Difference between revisions of "Inflammatory skin disorders"
m (→Eosinophils) |
|||
| (148 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Inflammatory skin disorders''', also '''inflammatory skin diseases''', are a significant part of [[dermatopathology]]. They lead to trepidation among pathologists that don't see lots of skin. | '''Inflammatory skin disorders''', also '''inflammatory skin diseases''', are a significant part of [[dermatopathology]]. They lead to trepidation among pathologists that don't see lots of skin. Non-inflammatory skin disease is covered in ''[[dermatologic neoplasms]]'' and ''[[non-malignant skin disease]]''. | ||
=Classification= | =Classification= | ||
| Line 11: | Line 11: | ||
*Psoriasiform. | *Psoriasiform. | ||
'''Tabular comparison of inflammatory skin disease (adapted from ''Brinster''<ref name=pmid18418089>{{cite journal |author=Brinster NK |title=Dermatopathology for the surgical pathologist: a pattern based approach to the diagnosis of inflammatory skin disorders (part I) |journal=Adv Anat Pathol |volume=15 |issue=2 |pages=76–96 |year=2008 |month=March |pmid=18418089 |doi=10.1097/PAP.0b013e3181664e8d |url=}}</ref>):''' | '''Tabular comparison of inflammatory skin disease (adapted from ''Brinster''<ref name=pmid18418089>{{cite journal |author=Brinster NK |title=Dermatopathology for the surgical pathologist: a pattern based approach to the diagnosis of inflammatory skin disorders (part I) |journal=Adv Anat Pathol |volume=15 |issue=2 |pages=76–96 |year=2008 |month=March |pmid=18418089 |doi=10.1097/PAP.0b013e3181664e8d |url=}}</ref><ref name=pmid18948765>{{Cite journal | last1 = Brinster | first1 = NK. | title = Dermatopathology for the surgical pathologist: a pattern-based approach to the diagnosis of inflammatory skin disorders (part II). | journal = Adv Anat Pathol | volume = 15 | issue = 6 | pages = 350-69 | month = Nov | year = 2008 | doi = 10.1097/PAP.0b013e31818b1ac6 | PMID = 18948765 }}</ref>):''' | ||
{| class="wikitable" | {| class="wikitable" | ||
| '''Pattern''' | | '''Pattern''' | ||
| Line 17: | Line 17: | ||
| '''Subclassifications''' | | '''Subclassifications''' | ||
| '''Example''' | | '''Example''' | ||
| '''Image''' | |||
|- | |- | ||
| [[Bullous disease|Bullous]] | | [[Bullous disease|Bullous]] | ||
| "empty | | large "empty spaces" | ||
| -subcorneal<br>-suprabasillar<br>-subepidermal | | -subcorneal<br>-suprabasillar<br>-subepidermal | ||
| -pemphigus foliaceus<br>-[[pemphigus vulgaris]]<br>-[[dermatitis herpetiformis]] | | -[[pemphigus foliaceus]]<br>-[[pemphigus vulgaris]]<br>-[[dermatitis herpetiformis]] | ||
| [[Image:Pemphigus_vulgaris_-_low_mag.jpg|thumb|150px|center|[[pemphigus vulgaris|PV]] (WC)]] | |||
|- | |- | ||
| Interface | | [[Interface_dermatitides|Interface]] | ||
| inflammation at DE junction | | inflammation at DE junction | ||
| -vacuolar (minimal)<br>-lichenoid (band-like) | | -vacuolar (minimal)<br>-lichenoid (band-like) | ||
| -[[erythema multiforme]], [[SLE]]<br>-[[lichen planus]] | | -[[erythema multiforme]], [[SLE]]<br>-[[lichen planus]] | ||
| [[Image:Vacuolar interface dermatitis - high mag.jpg|thumb|center|150px|[[vacuolar interface dermatitis|VID]] (WC)]] | |||
|- | |- | ||
| Nodular & diffuse | | [[Nodular and diffuse dermatitides|Nodular & diffuse]] | ||
| intradermal inflammatory infiltrate - nodular and/or diffuse | | intradermal inflammatory infiltrate - nodular and/or diffuse | ||
| - | | -neutrophic<br>-lymphocytic<br>-plasmic<br>-eosinophilic<br>-histocytic | ||
| - | | -follicular occlusion triad, ruptured cyst/follicle<br>-[[CTCL]], reactive<br>-[[plasma cell neoplasm]], [[syphilis]]<br>-eosinophilic cellulitis, [[Kimura disease]]<br>-[[granuloma annulare]], [[sarcoidosis]], [[TB]] | ||
| [[Image:Cutaneous_T-cell_lymphoma_-_very_high_mag.jpg|thumb|center|110px|[[CTCL]] (WC)]] | |||
|- | |- | ||
| Spongiotic | | [[Spongiotic_dermatitides|Spongiotic]] | ||
| | | small empty spaces between keratinocytes - can see squamous bridges (best seen at high power); +/- quasi-microvacuolar appearance | ||
| -acute<br>-subacute<br>-chronic | | -acute<br>-subacute<br>-chronic | ||
| -poison ivy<br>-nummular dermatitis<br>-atopic dermatitis | | -poison ivy<br>-nummular dermatitis<br>-[[atopic dermatitis]] | ||
| [http://commons.wikimedia.org/wiki/File:Spongiotic_dermatitis_%282%29_Dyshidrotic_.JPG severe (WC)], [http://commons.wikimedia.org/wiki/File:Spongiotic_dermatitis_-_very_high_mag.jpg mild (WC)] | |||
|- | |- | ||
| [[Vasculitis]] | | [[Vasculitis]] | ||
| Line 42: | Line 47: | ||
| -small vessel <br> -medium vessel <br> -large vessel | | -small vessel <br> -medium vessel <br> -large vessel | ||
| -[[leukocytoclastic vasculitis]]<br>-[[PAN]]<br>-[[giant cell arteritis]] | | -[[leukocytoclastic vasculitis]]<br>-[[PAN]]<br>-[[giant cell arteritis]] | ||
| [[Image:Churg-Strauss_syndrome_-_high_mag.jpg |thumb|150px|[[Eosinophilic granulomatosis with polyangiitis|EGPA]] (WC)]] | |||
|- | |- | ||
| Perivascular | | [[Dermatitides_with_perivascular_inflammation|Perivascular]] | ||
| inflammation around vessels | | inflammation around vessels | ||
| | | -neutrophilic<br>-lymphocytic<br>-mastocytic<br>-eosinophilic | ||
| | | -[[cellulitis]]<br>-viral exanthem, Rx reaction<br>-[[mastocytosis]]<br>-insect bite, Rx reaction | ||
| [[Image:Dermal_perivascular_lymphoeosinophilic_infiltrate_-_high_mag.jpg |thumb|center|110px|DPLI (WC)]] | |||
|- | |- | ||
| [[Panniculitis]] | | [[Panniculitis]] | ||
| inflammation of adipose tissue | | inflammation of adipose tissue | ||
| -septal<br>- | | -septal<br>-lobular | ||
| -[[erythema nodosum]], scleroderma panniculitis<br>-[[erythema induratum]], infection | | -[[erythema nodosum]], [[scleroderma panniculitis]]<br>-[[erythema induratum]], infection | ||
| | |||
|- | |- | ||
| Psoriasiform | | [[Psoriasiform dermatitides|Psoriasiform]] | ||
| epidermal thickening<br>and long rete ridges | | epidermal thickening<br>and long rete ridges | ||
| -regular<br>-irregular | | -regular<br>-irregular | ||
| -psoriasis<br>-[[lichen simplex chronicus]] | | -[[psoriasis]]<br>-[[lichen simplex chronicus]] | ||
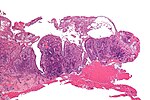
| [[Image:Lichen_simplex_chronicus_-_very_low_mag.jpg|thumb|150px|center|[[Lichen simplex chronicus|LSC]] (WC)]] | |||
|} | |} | ||
Notes: | Notes: | ||
| Line 71: | Line 80: | ||
*Psoriatic arthritis. | *Psoriatic arthritis. | ||
*Drug-induced. | *Drug-induced. | ||
*[[Dermatomycosis]] (fungal infection). | |||
*Others. | *Others. | ||
| Line 89: | Line 99: | ||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref>{{Ref PBoD8|1191}}</ref> | Features:<ref>{{Ref PBoD8|1191}}</ref> | ||
*Spongiosis (epidermal edema). | *[[Spongiosis]] (epidermal edema). | ||
*Acanthosis (epidermal thickening). | *Acanthosis (epidermal thickening). | ||
*"Follicular lipping" = parakeratosis with neutrophils. | *"Follicular lipping" = parakeratosis with neutrophils. | ||
*Perivascular neutrophils and lymphocytes. | *Perivascular neutrophils and lymphocytes. | ||
== | ==Lupus erythematosus== | ||
===General=== | ===General=== | ||
* | *A group of skin diseases - includes: | ||
**The systemic disease, [[systemic lupus erythematosus]], that typically has multi-organ involvement. | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features - classic: | ||
*Lymphocytic interface dermatitis.<ref>JAH. 20 February 2009.</ref> | *Lymphocytic interface dermatitis.<ref>JAH. 20 February 2009.</ref> | ||
