Inflammatory skin disorders
Inflammatory skin disorders, also inflammatory skin diseases, are a significant part of dermatopathology. They lead to trepidation among pathologists that don't see lots of skin. Non-inflammatory skin disease is covered in dermatologic neoplasms and non-malignant skin disease.
Classification
- Bullous.
- Interface.
- Nodular & diffuse.
- Spongiotic.
- Vasculitis.
- Perivascular.
- Panniculitis.
- Psoriasiform.
Tabular comparison of inflammatory skin disease (adapted from Brinster[1][2]):
| Pattern | Key histologic feature | Subclassifications | Example | Image |
| Bullous | large "empty spaces" | -subcorneal -suprabasillar -subepidermal |
-pemphigus foliaceus -pemphigus vulgaris -dermatitis herpetiformis |
 PV (WC) |
| Interface | inflammation at DE junction | -vacuolar (minimal) -lichenoid (band-like) |
-erythema multiforme, SLE -lichen planus |
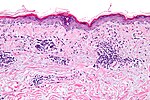 VID (WC) |
| Nodular & diffuse | intradermal inflammatory infiltrate - nodular and/or diffuse | -neutrophic -lymphocytic -plasmic -eosinophilic -histocytic |
-follicular occlusion triad, ruptured cyst/follicle -CTCL, reactive -plasma cell neoplasm, syphilis -eosinophilic cellulitis, Kimura disease -granuloma annulare, sarcoidosis, TB |
 CTCL (WC) |
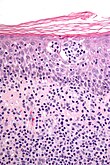
| Spongiotic | small empty spaces between keratinocytes - can see squamous bridges (best seen at high power); +/- quasi-microvacuolar appearance | -acute -subacute -chronic |
-poison ivy -nummular dermatitis -atopic dermatitis |
severe (WC), mild (WC) |
| Vasculitis | inflammation of vessel wall/vessel was destruction | -small vessel -medium vessel -large vessel |
-leukocytoclastic vasculitis -PAN -giant cell arteritis |
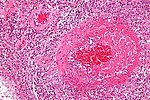 CCS (WC) |
| Perivascular | inflammation around vessels | -neutrophilic -lymphocytic -mastocytic -eosinophilic |
-cellulitis -viral exanthem, Rx reaction -mastocytosis -insect bite, Rx reaction |
|
| Panniculitis | inflammation of adipose tissue | -septal -lobular |
-erythema nodosum, scleroderma panniculitis -erythema induratum, infection |
|
| Psoriasiform | epidermal thickening and long rete ridges |
-regular -irregular |
-psoriasis -lichen simplex chronicus |
 LSC (WC) |
Notes:
- DE junction = dermal-epidermal junction.
- The "empty space" in bullous disease in situ is filled with fluid.
Non-specific patterns
Psoriasiform pattern
General
- Can be subclassified.
DDx:
- Psoriasis vulgaris (most common).
- Psoriatic arthritis.
- Drug-induced.
- Dermatomycosis (fungal infection).
- Others.
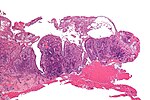
Microscopic
- Regular epidermal thickening - as very long rete ridges (described as "test tube-morphology") - key feature.
- Epidermis between rete ridges thin ("thinning of suprapapillary plate").
- Parakeratosis.
- Thin/absent granular layer.
- Dilated blood vessels in superficial dermis.
- Neutrophil clusters (Munro microabscess).
Specific diseases
Seborrheic dermatitis
General
- Very common.
Microscopic
Features:[4]
- Spongiosis (epidermal edema).
- Acanthosis (epidermal thickening).
- "Follicular lipping" = parakeratosis with neutrophils.
- Perivascular neutrophils and lymphocytes.
Lupus erythematosus
General
- A group of skin diseases - includes:
- The systemic disease, systemic lupus erythematosus, that typically has multi-organ involvement.
Microscopic
Features - classic:
- Lymphocytic interface dermatitis.[5]
- Basal layer vacuolization.[6]
- Intradermal mucin.
- Thin epidermis.
- Compact stratum corneum.
DDx:
- Discoid lupus erythematosus.
- Drug reaction (drug-induced lupus erythematosus).
- Solar elastosis - may be confused with mucin; vacuolar interface dermatitis not present
Images:
- WC:
Discoid lupus erythematosus
General
- Typically self-limited and isolated.
- It is not associated with systemic lupus erythematosus.
