Medical liver disease
This article deals with medical liver disease. An introduction to the liver and approach is found in the liver article.
Every differential in liver pathology has "drugs"[1] -- if it isn't clearly malignancy.
Liver neoplasms are dealt with in the liver neoplasms article.
Viral hepatitis
These are common. The diagnoses are based on serology. The serology is covered in the viral hepatitis section in the liver pathology article.
Typically classified as:[2][3]
- Acute < 6 months duration.
- Chronic > 6 months duration.
Hepatitis A
- Infection is self-limited, i.e. not persistent.
- May present as fulminant hepatic necrosis.
- Usually asymptomatic in children.[4]
- Serology is diagnostic.
Hepatitis B
- Hepatitis B virus, abbreviated HBV, redirects here.
General
- May lead to hepatocellular carcinoma without cirrhosis.
- High prevalence.
- Diagnosis is by serology.
Associated pathology:
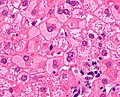
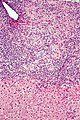
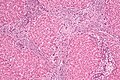
Microscopic
Features:
- Lobular inflammation - this is non-specific finding.
- Hepatocyte necrosis:
- Necrotic hepatocytes look a lot like neutrophils - however:
- Cytoplasm is more pink.
- Round apoptotic bodies.
- Necrotic hepatocytes look a lot like neutrophils - however:
- Hepatocyte necrosis:
- Ground glass hepatocytes - see liver pathology article.
DDx:
- Hepatitis C.
- Autoimmune hepatitis.
- Primary biliary cirrhosis without granulomas.
- Drug reaction.
Image
IHC
- Hepatitis B +ve.
Hepatitis C
General
- Leads to hepatocellular carcinoma in the setting of cirrhosis.
- Tends to be chronic; the "C" in "hepatitis C" stands for chronic.
- Diagnosis is by serology.
Associated pathology:
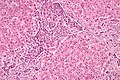
Microscopic
Features:
- Lobular inflammation - this is non-specific finding.
- Usually Grade 1, rarely Grade 2 and almost never Grade 3 or Grade 4.[5]
- Periportal steatosis in genotype 3.[6]
- Steatosis in hepatitis C is usually a secondary pathology, i.e. a separate pathologic process.[7]
DDx:
- Hepatitis B (without ground glass hepatocytes).
- Autoimmune hepatitis.
- Primary biliary cirrhosis without granulomas.
- Drug reaction.
Other infections
- Hydatid disease (Hydatid cyst).
- Ascaris.
- Fasciola
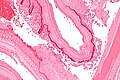
Hydatid disease
- AKA hydatid cyst.
General
- Etiology: Echinococcus.
Microscopic
Features:
- Laminated wall +/- calcification.[8]
- Organisms -- see Echinococcus.
Images
www:
Metabolic and toxic
Alcoholic liver disease
General
- Acute and/or chronic liver changes due to excessive alcohol use - includes:
Classic lab findings in EtOH abusers
- AST & ALT elevated with AST:ALT=2:1.
- GGT elevated.
- MCV increased.
Gross pathology/radiologic findings
- Classically micronodular pattern.
- May be macronodular.
Microscopic
See:
- Steatohepatitis section and ballooning degeneration section.
Features:
- Often zone III damage.
- Cholestatsis common, i.e. yellow staining.
- NASH (non-alcoholic steatohepatitis) usu. does not have cholestasis.[11]
- Fibrosis starts at central veins.
- Neutrophils (often helpful) -- few other things have PMNs. (???)
- Neutrophils cluster around cells with Mallory hyaline.
Notes:
- If portal inflammatory infiltrates more than mild, r/o other causes i.e. viral hepatitis.
- Mallory bodies once thought to be characteristic; now considered non-specific and generally poorly understood.[12]
- Some consider alcoholic liver disease a clinical diagnosis, i.e. as a pathologist one does not diagnose it.[13]
Non-alcoholic fatty liver disease
- Abbreviated NAFLD.
- Fatty liver that is not due to alcohol; includes obesity-related fatty liver, metabolic disease/diabetes-related fatty liver.
NASH
- Non-alcoholic steatohepatitis - see steatohepatitis section.
- Histologically indistinguishable from ASH.
- NASH is a clinical diagnosis based on exclusion of alcohol.
Steatohepatitis
General
- Steatohepatitis is a label for a set of histopathologic findings.
