Difference between revisions of "Uterine cervix"
| (192 intermediate revisions by the same user not shown) | |||
| Line 6: | Line 6: | ||
=Introduction= | =Introduction= | ||
*Most cervix cancer is squamous cell carcinoma. | ==Overview== | ||
*Most cervix cancer is [[squamous cell carcinoma of the uterine cervix|squamous cell carcinoma]]. | |||
**An effective screening test to detect this is the ''Pap test'', which is dealt with in the ''[[gynecologic cytopathology]]'' article. | **An effective screening test to detect this is the ''Pap test'', which is dealt with in the ''[[gynecologic cytopathology]]'' article. | ||
*The work-up of | *The work-up of a suspicious ''Pap test'' is a ''colposcopic examination'' and biopsies, which are the topic of ''this'' article. | ||
Indications for coloposcopic exam (based on the ''ASCCP Consensus Guidelines'' of 2001):<ref name=pmid16148248>{{Cite journal | last1 = Dresang | first1 = LT. | title = Colposcopy: an evidence-based update. | journal = J Am Board Fam Pract | volume = 18 | issue = 5 | pages = 383-92 | month = | year = | doi = | PMID = 16148248 |URL = www.jabfm.org/cgi/pmidlookup?view=long&pmid=16148248 }}</ref> | |||
*[[High-grade squamous intraepithelial lesion]] ([[HSIL]]). | |||
*Repeated [[low-grade squamous intraepithelial lesion]] ([[LSIL]]). | |||
*[[Atypical squamous cells of undetermined significance]] ([[ASCUS]]) and a positive [[HPV]] test. | |||
*[[ASC-H]]. | |||
*[[Atypical glandular cells]] ([[AGC]]) not otherwise specified. | |||
*[[Adenocarcinoma in situ]] ([[AIS]]). | |||
==Colposcopic examination== | |||
*Performed by gynecologists. | |||
*Exam usually includes a search for ''acetowhite epithelium'' (AWE); this is accomplished by the application of acetic acid (to help identify lesions for biopsy). | |||
**[[cervical intraepithelial neoplasia|Neoplastic cervical lesions]] are typically white.<ref name=pmid23224202>{{Cite journal | last1 = Zonios | first1 = G. | title = Reflectance model for acetowhite epithelium. | journal = J Biomed Opt | volume = 17 | issue = 8 | pages = 87003-1 | month = Aug | year = 2012 | doi = 10.1117/1.JBO.17.8.087003 | PMID = 23224202 }}</ref> | |||
**[[Squamous metaplasia of the uterine cervix|Squamous metaplasia]] is also white.<ref name=pmid19256708>{{Cite journal | last1 = Li | first1 = W. | last2 = Venkataraman | first2 = S. | last3 = Gustafsson | first3 = U. | last4 = Oyama | first4 = JC. | last5 = Ferris | first5 = DG. | last6 = Lieberman | first6 = RW. | title = Using acetowhite opacity index for detecting cervical intraepithelial neoplasia. | journal = J Biomed Opt | volume = 14 | issue = 1 | pages = 014020 | month = | year = | doi = 10.1117/1.3079810 | PMID = 19256708 }}</ref> | |||
*Cervical ectropian (AKA cervical eversion, AKA ectropian) = endocervical epithelium at external os, considered benign, grossly has a granulation tissue-like appearance.<ref name=pmid21270291>{{Cite journal | last1 = Casey | first1 = PM. | last2 = Long | first2 = ME. | last3 = Marnach | first3 = ML. | title = Abnormal cervical appearance: what to do, when to worry? | journal = Mayo Clin Proc | volume = 86 | issue = 2 | pages = 147-50; quiz 151 | month = Feb | year = 2011 | doi = 10.4065/mcp.2010.0512 | PMID = 21270291 | PMC = 3031439 }}</ref> | |||
==Cervical specimens== | ==Cervical specimens== | ||
Cytology | ===Cytology=== | ||
* Pap test - see ''[[gynecologic cytopathology]]''. | * Pap test - see ''[[gynecologic cytopathology]]''. | ||
===Biopsies=== | |||
The types of biopsies that are done are: | The types of biopsies that are done are: | ||
# Cervical biopsies - prompted by abnormal Pap test, e.g. [[HSIL]], to look for [[squamous cell carcinoma of the uterine cervix]]. | # Cervical biopsies - prompted by abnormal Pap test, e.g. [[HSIL]], to look for [[squamous cell carcinoma of the uterine cervix]]. | ||
# Endocervical curettage (ECC) - to work-up columnar dysplasia, e.g. [[endocervical adenocarcinoma]]/[[endometrial adenocarcinoma]]. | # Endocervical curettage (ECC) - to work-up columnar dysplasia, e.g. [[endocervical adenocarcinoma]]/[[endometrial adenocarcinoma]]. | ||
Surgical specimens | ===Surgical specimens=== | ||
# [[Loop electrosurgical excision procedure]] (LEEP). | # [[Loop electrosurgical excision procedure]] (LEEP). | ||
#* [[AKA]] large loop excision of the transformation zone (LLETZ).<ref>{{Cite journal | last1 = Kenwright | first1 = D. | last2 = Braam | first2 = G. | last3 = Maharaj | first3 = D. | last4 = Langdana | first4 = F. | title = Multiple levels on LLETZ biopsies do not contribute to patient management. | journal = Pathology | volume = 44 | issue = 1 | pages = 7-10 | month = Jan | year = 2012 | doi = 10.1097/PAT.0b013e32834d7b5d | PMID = 22173237 }}</ref><ref>URL: [http://www.webmd.com/cancer/cervical-cancer/loop-electrosurgical-excision-procedure-leep-for-abnormal-cervical-cell-changes http://www.webmd.com/cancer/cervical-cancer/loop-electrosurgical-excision-procedure-leep-for-abnormal-cervical-cell-changes]. Accessed on: 20 March 2014.</ref> | |||
# Radical trachelectomy - removal of the uterine cervix and parametria, preserves fertility. | # Radical trachelectomy - removal of the uterine cervix and parametria, preserves fertility. | ||
# Radical hysterectomy - advanced cervical carcinoma (Stage IA2 and Stage IB1), recurrent carcinoma.<ref name=pmid20871657>{{Cite journal | last1 = Ware | first1 = RA. | last2 = van Nagell | first2 = JR. | title = Radical hysterectomy with pelvic lymphadenectomy: indications, technique, and complications. | journal = Obstet Gynecol Int | volume = 2010 | issue = | pages = | month = | year = 2010 | doi = 10.1155/2010/587610 | PMID = 20871657 }}</ref> | # Radical hysterectomy - advanced cervical carcinoma (Stage IA2 and Stage IB1), recurrent carcinoma.<ref name=pmid20871657>{{Cite journal | last1 = Ware | first1 = RA. | last2 = van Nagell | first2 = JR. | title = Radical hysterectomy with pelvic lymphadenectomy: indications, technique, and complications. | journal = Obstet Gynecol Int | volume = 2010 | issue = | pages = | month = | year = 2010 | doi = 10.1155/2010/587610 | PMID = 20871657 }}</ref> | ||
Other | ===Other=== | ||
*Total abdominal hysterectomy - for non-cervical pathology, e.g. [[uterine leiomyoma]]s, [[uterine adenomyosis]]. | *Total abdominal hysterectomy - for non-cervical pathology, e.g. [[uterine leiomyoma]]s, [[uterine adenomyosis]]. | ||