Microscopic
Features:[7]
- Lymphocytic interface dermatitis with basal layer vacuolation and keratinocyte apoptosis.
- Deep dermal lymphocytes.
- Basket weave stratum corneum.
- Dermal mucin.
- Thick dermal-epidermal basement membrane.
DDx:
Image:
Dermatomyositis
- For the muscle manifestations see: Neuromuscular_pathology#Dermatomyositis.
General
- Complement mediated disease - membrane attack complex.
- Usually middle age.
- Associated skin rash is common.
- May precede or follow muscle pathology.
- Associated with malignancy in approximately 10% of cases.[8]
Clinical:
- Jo-1 +ve.
Gross
- Have lesions on the knuckles - Gottron's papules.
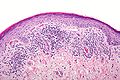
Microsopic
Features:
- Vacuolar interface dermatitis (lymphocytic inflammation at the dermal-epidermal junction).
- +/-Loss of rete ridges.
DDx:
- Lupus.
Lichen planus
- Should not be confused with lichen planus-like keratosis.
- Abbreviated LP.
General
- An oral pathology - classically.
- May be seen where the sun don't shine - penis,[9] vulva and vagina.[10]
Etiology:
- Autoimmune disease, T-cell–mediated.[11]
Clinical:[12]
- 6 Ps: pruritic (itchy), purple, polygonal, planar papules and plaques.
Note:
- Clinically, lichen planus and lichen sclerosus are similar. The main difference is lichen planus involves mucous membranes.[13]
Gross
- Wickham striae = white lines/dots.
- Due to hypergranulosis.
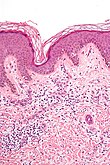
Microscopic
- Loss of basal cells (stratum basale) -- key feature.
- Loss of rete ridges/formation of pointed rete ridges "sawtoothing".
- Interface dermatitis (lymphocytes at dermal-epidermal junction).
- Hypergranulosis; stratum granulosum thickened (grossly seen as "Wickham stria" = white lines).
- Hyperkeratosis; stratum corneum thickened.
- Necrotic basal cell in dermis = colloid bodies = Civatte bodies.[16]
- Pink bodies approximately the size of a keratinocyte.
Notes:
- Hyperkeratosis and hypergranulosis are not seen in erythema multiforme.
- Colloid bodies = cytoid bodies = Civatte bodies = hyaline bodies = apoptotic bodies.[17]
DDx:
- Bullous disease, subepithelial vesicular.
- Lichenoid keratosis (lichen planus-like keratosis) - parakeratosis prominent, no oral mucosal involvement.
- Fungal infection.[18]
- Lichenoid drug reaction - unusual body site affected, separated clinically.
- Lichenoid actinic keratosis - basal atypia, solar elastosis.
Images
Stains
- PAS-D or PAS-F to exclude a fungal infection.
Sign out
FORESKIN, CIRCUMCISION: - LICHEN PLANUS.
VULVA, LEFT POSTERIOR FOURCHETTE, BIOPSY: - COMPATIBLE WITH LICHEN PLANUS.
Micro
The sections show skin with a lymphoplasmacytic interface dermatitis, basal cell loss, hypergranulosis, hyperkeratosis, loss of the rete ridges and Civatte bodies.
The epidermis matures to the surface. No significant nuclear atypia is identified.
Fungal organisms are not identified with a PAS-D stain.
Lichen sclerosus
Microscopic
Features:[19]
- Subepithelial fibrosis - key feature.
Psoriasis
General
- Chronic skin condition +/- systemic involvement:[20]
- Arthritis, i.e. psoriatic arthritis.
- Myopathy.
- Enteropathy, e.g. inflammatory bowel disease.
- Syondylitic joint disease (spondylos = vertebrae[21]).
- Other considerations:
- Drug-induced psoriasis.[22]
Clinical
- Auspitz sign = pin-point bleeding on removal of scale.
- Koebner phenomenon = lesions form at site of trauma.
Common locations:[20]
- Knees, elbows, scalp, glands penis.
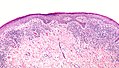
Microscopic
Features:[20]
- "Regular" acanthosis + long rete ridges (psoriasiform hyperplasia).
- "Regular" (psoriasiform change) = rete ridges are of similar length and thickness.
- Parakeratosis.
- Dilated vessels in superficial dermis (give rise to Auspitz sign).
- Spongiform pustules = PMNs in stratum spinosum.
- PMNs in parakeratotic stratum corneum (Munro microabscess).