*Basal layer | *Basal layer vacuolization.<ref name=pmid18384217>{{cite journal |author=Crowson AN, Magro CM, Mihm MC |title=Interface dermatitis |journal=Arch. Pathol. Lab. Med. |volume=132 |issue=4 |pages=652–66 |year=2008 |month=April |pmid=18384217 |doi= |url=http://www.archivesofpathology.org/doi/full/10.1043/1543-2165%282008%29132%5B652%3AID%5D2.0.CO%3B2}}</ref> | ||
*Intradermal mucin. | *Intradermal mucin. | ||
*Thin epidermis. | |||
*Compact stratum corneum. | |||
DDx: | |||
*[[Discoid lupus erythematosus]]. | |||
*Drug reaction (drug-induced lupus erythematosus). | |||
*[[Solar elastosis]] - may be confused with ''mucin''; vacuolar interface dermatitis ''not'' present | |||
====Images==== | |||
<gallery> | |||
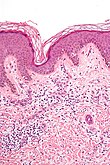
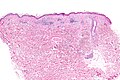
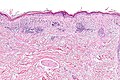
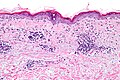
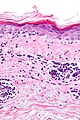
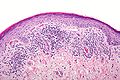
Image:Vacuolar_interface_dermatitis_-_low_mag.jpg | Vacuolar interface dermatitis with dermal mucin - low mag. (WC) | |||
Image:Vacuolar_interface_dermatitis_-_intermed_mag.jpg | Vacuolar interface dermatitis with dermal mucin - intermed. mag. (WC) | |||
Image:Vacuolar_interface_dermatitis_-_high_mag.jpg | Vacuolar interface dermatitis with dermal mucin - high mag. (WC) | |||
Image:Vacuolar_interface_dermatitis_-_very_high_mag.jpg | Vacuolar interface dermatitis with dermal mucin - very high mag. (WC) | |||
</gallery> | |||
==Discoid lupus erythematosus== | |||
===General=== | |||
*Typically self-limited and isolated. | |||
**It is '''not''' associated with ''[[systemic lupus erythematosus]]''. | |||
===Microscopic=== | |||
Features:<ref>URL: [http://www.dermpedia.org/baby-dermpedia-for-beginners/discoid-lupus-erythematosus http://www.dermpedia.org/baby-dermpedia-for-beginners/discoid-lupus-erythematosus]. Accessed on: 7 March 2012.</ref> | |||
*Lymphocytic interface dermatitis with basal layer vacuolation and keratinocyte apoptosis. | |||
*Deep dermal lymphocytes. | |||
*Basket weave stratum corneum. | |||
*Dermal mucin. | |||
*Thick dermal-epidermal basement membrane. | |||
DDx: | |||
*[[Lupus erythematosus]]. | |||
Image: | |||
*[http://www.dermpedia.org/baby-dermpedia-for-beginners/discoid-lupus-erythematosus DLE (dermpedia.org)]. | |||
==Dermatomyositis== | ==Dermatomyositis== | ||
| Line 113: | Line 157: | ||
**May precede or follow muscle pathology. | **May precede or follow muscle pathology. | ||
*Associated with malignancy in approximately 10% of cases.<ref name=pmid20398365>{{cite journal |author=Chen YJ, Wu CY, Huang YL, Wang CB, Shen JL, Chang YT |title=Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan |journal=Arthritis Res. Ther. |volume=12 |issue=2 |pages=R70 |year=2010 |pmid=20398365 |pmc=2888225 |doi=10.1186/ar2987 |url=}}</ref> | *Associated with malignancy in approximately 10% of cases.<ref name=pmid20398365>{{cite journal |author=Chen YJ, Wu CY, Huang YL, Wang CB, Shen JL, Chang YT |title=Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan |journal=Arthritis Res. Ther. |volume=12 |issue=2 |pages=R70 |year=2010 |pmid=20398365 |pmc=2888225 |doi=10.1186/ar2987 |url=}}</ref> | ||
Clinical: | |||
*Jo-1 +ve. | |||
===Gross=== | ===Gross=== | ||
| Line 119: | Line 166: | ||
===Microsopic=== | ===Microsopic=== | ||
Features: | Features: | ||
* | *Vacuolar interface dermatitis (lymphocytic inflammation at the dermal-epidermal junction). | ||
*Loss of rete ridges. | *+/-Loss of rete ridges. | ||
DDx: | |||
*Lupus. | |||
==Lichen planus== | ==Lichen planus== | ||
:''Should '''not''' be confused with [[lichen planus-like keratosis]]''. | |||
*Abbreviated ''LP''. | |||
===General=== | ===General=== | ||
*An oral pathology. | *An [[oral pathology]] - classically. | ||
*May be seen where the sun don't shine - [[penis]],<ref name=pmid20082512>{{Cite journal | last1 = Teichman | first1 = JM. | last2 = Sea | first2 = J. | last3 = Thompson | first3 = IM. | last4 = Elston | first4 = DM. | title = Noninfectious penile lesions. | journal = Am Fam Physician | volume = 81 | issue = 2 | pages = 167-74 | month = Jan | year = 2010 | doi = | PMID = 20082512 }}</ref> [[vulva]] and [[vagina]].<ref name=pmid20062629>{{Cite journal | last1 = Gupta | first1 = R. | last2 = Bansal | first2 = B. | last3 = Singh | first3 = S. | last4 = Yadav | first4 = I. | last5 = Gupta | first5 = K. | last6 = Kudesia | first6 = M. | title = Lichen planus of uterine cervix - the first report of a novel site of occurrence: a case report. | journal = Cases J | volume = 2 | issue = | pages = 9306 | month = | year = 2009 | doi = 10.1186/1757-1626-2-9306 | PMID = 20062629 }}</ref> | *May be seen where the sun don't shine - [[penis]],<ref name=pmid20082512>{{Cite journal | last1 = Teichman | first1 = JM. | last2 = Sea | first2 = J. | last3 = Thompson | first3 = IM. | last4 = Elston | first4 = DM. | title = Noninfectious penile lesions. | journal = Am Fam Physician | volume = 81 | issue = 2 | pages = 167-74 | month = Jan | year = 2010 | doi = | PMID = 20082512 }}</ref> [[vulva]] and [[vagina]].<ref name=pmid20062629>{{Cite journal | last1 = Gupta | first1 = R. | last2 = Bansal | first2 = B. | last3 = Singh | first3 = S. | last4 = Yadav | first4 = I. | last5 = Gupta | first5 = K. | last6 = Kudesia | first6 = M. | title = Lichen planus of uterine cervix - the first report of a novel site of occurrence: a case report. | journal = Cases J | volume = 2 | issue = | pages = 9306 | month = | year = 2009 | doi = 10.1186/1757-1626-2-9306 | PMID = 20062629 }}</ref> | ||
| Line 133: | Line 185: | ||
*6 Ps: pruritic (itchy), purple, polygonal, planar papules and plaques. | *6 Ps: pruritic (itchy), purple, polygonal, planar papules and plaques. | ||
Note: | |||
*Clinically, lichen planus and [[lichen sclerosus]] are similar. The main difference is lichen planus involves mucous membranes.<ref name=pmid20868406>{{Cite journal | last1 = McPherson | first1 = T. | last2 = Cooper | first2 = S. | title = Vulval lichen sclerosus and lichen planus. | journal = Dermatol Ther | volume = 23 | issue = 5 | pages = 523-32 | month = | year = | doi = 10.1111/j.1529-8019.2010.01355.x | PMID = 20868406 }}</ref> | |||
===Gross=== | ===Gross=== | ||
*Wickham striae = white lines/dots. | *Wickham striae = white lines/dots. | ||
| Line 145: | Line 199: | ||
*Hyperkeratosis; stratum corneum thickened. | *Hyperkeratosis; stratum corneum thickened. | ||
*Necrotic basal cell in dermis = colloid bodies = Civatte bodies.<ref name=Ref_PCPBoD8_604>{{Ref PCPBoD8|604}}</ref> | *Necrotic basal cell in dermis = colloid bodies = Civatte bodies.<ref name=Ref_PCPBoD8_604>{{Ref PCPBoD8|604}}</ref> | ||
**Pink bodies approximately the size of a keratinocyte. | |||
Notes: | |||
*Hyperkeratosis and hypergranulosis are not seen in [[erythema multiforme]]. | |||
*Colloid bodies = cytoid bodies = Civatte bodies = hyaline bodies = apoptotic bodies.<ref>URL: [http://www.careforumwales.org/cell-carcinoma/histopathologic-terminology.html http://www.careforumwales.org/cell-carcinoma/histopathologic-terminology.html]. Accessed on: 28 August 2011.</ref> | |||
**DDx: [[systemic lupus erythematosus]], [[lichen planus]], and [[graft-versus-host disease]]. | |||
DDx: | DDx: | ||
*[[Bullous disease]], subepithelial vesicular. | *[[Bullous disease]], subepithelial vesicular. | ||
