Difference between revisions of "Testis"
(→Benign: split out) |
(→Testicular atrophy: split out) |
||
| Line 208: | Line 208: | ||
=Benign= | =Benign= | ||
==Testicular atrophy== | ==Testicular atrophy== | ||
*[[AKA]] ''atrophic testis''. | *[[AKA]] ''atrophic testis''. | ||
*[[AKA]] ''atrophy of the testis''. | *[[AKA]] ''atrophy of the testis''. | ||
{{Main|Testicular atrophy}} | |||
==Spermatocele== | ==Spermatocele== | ||
Revision as of 04:39, 24 July 2014
The testis, plural testes, are important for survival of the species. Tumours occasionally arise in 'em. They generally are not biopsied.
If the testis is biopsied, it is usually for fertility -- to understand whether the man is really azoospermic.
Normal testis
Gross
Anatomy - deep to superficial:
- Tunica albuginea - fibrous layer.
- Tunica vaginalis - thin mesothelial layer.
Microscopic
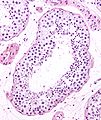
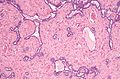
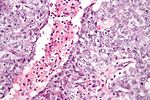
Seminiferous tubules
- Sertoli cells (AKA sustentacular cell AKA nurse cell).
- Large cells with oval nucleus.
- Primary spermatocyte.
- Small cells with dark nucleus on basement membrane.
- Secondary spermatocyte.
- Rarely seen on light microscopy.
- Spermatids.
- Round small.
- Usually close to the centre of the lumen.
- Spermatozoa.
- You don't see the tail on light microscopy.
Images
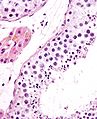
Interstitial
- Leydig cell (AKA interstitial cell).
- Large eosinophilic cell.
- Blood vessels.
Image
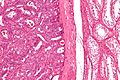
Associated structures
- Epididymis - stores the sperm.
- Pseudostratified epithelium with cilia.
Image:
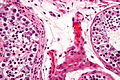
Rete testis
- Receives stuff from the tubules.
- Very rarely give rise to an adenocarcinoma of the rete testis.
- May be involved by seminoma - increases risk of relapse in a univariate analysis.[1]
Microscopic:
- Delicate anastomosing channels lined by cuboid epithelium.
Images
www:
Appendix of testis
- Muellerian duct remnant.
Microscopic:
- Polypoid structure.
Images:
Sign out
TESTICLE, RIGHT, ORCHIECTOMY: - TESTICLE WITHOUT APPARENT PATHOLOGY. - NEGATIVE FOR INTRATUBULAR GERM CELL NEOPLASIA. - NEGATIVE FOR MALIGNANCY.
Alternate
RIGHT TESTICLE, ORCHIDECTOMY: - BENIGN TESTIS WITH SPERMATOGENESIS. - NEGATIVE FOR INTRATUBULAR GERM CELL NEOPLASIA. - NEGATIVE FOR MALIGNANCY.
Diagnoses (overview)
- Benign.
- Spermatid present/not present.
- Infertility - azoospermic.
- No sperm present.
- Germ cell tumours (GCTs).
- Intratubular germ cell neoplasia.
- Seminoma.
- Spermatocytic seminoma.
- Yolk sac tumour (endodermal sinus tumour).
- Embryonal carcinoma.
- Choriocarcinoma.
- Teratoma.
- Mixed GCT - 60% of GCTs are mixed.
- Common combinations:
- teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- seminoma + embryonal (SE).
- embryonal + teratoma (TE).
- Common combinations:
- Sex-cord stromal tumour.
IHC for GCTs
ABCDs of GCTs:
- AFP - yolk sac tumour.
- Beta-hCG - choriocarcinoma.
- CD30 - embryonal carcinoma.
- D2-40 - seminoma.