- Thinning of the suprapapillary plate.
- The epidermis between rete ridges is thinner than in the normal adjacent skin - key feature.
DDx:
- Dermatomycosis (fungal infection).
- Drug reaction.
Note:
- Dermatophytosis = ring worm; dermatophystosis != dermatomycosis.
Images
www:
Stains
- PASD stain -ve for fungal organisms.
Sign out
SKIN LESION, LEFT ARM, PUNCH BIOPSY: - SKIN WITH ACANTHOSIS, HYPERKERATOSIS, FOCAL PARAKERATOSIS, PROMINENT DILATED VESSELS IN THE SUPERFICIAL DERMIS, SUPERFICIAL SPONGIFORM PUSTULES. - MILD NONSPECIFIC PERIVASCULAR INFLAMMATION. - NEGATIVE FOR FUNGAL ORGANISMS WITH PAS STAINING. COMMENT: The findings are compatible with psoriasis.
Micro
The sections show skin with acanthosis, hyperkeratosis, focal parakeratosis, prominent dilated vessels in the superficial dermis, superficial clusters of intraepidermal neutrophils (spongiform pustules) and thinning of the suprapapillary plate is present. A few perivascular inflammatory cells are present.
There is no epidermal necrosis. Eosinophils are not apparent. The lymphocytes do not have significant atypia.
Lichen striatus
General
Features:[24]
- Benign, self-limited.
Clinical:
- Linear rash usu. on lower extremity.
- Associated with atopy, lichen sclerosus.[24]
- Children.
Clinical image:
Microscopic
Features:
- "Ball and glove" pattern:
- Rete ridges (glove) surround nexts of lymphocytes (ball).
- Hyperkeratosis.
- Parakeratosis.
DDx:
Images:
Lichen aureus
General
- Rare.
Clinical:[25]
- Plaques + minimal scale - erythematous/golden.
Microscopic
Features:[25]
- Lymphocyte-predominant perivascular pattern.
- May have features suggestive of vacuolar interface pattern.
- Fibrosis of superficial papillary dermis.
Images:
Granuloma faciale
General
- Considered a vasculitis.[26]
Microscopic
Features:[27]
- Neutrophilic vasculitis - often subtle:
- Neutrophils within blood vessel walls.
- Vessels destruction (fibrinoid necrosis or nuclear dust).
- Mixed inflammatory superficial dermal infiltrate.
- Eosinophils, neutrophils, plasma cells, histiocytes.
- Lesion separated from the (normal) epidermis (Grenz zone).[26]
DDx of chronic fibrosing leukocytoclastic vasculitis:[27]
- Granuloma faciale.
- Erythema elevatum diutinum - lacks Grenz zone.
- Inflammatory pseudotumour.
Image:
Atopic dermatitis
General
- Very common - especially in children.[28]
- Most children outgrow the condition.
Microscopic
Features:
- Spongiotic dermatitis.
DDx:
Images
Sweet syndrome
General
- Uncommon.
Microscopic
Features:
- Nodular and diffuse pattern - neutrophils predominant - without pus.
DDx rips:
- Rheumatoid neutrophilic dermatitis.
- Bowel-associated dermatosis-arthritis syndrome.
- Pyoderma gangrenosum.
- Sweet syndrome.
Image:
Granuloma inguinale
- Not to be confused with granuloma annulare.
- Previously known as donovanosis.
General
- Infection caused by Klebsiella granulomatis - Gram-negative, rod-shaped bacteria.
- Used to be known as Calymmatobacterium granulomatis.[30]
Location:
Clinical:[31]
- Sexually transmitted.
- Nodule or papule developing into a painless ulcer in the inguinal region.
- No lymphadenopathy (unlike syphilis).
Microscopic
Features:
- Donovan bodies - key feature:
- Rod-shaped bodies within histiocytes.
DDx:
Image:
Stains
- Giemsa stain - highlights organisms.
Pyoderma gangrenosum
General
Clinical
Gross
- Skin ulceration - classically on the legs.[32]
Microscopic
Features:[32]
- Early: lymphocytes cells only in the dermis - often perivascular & vascular.
- +/-Fibrinoid necrosis of vessels at edge of lesion.
- Late: abscess formation (neutrophils).
DDx:
Image:
Necrobiotic xanthogranuloma
- Abbreviated NXG.
General
- Usually elderly.[34]
Gross
Features:
- Periorbital - classic location.[35]
Microscopic
Features:[34]
- "Necrobiotic granuloma":
- Palisading granuloma with a core collagen-like material.
