Difference between revisions of "Microorganisms"
(→Fungi: +images) |
|||
| Line 23: | Line 23: | ||
| ? Immunosuppression | | ? Immunosuppression | ||
| <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | | <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
| [ | | [[Image:Pulmonary_aspergillosis.jpg|thumb|150px|center|Aspergillus (WC)]] | ||
|- | |- | ||
| Zygomycota ([[zygomycosis]]);<br>''more specific''<br>Mucorales ([[mucormycosis]]) | | Zygomycota ([[zygomycosis]]);<br>''more specific''<br>Mucorales ([[mucormycosis]]) | ||
| Line 33: | Line 33: | ||
| Diabetes, immunodeficient | | Diabetes, immunodeficient | ||
| <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | | <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
| [ | | [[Image:Zygomycosis.jpg |thumb|150px|center|Zygomycosis (WC)]] | ||
|- | |- | ||
| Coccidioides, usually C. immitis<br>([[coccidioidomycosis]]) | | Coccidioides, usually C. immitis<br>([[coccidioidomycosis]]) | ||
| Line 53: | Line 53: | ||
| Source: soil with bird droppings | | Source: soil with bird droppings | ||
| <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | | <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
| [ | | [[Image:Histoplasma_pas-d.jpg|thumb|150px|center|Histoplasmosis (WC)]] | ||
|- | |- | ||
| Blastomyces ([[blastomycosis]]) | | Blastomyces ([[blastomycosis]]) | ||
| Line 73: | Line 73: | ||
| Clinical??? | | Clinical??? | ||
| <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | | <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
| [ | | [[Image:Paracoccidioides_brasiliensis_01.jpg|thumb|150px|center|P. brasiliensis (WC)]] | ||
|- | |- | ||
| Pneumocystis jirovecii ([[pneumocystis pneumonia]]; abbrev. PCP) | | Pneumocystis jirovecii ([[pneumocystis pneumonia]]; abbrev. PCP) | ||
| Line 83: | Line 83: | ||
| [[HIV]]/AIDS associated | | [[HIV]]/AIDS associated | ||
| <ref name=Ref_APBR684>{{Ref APBR|684}}</ref> | | <ref name=Ref_APBR684>{{Ref APBR|684}}</ref> | ||
| [ | | [[Image:Pneumocystosis_carinii_of_lung_in_AIDS_959_lores.jpg |thumb|150px|center|PCP (WC)]] | ||
|- | |- | ||
| Cryptococcus ([[cryptococcosis]]) | | Cryptococcus ([[cryptococcosis]]) | ||
| Line 93: | Line 93: | ||
| HIV/AIDS associated, most common CNS fungus | | HIV/AIDS associated, most common CNS fungus | ||
| <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | | <ref name=Ref_APBR682>{{Ref APBR|682}}</ref> | ||
| [ | | [[Image:Cryptococcosis_of_lung_in_patient_with_AIDS._Mucicarmine_stain_962_lores.jpg |thumb|150px|center|Crytococcosis - mucicarmine (WC)]] | ||
|} | |} | ||
Notes: | Notes: | ||
Revision as of 01:43, 17 October 2013
Microorganisms show-up every once in a while. It is essential to know 'em.