*[[Lichenoid keratosis]] - parakeratosis prominent. | *[[Lichenoid keratosis]] (lichen planus-like keratosis) - parakeratosis prominent, no oral mucosal involvement. | ||
*Fungal infection.<ref name=Ref_Derm36>{{Ref Derm|36}}</ref> | |||
*Lichenoid drug reaction - unusual body site affected, separated clinically. | |||
*Lichenoid [[actinic keratosis]] - basal atypia, [[solar elastosis]]. | |||
====Images==== | |||
<gallery> | |||
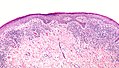
Image:Lichen_planus_intermed_mag.jpg | Lichen planus - intermed. mag. (WC/Nephron) | |||
Image:Lichen_planus_low_mag.jpg | Lichen planus - low mag. (WC/Nephron) | |||
</gallery> | |||
===Stains=== | |||
*PAS-D or PAS-F to exclude a fungal infection. | |||
===Sign out=== | |||
<pre> | |||
FORESKIN, CIRCUMCISION: | |||
- LICHEN PLANUS. | |||
</pre> | |||
<pre> | |||
VULVA, LEFT POSTERIOR FOURCHETTE, BIOPSY: | |||
- COMPATIBLE WITH LICHEN PLANUS. | |||
</pre> | |||
====Micro==== | |||
The sections show skin with a lymphoplasmacytic interface dermatitis, basal cell loss, hypergranulosis, hyperkeratosis, loss of the rete ridges and Civatte bodies. | |||
The epidermis matures to the surface. No significant nuclear atypia is identified. | |||
Fungal organisms are not identified with a PAS-D stain. | |||
==Lichen sclerosus== | ==Lichen sclerosus== | ||
| Line 169: | Line 250: | ||
===General=== | ===General=== | ||
*Chronic skin condition +/- systemic involvement:<ref name=Ref_PCPBoD8_603>{{Ref PCPBoD8|603}}</ref> | *Chronic skin condition +/- systemic involvement:<ref name=Ref_PCPBoD8_603>{{Ref PCPBoD8|603}}</ref> | ||
**[[Arthritis]]. | **[[Arthritis]], i.e. psoriatic arthritis. | ||
**[[Myopathy]]. | **[[Myopathy]]. | ||
**Enteropathy, e.g. [[inflammatory bowel disease]]. | **Enteropathy, e.g. [[inflammatory bowel disease]]. | ||
**Syondylitic joint disease (spondylos = vertebrae<ref>URL: [http://medical-dictionary.thefreedictionary.com/spondylosis http://medical-dictionary.thefreedictionary.com/spondylosis]. Accessed on: 28 August 2011.</ref>). | **Syondylitic joint disease (spondylos = vertebrae<ref>URL: [http://medical-dictionary.thefreedictionary.com/spondylosis http://medical-dictionary.thefreedictionary.com/spondylosis]. Accessed on: 28 August 2011.</ref>). | ||
Clinical | *Other considerations: | ||
**Drug-induced psoriasis.<ref name=pmid21489366>{{Cite journal | last1 = Milavec-Puretić | first1 = V. | last2 = Mance | first2 = M. | last3 = Ceović | first3 = R. | last4 = Lipozenčić | first4 = J. | title = Drug induced psoriasis. | journal = Acta Dermatovenerol Croat | volume = 19 | issue = 1 | pages = 39-42 | month = Mar | year = 2011 | doi = | PMID = 21489366 }}</ref> | |||
====Clinical==== | |||
*''Auspitz sign'' = pin-point bleeding on removal of scale. | *''Auspitz sign'' = pin-point bleeding on removal of scale. | ||
*''Koebner phenomenon'' = lesions form at site of trauma. | *''Koebner phenomenon'' = lesions form at site of trauma. | ||
Common locations:<ref name=Ref_PCPBoD8_603>{{Ref PCPBoD8|603}}</ref> | |||
*Knees, elbows, scalp, glans [[penis]]. | |||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name=Ref_PCPBoD8_603>{{Ref PCPBoD8|603}}</ref> | Features:<ref name=Ref_PCPBoD8_603>{{Ref PCPBoD8|603}}</ref> | ||
* | *"Regular" acanthosis + long rete ridges (psoriasiform hyperplasia). | ||
**"Regular" ([[Psoriasiform dermatitides|psoriasiform change]]) = rete ridges are of similar length and thickness. | |||
*Parakeratosis. | *Parakeratosis. | ||
*Dilated vessels in superficial dermis (give rise to ''Auspitz sign''). | *Dilated vessels in superficial dermis (give rise to ''Auspitz sign''). | ||
*Spongiform pustules = | *Spongiform pustules = [[PMN]]s in stratum spinosum. | ||
*PMNs in parakeratotic stratum corneum (Munro microabscess). | *PMNs in parakeratotic stratum corneum (Munro microabscess). | ||
*Thinning of the suprapapillary plate. | |||
**The epidermis between rete ridges is thinner than in the normal adjacent skin - '''key feature'''. | |||
DDx: | |||
*[[Dermatomycosis]] ([[Fungi|fungal infection]]). | |||
*Drug reaction. | |||
Note: | |||
*[[Dermatophytosis]] = ring worm; dermatophystosis != [[dermatomycosis]]. | |||
====Images==== | |||
www: | |||
*[http://missinglink.ucsf.edu/lm/dermatologyglossary/img/Dermatology%20Glossary/Glossary%20Histo%20Images/Psoriasis_low_power.jpg Psoriasis - low mag. (ucsf.edu)].<ref>URL: [http://missinglink.ucsf.edu/lm/dermatologyglossary/psoriasis.html http://missinglink.ucsf.edu/lm/dermatologyglossary/psoriasis.html]. Accessed on: 4 September 2013.</ref> | |||
===Stains=== | |||
*[[PASD stain]] -ve for [[fungi|fungal]] organisms. | |||
===Sign out=== | |||
<pre> | |||
SKIN LESION, LEFT ARM, PUNCH BIOPSY: | |||
- SKIN WITH ACANTHOSIS, HYPERKERATOSIS, FOCAL PARAKERATOSIS, PROMINENT | |||
DILATED VESSELS IN THE SUPERFICIAL DERMIS, SUPERFICIAL SPONGIFORM PUSTULES. | |||
- MILD NONSPECIFIC PERIVASCULAR INFLAMMATION. | |||
- NEGATIVE FOR FUNGAL ORGANISMS WITH PAS STAINING. | |||
COMMENT: | |||
The findings are compatible with psoriasis. | |||
</pre> | |||
====Micro==== | |||
The sections show skin with regular psoriasiform change, hyperkeratosis, focal parakeratosis, prominent dilated vessels in the superficial dermis, superficial clusters of intraepidermal neutrophils (spongiform pustules) and thinning of the suprapapillary plate is present. A few perivascular inflammatory cells are present. | |||
There is no epidermal necrosis. Eosinophils are not apparent. The lymphocytes do not have significant atypia. | |||
==Lichen striatus== | |||
===General=== | |||
Features:<ref name=pmid15283785>{{Cite journal | last1 = Taniguchi Abagge | first1 = K. | last2 = Parolin Marinoni | first2 = L. | last3 = Giraldi | first3 = S. | last4 = Carvalho | first4 = VO. | last5 = de Oliveira Santini | first5 = C. | last6 = Favre | first6 = H. | title = Lichen striatus: description of 89 cases in children. | journal = Pediatr Dermatol | volume = 21 | issue = 4 | pages = 440-3 | month = | year = | doi = 10.1111/j.0736-8046.2004.21403.x | PMID = 15283785 }}</ref> | |||
*Benign, self-limited. | |||
Clinical: | |||
*Linear rash usu. on lower extremity. | |||
*Associated with atopy, [[lichen sclerosus]].<ref name=pmid15283785/> | |||
*Children. | |||
Clinical image: | |||
*[http://perridermatology.com/blog/2011/3/7/lichen-planus-lichen-striatus.html LS (perridermatology.com)]. | |||
===Microscopic=== | |||
Features: | |||
*"Ball and glove" pattern: | |||
**Rete ridges (glove) surround nexts of lymphocytes (ball). | |||
*Hyperkeratosis. | |||
*Parakeratosis. | |||
DDx: | |||
*[[Lichen planus]]. | |||
Images: | |||
*[http://www.dermpathdiagnostics.com/dxref.asp?catid=25&id=57 Lichen striatus (dermpathdiagnostics.com)]. | |||
*[http://www.drmihm.com/cases/case.cfm?CaseID=42 Lichen striatus (drmihm.com)]. | |||
==Lichen aureus== | |||
===General=== | |||
*Rare. | |||
Clinical:<ref name=pmid17511956/> | |||
*Plaques + minimal scale - erythematous/golden. | |||
===Microscopic=== | |||
Features:<ref name=pmid17511956>{{Cite journal | last1 = Hazan | first1 = C. | last2 = Fangman | first2 = B. | last3 = Cohen | first3 = D. | title = Lichen aureus. | journal = Dermatol Online J | volume = 13 | issue = 1 | pages = 23 | month = | year = 2007 | doi = | PMID = 17511956 | URL = http://dermatology.cdlib.org/131/cases/NYUcases/051606_9.html }}</ref> | |||
*Lymphocyte-predominant perivascular pattern. | |||