*Radical hysterectomy - for [[endometrial carcinoma]] with endocervical involvement. | *Radical hysterectomy - for [[endometrial carcinoma]] with endocervical involvement. | ||
=Normal histology= | =Normal histology= | ||
Features: | |||
*The uterine cervix consists of non-keratinized squamous epithelium and simple columnar epithelium. | *The uterine cervix consists of non-keratinized squamous epithelium and simple columnar epithelium. | ||
*The area of overlap (between squamous & columnar) is known as the "transformation zone".<ref>URL: [http://www.med-ed.virginia.edu/Courses/path/gyn/cervix1.cfm http://www.med-ed.virginia.edu/Courses/path/gyn/cervix1.cfm]. Accessed on: 12 May 2010.</ref> | *The area of overlap (between squamous & columnar) is known as the "transformation zone".<ref>URL: [http://www.med-ed.virginia.edu/Courses/path/gyn/cervix1.cfm http://www.med-ed.virginia.edu/Courses/path/gyn/cervix1.cfm]. Accessed on: 12 May 2010.</ref> | ||
**Also known as "transition zone". | **Also known as "transition zone". | ||
Notes: | |||
*Considered from the perspective of histology: | |||
**The squamous component is referred to as the ''exocervix'' (or ''ectocervix''<ref>URL: [http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-what-is-cervical-cancer http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-what-is-cervical-cancer]. Accessed on: 27 January 2014.</ref>). | |||
**The simple columnar (or glandular) component is referred to as the ''endocervix''. | |||
Images: | |||
*[http://www.proteinatlas.org/dictionary/normal/cervix,+uterine+1 Normal cervix (proteinatlas.org)]. | |||
==Negative LEEP== | |||
{{Main|LEEP}} | |||
==Transformation zone - biopsy== | |||
===Microscopic=== | |||
Features: | |||
*Small round cells. | |||
*Usually no halos. | |||
**May be seen in pseudokoilocytes. | |||
*No nuclear membrane irregularities. | |||
*No nuclear hyperchromasia. | |||
===Images=== | |||
<gallery> | |||
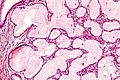
Image: Uterine cervix -- intermed mag.jpg | [[NILM]] with pseudokoilocytes - intermed. mag. (WC) | |||
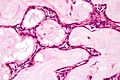
Image: Uterine cervix -- high mag.jpg | NILM with pseudokoilocytes - high mag. (WC) | |||
Image: Uterine cervix -- very high mag.jpg | NILM with pseudokoilocytes - very high mag. (WC) | |||
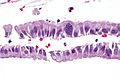
Image: Exocervix_--_high_mag.jpg | Benign stripped exocervix - high mag. (WC) | |||
</gallery> | |||
www: | |||
*[http://www.flickr.com/photos/euthman/2797778604/in/photostream/ Normal cervix (flickr.com/euthman)]. | |||
*[http://www.flickr.com/photos/euthman/2796932803/in/photostream/ CIN I versus normal (flickr.com/euthman)]. | |||
===Sign out=== | |||
<pre> | |||
UTERINE CERVIX, BIOPSY: | |||
- TRANSFORMATION ZONE WITHOUT APPARENT PATHOLOGY. | |||
- NEGATIVE FOR DYSPLASIA. | |||
</pre> | |||
<pre> | |||
UTERINE CERVIX, BIOPSY: | |||
- SQUAMOUS MUCOSA WITHOUT APPARENT PATHOLOGY. | |||
- STRIPPED ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY. | |||
- NEGATIVE FOR DYSPLASIA. | |||
</pre> | |||
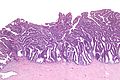
==Endocervical glands== | ==Endocervical glands== | ||
===Microscopic=== | |||
Features: | |||
Cervical glands normally have round nuclei and vaguely resemble the colonic mucosa. | Cervical glands normally have round nuclei and vaguely resemble the colonic mucosa. | ||
Notes: | |||
*If the nuclei are columnar think cancer! This is like in the colon-- columnar nuclei = badness. | *If the nuclei are columnar think cancer! This is like in the colon-- columnar nuclei = badness. | ||
**Memory device: The Cs (Cervix & Colon) are similar. | |||
*Endocervical epithelium (ECE) has a morphology similar to the epithelium of [[secretory phase endometrium]] (SPE): | |||
**ECE - grey foamy appearing cytoplasm. | |||
**SPE - eosinophilic cytoplasm. | |||
***Most useful feature to differentiate ECE and SPE is the accompanying stroma. | |||
===Sign out=== | |||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- ENDOCERVICAL MUCOSA AND STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. | |||
</pre> | |||
== | ====Inflamed with squamous epithelium==== | ||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- BENIGN STRIPPED ENDOCERVICAL EPITHELIUM AND SCANT INFLAMED ENDOCERVICAL MUCOSA. | |||
- VERY SCANT SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. | |||
</pre> | |||
====Squamous epithelium present==== | |||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- ENDOCERVICAL MUCOSA WITHIN NORMAL LIMITS. | |||
- SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. | |||
</pre> | |||
====Endometrium present==== | |||
<pre> | <pre> | ||
UTERINE ENDOCERVIX, CURETTAGE: | UTERINE ENDOCERVIX, CURETTAGE: | ||
| Line 45: | Line 137: | ||
</pre> | </pre> | ||
====Inflamed==== | |||
<pre> | <pre> | ||
UTERINE ENDOCERVIX, CURETTAGE: | UTERINE ENDOCERVIX, CURETTAGE: | ||
- ENDOCERVICAL MUCOSA | - INFLAMED ENDOCERVICAL MUCOSA. | ||
- SQUAMOUS EPITHELIUM | - REACTIVE SQUAMOUS EPITHELIUM. | ||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | </pre> | ||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- BENIGN INFLAMED ENDOCERVICAL MUCOSA. | |||
- STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS. | |||
</pre> | |||
====No stroma present==== | |||
====No stroma==== | |||
<pre> | <pre> | ||
UTERINE ENDOCERVIX, CURETTAGE: | UTERINE ENDOCERVIX, CURETTAGE: | ||
- STRIPPED ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY. | - STRIPPED ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY. | ||
</pre> | </pre> | ||
====Limited tissue==== | |||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- ONE MINUTE FRAGMENT OF ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY, | |||
SEE COMMENT. | |||
- VERY SCANT SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. | |||
COMMENT: | |||
The assessment is severely limited by the small amount of tissue. A re-biopsy | |||
should be considered within the clinical context. | |||
</pre> | |||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- ONE MINUTE FRAGMENT OF ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY, | |||
SEE COMMENT. | |||
- VERY SCANT SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. | |||
COMMENT: | |||
The assessment is severely limited by the small amount of tissue. Clinical correlation is | |||
suggested. | |||
</pre> | |||
<pre> | |||