Tabular summary of GCTs
| Tumour | Key feature | Microscopic | IHC | Other | Image |
|---|---|---|---|---|---|
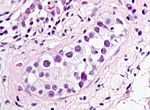
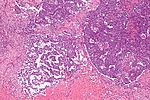
| Intratubular germ cell neoplasia (ITGCN) | nests of small fried egg cells | large central nucleus, clear cytoplasm, round or polygonal nuclear membrane, nucleoli[2] |
CD117 | appearance similar to seminoma | |
| Seminoma | fried egg cells | fried egg-like cells (central nucleus, clear cytoplasm) with squared-off nuclear membrane, nucleoli, lymphocytic infiltrate, granulomata, syncytiotrophoblastic giant cells[3] |
D2-40 | Dysgerminoma = female version of this tumour | |
| Yolk sac tumour (endodermal sinus tumour) | Schiller-Duval bodies | Schiller-Duval b. = central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells, variable arch. | AFP | patterns: microcystic, solid, hepatoid | |
| Embryonal carcinoma | prominent nucleoli, vescicular nuclei | var. arch.: tubulopapillary, glandular, solid, embryoid bodies (ball of cells in surrounded by empty space on three sides), +/-nuclear overlap, mitoses common | CD30 | usu. part of a mixed GCT | |
| Choriocarcinoma | marked nuclear atypia | cells with clear cytoplasm (cytotrophoblast), multinucleated cells (syncytiotrophoblast) | beta-hCG | not commonly pure, usu. a component of a mixed GCT | |
| Teratoma | skin, GI tract-like epithelium | skin (epidermis, adnexal structures - sebaceous glands, hair follicles), GI tract-like glands (simple tall columnar epithelium), fat +/-primitive neuroepithelium (pseudostratified epithelium in rosettes) | None | testicular teratomas in post-pubertal males are all considered malignant[4] | |
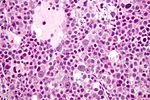
| Spermatocytic seminoma | population of 3 cells | pop.: (1) small cell with high NC ratio (mature lymphocyte-like), (2) medium with nucleoli, (3) large cells with filamentous chromatin - few present | ? | does not arise from ITGCN, no lymphocytic infiltrate (like in seminoma) | |
| Mixed germ cell tumour | NA | common combinations: teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE); seminoma + embryonal (SE); embryonal + teratoma (TE) | NA | - |
Tabular summary of (male) SCSTs
| Tumour | Key feature | Microscopic | IHC | Other | Image |
|---|---|---|---|---|---|
| Leydig cell tumour | intersitial cell cluster with eosinophilic cytoplasm | cytoplasmic vacuolization, uniform nuclei with nucleoli | MART-1, calretinin, inhibin | +/-Reinke crystals (cylindrical crystalloid eosinophilic cytoplasmic bodies) | |
| Sertoli cell tumour | cells in cords or trabeculae | light staining bubbly cytoplasm +/- large cytoplasmic vacuoles, granular chromatin | ? | usu. no significant nuclear atypia, no mitoses |
Benign
Testicular atrophy
Spermatocele
General
- Benign.
- Cyst of the epididymis (classic).
- May arise in the rete testis or vas deferens.[5]
Clinical:
- Often asymptomatic.
- Excised due to pain or mass effect.[6]
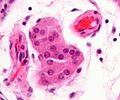
Microscopic
Features:
- Cyst lined by a simple ciliated epithelium.
- Contain sperm.
- Head: ~1/2 the size of a RBC, black.
- Tail: infrequently seen.
Note:
- Small cellular clusters may be present.
- May mimic small cell carcinoma.[7]
DDx:
- Hydrocele testis - do not contain sperm.
Images
www:
Hydrocele testis
- AKA hydrocele.
General
Clinical:
- Scrotal mass.
Microscopic
Features:
- Cyst lined by a simple ciliated epithelium.
- Does not contain sperm.
DDx:
- Spermatocele - contains sperm.
Sign out
HYDROCELE SAC, LEFT, EXCISION: - CONSISTENT WITH HYDROCELE SAC.
SOFT TISSUE ("HYDROCELE SAC"),LEFT, EXCISION:
- FIBROADIPOSE TISSUE COVERED BY MESOTHELIUM WITH REACTIVE CHANGES -- CONSISTENT
WITH HYDROCELE SAC.
- EPIDIDYMIS WITH SPERM (INCIDENTAL FINDING).
Micro
The sections shows fragments of tissue compatible with a benign cyst, that had a fibrous wall and was lined by a simple epithelium. No spermatocytes are identified.
Benign connective tissue (including skeletal muscle, nerves and blood vessels) is also present.
Idiopathic granulomatous orchitis
- Granulomatous orchitis redirects here.
General
- Rare.
- Unknown etiology -- possibly trauma + immune reaction to sperm.[10]
Microscopic
Features:[10]
- Granulomas +/- necrosis.
- +/-Destruction of seminiferous tubules.
- Prominent collagen fibrosis.
DDx:
- ITGCN.
- Seminoma.
- Tertiary syphilis - classically, plasma cell rich.[11]
- Syphilis, unlike other infections of the GU tract, is said to affect the testis before the epididymis.[12]
- Tuberculosis.
- Lymphoma.[10]
- Malakoplakia.[10]
Stains
- AFB -ve -- for tuberculosis.
- Dieterle stain -ve -- for syphilis.
Testicular scar
Testicular abscess
Premalignant
Intratubular germ cell neoplasia
- Abbreviated ITGCN.
Germ cell tumours
Seminoma
Spermatocytic seminoma
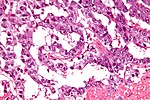
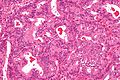
Yolk sac tumour
- Most common GCT in infants and young boys.
Microscopic
Classic feature:
- Schiller-Duval bodies.
- Look like glomerulus - central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells
- Architecure - variable.
- Most common microcystic pattern.[13]
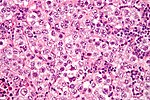
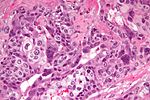
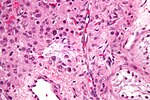
Embryonal carcinoma
These often look like a poorly differentiated carcinoma.