**May have features suggestive of vacuolar interface pattern. | |||
*Fibrosis of superficial papillary dermis. | |||
Images: | |||
*[http://dermatology.cdlib.org/131/cases/NYUcases/051606_9.html Lichen aureus (cdlib.org)]. | |||
==Granuloma faciale== | |||
===General=== | |||
*Considered a [[vasculitis]].<ref name=dermatlas_gf>URL: [http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309 http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309]. Accessed on: 23 September 2011.</ref> | |||
===Microscopic=== | |||
Features:<ref name=Ref_Derm198-9>{{Ref Derm|198-9}}</ref> | |||
*Neutrophilic vasculitis - often subtle: | |||
**Neutrophils within blood vessel walls. | |||
**Vessels destruction ([[fibrinoid necrosis]] or nuclear dust). | |||
*Mixed inflammatory superficial dermal infiltrate. | |||
**Eosinophils, neutrophils, plasma cells, histiocytes. | |||
*Lesion separated from the (normal) epidermis (Grenz zone).<ref name=dermatlas_gf>URL: [http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309 http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309]. Accessed on: 23 September 2011.</ref> | |||
DDx of chronic fibrosing [[leukocytoclastic vasculitis]]:<ref name=Ref_Derm198-9>{{Ref Derm|198-9}}</ref> | |||
*Granuloma faciale. | |||
*Erythema elevatum diutinum - lacks Grenz zone. | |||
*Inflammatory pseudotumour. | |||
Image: | |||
*[http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309 Granuloma faciale (dermatlas.med.jhmi.edu)]. | |||
==Atopic dermatitis== | |||
*[[AKA]] ''atopic eczema'', [[AKA]] ''infantile eczema''. | |||
===General=== | |||
*Very common - especially in children.<ref name=ad_nih>URL: [http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001856/ http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001856/]. Accessed on: 28 December 2011.</ref> | |||
**Most children outgrow the condition. | |||
===Microscopic=== | |||
Features: | |||
*Spongiotic dermatitis. | |||
DDx: | |||
*[[Spongiotic dermatitides]]. | |||
====Images==== | |||
<gallery> | |||
Image:Spongiotic_dermatitis_-_high_mag.jpg | Mild spongiotic dermatitis - high mag. (WC) | |||
Image:Spongiotic_dermatitis_-_very_high_mag.jpg | Mild spongiotic dermatitis - very high mag. (WC) | |||
</gallery> | |||
==Sweet syndrome== | |||
===General=== | |||
*Uncommon. | |||
===Microscopic=== | |||
Features: | |||
*Nodular and diffuse pattern - neutrophils predominant - without pus. | |||
DDx ''rips'': | |||
*Rheumatoid neutrophilic dermatitis. | |||
*[[Bowel-associated dermatosis-arthritis syndrome]] (BADAS). | |||
*[[Pyoderma gangrenosum]]. | |||
*Sweet syndrome. | |||
Image: | |||
*[http://dermatology.cdlib.org/94/NYU/Apr2002/041602-7b.jpg Sweet syndrome (cdlib.org)].<ref>URL: [http://dermatology.cdlib.org/94/NYU/Apr2002/7.html http://dermatology.cdlib.org/94/NYU/Apr2002/7.html]. Accessed on: 4 January 2012.</ref> | |||
==Granuloma inguinale== | |||
:'''Not''' to be confused with ''[[granuloma annulare]]''. | |||
*Previously known as ''donovanosis''. | |||
===General=== | |||
*Infection caused by ''Klebsiella granulomatis'' - [[Gram stain|Gram]]-negative, rod-shaped bacteria. | |||
**Used to be known as ''Calymmatobacterium granulomatis''.<ref name=pmid12473810>{{cite journal |author=O'Farrell N |title=Donovanosis |journal=Sex Transm Infect |volume=78 |issue=6 |pages=452–7 |year=2002 |month=December |pmid=12473810 |pmc=1758360 |doi= |url=http://sti.bmj.com/cgi/pmidlookup?view=long&pmid=12473810}}</ref> | |||
Location: | |||
*[[Penis]]. | |||
*[[Vulva]]. | |||
Clinical:<ref name=pmid21738983>{{Cite journal | last1 = Bezerra | first1 = SM. | last2 = Jardim | first2 = MM. | last3 = Silva | first3 = VB. | title = Granuloma inguinale (Donovanosis). | journal = An Bras Dermatol | volume = 86 | issue = 3 | pages = 585-6 | month = Jun | year = 2011 | doi = | PMID = 21738983 |URL = http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0365-05962011000300028&lng=en&nrm=iso&tlng=en }}</ref> | |||
*Sexually transmitted. | |||
*Nodule or papule developing into a painless ulcer in the inguinal region. | |||
*No lymphadenopathy (unlike [[syphilis]]). | |||
===Microscopic=== | |||
Features: | |||
*Donovan bodies - '''key feature''': | |||
**Rod-shaped bodies within histiocytes. | |||
DDx: | |||
*[[Syphilis]]. | |||
Image: | |||
*[http://microblog.me.uk/213 Granuloma inguinale - crappy image (microblog.me.uk)]. | |||
===Stains=== | |||
*[[Giemsa stain]] - highlights organisms. | |||
==Pyoderma gangrenosum== | |||
{{Main|Pyoderma gangrenosum}} | |||
==Necrobiotic xanthogranuloma== | |||
*Abbreviated ''NXG''. | |||
{{Main|Necrobiotic xanthogranuloma}} | |||
=DDx for pattern= | =DDx for pattern= | ||
==Spongiotic dermatitides== | ==Spongiotic dermatitides== | ||
DDx:<ref name=pmid18418089>{{cite journal |author=Brinster NK |title=Dermatopathology for the surgical pathologist: a pattern based approach to the diagnosis of inflammatory skin disorders (part I) |journal=Adv Anat Pathol |volume=15 |issue=2 |pages=76–96 |year=2008 |month=March |pmid=18418089 |doi=10.1097/PAP.0b013e3181664e8d |url=}}</ref> | DDx:<ref name=pmid18418089>{{cite journal |author=Brinster NK |title=Dermatopathology for the surgical pathologist: a pattern based approach to the diagnosis of inflammatory skin disorders (part I) |journal=Adv Anat Pathol |volume=15 |issue=2 |pages=76–96 |year=2008 |month=March |pmid=18418089 |doi=10.1097/PAP.0b013e3181664e8d |url=}}</ref> | ||
*Atopic dermatitis. | *[[Atopic dermatitis]]. | ||
*Contact dermatitis. | *[[Contact dermatitis]]. | ||
*Stasis dermatitis. | *Stasis dermatitis. | ||
*[[Seborrheic dermatitis]]. | *[[Seborrheic dermatitis]]. | ||
| Line 201: | Line 459: | ||
*Psoriasis vulgaris. | *Psoriasis vulgaris. | ||
*Dermatophyte infection. | *Dermatophyte infection. | ||
*Pityriasis rubra pilaris. | *[[Pityriasis rubra pilaris]]. | ||
===Irregular psoriasiform dermatitis=== | ===Irregular psoriasiform dermatitis=== | ||
| Line 218: | Line 476: | ||
*[[Systemic lupus erythematosus]]. | *[[Systemic lupus erythematosus]]. | ||
*Morbillifrom viral exanthem. | *Morbillifrom viral exanthem. | ||
Additional:<ref name=pmid16311340>{{Cite journal | last1 = Alsaad | first1 = KO. | last2 = Ghazarian | first2 = D. | title = My approach to superficial inflammatory dermatoses. | journal = J Clin Pathol | volume = 58 | issue = 12 | pages = 1233-41 | month = Dec | year = 2005 | doi = 10.1136/jcp.2005.027151 | PMID = 16311340 | PMC = 1770784}}</ref> | |||
*Phototoxic dermatitis. | |||
*Acute radiation dermatitis. | |||
*Erythema multiforme-like drug eruption. | |||
*Lichen sclerosis et atrophicus. | |||
*[[Erythema dyschromicum perstans]] (ashy dermatosis). | |||
Super lame mnemonic ''Danny G & SLE'': | |||
*'''D'''ermatomyositis, '''G'''VHD, '''S'''LE, '''L'''ichen sclerosus, '''E'''rythema multiforme. | |||
===Lichenoid interface dermatitides=== | ===Lichenoid interface dermatitides=== | ||
| Line 226: | Line 494: | ||
*Lichenoid drug eruption. | *Lichenoid drug eruption. | ||
*Fixed drug eruption. | *Fixed drug eruption. | ||
Additional:<ref name=pmid16311340>{{Cite journal | last1 = Alsaad | first1 = KO. | last2 = Ghazarian | first2 = D. | title = My approach to superficial inflammatory dermatoses. | journal = J Clin Pathol | volume = 58 | issue = 12 | pages = 1233-41 | month = Dec | year = 2005 | doi = 10.1136/jcp.2005.027151 | PMID = 16311340 | PMC = 1770784}}</ref> | |||
*[[Lichen planus-like keratosis]]. | |||
*Lichenoid [[actinic keratosis]]. | |||