UTERINE ENDOCERVIX, CURETTAGE: | |||
- BENIGN SQUAMOUS EPITHELIUM WITH METAPLASTIC CHANGE. | |||
- VERY SCANT BENIGN ENDOCERVICAL EPITHELIUM, SUBOPTIMAL SAMPLING. | |||
</pre> | |||
<pre> | |||
UTERINE CERVIX, BIOPSY: | |||
- MINUTE FRAGMENTS OF SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. | |||
- SCANT MUCOUS AND INFLAMMATORY CELLS. | |||
- SEE COMMENT. | |||
COMMENT: | |||
The assessment is severely limited by the small amount of tissue. A re-biopsy should be | |||
considered within the clinical context. | |||
</pre> | |||
=Inadequate biopsy= | |||
*Unfortunately, inadequate biopsies are common. | |||
==Endocervix== | |||
===Sign out=== | |||
====No endocervical epithelium==== | ====No endocervical epithelium==== | ||
<pre> | <pre> | ||
| Line 92: | Line 231: | ||
COMMENT: | COMMENT: | ||
No tissue identified on microscopy. No tissue is seen on inspection of the | No tissue identified on microscopy. No tissue is seen on inspection of the paraffin block. | ||
</pre> | </pre> | ||
| Line 101: | Line 240: | ||
#Identify possible endocervical lesions. | #Identify possible endocervical lesions. | ||
=Benign | ==Benign entities of the cervix== | ||
The cervix is ''MANTLED'': | |||
* Mullerian papilloma/Mesonephric hyperplasia/[[Microglandular hyperplasia]]. | |||
* [[Arias Stella reaction]]. | |||
* [[Nabothian cyst]]. | |||
* [[Tunnel cluster]]/Tuboendometrioid metaplasia. | |||
* Lobular endocervical glandular hyperplasia. | |||
* [[Endocervical polyp]]/Endocervicosis/[[Endometriosis]]/Ectopic prostatic tissue. | |||
* Diffuse laminar endocervical hyperplasia. | |||
=Benign= | |||
==Nabothian cyst== | ==Nabothian cyst== | ||
===General=== | ===General=== | ||
| Line 107: | Line 256: | ||
*Common. | *Common. | ||
===Gross=== | |||
*Bump. | |||
*Pale colour. | |||
DDx - clinical: | |||
*[[Benign endocervical polyp]]. | |||
====Image==== | |||
<gallery> | |||
Image:Ovula_nabothi.jpg | Nabothian cyst. (WC/euthman) | |||
</gallery> | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
| Line 122: | Line 282: | ||
Image: | Image: | ||
*[http://www.gfmer.ch/selected_images_v2/detail_list.php?cat1=4&cat2=23&cat3=130&cat4=5&stype=n Nabothian cyst (gfmer.ch)]. | *[http://www.gfmer.ch/selected_images_v2/detail_list.php?cat1=4&cat2=23&cat3=130&cat4=5&stype=n Nabothian cyst (gfmer.ch)]. | ||
===Sign out=== | |||
<pre> | |||
CERVICAL POLYP, REMOVAL: | |||
- BENIGN POLYPOID FRAGMENT OF EXOCERVICAL MUCOSA WITH NABOTHIAN CYSTS AND | |||
BENIGN ENDOCERVICAL EPITHELIUM. | |||
</pre> | |||
<pre> | |||
POLYPOID LESION ("CERVICAL POLYP"), EXCISION: | |||
- POLYPOID NABOTHIAN CYST. | |||
</pre> | |||
==Tunnel cluster== | ==Tunnel cluster== | ||
| Line 127: | Line 299: | ||
*Benign.<ref name=pmid12352183>{{Cite journal | last1 = Nucci | first1 = MR. | title = Symposium part III: tumor-like glandular lesions of the uterine cervix. | journal = Int J Gynecol Pathol | volume = 21 | issue = 4 | pages = 347-59 | month = Oct | year = 2002 | doi = | PMID = 12352183 }}</ref> | *Benign.<ref name=pmid12352183>{{Cite journal | last1 = Nucci | first1 = MR. | title = Symposium part III: tumor-like glandular lesions of the uterine cervix. | journal = Int J Gynecol Pathol | volume = 21 | issue = 4 | pages = 347-59 | month = Oct | year = 2002 | doi = | PMID = 12352183 }}</ref> | ||
*Not the same as ''[[microglandular hyperplasia]]''.<ref name=pmid10757337>{{Cite journal | last1 = Zaino | first1 = RJ. | title = Glandular lesions of the uterine cervix. | journal = Mod Pathol | volume = 13 | issue = 3 | pages = 261-74 | month = Mar | year = 2000 | doi = 10.1038/modpathol.3880047 | PMID = 10757337 | URL = http://www.nature.com/modpathol/journal/v13/n3/full/3880047a.html }}</ref> | *Not the same as ''[[microglandular hyperplasia]]''.<ref name=pmid10757337>{{Cite journal | last1 = Zaino | first1 = RJ. | title = Glandular lesions of the uterine cervix. | journal = Mod Pathol | volume = 13 | issue = 3 | pages = 261-74 | month = Mar | year = 2000 | doi = 10.1038/modpathol.3880047 | PMID = 10757337 | URL = http://www.nature.com/modpathol/journal/v13/n3/full/3880047a.html }}</ref> | ||
*Considered a special type of [[nabothian cyst]].<ref name=pmid12640157>{{Cite journal | last1 = Okamoto | first1 = Y. | last2 = Tanaka | first2 = YO. | last3 = Nishida | first3 = M. | last4 = Tsunoda | first4 = H. | last5 = Yoshikawa | first5 = H. | last6 = Itai | first6 = Y. | title = MR imaging of the uterine cervix: imaging-pathologic correlation. | journal = Radiographics | volume = 23 | issue = 2 | pages = 425-45; quiz 534-5 | month = | year = | doi = | PMID = 12640157 | URL = http://radiographics.rsna.info/content/23/2/425.full }}</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 141: | Line 314: | ||
#Important only as one could possibly mistake it as ''[[minimal deviation adenocarcinoma of the uterine cervix|minimal deviation adenocarcinoma]]'', [[AKA]] ''adenoma malignum''.<ref name=pmid2764221>{{cite journal |author=Gilks CB, Young RH, Aguirre P, DeLellis RA, Scully RE |title=Adenoma malignum (minimal deviation adenocarcinoma) of the uterine cervix. A clinicopathological and immunohistochemical analysis of 26 cases |journal=Am. J. Surg. Pathol. |volume=13 |issue=9 |pages=717–29 |year=1989 |month=September |pmid=2764221 |doi= |url=}}</ref> | #Important only as one could possibly mistake it as ''[[minimal deviation adenocarcinoma of the uterine cervix|minimal deviation adenocarcinoma]]'', [[AKA]] ''adenoma malignum''.<ref name=pmid2764221>{{cite journal |author=Gilks CB, Young RH, Aguirre P, DeLellis RA, Scully RE |title=Adenoma malignum (minimal deviation adenocarcinoma) of the uterine cervix. A clinicopathological and immunohistochemical analysis of 26 cases |journal=Am. J. Surg. Pathol. |volume=13 |issue=9 |pages=717–29 |year=1989 |month=September |pmid=2764221 |doi= |url=}}</ref> | ||
Images: | ====Images==== | ||
<gallery> | |||
Image:Tunnel_cluster_-_very_low_mag.jpg | Tunnel cluster - very low mag. (WC) | |||
Image:Tunnel_cluster_-_low_mag.jpg | Tunnel cluster - low mag. (WC) | |||
Image:Tunnel_cluster_-_intermed_mag.jpg | Tunnel cluster - intermed. mag. (WC) | |||
Image:Tunnel_cluster_-_high_mag.jpg | Tunnel cluster - high mag. (WC) | |||
Image:Tunnel_cluster_-_very_high_mag.jpg | Tunnel cluster - very high mag. (WC) | |||
</gallery> | |||
[[www]]: | |||
*[http://surgpath4u.com/caseviewer.php?case_no=477 Tunnel cluster (surgpath4u.com)]. | |||