General
- Affects young adults.
- May be seen in women.
Microscopic
Features:[14]
- Nucleoli - key feature.
- Vesicular nuclei (clear, empty appearing nuclei) - key feature.
- Nuclei overlap.
- Necrosis - common.
- Not commonly present in seminoma.
- Indistinct cell borders
- Mitoses - common.
- Variable architecture:
- Tubulopapillary.
- Glandular.
- Solid.
- Embryoid bodies - ball of cells in surrounded by empty space on three sides.
Notes:
- Cytoplasmic staining variable (eosinophilic to basophilic).
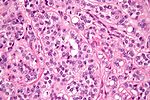
Choriocarcinoma
These are aggressive tumours.
Microscopic
Features:
- Syncytiotrophoblasts:
- Large + many irreg. or lobular hyperchromatic nuclei.
- Eosinophilic vacuolated cytoplasm (contains hCG).
- Cytotrophoblasts:
- Clear cytoplasm.
- Polygonal shaped cells in cords/masses.
- Distinct cell borders.
- Single uniform nucleus.
- +/-Hemorrhage.
- +/-Necrosis.
Teratoma of the testis
In post-pubertal males these (testicular) tumours are considered malignant. They usually consist of all three germ layers.[15]
Sex cord stromal tumours
Leydig cell tumour
- AKA interstitial cell tumour.
Sertoli cell nodule
- Abbreviated SCN.
- AKA Pick's adenoma.
- AKA testicular tubular adenoma.
- AKA tubular adenoma of the testis.
Sertoli cell tumour
Other
These tumours are rare.
Adenocarcinoma of the rete testis
General
- Extremely rare - a few dozen cases in the world literature.[16]
- Possible association of diethylstilbestrol.[16]
Microscopic
Features:
- Adenocarcinoma:
- Tubular or papillary architecture.[16]
- Columnar cells with cigar-shaped nuclei.
Images
See also
References
- ↑ Soper, MS.; Hastings, JR.; Cosmatos, HA.; Slezak, JM.; Wang, R.; Lodin, K. (Dec 2012). "Observation Versus Adjuvant Radiation or Chemotherapy in the Management of Stage I Seminoma: Clinical Outcomes and Prognostic Factors for Relapse in a Large US Cohort.". Am J Clin Oncol. doi:10.1097/COC.0b013e318277d839. PMID 23275274.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 538. ISBN 978-0443066771.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 542. ISBN 978-0443066771.
- ↑ Carver, BS.; Al-Ahmadie, H.; Sheinfeld, J. (May 2007). "Adult and pediatric testicular teratoma.". Urol Clin North Am 34 (2): 245-51; abstract x. doi:10.1016/j.ucl.2007.02.013. PMID 17484929.
- ↑ URL: http://emedicine.medscape.com/article/443432-overview. Accessed on: 5 March 2012.
- ↑ Walsh, TJ.; Seeger, KT.; Turek, PJ.. "Spermatoceles in adults: when does size matter?". Arch Androl 53 (6): 345-8. PMID 18357964.
- ↑ Lane, Z.; Epstein, JI. (Jan 2010). "Small blue cells mimicking small cell carcinoma in spermatocele and hydrocele specimens: a report of 5 cases.". Hum Pathol 41 (1): 88-93. doi:10.1016/j.humpath.2009.06.018. PMID 19740515.
- ↑ Junnila, J.; Lassen, P. (Feb 1998). "Testicular masses.". Am Fam Physician 57 (4): 685-92. PMID 9490992.
- ↑ Wampler, SM.; Llanes, M. (Sep 2010). "Common scrotal and testicular problems.". Prim Care 37 (3): 613-26, x. doi:10.1016/j.pop.2010.04.009. PMID 20705202.
- ↑ 10.0 10.1 10.2 10.3 Roy, S.; Hooda, S.; Parwani, AV. (May 2011). "Idiopathic granulomatous orchitis.". Pathol Res Pract 207 (5): 275-8. doi:10.1016/j.prp.2011.02.005. PMID 21458170.
- ↑ Sekita, N.; Nishikawa, R.; Fujimura, M.; Sugano, I.; Mikami, K. (Jan 2012). "[Syphilitic orchitis: a case report].". Hinyokika Kiyo 58 (1): 53-5. PMID 22343746.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 364. ISBN 978-0781765275.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=1. Accessed on: March 8, 2010.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 549. ISBN 978-0443066771.
- ↑ Moore, Keith L.; Persaud, T.V.N. (2002). The Developing Human: Clinically Oriented Embryology (7th ed.). Saunders. pp. 83. ISBN 978-0721694122.
- ↑ 16.0 16.1 16.2 Newbold, RR.; Bullock, BC.; McLachlan, JA. (Dec 1986). "Adenocarcinoma of the rete testis. Diethylstilbestrol-induced lesions of the mouse rete testis.". Am J Pathol 125 (3): 625-8. PMC 1888460. PMID 3799821. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888460/.