*Lichen nitidus. | |||
*Pigmented purpuric dermatosis. | |||
*Lichen [[amyloidosis]]. | |||
*Pityriasis lichenoides chronica. | |||
*[[HIV]] dermatitis. | |||
*[[Syphilis]]. | |||
*[[Urticaria pigmentosa]]. | |||
*Chronic [[graft versus host disease]]. | |||
==Bullous disease== | ==Bullous disease== | ||
| Line 231: | Line 511: | ||
===Subcorneal bullous disorders=== | ===Subcorneal bullous disorders=== | ||
DDx '''with''' acantholysis:<ref name=pmid18418089/> | DDx '''with''' acantholysis:<ref name=pmid18418089/> | ||
*[[Pemphigus | *[[Pemphigus foliaceus]]. | ||
*[[Bullous impetigo]]. | *[[Bullous impetigo]]. | ||
*[[ | *[[Staphylococcal scalded skin syndrome]]. | ||
DDx '''without''' acantholysis:DDx:<ref name=pmid18418089/> | DDx '''without''' acantholysis:DDx:<ref name=pmid18418089/> | ||
*Subcorneal pustular | *Subcorneal pustular dermatosis (Sneddon-Wilkinson disease). | ||
*Pustular psoriasis. | *Pustular psoriasis. | ||
*Pustular drug eruption ([[acute generalized exanthematous pustulosis]]). | *Pustular drug eruption ([[acute generalized exanthematous pustulosis]]). | ||
| Line 246: | Line 526: | ||
*[[Darier disease]]. | *[[Darier disease]]. | ||
*[[Grover disease]] (transient acantholytic dermatosis). | *[[Grover disease]] (transient acantholytic dermatosis). | ||
Memory device - ''PhD'' + ''Grover'' = '''P'''emphigus vulgaris, '''H'''ailey-Hailey, '''D'''arier, '''G'''rover. | |||
===Subepidermal bullous disorders=== | ===Subepidermal bullous disorders=== | ||
| Line 253: | Line 535: | ||
*[[Porphyria cutanea tarda]]. | *[[Porphyria cutanea tarda]]. | ||
*Epidermolysis bullosa acquista. | *Epidermolysis bullosa acquista. | ||
*[[Dermatitis | *[[Dermatitis herpetiformis]]. | ||
*Linear IgA disease. | *Linear IgA disease. | ||
| Line 261: | Line 543: | ||
*Bullous [[systemic lupus erythematosus]]. | *Bullous [[systemic lupus erythematosus]]. | ||
== | Mnemonic ''DELPHI'': | ||
*'''D'''ermatitis herpetiformis. | |||
*'''E'''pidermolysis bullosa acquisita. | |||
*Bullous '''l'''upus erythematosis. | |||
*'''P'''emphigoid, bullous. | |||
*'''H'''erpes gestationis - rare autoimmune bullous dermatosis of pregnancy, not related to HSV.<ref>URL: [http://emedicine.medscape.com/article/1063499-overview http://emedicine.medscape.com/article/1063499-overview]. Accessed on: 23 September 2011.</ref> | |||
*Linear '''I'''gA disease. | |||
==Dermatitides with perivascular inflammation== | |||
===Lymphocytes=== | ===Lymphocytes=== | ||
Lymphocytes (tightly cuffed):<ref name=pmid18418089/> | Lymphocytes (tightly cuffed):<ref name=pmid18418089/> | ||
| Line 268: | Line 558: | ||
*Malignancy. | *Malignancy. | ||
*Vitiligo (with absent melanocytes). | *Vitiligo (with absent melanocytes). | ||
*Scleroderma/morphea. | *[[Scleroderma]]/morphea. | ||
Lymphocytes & plasma cells +/-eosinophils: | Lymphocytes & plasma cells +/-eosinophils: | ||
| Line 281: | Line 571: | ||
*Insect bite. | *Insect bite. | ||
*Dermatophyte infection. | *Dermatophyte infection. | ||
A simple memory device - 6 Ls:<ref name=dermpathmd>URL: [http://www.dermpathmd.com/mnemonics/mnemonics_dermatopathology.htm http://www.dermpathmd.com/mnemonics/mnemonics_dermatopathology.htm]. Accessed on: 23 September 2011.</ref> | |||
*'''L'''ymphoma. | |||
*Pseudo'''l'''ymphoma (cutaneous lymphoid hyperplasia, lymphocytoma cutis). | |||
*'''L'''upus erythematosus. | |||
*'''L'''ymphocytic infiltrate of Jessner / tumid lupus erythematosus. | |||
*[[polymorphous light eruption|Polymorphous '''l'''ight eruption]]. | |||
*'''L'''yme disease. | |||
===Neutrophils=== | ===Neutrophils=== | ||
DDx:<ref name=pmid18418089/> | DDx:<ref name=pmid18418089/> | ||
*Cellulitis. | *[[Cellulitis]]. | ||
*Neutrophilic eccrine hidradenitis (idiopathic palmar-plantar hidradenitis) | *Neutrophilic eccrine hidradenitis (idiopathic palmar-plantar hidradenitis) | ||
| Line 292: | Line 590: | ||
===Eosinophils=== | ===Eosinophils=== | ||
DDx:<ref name=pmid18418089/> | DDx:<ref name=pmid18418089/> | ||
*Hypersensitivity reaction/drug reaction. | *[[Hypersensitivity]] reaction/drug reaction. | ||
*Insect bite. | *Insect bite. | ||
*Bullous pemphigoid, urticarial. | *Bullous pemphigoid, urticarial. | ||
| Line 319: | Line 617: | ||
*[[Microscopic polyangiitis]]. | *[[Microscopic polyangiitis]]. | ||
*Mixed cryoglobulinemia. | *Mixed cryoglobulinemia. | ||
*Connective tissue diseases. | *[[Connective tissue diseases]]. | ||
Large vessel: | Large vessel: | ||
*[[Giant cell arteritis]]. | *[[Giant cell arteritis]]. | ||
==Nodular and diffuse== | ==Nodular and diffuse dermatitides== | ||
===Neutrophils=== | ===Neutrophils=== | ||
====With pus (suppurative)==== | ====With pus (suppurative)==== | ||
| Line 337: | Line 635: | ||
With vasculitis: | With vasculitis: | ||
*Neutrophils only: see ''[[vasculitides]]''. | *Neutrophils only: see ''[[vasculitides]]''. | ||
*Mixed infiltrate: granuloma faciale, erythema elevatinum diutinum. | *Mixed infiltrate: [[granuloma faciale]], erythema elevatinum diutinum. | ||
Without vasculitis: | Without vasculitis: | ||
*Sweet syndrome. | *[[Sweet syndrome]]. | ||
*Pyoderma gangrenosum. | *[[Pyoderma gangrenosum]]. | ||
*Rheumatoid neutrophilic | *[[Rheumatoid arthritis|Rheumatoid neutrophilic dermatitis]]. | ||
*Bowel-associated | *Bowel-associated dermatosis-arthritis syndrome. | ||
===Lymphocytes=== | ===Lymphocytes=== | ||
| Line 361: | Line 659: | ||
**Insect bites. | **Insect bites. | ||
*Hypereosinophilic syndrome (HES). | *Hypereosinophilic syndrome (HES). | ||
*Angiolymphoid hyperplasia with eosinophilia (ALHE). | *[[Angiolymphoid hyperplasia with eosinophilia]] (ALHE). | ||
*[[Kimura disease]]. | *[[Kimura disease]]. | ||
===Histiocytes=== | ===Histiocytes=== | ||
*[[Sarcoidosis]] | ====Granulomatous==== | ||
* | =====Sarcoidal===== | ||
*[[Sarcoidosis]] - have few lymphoid cells around them; thus called "naked granulomas".<ref name=pmid18948765>{{Cite journal | last1 = Brinster | first1 = NK. | title = Dermatopathology for the surgical pathologist: a pattern-based approach to the diagnosis of inflammatory skin disorders (part II). | journal = Adv Anat Pathol | volume = 15 | issue = 6 | pages = 350-69 | month = Nov | year = 2008 | doi = 10.1097/PAP.0b013e31818b1ac6 | PMID = 18948765 }}</ref> | |||
=====Tuberculoid===== | |||
*[[Tuberculosis]]. | |||
*Tertiary [[syphilis]] - usu. abundant plasma cells. | |||
*Cutaneous leishmaniasis. | |||
=====Foreign body-type granulomas===== | |||
=====Palisaded granumolas===== | |||
Blue granuloma: | |||
*[[Granuloma annulare]]. | |||
*[[Wegener granulomatosis]]. | |||
*Rheumatoid vasculitis. | |||
Red granuloma: | |||
*[[Rheumatoid nodule]]. | |||
*[[Necrobiosis lipoidica]]. | |||
*[[Necrobiotic xanthogranuloma]]. | |||
*[[Churg-Strauss syndrome]]. | |||
=See also= | =See also= | ||
| Line 374: | Line 692: | ||
=References= | =References= | ||
{{Reflist|2}} | {{Reflist|2}} | ||
=External links= | |||
*[http://www.dermpathmd.com/mnemonics/mnemonics_dermatopathology.htm Dermatopathology mnemonics (dermpathmd.com)]. | |||
[[Category:Dermatopathology]] | [[Category:Dermatopathology]] | ||
Latest revision as of 22:18, 5 December 2018
Inflammatory skin disorders, also inflammatory skin diseases, are a significant part of dermatopathology. They lead to trepidation among pathologists that don't see lots of skin. Non-inflammatory skin disease is covered in dermatologic neoplasms and non-malignant skin disease.