*[http://www.ajronline.org/content/195/2/517/F30.expansion Tunnel cluster (ajronline.org)]. | |||
==Microglandular hyperplasia== | ==Microglandular hyperplasia== | ||
| Line 153: | Line 330: | ||
*Abbreviated ''MGH''. | *Abbreviated ''MGH''. | ||
*[[AKA]] ''microglandular change''. | *[[AKA]] ''microglandular change''. | ||
{{Main|Microglandular hyperplasia}} | |||
==Wolffian duct hyperplasia== | ==Wolffian duct hyperplasia== | ||
| Line 194: | Line 340: | ||
*Abundant small tubules with a simple cuboidal epithelium. | *Abundant small tubules with a simple cuboidal epithelium. | ||
*Round small bland nucleus. | *Round small bland nucleus. | ||
DDx: | |||
*[[Wolffian duct remnant]]. | |||
===Stains=== | ===Stains=== | ||
| Line 199: | Line 348: | ||
==Squamous metaplasia of the uterine cervix== | ==Squamous metaplasia of the uterine cervix== | ||
*Abbreviated ''SMC''. | |||
{{Main|Squamous metaplasia of the uterine cervix}} | |||
==Reactive squamous epithelium of the uterine cervix== | |||
*[[AKA]] ''reactive squamous epithelium''. | |||
*[[AKA]] ''reactive changes''. | |||
===General=== | ===General=== | ||
* | *Common. | ||
*Individuals with persistent inflammation on [[Pap test]] may have occult [[SIL]].<ref name=pmid21768670>{{Cite journal | last1 = Bhutia | first1 = K. | last2 = Puri | first2 = M. | last3 = Gami | first3 = N. | last4 = Aggarwal | first4 = K. | last5 = Trivedi | first5 = SS. | title = Persistent inflammation on Pap smear: does it warrant evaluation? | journal = Indian J Cancer | volume = 48 | issue = 2 | pages = 220-2 | month = | year = | doi = 10.4103/0019-509X.82901 | PMID = 21768670 }}</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
#Inflammation - '''key feature'''. | |||
* | #*Lymphocytes. | ||
* | #*Plasma cells. | ||
#Mild nuclear enlargement. † | |||
#Nucleoli - '''important'''. | |||
Note: | |||
* | *† Normal squamous cell nuclei are approximately 8 μm.<ref>URL: [http://www.curran.pwp.blueyonder.co.uk/cytology.htm http://www.curran.pwp.blueyonder.co.uk/cytology.htm]. Accessed on: 5 November 2012.</ref> | ||
**Mild enlargement ~ 2-3x normal. | |||
**CIN I nuclei are ~ 3x normal (24 μm). | |||
* | |||
DDx: | DDx: | ||
*[[CIN | *[[Cervical intraepithelial neoplasia I]]. | ||
*[[ | *[[CIN II|Cervical intraepithelial neoplasia II]]. | ||
*[[NILM]]. | |||
===IHC=== | ===IHC=== | ||
*p16 | *p16 -ve. | ||
===Sign out=== | |||
<pre> | |||
UTERINE CERVIX, BIOPSY: | |||
- REACTIVE SQUAMOUS EPITHELIUM. | |||
- BENIGN ENDOCERVICAL GLANDS. | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
<pre> | |||
COMMENT: | |||
The squamous epithelium is negative for p16 staining. Ki-67 staining is predominantly in | |||
the lower third of the epithelium. | |||
</pre> | |||
==Tubal metaplasia of the uterine cervix== | |||
*[[AKA]] ''tubal metaplasia'', abbreviated ''TM''. | |||
===General=== | ===General=== | ||
* | *Benign. | ||
*Mimics the appearance of [[Endocervical adenocarcinoma in situ|AIS]] - especially at low power. | |||
===Microscopic=== | |||
* | Features - like the [[fallopian tube]]: | ||
* | *Nuclear crowding vis-à-vis benign endocervical epithelium (low power). | ||
* | *Mixed cell population (high power): | ||
**Peg cells - "tall" and "skinny". | |||
***Columnar/golf tee-like appearance. | |||
**Ciliated cells - cilia, pale cytoplasm, round central nucleus. | |||
**Secretory cells - non-ciliated, basophilic cytoplasm, round small basal nuclei. | |||
DDx: | |||
* | *[[Endocervical adenocarcinoma in situ]]. | ||
Image: | |||
*[ | *[http://www.nature.com/modpathol/journal/v13/n3/fig_tab/3880047f17.html Tubal metaplasia (nature.com)]. | ||
[[ | ===IHC=== | ||
* | Features:<ref name=pmid8803599>{{Cite journal | last1 = Marques | first1 = T. | last2 = Andrade | first2 = LA. | last3 = Vassallo | first3 = J. | title = Endocervical tubal metaplasia and adenocarcinoma in situ: role of immunohistochemistry for carcinoembryonic antigen and vimentin in differential diagnosis. | journal = Histopathology | volume = 28 | issue = 6 | pages = 549-50 | month = Jun | year = 1996 | doi = | PMID = 8803599 }}</ref> | ||
*[[Vimentin]] +ve. | |||
*CEA -ve/+ve. | |||
*p16 -ve.{{fact}} | |||
==Atrophy of the uterine cervix== | |||
* | *[[AKA]] ''cervical atrophy''. | ||
* | *[[AKA]] ''atrophy of the cervix''. | ||
*[[AKA]] ''cervix with atrophic changes''. | |||
{{Main|Uterine cervix with atrophic changes}} | |||
==Radiation changes of the endocervical epithelium== | |||
{{Main|Radiation changes}} | |||
{{Main|Radiation changes in cervical cytology}} | |||
===General=== | |||
*Uncommon. | |||
*Clinical history: radiation treatment for cervical carcinoma.<ref name=pmid2209348/> | |||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name=pmid2209348>{{Cite journal | last1 = Frierson | first1 = HF. | last2 = Covell | first2 = JL. | last3 = Andersen | first3 = WA. | title = Radiation changes in endocervical cells in brush specimens. | journal = Diagn Cytopathol | volume = 6 | issue = 4 | pages = 243-7 | month = | year = 1990 | doi = | PMID = 2209348 }}</ref> | |||
Features | *Nuclear enlargement with a normal [[NC ratio]]. | ||
*+/-Coarse chromatin. | |||
*+/-Nucleoli. | |||
*+/-Multinucleation - very common. | |||
*Histiocytes - common. | |||
==Reactive endocervical cells== | |||
===General=== | |||
* | *Benign. | ||
=== | ===Microscopic=== | ||
Features | Features: | ||
* | *Mild nuclear enlargement. | ||
* | *+/-Multinucleation.<ref>URL: [http://www.surgpath4u.com/caseviewer.php?case_no=229 http://www.surgpath4u.com/caseviewer.php?case_no=229]. Accessed on: 2 January 2014.</ref> | ||
= | |||
Notes: | Notes: | ||
DDx of multinucleated endocervical cells: | |||
*[[HSV]].<ref name=pmid4352382>{{Cite journal | last1 = Naib | first1 = ZM. | last2 = Nahmias | first2 = AJ. | last3 = Josey | first3 = WE. | last4 = Zaki | first4 = SA. | title = Relation of cytohistopathology of genital herpesvirus infection to cervical anaplasia. | journal = Cancer Res | volume = 33 | issue = 6 | pages = 1452-63 | month = Jun | year = 1973 | doi = | PMID = 4352382 | URL = http://cancerres.aacrjournals.org/cgi/pmidlookup?view=long&pmid=4352382 }}</ref> | |||
*Benign endocervical cells. | |||
</ref> | |||
==== | ====Images==== | ||
<gallery> | |||
Image: Endocervical epithelium with multinucleation -- high mag.jpg | Multinucleated endocervix - high mag. | |||