- +/-Cholesterol clefts - common.
- +/-Touton giant cells.
- +/-Atypical foreign body-type giant cells +/- asteroid bodies.
DDx:
- Granuloma annulare.
- Necrobiosis lipoidica - has plasma cells.
- Granuloma-forming infections - positive stains for microorganisms.
Image:
DDx for pattern
Spongiotic dermatitides
DDx:[1]
- Atopic dermatitis.
- Contact dermatitis.
- Stasis dermatitis.
- Seborrheic dermatitis.
- Nummular dermatitis.
- Spongiotic drug eruption.
Psoriasiform dermatitides
Regular psoriasiform dermatitis
DDx:[1]
- Psoriasis vulgaris.
- Dermatophyte infection.
- Pityriasis rubra pilaris.
Irregular psoriasiform dermatitis
Interface dermatitides
Vacuolar interface dermatitides
DDx:[1]
- Erythema multiforme.
- Lichen sclerosus.
- Fixed drug eruption.
Others:[1]
- Graft versus host disease.
- Dermatomyositis.
- Systemic lupus erythematosus.
- Morbillifrom viral exanthem.
Additional:[36]
- Phototoxic dermatitis.
- Acute radiation dermatitis.
- Erythema multiforme-like drug eruption.
- Lichen sclerosis et atrophicus.
- Erythema dyschromicum perstans (ashy dermatosis).
Super lame mnemonic Danny G & SLE:
- Dermatomyositis, GVHD, SLE, Lichen sclerosus, Erythema multiforme.
Lichenoid interface dermatitides
DDx:[1]
- Lichen planus
- Mycosis fungoides.
- Discoid lupus erythematosus.
- Lichenoid drug eruption.
- Fixed drug eruption.
Additional:[36]
- Lichen planus-like keratosis.
- Lichenoid actinic keratosis.
- Lichen nitidus.
- Pigmented purpuric dermatosis.
- Lichen amyloidosis.
- Pityriasis lichenoides chronica.
- HIV dermatitis.
- Syphilis.
- Urticaria pigmentosa.
- Chronic graft versus host disease.
Bullous disease
Subcorneal bullous disorders
DDx with acantholysis:[1]
DDx without acantholysis:DDx:[1]
- Subcorneal pustular dermatosis (Sneddon-Wilkinson disease).
- Pustular psoriasis.
- Pustular drug eruption (acute generalized exanthematous pustulosis).
Suprabasilar bullous disorders
DDx:[1]
- Pemphigus vulgaris.
- Hailey-Hailey disease (benign familial pemphigus).
- Darier disease.
- Grover disease (transient acantholytic dermatosis).
Memory device - PhD + Grover = Pemphigus vulgaris, Hailey-Hailey, Darier, Grover.
Subepidermal bullous disorders
DDx:[1]
- Bullous pemphigoid.
- Cicatricial pemphigoid.
- Porphyria cutanea tarda.
- Epidermolysis bullosa acquista.
- Dermatitis herpetiformis.
- Linear IgA disease.
Others:
- Insect bite.
- Coma blister.
- Bullous systemic lupus erythematosus.
Mnemonic DELPHI:
- Dermatitis herpetiformis.
- Epidermolysis bullosa acquisita.
- Bullous lupus erythematosis.
- Pemphigoid, bullous.
- Herpes gestationis - rare autoimmune bullous dermatosis of pregnancy, not related to HSV.[37]
- Linear IgA disease.
Dermatitides with perivascular inflammation
Lymphocytes
Lymphocytes (tightly cuffed):[1]
- Infections.
- Medications.
- Malignancy.
- Vitiligo (with absent melanocytes).
- Scleroderma/morphea.
Lymphocytes & plasma cells +/-eosinophils:
- Erythema chronicum migrans (Lyme disease).
Lymphocytes (not tightly cuffed):
- Viral exanthems.
- Drug eruptions.
Lymphocytes & eosinophils:
- Drug reaction.
- Insect bite.
- Dermatophyte infection.
A simple memory device - 6 Ls:[38]
- Lymphoma.
- Pseudolymphoma (cutaneous lymphoid hyperplasia, lymphocytoma cutis).
- Lupus erythematosus.
- Lymphocytic infiltrate of Jessner / tumid lupus erythematosus.
- Polymorphous light eruption.
- Lyme disease.