Classification
- Bullous.
- Interface.
- Nodular & diffuse.
- Spongiotic.
- Vasculitis.
- Perivascular.
- Panniculitis.
- Psoriasiform.
Tabular comparison of inflammatory skin disease (adapted from Brinster[1][2]):
| Pattern | Key histologic feature | Subclassifications | Example | Image |
| Bullous | large "empty spaces" | -subcorneal -suprabasillar -subepidermal |
-pemphigus foliaceus -pemphigus vulgaris -dermatitis herpetiformis |
 PV (WC) |
| Interface | inflammation at DE junction | -vacuolar (minimal) -lichenoid (band-like) |
-erythema multiforme, SLE -lichen planus |
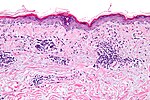 VID (WC) |
| Nodular & diffuse | intradermal inflammatory infiltrate - nodular and/or diffuse | -neutrophic -lymphocytic -plasmic -eosinophilic -histocytic |
-follicular occlusion triad, ruptured cyst/follicle -CTCL, reactive -plasma cell neoplasm, syphilis -eosinophilic cellulitis, Kimura disease -granuloma annulare, sarcoidosis, TB |
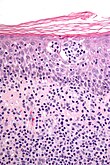 CTCL (WC) |
| Spongiotic | small empty spaces between keratinocytes - can see squamous bridges (best seen at high power); +/- quasi-microvacuolar appearance | -acute -subacute -chronic |
-poison ivy -nummular dermatitis -atopic dermatitis |
severe (WC), mild (WC) |
| Vasculitis | inflammation of vessel wall/vessel was destruction | -small vessel -medium vessel -large vessel |
-leukocytoclastic vasculitis -PAN -giant cell arteritis |
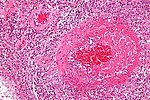 EGPA (WC) |
| Perivascular | inflammation around vessels | -neutrophilic -lymphocytic -mastocytic -eosinophilic |
-cellulitis -viral exanthem, Rx reaction -mastocytosis -insect bite, Rx reaction |
|
| Panniculitis | inflammation of adipose tissue | -septal -lobular |
-erythema nodosum, scleroderma panniculitis -erythema induratum, infection |
|
| Psoriasiform | epidermal thickening and long rete ridges |
-regular -irregular |
-psoriasis -lichen simplex chronicus |
 LSC (WC) |
Notes:
- DE junction = dermal-epidermal junction.
- The "empty space" in bullous disease in situ is filled with fluid.
Non-specific patterns
Psoriasiform pattern
General
- Can be subclassified.
DDx:
- Psoriasis vulgaris (most common).
- Psoriatic arthritis.
- Drug-induced.
- Dermatomycosis (fungal infection).
- Others.
Microscopic
- Regular epidermal thickening - as very long rete ridges (described as "test tube-morphology") - key feature.
- Epidermis between rete ridges thin ("thinning of suprapapillary plate").
- Parakeratosis.
- Thin/absent granular layer.
- Dilated blood vessels in superficial dermis.
- Neutrophil clusters (Munro microabscess).
Specific diseases
Seborrheic dermatitis
General
- Very common.
Microscopic
Features:[4]
- Spongiosis (epidermal edema).
- Acanthosis (epidermal thickening).
- "Follicular lipping" = parakeratosis with neutrophils.
- Perivascular neutrophils and lymphocytes.
Lupus erythematosus
General
- A group of skin diseases - includes:
- The systemic disease, systemic lupus erythematosus, that typically has multi-organ involvement.
Microscopic
Features - classic:
- Lymphocytic interface dermatitis.[5]
- Basal layer vacuolization.[6]
- Intradermal mucin.
- Thin epidermis.
- Compact stratum corneum.
DDx:
- Discoid lupus erythematosus.
- Drug reaction (drug-induced lupus erythematosus).
- Solar elastosis - may be confused with mucin; vacuolar interface dermatitis not present
Images
Discoid lupus erythematosus
General
- Typically self-limited and isolated.
- It is not associated with systemic lupus erythematosus.
Microscopic
Features:[7]
- Lymphocytic interface dermatitis with basal layer vacuolation and keratinocyte apoptosis.
- Deep dermal lymphocytes.
- Basket weave stratum corneum.
- Dermal mucin.
- Thick dermal-epidermal basement membrane.
DDx:
Image:
Dermatomyositis
- For the muscle manifestations see: Neuromuscular_pathology#Dermatomyositis.
General
- Complement mediated disease - membrane attack complex.
- Usually middle age.
- Associated skin rash is common.
- May precede or follow muscle pathology.
- Associated with malignancy in approximately 10% of cases.[8]
Clinical:
- Jo-1 +ve.
Gross
- Have lesions on the knuckles - Gottron's papules.
Microsopic
Features:
- Vacuolar interface dermatitis (lymphocytic inflammation at the dermal-epidermal junction).
- +/-Loss of rete ridges.
DDx:
- Lupus.
Lichen planus
- Should not be confused with lichen planus-like keratosis.
- Abbreviated LP.
General
- An oral pathology - classically.
- May be seen where the sun don't shine - penis,[9] vulva and vagina.[10]
Etiology:
- Autoimmune disease, T-cell–mediated.[11]
Clinical:[12]
- 6 Ps: pruritic (itchy), purple, polygonal, planar papules and plaques.
Note:
- Clinically, lichen planus and lichen sclerosus are similar. The main difference is lichen planus involves mucous membranes.[13]
Gross
- Wickham striae = white lines/dots.
- Due to hypergranulosis.
Microscopic
- Loss of basal cells (stratum basale) -- key feature.
- Loss of rete ridges/formation of pointed rete ridges "sawtoothing".
- Interface dermatitis (lymphocytes at dermal-epidermal junction).
- Hypergranulosis; stratum granulosum thickened (grossly seen as "Wickham stria" = white lines).
- Hyperkeratosis; stratum corneum thickened.
- Necrotic basal cell in dermis = colloid bodies = Civatte bodies.[16]
- Pink bodies approximately the size of a keratinocyte.
Notes:
- Hyperkeratosis and hypergranulosis are not seen in erythema multiforme.
- Colloid bodies = cytoid bodies = Civatte bodies = hyaline bodies = apoptotic bodies.[17]
DDx:
- Bullous disease, subepithelial vesicular.
- Lichenoid keratosis (lichen planus-like keratosis) - parakeratosis prominent, no oral mucosal involvement.
- Fungal infection.[18]
- Lichenoid drug reaction - unusual body site affected, separated clinically.