Image: Endocervical epithelium with multinucleation -- very high mag.jpg | Multinucleated endocervix - very high mag. | |||
Image: Endocervical epithelium with multinucleation -- extremely high mag.jpg | Multinucleated endocervix - extremely high mag. | |||
</gallery> | |||
www: | |||
*[http://www.surgpath4u.com/caseviewer.php?case_no=229 Reactive endocervical cells (surgpath4u.com)]. | |||
=Non-invasive= | |||
==Cervical intraepithelial neoplasia== | |||
*Previously known as ''cervical intraepithelial neoplasia'' and ''cervical dysplasia''. | |||
{{Main|Squamous intraepithelial lesion of the uterine cervix}} | |||
* | |||
==Endocervical adenocarcinoma in situ== | ==Endocervical adenocarcinoma in situ== | ||
:''For the cytology see [[Gynecologic cytopathology#Endocervical adenocarcinoma in situ]]'' | :''For the cytology see [[Gynecologic cytopathology#Endocervical adenocarcinoma in situ]]'' | ||
*[[AKA]] ''adenocarcinoma in situ'', abbreviated ''AIS''. | *[[AKA]] ''adenocarcinoma in situ'', abbreviated ''AIS''. | ||
{{Main|Endocervical adenocarcinoma in situ}} | |||
=Cancer= | =Cancer= | ||
| Line 379: | Line 479: | ||
{{Main|Squamous cell carcinoma}} | {{Main|Squamous cell carcinoma}} | ||
*[[AKA]] ''cervical squamous cell carcinoma''. | *[[AKA]] ''cervical squamous cell carcinoma''. | ||
{{Main|Squamous cell carcinoma of the uterine cervix}} | |||
==Adenocarcinoma of the uterine cervix== | ==Adenocarcinoma of the uterine cervix== | ||
*[[AKA]] ''endocervical adenocarcinoma''. | *[[AKA]] ''endocervical adenocarcinoma''. | ||
*[[AKA]] ''cervical adenocarcinoma''. | *[[AKA]] ''cervical adenocarcinoma''. | ||
{{Main|Adenocarcinoma of the uterine cervix}} | |||
=Uncommon non-invasive= | =Uncommon non-invasive= | ||
==Stratified mucin-producing intraepithelial lesions of the cervix== | ==Stratified mucin-producing intraepithelial lesions of the cervix== | ||
*Abbreviated ''SMILE'' ('''S'''tratified '''M'''ucin-producing '''I'''ntraepithelial '''LE'''sion). | *Abbreviated ''SMILE'' ('''S'''tratified '''M'''ucin-producing '''I'''ntraepithelial '''LE'''sion). | ||
{{Main|Stratified mucin-producing intraepithelial lesion of the cervix}} | |||
=Uncommon types of cervical cancer= | =Uncommon types of cervical cancer= | ||
There are a number of uncommon type of cervical cancer. | There are a number of uncommon type of cervical cancer. | ||
== | ==Serous carcinoma of the uterine cervix== | ||
===General=== | ===General=== | ||
* | *Poor prognosis.<ref name=pmid21876330>{{Cite journal | last1 = Togami | first1 = S. | last2 = Kasamatsu | first2 = T. | last3 = Sasajima | first3 = Y. | last4 = Onda | first4 = T. | last5 = Ishikawa | first5 = M. | last6 = Ikeda | first6 = S. | last7 = Kato | first7 = T. | last8 = Tsuda | first8 = H. | title = Serous adenocarcinoma of the uterine cervix: a clinicopathological study of 12 cases and a review of the literature. | journal = Gynecol Obstet Invest | volume = 73 | issue = 1 | pages = 26-31 | month = | year = 2012 | doi = 10.1159/000329319 | PMID = 21876330 }}</ref> | ||
*Extremely rare. | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
*Like [[ | *Like other [[serous carcinoma]]s. | ||
==Adenosquamous carcinoma of the uterine cervix== | |||
{{Main|Adenosquamous carcinoma of the uterine cervix}} | |||
==Clear cell carcinoma of the uterine cervix== | |||
{{Main|Clear cell carcinoma of the uterine cervix}} | |||
==Small cell carcinoma of the cervix== | ==Small cell carcinoma of the cervix== | ||
| Line 530: | Line 529: | ||
*Nests of cells with basaloid rim and squamoid center. | *Nests of cells with basaloid rim and squamoid center. | ||
**Basaloid cells look benign. | **Basaloid cells look benign. | ||
DDx: | |||
*Ectopic [[prostate gland]]. | |||
Image: | Image: | ||
| Line 535: | Line 537: | ||
==Glassy cell carcinoma== | ==Glassy cell carcinoma== | ||
{{Main|Glassy cell carcinoma}} | |||
==Villoglandular adenocarcinoma of the cervix== | ==Villoglandular adenocarcinoma of the cervix== | ||
| Line 582: | Line 558: | ||
*Serous carcinoma of the cervix. | *Serous carcinoma of the cervix. | ||
Images | ====Images==== | ||
www: | |||
*[http://www.webpathology.com/image.asp?n=11&Case=560 VGA (webpathology.com)]. | |||
<gallery> | |||
Image:Villoglandular_adenocarcinoma_-_very_low_mag.jpg | VGA - very low mag. (WC) | |||
Image:Villoglandular_adenocarcinoma_-_intermed_mag.jpg | VGA - intermed. mag. (WC) | |||
Image:Villoglandular_adenocarcinoma_-_very_high_mag.jpg | VGA - very high mag. (WC) | |||
</gallery> | |||
==Mucoepidermoid carcinoma of the uterine cervix== | ==Mucoepidermoid carcinoma of the uterine cervix== | ||
| Line 622: | Line 599: | ||
==Mesonephric adenocarcinoma== | ==Mesonephric adenocarcinoma== | ||
{{Main|Mesonephric adenocarcinoma}} | |||
==Minimal deviation adenocarcinoma of the uterine cervix== | ==Minimal deviation adenocarcinoma of the uterine cervix== | ||
*[[AKA]] ''adenoma malignum''. | *[[AKA]] ''adenoma malignum''. | ||
*[[AKA]] ''minimal deviation adenocarcinoma'', abbreviated ''MDA''. | *[[AKA]] ''minimal deviation adenocarcinoma'', abbreviated ''MDA''. | ||
{{Main|Minimal deviation adenocarcinoma of the uterine cervix}} | |||
=See also= | =See also= | ||
| Line 687: | Line 616: | ||
=External links= | =External links= | ||
*[http://www. | *[http://www.medecine.ups-tlse.fr/dcem1/histologie/courtade/CINtec.pdf Interpretation altas for p16 staining (ups-tlse.fr)]. | ||
*[http://www.glowm.com/section_view/heading/Pathology%20of%20Cervical%20Carcinoma/item/230#26011 Cervical carcinoma (glowm.com)]. | |||
*[http://www.obgyn.net/gynecological-oncology/electrosurgery-cervical-intraepithelial-neoplasia Treatments for CIN (obgyn.net)]. | |||
[[Category:Gynecologic pathology]] | [[Category:Gynecologic pathology]] | ||
Latest revision as of 18:31, 17 November 2021
The uterine cervix, also simply cervix, is the gateway to the uterine corpus. It is not infrequently afflicted by cancer -- squamous cell carcinoma. Prior to routine Pap tests it was a leading cause of cancer death in women in the Western world.
Polyps associated with the cervix are discussed the cervical polyp article.
Cytopathology of the uterine cervix is dealt with in the gynecologic cytopathology article.
Introduction
Overview
- Most cervix cancer is squamous cell carcinoma.
- An effective screening test to detect this is the Pap test, which is dealt with in the gynecologic cytopathology article.
