkfarbenem, geschwollenem Zytoplasma ("Gemistozyten" Bild 2). Die Granulome besitzen aussen einen Saum aus Lymphozyten an den sich nach innen sogenannte Epitheloidzellen mit länglichen, chromatindichten, Schuhsohlenartig geformten Kernen, Makrophagen sowie mehrkernige Riesenzellen vom Langhans-Typ (Bild 3) anschliessen. Das Zentrum der Granulome ist oft nekrotisch verändert, solche sogenannten "verkäsende Nekrosen" sind typisch für eine Tuberkulöse Meningitis (Bild 4) |
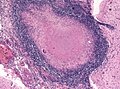
Brain abscess
At low magnification a cavity whithin brain tissue is evident (Picture 1). The necrotic core, filled with pus, consists mainly of neutrophils and macrophages. The abscess is surrounded by a fibrous capsule consisting of capillaries, macrophages, mononuclear cells, and reactive astrocytes (Picture 2). Collagen is produced by vascular cells and walls off the infection (Picture 3). Special stains (or molecular analyses) are needed to identify the causative agent.
- Further reading:http://neuropathology-web.org/chapter5/chapter5aSuppurative.html#abscess neuropathology-web.org]
Other language: German
|
|---|
|
Schon bei niedriger Vergrößerung ist ein zystischer Hohlraum im Hirngewebe sichtbar (Bild 1). Das nekrotische Zentrum, mit Eiter gefüllt, besteht hauptsächlich aus Granulozyten und Makrophagen. Der Abzess ist durch eine bindegewebige Kapsel bestehend aus Kapillaren, Makrophagen, Mononuklären Zellen und reaktiven Astrozyten gesäumt (Bild 2). Kollagen wird durch die Gefäße gebildet und schirmt den Infektionsherd ab (Bild 3). Spezielle Färbungen oder molekulare Analysen sind zur Erregeridentifikation notwendig.
|
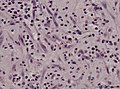
Poliomyelitis
On this cross section through the spinal cord the motor neurons of anterior and posterior horn are visible with cresyl violet staining (Picture 1). At higher magnification microglial nodules are present (Picture 2). These contain macrophages that phagocytose nerve cells (neurononophagia, Picture 3).
Other language: German
|
|---|
|
Auf diesem mit Kresylviolett gefärbten Querschnitt durch das Rückenmark sind Motorneuronen des Vorder- und Hinterhorn sichtbar (Bild 1). Bei höherer Vergrößerung erkennt man Mikrogliaknötchen (Bild 2). Diese enthalten Makrophagen, welche die Nervenzellen phagoyztieren (Neurononophagie, Bild 3). |
Molecular neuropathology
Day 1
Cells and tissues have numerous antigenic structures that serve as a target for the receptors of an adaptive immune response. These structures are found at cell surface, in cytoplasm or organelles (including the nucleus). Several antigens are found only in a specific tissue type (ie. epithelial cells) or at a given stage of the cell cycle (proliferating cells). Because human antigens are of diagnostic and/or prognostic relevance, especially in cancer diagnostics, they are often called biomarkers. Since its introduction in 1974 [1], the visualization of epitopes in paraffin-embedded specimens through immunohistochemistry has become standard practice in routine neuropathology supporting the morphology at light-microscope level.
A by far incomplete overview of antibodies used for immunohistochemical staining are found here.
Tissue processing
The dried slides are stained for H&E.
Tissue microarray
- Example of tissue cross-reactivity on human tissue microarray.jpeg
Immunohistochemical stains of a TMA section.
The tissue microarray method is sed mainly in research because of following advantages: [2]
- speed (parallel analysis of up to hundered specimen).
- cost efficient (the same amount of reagents required for a single large-section analysis)
- standardisation (the same staining conditions are applied).
- sample number (high statistical power for associations).
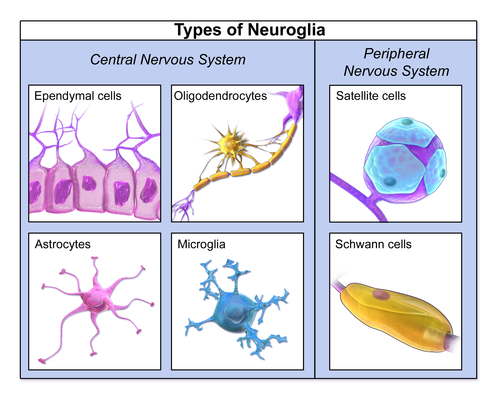
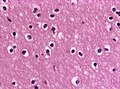
Neuropathology basics
This section deals with normal cellular constituents of the CNS.