Neutrophils
DDx:[1]
- Cellulitis.
- Neutrophilic eccrine hidradenitis (idiopathic palmar-plantar hidradenitis)
With eosinophils:
- Urticaria.
Eosinophils
DDx:[1]
- Hypersensitivity reaction/drug reaction.
- Insect bite.
- Bullous pemphigoid, urticarial.
Mast cells
Vasculitis
General DDx:
- Infection.
- Autoimmune.
- Malignancy.
- Toxic (medications).
Small vessel:
Medium vessel:
Medium vessels often with small vessel involvement:
- Churg-Strauss syndrome.
- Microscopic polyangiitis.
- Mixed cryoglobulinemia.
- Connective tissue diseases.
Large vessel:
Nodular and diffuse dermatitides
Neutrophils
With pus (suppurative)
Neutrophils only:
- Follicular occlusion triad.
- Ruptured cyst/follicle.
Neutrophils and eosinophils:
- Halogenoderma.
- Blastomycosis-like pyoderma (pyoderma vegetans) - due to bacterial infection, usu. S. aureus.
Without pus
With vasculitis:
- Neutrophils only: see vasculitides.
- Mixed infiltrate: granuloma faciale, erythema elevatinum diutinum.
Without vasculitis:
- Sweet syndrome.
- Pyoderma gangrenosum.
- Rheumatoid neutrophilic dermatitis.
- Bowel-associated dermatosis-arthritis syndrome.
Lymphocytes
- Reactive lymphoid hyperplasia - may be due to drugs.
- Lymphoid malignancy.
Plasma cells
- Inflammation.
- Plasma cell neoplasms.
- Infections:
- Syphilis - lichenoid/psoriasiform pattern.
- Chancroid.
- Granuloma inguinale.
- Lymphogranuloma venereum.
Eosinophils
- Eosinophilic cellulitis (Wells syndrome).
- Insect bites.
- Hypereosinophilic syndrome (HES).
- Angiolymphoid hyperplasia with eosinophilia (ALHE).
- Kimura disease.
Histiocytes
Granulomatous
Sarcoidal
- Sarcoidosis - have few lymphoid cells around them; thus called "naked granulomas".[2]
Tuberculoid
- Tuberculosis.
- Tertiary syphilis - usu. abundant plasma cells.
- Cutaneous leishmaniasis.
Foreign body-type granulomas
Palisaded granumolas
Blue granuloma:
- Granuloma annulare.
- Wegener granulomatosis.
- Rheumatoid vasculitis.
Red granuloma:
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Brinster NK (March 2008). "Dermatopathology for the surgical pathologist: a pattern based approach to the diagnosis of inflammatory skin disorders (part I)". Adv Anat Pathol 15 (2): 76–96. doi:10.1097/PAP.0b013e3181664e8d. PMID 18418089.
- ↑ 2.0 2.1 Brinster, NK. (Nov 2008). "Dermatopathology for the surgical pathologist: a pattern-based approach to the diagnosis of inflammatory skin disorders (part II).". Adv Anat Pathol 15 (6): 350-69. doi:10.1097/PAP.0b013e31818b1ac6. PMID 18948765.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1191. ISBN 978-1416031215.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1191. ISBN 978-1416031215.
- ↑ JAH. 20 February 2009.
- ↑ Crowson AN, Magro CM, Mihm MC (April 2008). "Interface dermatitis". Arch. Pathol. Lab. Med. 132 (4): 652–66. PMID 18384217. http://www.archivesofpathology.org/doi/full/10.1043/1543-2165%282008%29132%5B652%3AID%5D2.0.CO%3B2.
- ↑ URL: http://www.dermpedia.org/baby-dermpedia-for-beginners/discoid-lupus-erythematosus. Accessed on: 7 March 2012.
- ↑ Chen YJ, Wu CY, Huang YL, Wang CB, Shen JL, Chang YT (2010). "Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan". Arthritis Res. Ther. 12 (2): R70. doi:10.1186/ar2987. PMC 2888225. PMID 20398365. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2888225/.
- ↑ Teichman, JM.; Sea, J.; Thompson, IM.; Elston, DM. (Jan 2010). "Noninfectious penile lesions.". Am Fam Physician 81 (2): 167-74. PMID 20082512.
- ↑ Gupta, R.; Bansal, B.; Singh, S.; Yadav, I.; Gupta, K.; Kudesia, M. (2009). "Lichen planus of uterine cervix - the first report of a novel site of occurrence: a case report.". Cases J 2: 9306. doi:10.1186/1757-1626-2-9306. PMID 20062629.