Microorganisms
Fungi
| Name (disease) | Kingdom | Size | Shape | Stains | Other (microscopic) | Clinical | References | Image |
|---|---|---|---|---|---|---|---|---|
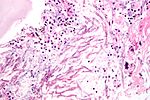
| Aspergillus (aspergillosis) | Fungi | ? | Hyphae that branching with 45 degrees angle |
PAS-D | Fruiting heads when aerobic | ? Immunosuppression | [1] | |
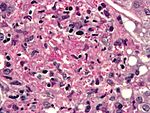
| Zygomycota (zygomycosis); more specific Mucorales (mucormycosis) |
Fungi | ? | Branching hyphae with variable width | ? | Granulomata assoc. | Diabetes, immunodeficient | [1] | |
| Coccidioides, usually C. immitis (coccidioidomycosis) |
Fungi | Large - 20-60 micrometers, endospores 1-5 micrometers |
Spherules | Stains? | Other? | Immunodeficient | [1] | Coccidioidomycosis (med.sc.edu) C. immitis (WC) (webpathology.com) |
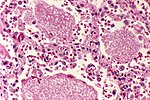
| Histoplasma (histoplasmosis) | Fungi | 2-5 micrometers | Spherical | GMS | Intracellular (unlike candida), granulomata | Source: soil with bird droppings | [1] | |
| Blastomyces (blastomycosis) | Fungi | 5-15 micrometres | Spherical (yeast) | Stains? | Granulomas, broad-based budding yeast | Habitat: Northeast America, Africa | [1][2] | Blastomyces |
| Paracoccidioides (paracoccidioidomycosis) | Fungi | 6-60 micrometres | Spherical (yeast) | Stains? | Multiple budding "steering wheel" appearance | Clinical??? | [1] | |
| Pneumocystis jirovecii (pneumocystis pneumonia; abbrev. PCP) | Fungi (previously thought to be a protozoan) | 7-8 micrometres | "Dented ping-pong ball" | GMS | Usually in clusters of alveolar casts with a honeycomb appearance | HIV/AIDS associated | [3] | |
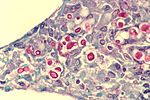
| Cryptococcus (cryptococcosis) | Fungi | 5-15 micrometres | Yeast | GMS | Prominent (i.e. thick polysaccharide) capsule | HIV/AIDS associated, most common CNS fungus | [1] |
Notes:
- Bold text = key features.
Fungi
- There are lots of 'em. Below are a few of 'em.
Terminology:[4]
- Hyphae = microscopic filamentous growth (of fungi) -- single cell.
- Mycelial = filamentous network of hyphae.
- Septae/septation = hyphae may be subdivided by septae -- if they aren't they are one mass of protoplasm. (?)
- Dimorphism = exist in two forms; e.g. single cell (yeast) and mycelial growth.
- Pseudohyphae = looks like hyphae --but branching pattern is created by separate cells.[5]
Tissue invasive fungi
Typically:[6]
- Mucor.
- Aspergillus.
List
- Histoplasmosis.
- Coccidioidomycosis.
- Pneumocystis pneumonia.
- Cryptococcus.
- Cryptosporidiosis.
- Candidiasis.
- Blastomycosis.
- Mucormycosis.
Worms & stuff
Schistosomiasis
- See Urine cytopathology.
General
- Trematode, i.e. type of worm.
- Due to:
- Schistosoma mansoni.
- Schistosoma haematobium.
- Schistosoma japonicum
- S. haematobium infection associated with squamous cell carcinoma of the urinary bladder.
- Classically presents with hematuria.
Microscopic
Features of ova (S. haematobium):[7]
- Elliptical ~140 micrometres max dimension.
- "Spike" approx. the size of a PMN.
Images:
- WC:
- www:
Toxoplasma
General
- Common CNS infection.
- Toxoplasma gondii - pathogenic; causes toxoplasmosis.
- Protozoa.
- A TORCH infection.
Microscopic
General:
- Dependent on location in body.
Lymph node
LN features:[8]
- Reactive germinal centers (pale areas - larger than usual).
- Often poorly demarcated - due to loose epithelioid cell clusters at germinal center edge - key feature.
- Epithelioid cells - perifollicular & intrafollicular.
- Loose aggregates of histiocytes (do not form round granulomas):
- Abundant pale cytoplasm.
- Nucleoli.
- Loose aggregates of histiocytes (do not form round granulomas):
- Monocytoid cells (monocyte-like cells) - in cortex & paracortex.
- Large cells in islands/sheets key feature with:
- Abundant pale cytoplasm - important.
- Well-defined cell border - important.
- Singular nucleus.
- Cell clusters usually have interspersed neutrophils.
- Large cells in islands/sheets key feature with:
Images (lymph node):
CNS
CNS features:[9]
- Granular appearing ball ~ 2x the size of resting lymphocyte.
Images (CNS):
- WC:
- www:
Heart
Features:
- Intramuscular organisms.