- The work-up of a suspicious Pap test is a colposcopic examination and biopsies, which are the topic of this article.
Indications for coloposcopic exam (based on the ASCCP Consensus Guidelines of 2001):[1]
- High-grade squamous intraepithelial lesion (HSIL).
- Repeated low-grade squamous intraepithelial lesion (LSIL).
- Atypical squamous cells of undetermined significance (ASCUS) and a positive HPV test.
- ASC-H.
- Atypical glandular cells (AGC) not otherwise specified.
- Adenocarcinoma in situ (AIS).
Colposcopic examination
- Performed by gynecologists.
- Exam usually includes a search for acetowhite epithelium (AWE); this is accomplished by the application of acetic acid (to help identify lesions for biopsy).
- Neoplastic cervical lesions are typically white.[2]
- Squamous metaplasia is also white.[3]
- Cervical ectropian (AKA cervical eversion, AKA ectropian) = endocervical epithelium at external os, considered benign, grossly has a granulation tissue-like appearance.[4]
Cervical specimens
Cytology
- Pap test - see gynecologic cytopathology.
Biopsies
The types of biopsies that are done are:
- Cervical biopsies - prompted by abnormal Pap test, e.g. HSIL, to look for squamous cell carcinoma of the uterine cervix.
- Endocervical curettage (ECC) - to work-up columnar dysplasia, e.g. endocervical adenocarcinoma/endometrial adenocarcinoma.
Surgical specimens
- Loop electrosurgical excision procedure (LEEP).
- Radical trachelectomy - removal of the uterine cervix and parametria, preserves fertility.
- Radical hysterectomy - advanced cervical carcinoma (Stage IA2 and Stage IB1), recurrent carcinoma.[7]
Other
- Total abdominal hysterectomy - for non-cervical pathology, e.g. uterine leiomyomas, uterine adenomyosis.
- Radical hysterectomy - for endometrial carcinoma with endocervical involvement.
Normal histology
Features:
- The uterine cervix consists of non-keratinized squamous epithelium and simple columnar epithelium.
- The area of overlap (between squamous & columnar) is known as the "transformation zone".[8]
- Also known as "transition zone".
Notes:
- Considered from the perspective of histology:
- The squamous component is referred to as the exocervix (or ectocervix[9]).
- The simple columnar (or glandular) component is referred to as the endocervix.
Images:
Negative LEEP
Transformation zone - biopsy
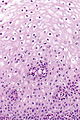
Microscopic
Features:
- Small round cells.
- Usually no halos.
- May be seen in pseudokoilocytes.
- No nuclear membrane irregularities.
- No nuclear hyperchromasia.
Images
NILM with pseudokoilocytes - intermed. mag. (WC)
www:
Sign out
UTERINE CERVIX, BIOPSY: - TRANSFORMATION ZONE WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR DYSPLASIA.
UTERINE CERVIX, BIOPSY: - SQUAMOUS MUCOSA WITHOUT APPARENT PATHOLOGY. - STRIPPED ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR DYSPLASIA.
Endocervical glands
Microscopic
Features: Cervical glands normally have round nuclei and vaguely resemble the colonic mucosa.
Notes:
- If the nuclei are columnar think cancer! This is like in the colon-- columnar nuclei = badness.
- Memory device: The Cs (Cervix & Colon) are similar.
- Endocervical epithelium (ECE) has a morphology similar to the epithelium of secretory phase endometrium (SPE):
- ECE - grey foamy appearing cytoplasm.
- SPE - eosinophilic cytoplasm.
- Most useful feature to differentiate ECE and SPE is the accompanying stroma.
Sign out
UTERINE ENDOCERVIX, CURETTAGE: - ENDOCERVICAL MUCOSA AND STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS.
Inflamed with squamous epithelium
UTERINE ENDOCERVIX, CURETTAGE: - BENIGN STRIPPED ENDOCERVICAL EPITHELIUM AND SCANT INFLAMED ENDOCERVICAL MUCOSA. - VERY SCANT SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY.
Squamous epithelium present
UTERINE ENDOCERVIX, CURETTAGE: - ENDOCERVICAL MUCOSA WITHIN NORMAL LIMITS. - SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY.
Endometrium present
UTERINE ENDOCERVIX, CURETTAGE: - ENDOCERVICAL MUCOSA WITHIN NORMAL LIMITS. - SCANT NON-PROLIFERATIVE ENDOMETRIUM.
Inflamed
UTERINE ENDOCERVIX, CURETTAGE: - INFLAMED ENDOCERVICAL MUCOSA. - REACTIVE SQUAMOUS EPITHELIUM. - NEGATIVE FOR MALIGNANCY.
UTERINE ENDOCERVIX, CURETTAGE: - BENIGN INFLAMED ENDOCERVICAL MUCOSA. - STRIPPED ENDOCERVICAL EPITHELIUM WITHIN NORMAL LIMITS.
No stroma present
UTERINE ENDOCERVIX, CURETTAGE: - STRIPPED ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY.
Limited tissue
UTERINE ENDOCERVIX, CURETTAGE: - ONE MINUTE FRAGMENT OF ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY, SEE COMMENT. - VERY SCANT SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. COMMENT: The assessment is severely limited by the small amount of tissue. A re-biopsy should be considered within the clinical context.
UTERINE ENDOCERVIX, CURETTAGE: - ONE MINUTE FRAGMENT OF ENDOCERVICAL EPITHELIUM WITHOUT APPARENT PATHOLOGY, SEE COMMENT. - VERY SCANT SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. COMMENT: The assessment is severely limited by the small amount of tissue. Clinical correlation is suggested.
UTERINE ENDOCERVIX, CURETTAGE: - BENIGN SQUAMOUS EPITHELIUM WITH METAPLASTIC CHANGE. - VERY SCANT BENIGN ENDOCERVICAL EPITHELIUM, SUBOPTIMAL SAMPLING.
UTERINE CERVIX, BIOPSY: - MINUTE FRAGMENTS OF SUPERFICIAL SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. - SCANT MUCOUS AND INFLAMMATORY CELLS. - SEE COMMENT. COMMENT: The assessment is severely limited by the small amount of tissue. A re-biopsy should be considered within the clinical context.
Inadequate biopsy
- Unfortunately, inadequate biopsies are common.
Endocervix
Sign out
No endocervical epithelium
UTERINE ENDOCERVIX, CURETTAGE: - SQUAMOUS EPITHELIUM WITHOUT APPARENT PATHOLOGY. - NO ENDOCERVICAL EPITHELIUM IDENTIFIED. - MUCOUS AND INFLAMMATORY CELLS.
No epithelium
UTERINE ENDOCERVIX, CURETTAGE: - MUCOUS AND INFLAMMATORY CELLS. - NO EPITHELIUM IDENTIFIED.
No tissue
UTERINE ENDOCERVIX, CURETTAGE: - NO TISSUE PRESENT, SEE COMMENT. COMMENT: No tissue identified on gross or microscopy.
UTERINE ENDOCERVIX, CURETTAGE: - NO TISSUE PRESENT, SEE COMMENT. COMMENT: No tissue identified on microscopy. No tissue is seen on inspection of the paraffin block.
Where to start
- Identify epithelium - exocervical (stratified squamous), endocervical (simple columnar), both.
- If there is both exocervix and endocervix --> transition zone.
- Identify possible squamous lesions.
- Identify possible endocervical lesions.
Benign entities of the cervix
The cervix is MANTLED:
- Mullerian papilloma/Mesonephric hyperplasia/Microglandular hyperplasia.