Neurons are often very large cells, with angled edges and abundant cytoplasm that contains Nissl substance (granular perinuclear material = rough endoplasmic reticulum). The round nucleus of larger cells has weak chromatin and a prominent nucleolus. Some neurons such as the granular layer in the cerebellum are quite small instead. There are several types of glial cells. Oligodendrocytes have a small round, centrally located nucleus (lymphocyte-like). The cytoplasm is often glassy. Astrocytes have am irregular non-ovoid nucleus. They are often close to blood vessels where the form the blood-brain barrier. Their stellate cytoplasmic processes are normally not visible in normal neuropil backgeound. Ependymal cells are a simple ciliated cuboidal epithelium psitioned at the surface of the ventricles and central canal. Cells of the choroid plexus. are specialized ependymal cells surrounding a core of capillaries and loose connective tissue and are located within the ventricels where they produce the cerebrospinal fluid. Microglia are the immune-competent cells of the brain (macrophages). They often have vesicles and are rarely seen in normal tissue
Day 2
Antibodies in neurooncology
The exact classification of brain tumours is essential for proper treatment of patients. Although morphological evalutaion of the H&E stained tumour specimen is a crucial first step, subsequent immunhistochemical stains and molecular analyses help to secure the diagnosis. The following five antibodies: GFAP, MAP2, ATRX, IDH-1, pan-Cytokeratin and Ki-67 (MiB-1) allow for good classification of the most common tumours observed in the brain. A short introduction:
- Ki-67 (Kiel-67, clone MiB-1 which stands for Made in Borstel) is a nuclear protein that is associated with cellular proliferation. During interphase, the Ki-67 antigen can be exclusively detected within the cell nucleus, whereas in mitosis most of the protein is relocated to the surface of the chromosomes. Ki-67 protein is present during all active phases of the cell cycle (G1, S, G2, and mitosis), but is absent from resting cells (G0).[3] Ki-67 is an excellent marker to determine the growth fraction of a given cell population. The fraction of Ki-67-positive tumor cells (the Ki-67 labeling index) is often correlated with the clinical course of cancer. [4] An astrocytoma with 2% positive tumor cells is growing considerably slower than a glioblastoma with a labelling index of 20%. Cells with a quick turnover therefore serve as good positive controls for this antibody.
- panCK (MNF-116) Cytokeratins are proteins of keratin-containing intermediate filaments found in the intracytoplasmic cytoskeleton of eukaryontic epithelial tissue and their derived tumours. The 20 different cytokeratins can be divided into low versus high molecular weight solely based on their molecular weight. The current cocktail detects almost all types of epithelial, from simple glandular to stratfied squamous epithelia and therefore is ideal to detect malignant epithelial tumours (carcinomas). Rarely a cross-reaction with dendritic cells in the tonsil or smooth muscle cells of vessels is observed. Most brain metastases are carcinomas of breast, lung or prostrate and therefore stain intensely for pan-cytokeratin. In contrast, glial and neuronal brain tumours as well as melanomas do not stain for this marker. Expression of these cytokeratin types is frequently organ or tissue specific. Pathologists employ different cytokeratins to detect the cell of origin of various tumors. As an example, CK7 is typically expressed in the ductal epithelium of the genitourinary tract and CK20 most commonly in the gastrointestinal tract. Best results are obtained with Trypsin or Pronase pretreatment for antigen demasking. Normal epithelial tissue (gut, skin) may serve as positive control.
- GFAP (Ab-1) The 49kDa glial fibrillary acidic protein is an intermediate filament protein that is expressed by numerous cell types of the CNS including astrocytes and ependymal cells. It is related to otherintermediate filaments such as desmin and vimentin. Loss of GFAP through mutations results in Alexanders Disease where the white matter degenerates. Brain tumors that are derived of astrocytes (astroccatoma and glioblastoma stain for GFAP, that is absent in metastatic carcinomas and oligodendrogliomas [except for minigemistocytes. Local and reactive astrocytes between brain tumor cells may mark for GFAP and should not confused with tumour positivity. White matter serves as ideal positive control. Cross-reactivity is seen with peripheral Schwann cells.