DDx:
- Chagas disease. (???)
Images (heart):
IHC
- IHC for toxoplasma.[10]
Strongyloidiasis
General
- Causes by worm Strongyloides stercoralis.
- High case mortality rate ~ 70%.[11]
- May present after years of latency due to immune suppression.[12]
Location:
- Lung. (???)
Microscopic
Features:
- Long worms.
- ~10-15 micrometers wide.
Images:
Echinococcus
- Several species - most common: Echinococcus granulosus.
- Causes hydatid disease in the liver.
Microscopic
Features:
- Laminated wall +/- calcification.[13]
- Organisms:
- Hooklets.
- Scoleces - knoblike anterior end of a tapeworm.[14]
Enterobius vermicularis
- AKA pinworm.
General
- Classically found in a vermiform appendix removed for appendicitis that does not have acute appendicitis.[15]
Gross
- Peri-anal white squiggly thing ~ 2-13 mm in length.
Image:
Microscopic
Features - organism:
- 0.2-0.5 mm width x 2-13 mm length.
- Characteristic triangular "spikes" seen on cross section - base x height ~ 30 x 30 μm.
- Spikes is in quotations, as these are really a longitudinal blade-like ridges, that run the length of the worm.
Features - eggs:[16]
- Ovoid - double walled shells, one side flat.
Images:
- www:
- WC:
Trichinella
General
- Causes Trichinosis.
- Classically associated with uncooked pork.[17]
- Several types; most due to T. spiralis.[17]
Microscopic
Features:
- Worm.
Image:
Cysticercosis
General
- Caused by Taenia solium; pork tapeworm.
- May cause epilepsy; most common parasitic CNS infection.[19]
Gross
- Multiple cystic spaces.
Image:
Microscopic
Features:
- Large ovoid body with complex structures (cross-section of worm) - size: millimetres.
- +/-External eosinophilic microvilli.
- +/-Gastrointestinal tract - ovoid structure within the worm.
Notes:
- Histomorphology is not distinctive for the type... microbiology usually figures it out.
Images:
- Cysticercosis (cdc.gov).
- Cysticercosis (sciencephoto.com).
- Neurocysticercosis - case 1 (upmc.edu).
- Neurocysticercosis - case 2 (upmc.edu).
Rhinosporidiosis
- Not to be confused with rhinoscleroma.
General
- Caused by parasite Rinosporidium seeberi.
- India, Sri Lanka.
- Nasal mass.
- May present with obstruction.[20]
Microscopic
- Globular cysts ~ 100 micrometers with endospores:
- Hyperchromatic (blue) spherical 10-100 micrometer.
Images:
- Rhinosporidiosis (arquivosdeorl.org.br).[22]
- Rhinosporidiosis (nih.gov).[20]
- Rhinosporidiosis (nih.gov).
Stains
- GMS stain +ve organisms.
Leishmaniasis
General
- Caused by protozoa in the group Leishmania group.
- Transmitted to humans by the sand fly.
May be:
Microscopic
Features:
- Small ~1-2 micrometers.
Images:
Stains
- Giemsa stain - highlights organisms.
Viruses
This is a fairly big topic. There are about half a dozen viral inclusions (e.g. CMV, HSV, VZV, adenovirus) a decent pathologist ought to be able to identify. The virus article covers 'em.
Bacteria
This is a small topic when considered from the perspective of an anatomical pathologist. Most stuff is sorted-out by microbiology.
Microorganisms and cancer
Viruses and cancer
A number of microorganisms are associated with the development of cancer:[25]
- Human papillomavirus (HPV) - cancer of cervix, vulva, vagina, penis, anus, head & neck.
- Epstein-Barr virus - Burkitt lymphoma, Post-transplant lymphoproliferative disorder, classical Hodgkin lymphoma (all but nodular sclerosis HL), nasopharyngeal carcinoma.
- Hepatitis B - HCC.
- Hepatitis C - HCC.
- Human T-cell lymphotropic virus type I (HTLV-1) - Adult T-cell leukemia/lymphoma.