- Arias Stella reaction.
- Nabothian cyst.
- Tunnel cluster/Tuboendometrioid metaplasia.
- Lobular endocervical glandular hyperplasia.
- Endocervical polyp/Endocervicosis/Endometriosis/Ectopic prostatic tissue.
- Diffuse laminar endocervical hyperplasia.
Benign
Nabothian cyst
General
- Benign.
- Common.
Gross
- Bump.
- Pale colour.
DDx - clinical:
Image
Microscopic
Features:
- Simple endocervical cyst.
- Usually lined by endocervical epithelial cells - may be flattened.
- Columnar morphology with large clear, apical vacuoles.
- +/-Macrophages.
- +/-Mucus.
- Usually lined by endocervical epithelial cells - may be flattened.
Note:
- May be lined by tubal epithelium.
- Cilia.
- High NC ratio ~ 1:1.[citation needed]
Image:
Sign out
CERVICAL POLYP, REMOVAL: - BENIGN POLYPOID FRAGMENT OF EXOCERVICAL MUCOSA WITH NABOTHIAN CYSTS AND BENIGN ENDOCERVICAL EPITHELIUM.
POLYPOID LESION ("CERVICAL POLYP"), EXCISION:
- POLYPOID NABOTHIAN CYST.
Tunnel cluster
General
- Benign.[10]
- Not the same as microglandular hyperplasia.[11]
- Considered a special type of nabothian cyst.[12]
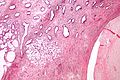
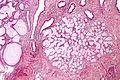
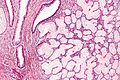
Microscopic
- Well-circumscribed lesion consisting of:
- Benign endocervical glands.
- Dilated & filled with mucin or (less commonly) eosinophilic secretions.
- Lining epithelium compressed/flattened (attenuated).
- Gland architecture: branching, tortuous.
- Scant intervening stroma.
Notes:
- Usually no nuclear atypia and no mitotic activity.
- Important only as one could possibly mistake it as minimal deviation adenocarcinoma, AKA adenoma malignum.[15]
Images
www:
Microglandular hyperplasia
- Not to be confused with microglandular adenosis.
- Abbreviated MGH.
- AKA microglandular change.
Wolffian duct hyperplasia
General
- Benign.
Microscopic
Features:
- Abundant small tubules with a simple cuboidal epithelium.
- Round small bland nucleus.
DDx:
Stains
- PAS-D+ve (cytoplasm).
Squamous metaplasia of the uterine cervix
- Abbreviated SMC.
Reactive squamous epithelium of the uterine cervix
General
Microscopic
Features:
- Inflammation - key feature.
- Lymphocytes.
- Plasma cells.
- Mild nuclear enlargement. †
- Nucleoli - important.
Note:
- † Normal squamous cell nuclei are approximately 8 μm.[17]
- Mild enlargement ~ 2-3x normal.
- CIN I nuclei are ~ 3x normal (24 μm).
DDx:
IHC
- p16 -ve.
Sign out
UTERINE CERVIX, BIOPSY: - REACTIVE SQUAMOUS EPITHELIUM. - BENIGN ENDOCERVICAL GLANDS. - NEGATIVE FOR MALIGNANCY.
COMMENT: The squamous epithelium is negative for p16 staining. Ki-67 staining is predominantly in the lower third of the epithelium.
Tubal metaplasia of the uterine cervix
- AKA tubal metaplasia, abbreviated TM.
General
- Benign.
- Mimics the appearance of AIS - especially at low power.
Microscopic
Features - like the fallopian tube:
- Nuclear crowding vis-à-vis benign endocervical epithelium (low power).
- Mixed cell population (high power):
- Peg cells - "tall" and "skinny".
- Columnar/golf tee-like appearance.
- Ciliated cells - cilia, pale cytoplasm, round central nucleus.
- Secretory cells - non-ciliated, basophilic cytoplasm, round small basal nuclei.
- Peg cells - "tall" and "skinny".
DDx:
Image:
IHC
Features:[18]
- Vimentin +ve.
- CEA -ve/+ve.
- p16 -ve.[citation needed]
Atrophy of the uterine cervix
Radiation changes of the endocervical epithelium
General
- Uncommon.
- Clinical history: radiation treatment for cervical carcinoma.[19]
Microscopic
Features:[19]
- Nuclear enlargement with a normal NC ratio.
- +/-Coarse chromatin.
- +/-Nucleoli.
- +/-Multinucleation - very common.
- Histiocytes - common.
Reactive endocervical cells
General
- Benign.
Microscopic
Features:
- Mild nuclear enlargement.
- +/-Multinucleation.[20]
Notes: DDx of multinucleated endocervical cells:
Images
www:
Non-invasive
Cervical intraepithelial neoplasia
- Previously known as cervical intraepithelial neoplasia and cervical dysplasia.
Endocervical adenocarcinoma in situ
- For the cytology see Gynecologic cytopathology#Endocervical adenocarcinoma in situ
- AKA adenocarcinoma in situ, abbreviated AIS.
Cancer
Squamous cell carcinoma of the uterine cervix
- AKA cervical squamous cell carcinoma.
Adenocarcinoma of the uterine cervix
Uncommon non-invasive
Stratified mucin-producing intraepithelial lesions of the cervix
- Abbreviated SMILE (Stratified Mucin-producing Intraepithelial LEsion).
Uncommon types of cervical cancer
There are a number of uncommon type of cervical cancer.
Serous carcinoma of the uterine cervix
General
- Poor prognosis.[22]
- Extremely rare.
Microscopic
Features:
- Like other serous carcinomas.
Adenosquamous carcinoma of the uterine cervix
Clear cell carcinoma of the uterine cervix
Small cell carcinoma of the cervix
- Like small cell carcinoma elsewhere.
DDx:
IHC
- HPV +ve.
Adenoid basal carcinoma
- See also: Basal cell carcinoma.
General
- Good prognosis.[23]
Microscopic
Features:[23]
- Nests of cells with basaloid rim and squamoid center.
- Basaloid cells look benign.
DDx:
- Ectopic prostate gland.
Image:
Glassy cell carcinoma
Villoglandular adenocarcinoma of the cervix
- AKA well-differentiated papillary villoglandular adenocarcinoma,[24] AKA villoglandular papillary adenocarcinoma, AKA well-differentiated villoglandular adenocarcinoma.
General
- Rare.
- Younger patients and relatively good prognosis.[25]
- Associated with HPV.
- May also arise from the endometrium.[26]
Microscopic
Features:[27]
- Papillary structures (nipple-like shapes with a fibrovascular core) that are long.
- Nobody defines "long".
- Perhaps - long >3:1 length:width.
- Nobody defines "long".
- Covered by columnar (or cuboidal) epithelium.
- Intracellular mucin (focal).
DDx:
- Serous carcinoma of the cervix.
Images
www:
Mucoepidermoid carcinoma of the uterine cervix
General
- Controversial - not in the WHO.[28]
Microscopic
Features:[29]
- Squamous cell carcinoma-like with:
- No glands formation.
- Intracellular mucin.
- Classically have mucous cells - cells with abundant fluffy cytoplasm and large mucin vacuoles - key feature.
Notes:
- Similar to the salivary gland tumour.[28]
DDx:
- Cervical intraepithelial neoplasia, i.e. CIN II, CIN III.
- Adenosquamous carcinoma.
Stains
Mucin stains:[29]
IHC
- CEA +ve.[29]
Molecular
Like the salivary gland tumour:
- t(11;19) CRTC1/MAML2.[28]
Mesonephric adenocarcinoma
Minimal deviation adenocarcinoma of the uterine cervix
See also
References
- ↑ Dresang, LT.. "Colposcopy: an evidence-based update.". J Am Board Fam Pract 18 (5): 383-92. PMID 16148248.