- IDH1 (IDH1 R132H) The isocitrate dehydrogenase is an important enzyme catalyzing the oxidative decarboxylation of isocitrate to 2-oxoglutarate. Mutations in motochondrial IDH1 and its cytoplasmic homologue IDH2 are among the most frequent mutations in diffuse gliomas, including astrocytoma, oligodendroglioma and the secondary glioblastomas that are derived therof. In contrast primary (de novo) glioblastomas usually do not carry this mutation. IDH1 mutations are heterozygous, typically involving an amino acid substitution in the active site of the enzyme in codon 132. The employed antibody is specific for the very common R132H amino acid exchange. It doesn't detect rare R132C or other IDH2 mutations. In such cases direct sequencing is necessary. Because the R132H mutation is tumor specfic, positive staining (oligodendrogliomas are ideal controls) is proves presence of a neoplasm.
- ATRX - Alpha thalassemia/mental retardation syndrome X-linked is a member of the WSI/SNF chromatin remodelling family of proteins that have an important roel in sgegation of chromosomes during mitosis. It is expressed in the nuclei of all normal tissues and is lost in astrocytomas that use alternative lengthening of telomeres (ALT) as their telomere maintenance mechanism. Since nuclear staining is lost only in IDH1 mutated astrocytomas, the antibody is a very usefula diagnostic biomarker to separate astrocytoma from oligodendroglioma. Itis however not useful to separate primary glioblastoma from other ATRX-positive tumors such as oligodendroglioma or brain metastases.
Typical staining patterns
- Glioblastoma
Glioblastoma is a pleomorphic astroglial tumor with endothelial proliferations and necrosis. As expected by a malignant tumor, the number of proliferating cells (MIB-1) is high. The tumour cells often stain for GFAP. There is no ATRX loss and the IDH-1 R132H mutation is absent (negative staining).
Other language: German
|
|---|
Glioblastome sind pleomorphe astrogliale Tumore mit Gefäßproliferaten und Nekrosen. Entsprechend einem malignen Tumor ist die Anzahl der proliferierenden Zellen (MIB-1) hoch. Die Tumorzellen markieren sich für GFAP. Es besteht kein Verlust von ATRX und die IDH1 R132H Mutationsfärbung ist negativ. |
- Oligodendroglioma
Oligodendroglioma is a diffuse geowing glial tumour with clear cell morphology. In WHO grade II the MIB-1 proliferation index is rather low. GFAP stains the neuropil background and minigemistocytes (if present). There is no ATRX loss. The vast majority of oligodendrogliomas stain positively for IDH-1 R132H mutation.There is no expression of epithelial markers (panCK).
Other language: German
|
|---|
|
Oligodendrogliome sind diffus wachsende gliale Tumore mit klarzelligem Aspekt in der Morphologie. In WHO Grad II Tumoren ist der MIB-1 Proliferationsindex gering. GFAP färbt vor allem das Neuropil im Hintergrund sowie Minigemistozyten, wenn diese im Tumor vorkommen. Es findet sich kein ATRX Verlust. Der Großteil der Oligodendrogliome ist positiv für die IDH1 R132H Mutation. Epitheliale Marker wie panCK werden nicht exprimiert. |
- Astrocytoma
Astrocytoma is a diffusely growing tumor with low cell density, neoplastic astrocytes resting in a fibrillary backrgound and low MIB1 index. GFAP is strong and also stains the cell processes. IDH-1 R132H postive astrocytomas usually exhibit nuclear ATRX loss. There is no expression of epithelial markers (panCK).
Other language: German
|
|---|
|
Astrozytome sind diffus wachsende gliale Tumore mit sternförmigen Astrozyten auf einem fibrillärem Untergrund. In WHO Grad II Tumoren ist der MIB-1 Proliferationsindex gering. GFAP färbt die Tumorzellen und den Hintergrund stark an Es findet sich in IDH1 R132H mutierten Tumoren häufig ein ATRX Verlust. Epitheliale Marker wie panCK werden nicht exprimiert. |
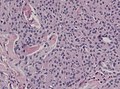
- Carcinoma metastasis
Brain metastases are usually circumscribed lesions that infiltrate the brain parenchyma. Most metastases are carcinomas as in this case of a renal clear cell carcinoma. At the first glance, it's morphology is similiar to oligodendroglioma, but absence of GFAP and postive cytokeratin staining confirms epithelial origin. As expected from a malignant tumor, MIB-1 proliferation is elevated. There is no ATRX loss and no IDH-1 mutation present.