- ↑ URL: http://emedicine.medscape.com/article/1078327-overview. Accessed on: 11 September 2010.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1191. ISBN 978-1416031215.
- ↑ McPherson, T.; Cooper, S.. "Vulval lichen sclerosus and lichen planus.". Dermatol Ther 23 (5): 523-32. doi:10.1111/j.1529-8019.2010.01355.x. PMID 20868406.
- ↑ URL: http://emedicine.medscape.com/article/1078327-overview. Accessed on: 11 September 2010.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1192. ISBN 978-1416031215.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 604. ISBN 978-1416054542.
- ↑ URL: http://www.careforumwales.org/cell-carcinoma/histopathologic-terminology.html. Accessed on: 28 August 2011.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 36. ISBN 978-0443066542.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1065-6. ISBN 0-7216-0187-1.
- ↑ 20.0 20.1 20.2 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 603. ISBN 978-1416054542.
- ↑ URL: http://medical-dictionary.thefreedictionary.com/spondylosis. Accessed on: 28 August 2011.
- ↑ Milavec-Puretić, V.; Mance, M.; Ceović, R.; Lipozenčić, J. (Mar 2011). "Drug induced psoriasis.". Acta Dermatovenerol Croat 19 (1): 39-42. PMID 21489366.
- ↑ URL: http://missinglink.ucsf.edu/lm/dermatologyglossary/psoriasis.html. Accessed on: 4 September 2013.
- ↑ 24.0 24.1 Taniguchi Abagge, K.; Parolin Marinoni, L.; Giraldi, S.; Carvalho, VO.; de Oliveira Santini, C.; Favre, H.. "Lichen striatus: description of 89 cases in children.". Pediatr Dermatol 21 (4): 440-3. doi:10.1111/j.0736-8046.2004.21403.x. PMID 15283785.
- ↑ 25.0 25.1 Hazan, C.; Fangman, B.; Cohen, D. (2007). "Lichen aureus.". Dermatol Online J 13 (1): 23. PMID 17511956.
- ↑ 26.0 26.1 URL: http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309. Accessed on: 23 September 2011.
- ↑ 27.0 27.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 198-9. ISBN 978-0443066542.
- ↑ URL: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001856/. Accessed on: 28 December 2011.
- ↑ URL: http://dermatology.cdlib.org/94/NYU/Apr2002/7.html. Accessed on: 4 January 2012.
- ↑ O'Farrell N (December 2002). "Donovanosis". Sex Transm Infect 78 (6): 452–7. PMC 1758360. PMID 12473810. http://sti.bmj.com/cgi/pmidlookup?view=long&pmid=12473810.
- ↑ Bezerra, SM.; Jardim, MM.; Silva, VB. (Jun 2011). "Granuloma inguinale (Donovanosis).". An Bras Dermatol 86 (3): 585-6. PMID 21738983.
- ↑ 32.0 32.1 32.2 Brooklyn, T.; Dunnill, G.; Probert, C. (Jul 2006). "Diagnosis and treatment of pyoderma gangrenosum.". BMJ 333 (7560): 181-4. doi:10.1136/bmj.333.7560.181. PMC 1513476. PMID 16858047. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1513476/.
- ↑ Wong, WW.; Machado, GR.; Hill, ME.. "Pyoderma gangrenosum: the great pretender and a challenging diagnosis.". J Cutan Med Surg 15 (6): 322-8. PMID 22202507.
- ↑ 34.0 34.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 629. ISBN 978-0443066542.
- ↑ Fernández-Herrera, J.; Pedraz, J. (Jun 2007). "Necrobiotic xanthogranuloma.". Semin Cutan Med Surg 26 (2): 108-13. doi:10.1016/j.sder.2007.02.008. PMID 17544963.
- ↑ 36.0 36.1 Alsaad, KO.; Ghazarian, D. (Dec 2005). "My approach to superficial inflammatory dermatoses.". J Clin Pathol 58 (12): 1233-41. doi:10.1136/jcp.2005.027151. PMC 1770784. PMID 16311340. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770784/.
- ↑ URL: http://emedicine.medscape.com/article/1063499-overview. Accessed on: 23 September 2011.
- ↑ URL: http://www.dermpathmd.com/mnemonics/mnemonics_dermatopathology.htm. Accessed on: 23 September 2011.