- Lichenoid actinic keratosis - basal atypia, solar elastosis.
Images
Stains
- PAS-D or PAS-F to exclude a fungal infection.
Sign out
FORESKIN, CIRCUMCISION: - LICHEN PLANUS.
VULVA, LEFT POSTERIOR FOURCHETTE, BIOPSY: - COMPATIBLE WITH LICHEN PLANUS.
Micro
The sections show skin with a lymphoplasmacytic interface dermatitis, basal cell loss, hypergranulosis, hyperkeratosis, loss of the rete ridges and Civatte bodies.
The epidermis matures to the surface. No significant nuclear atypia is identified.
Fungal organisms are not identified with a PAS-D stain.
Lichen sclerosus
Microscopic
Features:[19]
- Subepithelial fibrosis - key feature.
Psoriasis
General
- Chronic skin condition +/- systemic involvement:[20]
- Arthritis, i.e. psoriatic arthritis.
- Myopathy.
- Enteropathy, e.g. inflammatory bowel disease.
- Syondylitic joint disease (spondylos = vertebrae[21]).
- Other considerations:
- Drug-induced psoriasis.[22]
Clinical
- Auspitz sign = pin-point bleeding on removal of scale.
- Koebner phenomenon = lesions form at site of trauma.
Common locations:[20]
- Knees, elbows, scalp, glans penis.
Microscopic
Features:[20]
- "Regular" acanthosis + long rete ridges (psoriasiform hyperplasia).
- "Regular" (psoriasiform change) = rete ridges are of similar length and thickness.
- Parakeratosis.
- Dilated vessels in superficial dermis (give rise to Auspitz sign).
- Spongiform pustules = PMNs in stratum spinosum.
- PMNs in parakeratotic stratum corneum (Munro microabscess).
- Thinning of the suprapapillary plate.
- The epidermis between rete ridges is thinner than in the normal adjacent skin - key feature.
DDx:
- Dermatomycosis (fungal infection).
- Drug reaction.
Note:
- Dermatophytosis = ring worm; dermatophystosis != dermatomycosis.
Images
www:
Stains
- PASD stain -ve for fungal organisms.
Sign out
SKIN LESION, LEFT ARM, PUNCH BIOPSY: - SKIN WITH ACANTHOSIS, HYPERKERATOSIS, FOCAL PARAKERATOSIS, PROMINENT DILATED VESSELS IN THE SUPERFICIAL DERMIS, SUPERFICIAL SPONGIFORM PUSTULES. - MILD NONSPECIFIC PERIVASCULAR INFLAMMATION. - NEGATIVE FOR FUNGAL ORGANISMS WITH PAS STAINING. COMMENT: The findings are compatible with psoriasis.
Micro
The sections show skin with regular psoriasiform change, hyperkeratosis, focal parakeratosis, prominent dilated vessels in the superficial dermis, superficial clusters of intraepidermal neutrophils (spongiform pustules) and thinning of the suprapapillary plate is present. A few perivascular inflammatory cells are present.
There is no epidermal necrosis. Eosinophils are not apparent. The lymphocytes do not have significant atypia.
Lichen striatus
General
Features:[24]
- Benign, self-limited.
Clinical:
- Linear rash usu. on lower extremity.
- Associated with atopy, lichen sclerosus.[24]
- Children.
Clinical image:
Microscopic
Features:
- "Ball and glove" pattern:
- Rete ridges (glove) surround nexts of lymphocytes (ball).
- Hyperkeratosis.
- Parakeratosis.
DDx:
Images:
Lichen aureus
General
- Rare.
Clinical:[25]
- Plaques + minimal scale - erythematous/golden.
Microscopic
Features:[25]
- Lymphocyte-predominant perivascular pattern.
- May have features suggestive of vacuolar interface pattern.
- Fibrosis of superficial papillary dermis.
Images:
Granuloma faciale
General
- Considered a vasculitis.[26]
Microscopic
Features:[27]
- Neutrophilic vasculitis - often subtle:
- Neutrophils within blood vessel walls.
- Vessels destruction (fibrinoid necrosis or nuclear dust).
- Mixed inflammatory superficial dermal infiltrate.
- Eosinophils, neutrophils, plasma cells, histiocytes.
- Lesion separated from the (normal) epidermis (Grenz zone).[26]
DDx of chronic fibrosing leukocytoclastic vasculitis:[27]
- Granuloma faciale.
- Erythema elevatum diutinum - lacks Grenz zone.
- Inflammatory pseudotumour.
Image:
Atopic dermatitis
General
- Very common - especially in children.[28]
- Most children outgrow the condition.
Microscopic
Features:
- Spongiotic dermatitis.
DDx:
Images
Sweet syndrome
General
- Uncommon.
Microscopic
Features:
- Nodular and diffuse pattern - neutrophils predominant - without pus.
DDx rips:
- Rheumatoid neutrophilic dermatitis.
- Bowel-associated dermatosis-arthritis syndrome (BADAS).
- Pyoderma gangrenosum.
- Sweet syndrome.
Image:
Granuloma inguinale
- Not to be confused with granuloma annulare.
- Previously known as donovanosis.
General
- Infection caused by Klebsiella granulomatis - Gram-negative, rod-shaped bacteria.
- Used to be known as Calymmatobacterium granulomatis.[30]
Location:
Clinical:[31]
- Sexually transmitted.
- Nodule or papule developing into a painless ulcer in the inguinal region.
- No lymphadenopathy (unlike syphilis).
Microscopic
Features:
- Donovan bodies - key feature:
- Rod-shaped bodies within histiocytes.
DDx:
Image:
Stains
- Giemsa stain - highlights organisms.
Pyoderma gangrenosum
Necrobiotic xanthogranuloma
- Abbreviated NXG.
DDx for pattern
Spongiotic dermatitides
DDx:[1]
- Atopic dermatitis.
- Contact dermatitis.
- Stasis dermatitis.
- Seborrheic dermatitis.
- Nummular dermatitis.
- Spongiotic drug eruption.
Psoriasiform dermatitides
Regular psoriasiform dermatitis
DDx:[1]
- Psoriasis vulgaris.
- Dermatophyte infection.
- Pityriasis rubra pilaris.
Irregular psoriasiform dermatitis
Interface dermatitides
Vacuolar interface dermatitides
DDx:[1]
- Erythema multiforme.
- Lichen sclerosus.
- Fixed drug eruption.
Others:[1]
- Graft versus host disease.
- Dermatomyositis.
- Systemic lupus erythematosus.
- Morbillifrom viral exanthem.
Additional:[32]
- Phototoxic dermatitis.
- Acute radiation dermatitis.
- Erythema multiforme-like drug eruption.
- Lichen sclerosis et atrophicus.
- Erythema dyschromicum perstans (ashy dermatosis).
Super lame mnemonic Danny G & SLE:
- Dermatomyositis, GVHD, SLE, Lichen sclerosus, Erythema multiforme.
Lichenoid interface dermatitides
DDx:[1]
- Lichen planus
- Mycosis fungoides.
- Discoid lupus erythematosus.
- Lichenoid drug eruption.
- Fixed drug eruption.
Additional:[32]
- Lichen planus-like keratosis.
- Lichenoid actinic keratosis.
- Lichen nitidus.
- Pigmented purpuric dermatosis.
- Lichen amyloidosis.
- Pityriasis lichenoides chronica.
- HIV dermatitis.
- Syphilis.
- Urticaria pigmentosa.
- Chronic graft versus host disease.
Bullous disease
Subcorneal bullous disorders
DDx with acantholysis:[1]
DDx without acantholysis:DDx:[1]
- Subcorneal pustular dermatosis (Sneddon-Wilkinson disease).
- Pustular psoriasis.
- Pustular drug eruption (acute generalized exanthematous pustulosis).
Suprabasilar bullous disorders
DDx:[1]
- Pemphigus vulgaris.
- Hailey-Hailey disease (benign familial pemphigus).
- Darier disease.
- Grover disease (transient acantholytic dermatosis).
Memory device - PhD + Grover = Pemphigus vulgaris, Hailey-Hailey, Darier, Grover.
Subepidermal bullous disorders
DDx:[1]
- Bullous pemphigoid.
- Cicatricial pemphigoid.
- Porphyria cutanea tarda.
- Epidermolysis bullosa acquista.
- Dermatitis herpetiformis.
- Linear IgA disease.
Others:
- Insect bite.
- Coma blister.
- Bullous systemic lupus erythematosus.
Mnemonic DELPHI:
- Dermatitis herpetiformis.
- Epidermolysis bullosa acquisita.
- Bullous lupus erythematosis.
- Pemphigoid, bullous.
- Herpes gestationis - rare autoimmune bullous dermatosis of pregnancy, not related to HSV.[33]
- Linear IgA disease.