- Human herpesvirus-8 (HHV-8) - Kaposi sarcoma, primary effusion lymphoma, body cavity lymphoma.
- Merkel cell polyomavirus - Merkel cell carcinoma.
Bacteria and cancer
Parasites and cancer
- Schistosoma haematobium - squamous cell carcinoma of the urinary bladder.
- Clonorchis sinensis (AKA Opisthorchis sinensis) - cholangiocarcinoma.
- Opisthorchis viverrini - cholangiocarcinoma.
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 682. ISBN 978-1416025887.
- ↑ http://pathmicro.med.sc.edu/mycology/mycology-6.htm
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 684. ISBN 978-1416025887.
- ↑ http://www.fungionline.org.uk/1intro/3growth_forms.html
- ↑ http://pathmicro.med.sc.edu/mycology/mycology-3.htm
- ↑ CM 17 Apr 2009.
- ↑ URL: http://path.upmc.edu/cases/case622/dx.html. Accessed on: 26 January 2012.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 113. ISBN 978-0781775960.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/N0I001-PQ01-M.htm. Accessed on: 19 October 2010.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/N0I001-PQ01-M.htm. Accessed on: 19 October 2010.
- ↑ Lim, S.; Katz, K.; Krajden, S.; Fuksa, M.; Keystone, JS.; Kain, KC. (Aug 2004). "Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.". CMAJ 171 (5): 479-84. doi:10.1503/cmaj.1031698. PMID 15337730.
- ↑ Siddiqui, AA.; Berk, SL. (Oct 2001). "Diagnosis of Strongyloides stercoralis infection.". Clin Infect Dis 33 (7): 1040-7. doi:10.1086/322707. PMID 11528578.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 448. ISBN 978-1416054542.
- ↑ http://www.thefreedictionary.com/scoleces. Accessed on: 10 January 2010.
- ↑ Dahlstrom, JE.; Macarthur, EB. (Oct 1994). "Enterobius vermicularis: a possible cause of symptoms resembling appendicitis.". Aust N Z J Surg 64 (10): 692-4. PMID 7945067.
- ↑ Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 685. ISBN 978-1416025887.
- ↑ 17.0 17.1 Kaewpitoon N, Kaewpitoon SJ, Philasri C, et al. (October 2006). "Trichinosis: epidemiology in Thailand". World J. Gastroenterol. 12 (40): 6440–5. PMID 17072975. http://www.wjgnet.com/1007-9327/12/6440.asp.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/msfrm.html. Accessed on: 5 December 2010.
- ↑ Prasad KN, Prasad A, Verma A, Singh AK (November 2008). "Human cysticercosis and Indian scenario: a review". J. Biosci. 33 (4): 571–82. PMID 19208982.
- ↑ 20.0 20.1 20.2 Morelli, L.; Polce, M.; Piscioli, F.; Del Nonno, F.; Covello, R.; Brenna, A.; Cione, A.; Licci, S. (2006). "Human nasal rhinosporidiosis: an Italian case report.". Diagn Pathol 1: 25. doi:10.1186/1746-1596-1-25. PMC 1560165. PMID 16945122. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1560165/.
- ↑ URL: http://www.histopathology-india.net/Rhino.htm. Accessed on: 4 January 2012.
- ↑ URL: http://www.arquivosdeorl.org.br/conteudo/acervo_eng.asp?id=428. 4 January 2012.
- ↑ 23.0 23.1 Goto, H.; Lindoso, JA. (Apr 2010). "Current diagnosis and treatment of cutaneous and mucocutaneous leishmaniasis.". Expert Rev Anti Infect Ther 8 (4): 419-33. doi:10.1586/eri.10.19. PMID 20377337.
- ↑ den Boer, ML.; Alvar, J.; Davidson, RN.; Ritmeijer, K.; Balasegaram, M. (Sep 2009). "Developments in the treatment of visceral leishmaniasis.". Expert Opin Emerg Drugs 14 (3): 395-410. doi:10.1517/14728210903153862. PMID 19708817.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 168. ISBN 978-1416054542.