Other language: German
|
|---|
|
Hirnmetastasen sind in der Regel umschriebene Läsionen, die das Hirnparenchym infiltrieren. Die meisten Metastasen sind Karzinome, wie in diesem Fall eines klarzelligen Nierenzellkarzinom. Auf den ersten Blick ist die Morphologie zum Oligodendrogliom sehr ähnlich, aber das Fehlen von GFAP und die Immunreaktivität für pan-Zytokeratin bestätigen die epitheliale Herkunft. Wie bei malignen Tumoren zu erwarten, ist die MIB-1 Proliferationsrate erhöht. Es existiert kein ATRX-Verlust und keine IDH1-Mutation. |
A descriptive overview of various brain tumours is found here.
Molecular neurooncology
Because IDH-1 and IDH-2 mutations are found in up to 80% of astrocytomas and oligodendroglioma, IDH-1 R132H (which detects only the R132H substitution [5]) stained negative cases are sequenced for other rare mutations that include IDH1 R132C or IDH2 R172K among others. These mutations are not only useful in differential diagnosis of brain tumours but also prognostic, because tumours carrying a IDH-1 or IDH-2 mutation usually show a more favourable course than their wild-type counterparts [6].
Oligodendrogliomas show a more favourable course and therfore are treated differently than astrocytomas. A clear separation of these two entities is important, because H&E morphology is not always convincing. Succesful treatment depends on allelic losses on chromosomal arms 1p and 19q in oligodendroglioma that can be obtained by copy-number analysis or microsatellite PCR. By combining LOH (loss of heterozygosity) 1p/19q and ATRX status it is also possible to place the mixed oligoastrocytomas into the astrocytoma or oligodendroglioma group.
Day 1
Immunofluorescence
Immunofluorescence is a technique used for light microscopy with a fluorescence microscope (usually a confocal microscope). This technique uses the specificity of antibodies to their antigen to target fluorescent dyes to specific biomolecule targets within a cell, and therefore allows visualisation of the distribution of the target molecule through the sample. The typical approach uses a unlabeled first (primary) antibody that specifically binds the target molecule, and the secondary antibody, which carries the fluorophore, recognises the primary antibody and binds to it. Advantages of immunofluorescence are the usually better resolution of the signals compared with standard light-microscope stains and the possibility to combine antibodies of different species to target two or more epitopes with different fluorophores. These different signals can be merged into a single image.
Myopathology
The skeletal muscle is anchored by tendons (or by aponeuroses at a few places) to bone and is used to effect skeletal movement such as locomotion and to maintain posture. Striated or skeletal muscle only contracts voluntarily, upon influence of the central nervous system.Skeletal muscle is further divided into several subtypes:
- Type I, slow oxidative, slow twitch, or "red" muscle is dense with capillaries and is rich in mitochondria and myoglobin, giving the muscle tissue its characteristic red color. It can carry more oxygen and sustain aerobic activity.
- Type II, fast twitch muscle, has three major kinds that are, in order of increasing contractile speed.
Muscle biopsies are performed to obtain a specific diagnosis in persisting weakness or muscle pain.
References
- ↑ Taylor, CR.; Burns, J. (Jan 1974). "The demonstration of plasma cells and other immunoglobulin-containing cells in formalin-fixed, paraffin-embedded tissues using peroxidase-labelled antibody.". J Clin Pathol 27 (1): 14-20. PMID 4132252.
- ↑ Simon, R.; Sauter, G. (Oct 2003). "Tissue microarray (TMA) applications: implications for molecular medicine.". Expert Rev Mol Med 5 (26): 1-12. doi:doi:10.1017/S1462399403006781. PMID 14987401.
- ↑ Scholzen, T.; Gerdes, J. (Mar 2000). "The Ki-67 protein: from the known and the unknown.". J Cell Physiol 182 (3): 311-22. doi:10.1002/(SICI)1097-4652(200003)182:3<311::AID-JCP1>3.0.CO;2-9. PMID 10653597.
- ↑ https://en.wikipedia.org/wiki/Ki-67_%28protein%29
- ↑ Capper, D.; Zentgraf, H.; Balss, J.; Hartmann, C.; von Deimling, A. (Nov 2009). "Monoclonal antibody specific for IDH1 R132H mutation.". Acta Neuropathol 118 (5): 599-601. doi:10.1007/s00401-009-0595-z. PMID 19798509.
- ↑ Hartmann, C.; Hentschel, B.; Wick, W.; Capper, D.; Felsberg, J.; Simon, M.; Westphal, M.; Schackert, G. et al. (Dec 2010). "Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas, and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas.". Acta Neuropathol 120 (6): 707-18. doi:10.1007/s00401-010-0781-z. PMID 21088844.
Day 2
Adavanced neuropathology
Coming soon.