Dermatitides with perivascular inflammation
Lymphocytes
Lymphocytes (tightly cuffed):[1]
- Infections.
- Medications.
- Malignancy.
- Vitiligo (with absent melanocytes).
- Scleroderma/morphea.
Lymphocytes & plasma cells +/-eosinophils:
- Erythema chronicum migrans (Lyme disease).
Lymphocytes (not tightly cuffed):
- Viral exanthems.
- Drug eruptions.
Lymphocytes & eosinophils:
- Drug reaction.
- Insect bite.
- Dermatophyte infection.
A simple memory device - 6 Ls:[34]
- Lymphoma.
- Pseudolymphoma (cutaneous lymphoid hyperplasia, lymphocytoma cutis).
- Lupus erythematosus.
- Lymphocytic infiltrate of Jessner / tumid lupus erythematosus.
- Polymorphous light eruption.
- Lyme disease.
Neutrophils
DDx:[1]
- Cellulitis.
- Neutrophilic eccrine hidradenitis (idiopathic palmar-plantar hidradenitis)
With eosinophils:
- Urticaria.
Eosinophils
DDx:[1]
- Hypersensitivity reaction/drug reaction.
- Insect bite.
- Bullous pemphigoid, urticarial.
Mast cells
Vasculitis
General DDx:
- Infection.
- Autoimmune.
- Malignancy.
- Toxic (medications).
Small vessel:
Medium vessel:
Medium vessels often with small vessel involvement:
- Churg-Strauss syndrome.
- Microscopic polyangiitis.
- Mixed cryoglobulinemia.
- Connective tissue diseases.
Large vessel:
Nodular and diffuse dermatitides
Neutrophils
With pus (suppurative)
Neutrophils only:
- Follicular occlusion triad.
- Ruptured cyst/follicle.
Neutrophils and eosinophils:
- Halogenoderma.
- Blastomycosis-like pyoderma (pyoderma vegetans) - due to bacterial infection, usu. S. aureus.
Without pus
With vasculitis:
- Neutrophils only: see vasculitides.
- Mixed infiltrate: granuloma faciale, erythema elevatinum diutinum.
Without vasculitis:
- Sweet syndrome.
- Pyoderma gangrenosum.
- Rheumatoid neutrophilic dermatitis.
- Bowel-associated dermatosis-arthritis syndrome.
Lymphocytes
- Reactive lymphoid hyperplasia - may be due to drugs.
- Lymphoid malignancy.
Plasma cells
- Inflammation.
- Plasma cell neoplasms.
- Infections:
- Syphilis - lichenoid/psoriasiform pattern.
- Chancroid.
- Granuloma inguinale.
- Lymphogranuloma venereum.
Eosinophils
- Eosinophilic cellulitis (Wells syndrome).
- Insect bites.
- Hypereosinophilic syndrome (HES).
- Angiolymphoid hyperplasia with eosinophilia (ALHE).
- Kimura disease.
Histiocytes
Granulomatous
Sarcoidal
- Sarcoidosis - have few lymphoid cells around them; thus called "naked granulomas".[2]
Tuberculoid
- Tuberculosis.
- Tertiary syphilis - usu. abundant plasma cells.
- Cutaneous leishmaniasis.
Foreign body-type granulomas
Palisaded granumolas
Blue granuloma:
- Granuloma annulare.
- Wegener granulomatosis.
- Rheumatoid vasculitis.
Red granuloma:
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Brinster NK (March 2008). "Dermatopathology for the surgical pathologist: a pattern based approach to the diagnosis of inflammatory skin disorders (part I)". Adv Anat Pathol 15 (2): 76–96. doi:10.1097/PAP.0b013e3181664e8d. PMID 18418089.
- ↑ 2.0 2.1 Brinster, NK. (Nov 2008). "Dermatopathology for the surgical pathologist: a pattern-based approach to the diagnosis of inflammatory skin disorders (part II).". Adv Anat Pathol 15 (6): 350-69. doi:10.1097/PAP.0b013e31818b1ac6. PMID 18948765.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1191. ISBN 978-1416031215.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1191. ISBN 978-1416031215.
- ↑ JAH. 20 February 2009.
- ↑ Crowson AN, Magro CM, Mihm MC (April 2008). "Interface dermatitis". Arch. Pathol. Lab. Med. 132 (4): 652–66. PMID 18384217. http://www.archivesofpathology.org/doi/full/10.1043/1543-2165%282008%29132%5B652%3AID%5D2.0.CO%3B2.
- ↑ URL: http://www.dermpedia.org/baby-dermpedia-for-beginners/discoid-lupus-erythematosus. Accessed on: 7 March 2012.
- ↑ Chen YJ, Wu CY, Huang YL, Wang CB, Shen JL, Chang YT (2010). "Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan". Arthritis Res. Ther. 12 (2): R70. doi:10.1186/ar2987. PMC 2888225. PMID 20398365. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2888225/.
- ↑ Teichman, JM.; Sea, J.; Thompson, IM.; Elston, DM. (Jan 2010). "Noninfectious penile lesions.". Am Fam Physician 81 (2): 167-74. PMID 20082512.
- ↑ Gupta, R.; Bansal, B.; Singh, S.; Yadav, I.; Gupta, K.; Kudesia, M. (2009). "Lichen planus of uterine cervix - the first report of a novel site of occurrence: a case report.". Cases J 2: 9306. doi:10.1186/1757-1626-2-9306. PMID 20062629.
- ↑ URL: http://emedicine.medscape.com/article/1078327-overview. Accessed on: 11 September 2010.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1191. ISBN 978-1416031215.
- ↑ McPherson, T.; Cooper, S.. "Vulval lichen sclerosus and lichen planus.". Dermatol Ther 23 (5): 523-32. doi:10.1111/j.1529-8019.2010.01355.x. PMID 20868406.
- ↑ URL: http://emedicine.medscape.com/article/1078327-overview. Accessed on: 11 September 2010.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1192. ISBN 978-1416031215.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 604. ISBN 978-1416054542.
- ↑ URL: http://www.careforumwales.org/cell-carcinoma/histopathologic-terminology.html. Accessed on: 28 August 2011.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 36. ISBN 978-0443066542.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1065-6. ISBN 0-7216-0187-1.
- ↑ 20.0 20.1 20.2 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 603. ISBN 978-1416054542.
- ↑ URL: http://medical-dictionary.thefreedictionary.com/spondylosis. Accessed on: 28 August 2011.
- ↑ Milavec-Puretić, V.; Mance, M.; Ceović, R.; Lipozenčić, J. (Mar 2011). "Drug induced psoriasis.". Acta Dermatovenerol Croat 19 (1): 39-42. PMID 21489366.
- ↑ URL: http://missinglink.ucsf.edu/lm/dermatologyglossary/psoriasis.html. Accessed on: 4 September 2013.
- ↑ 24.0 24.1 Taniguchi Abagge, K.; Parolin Marinoni, L.; Giraldi, S.; Carvalho, VO.; de Oliveira Santini, C.; Favre, H.. "Lichen striatus: description of 89 cases in children.". Pediatr Dermatol 21 (4): 440-3. doi:10.1111/j.0736-8046.2004.21403.x. PMID 15283785.
- ↑ 25.0 25.1 Hazan, C.; Fangman, B.; Cohen, D. (2007). "Lichen aureus.". Dermatol Online J 13 (1): 23. PMID 17511956.
- ↑ 26.0 26.1 URL: http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1289066309. Accessed on: 23 September 2011.
- ↑ 27.0 27.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 198-9. ISBN 978-0443066542.
- ↑ URL: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001856/. Accessed on: 28 December 2011.
- ↑ URL: http://dermatology.cdlib.org/94/NYU/Apr2002/7.html. Accessed on: 4 January 2012.
- ↑ O'Farrell N (December 2002). "Donovanosis". Sex Transm Infect 78 (6): 452–7. PMC 1758360. PMID 12473810. http://sti.bmj.com/cgi/pmidlookup?view=long&pmid=12473810.
- ↑ Bezerra, SM.; Jardim, MM.; Silva, VB. (Jun 2011). "Granuloma inguinale (Donovanosis).". An Bras Dermatol 86 (3): 585-6. PMID 21738983.
- ↑ 32.0 32.1 Alsaad, KO.; Ghazarian, D. (Dec 2005). "My approach to superficial inflammatory dermatoses.". J Clin Pathol 58 (12): 1233-41. doi:10.1136/jcp.2005.027151. PMC 1770784. PMID 16311340. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770784/.
- ↑ URL: http://emedicine.medscape.com/article/1063499-overview. Accessed on: 23 September 2011.
- ↑ URL: http://www.dermpathmd.com/mnemonics/mnemonics_dermatopathology.htm. Accessed on: 23 September 2011.