- ↑ Zonios, G. (Aug 2012). "Reflectance model for acetowhite epithelium.". J Biomed Opt 17 (8): 87003-1. doi:10.1117/1.JBO.17.8.087003. PMID 23224202.
- ↑ Li, W.; Venkataraman, S.; Gustafsson, U.; Oyama, JC.; Ferris, DG.; Lieberman, RW.. "Using acetowhite opacity index for detecting cervical intraepithelial neoplasia.". J Biomed Opt 14 (1): 014020. doi:10.1117/1.3079810. PMID 19256708.
- ↑ Casey, PM.; Long, ME.; Marnach, ML. (Feb 2011). "Abnormal cervical appearance: what to do, when to worry?". Mayo Clin Proc 86 (2): 147-50; quiz 151. doi:10.4065/mcp.2010.0512. PMC 3031439. PMID 21270291. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3031439/.
- ↑ Kenwright, D.; Braam, G.; Maharaj, D.; Langdana, F. (Jan 2012). "Multiple levels on LLETZ biopsies do not contribute to patient management.". Pathology 44 (1): 7-10. doi:10.1097/PAT.0b013e32834d7b5d. PMID 22173237.
- ↑ URL: http://www.webmd.com/cancer/cervical-cancer/loop-electrosurgical-excision-procedure-leep-for-abnormal-cervical-cell-changes. Accessed on: 20 March 2014.
- ↑ Ware, RA.; van Nagell, JR. (2010). "Radical hysterectomy with pelvic lymphadenectomy: indications, technique, and complications.". Obstet Gynecol Int 2010. doi:10.1155/2010/587610. PMID 20871657.
- ↑ URL: http://www.med-ed.virginia.edu/Courses/path/gyn/cervix1.cfm. Accessed on: 12 May 2010.
- ↑ URL: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-what-is-cervical-cancer. Accessed on: 27 January 2014.
- ↑ Nucci, MR. (Oct 2002). "Symposium part III: tumor-like glandular lesions of the uterine cervix.". Int J Gynecol Pathol 21 (4): 347-59. PMID 12352183.
- ↑ Zaino, RJ. (Mar 2000). "Glandular lesions of the uterine cervix.". Mod Pathol 13 (3): 261-74. doi:10.1038/modpathol.3880047. PMID 10757337.
- ↑ Okamoto, Y.; Tanaka, YO.; Nishida, M.; Tsunoda, H.; Yoshikawa, H.; Itai, Y.. "MR imaging of the uterine cervix: imaging-pathologic correlation.". Radiographics 23 (2): 425-45; quiz 534-5. PMID 12640157.
- ↑ URL: http://pathologyoutlines.com/cervix.html#tunnelclusters. Accessed on: 27 February 2011.
- ↑ URL: http://surgpath4u.com/caseviewer.php?case_no=477. Accessed on: 5 September 2011.
- ↑ Gilks CB, Young RH, Aguirre P, DeLellis RA, Scully RE (September 1989). "Adenoma malignum (minimal deviation adenocarcinoma) of the uterine cervix. A clinicopathological and immunohistochemical analysis of 26 cases". Am. J. Surg. Pathol. 13 (9): 717–29. PMID 2764221.
- ↑ Bhutia, K.; Puri, M.; Gami, N.; Aggarwal, K.; Trivedi, SS.. "Persistent inflammation on Pap smear: does it warrant evaluation?". Indian J Cancer 48 (2): 220-2. doi:10.4103/0019-509X.82901. PMID 21768670.
- ↑ URL: http://www.curran.pwp.blueyonder.co.uk/cytology.htm. Accessed on: 5 November 2012.
- ↑ Marques, T.; Andrade, LA.; Vassallo, J. (Jun 1996). "Endocervical tubal metaplasia and adenocarcinoma in situ: role of immunohistochemistry for carcinoembryonic antigen and vimentin in differential diagnosis.". Histopathology 28 (6): 549-50. PMID 8803599.
- ↑ 19.0 19.1 Frierson, HF.; Covell, JL.; Andersen, WA. (1990). "Radiation changes in endocervical cells in brush specimens.". Diagn Cytopathol 6 (4): 243-7. PMID 2209348.
- ↑ URL: http://www.surgpath4u.com/caseviewer.php?case_no=229. Accessed on: 2 January 2014.
- ↑ Naib, ZM.; Nahmias, AJ.; Josey, WE.; Zaki, SA. (Jun 1973). "Relation of cytohistopathology of genital herpesvirus infection to cervical anaplasia.". Cancer Res 33 (6): 1452-63. PMID 4352382.
- ↑ Togami, S.; Kasamatsu, T.; Sasajima, Y.; Onda, T.; Ishikawa, M.; Ikeda, S.; Kato, T.; Tsuda, H. (2012). "Serous adenocarcinoma of the uterine cervix: a clinicopathological study of 12 cases and a review of the literature.". Gynecol Obstet Invest 73 (1): 26-31. doi:10.1159/000329319. PMID 21876330.
- ↑ 23.0 23.1 Senzaki H, Osaki T, Uemura Y, et al. (December 1997). "Adenoid basal carcinoma of the uterine cervix: immunohistochemical study and literature review". Jpn. J. Clin. Oncol. 27 (6): 437–41. PMID 9438010. http://jjco.oxfordjournals.org/cgi/content/full/27/6/437.
- ↑ Fadare, O.; Zheng, W. (Nov 2005). "Well-differentiated papillary villoglandular adenocarcinoma of the uterine cervix with a focal high-grade component: is there a need for reassessment?". Virchows Arch 447 (5): 883-7. doi:10.1007/s00428-005-0030-3. PMID 16088403.
- ↑ Korach, J.; Machtinger, R.; Perri, T.; Vicus, D.; Segal, J.; Fridman, E.; Ben-Baruch, G. (2009). "Villoglandular papillary adenocarcinoma of the uterine cervix: a diagnostic challenge.". Acta Obstet Gynecol Scand 88 (3): 355-8. doi:10.1080/00016340902730359. PMID 19172445.
- ↑ Zaino, RJ.; Kurman, RJ.; Brunetto, VL.; Morrow, CP.; Bentley, RC.; Cappellari, JO.; Bitterman, P. (Nov 1998). "Villoglandular adenocarcinoma of the endometrium: a clinicopathologic study of 61 cases: a gynecologic oncology group study.". Am J Surg Pathol 22 (11): 1379-85. PMID 9808130.
- ↑ Nucci, Marisa R.; Oliva, Esther (2009). Gynecologic Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 180-1. ISBN 978-0443069208.
- ↑ 28.0 28.1 28.2 Lennerz, JK.; Perry, A.; Mills, JC.; Huettner, PC.; Pfeifer, JD. (Jun 2009). "Mucoepidermoid carcinoma of the cervix: another tumor with the t(11;19)-associated CRTC1-MAML2 gene fusion.". Am J Surg Pathol 33 (6): 835-43. doi:10.1097/PAS.0b013e318190cf5b. PMID 19092631.
- ↑ 29.0 29.1 29.2 Thelmo, WL.; Nicastri, AD.; Fruchter, R.; Spring, H.; DiMaio, T.; Boyce, J. (1990). "Mucoepidermoid carcinoma of uterine cervix stage IB. Long-term follow-up, histochemical and immunohistochemical study.". Int J Gynecol Pathol 9 (4): 316-24. PMID 1700969.