- Fat accumulation in hepatocytes.
- It may be a pattern seen in drug toxicity, e.g. methotrexate toxicity.[14]
Etiology:
- Alcohol = alcoholic steatohepatitis (ASH).
- Not alcohol = non-alcoholic steatohepatitis (NASH).
- Drug/toxin.[15]
Notes:
- Pathologists can comment on the etiology; however, the histomorphology is not distinctive. In other words, ASH and NASH are clinical diagnoses.
- Steatohepatitis is a misnomer. It is not an -itis; inflammation is not the (predominant) pathologic process.
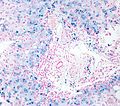
Microscopic
Features:
- Steatosis (usually macrovesicular) - key feature.
- If less than 10% ... consider alt. diagnosis/disease process.
- Hepatocyte injury:
- Ballooning degeneration - key feature (see introduction to liver).
- Mallory bodies.
- Mallory body wannabes: "occasional cytoplasmic clumping".
- +/-Chicken-wire perisinusoidal fibrosis +/- zone III (centrilobular) fibrosis (early).
- Late-stage disease - portal bridging.[16]
Image: Steatohepatitis (WC).
DDx:
Grading steatohepatitis
Grading inflammation:[17]
- Grade 1 - steatosis, occasional ballooning degeneration, PMNs.
- Grade 2 - obvious ballooning, obvious PMNs, chronic inflammation.
- Grade 3 - panacinar steatosis.
Autoimmune
Autoimmune hepatitis
Primary biliary cirrhosis
- Abbreviated PBC.
General
Epidemiology:
- Female>male (~9:1).[18]
- Usually middle age.
- Associated with other autoimmune conditions (Sjögren syndrome, progressive systemic sclerosis, celiac disease).
Etiology:
- Autoimmune.
Serology:
- AMA +ve.[19]
Classic presentation:
- Pruritis.
Pathophysiology:
- Septal bile duct attacked.
Treatment:
- Ursodeoxycholic acid.
- May be indication for transplant.
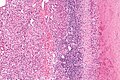
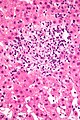
Microscopic
Features:
- "Florid duct lesion":[20]
- Intraepithelial lymphocytes - in bile duct - key feature.
- Bile duct epithelial cells with eosinophilic cytoplasm.[21]
- Plasma cells.
- Granulomas - close to bile duct.
- Seen in classic presentation -- often not present or poorly formed.
- Focal damage (may be missed on biopsy -- due to sampling).
- "Garland" cirrhosis -- has irregular border (unlike in EtOH).
- Garland originally "wreath of flowers" (in French).[22]
DDx:[23]
- Sarcoidosis (if granulomas present).
- Primary sclerosing cholangitis.
- Viral hepatitis.
- Autoimmune hepatitis.
- Drugs.
- Hodgkin's lymphoma.[24]
Notes:
- PAS stain useful for examining basement membrane... which is lost in PBC.
- Lobular inflammation should be minimal.
Images
www:
Staging PBC
PBC is staged according to Ludwig:[25]
- Stage 1: Portal - inflammation or bile duct abnormalities.
- Stage 2: Periportal - periportal fibrosis (enlargement of portal tracts) +/- inflammation.
- Stage 3: Septal - septal fibrosis +/-inflammation in septa.
- Stage 4: Cirrhosis - nodules of hepatocytes +/- inflammation.
Notes:
- There can be significant variation in staging on biopsy - due to variability of fibrosis in a PBC liver.[26]
- "Worst area" in biopsy specimen is used to determine stage.
Autoimmune hepatitis-primary biliary cirrhosis overlap syndrome
- Abbreviation AIH-PBC OS.
General
Epidemiology:
- Rare.
Serology:[27]
- AMA +ve.
- Anti-dsDNA +ve.
Microscopic
Primary sclerosing cholangitis
General
- Strongly associated with ulcerative colitis; 75-90% of PSC patients have inflammatory bowel disease (IBD).[29]
- Risk for cholangiocarcinoma.[30]
Serology:
- p-ANCA (MPO-ANCA) +ve in ~ 90% of cases.[31]
Diagnosis
- Diagnosed radiologically.
- Liver biopsy is rarely useful diagnostically[32] - as the disease may be patchy.
- The utility of the biopsy is staging.
Treatment
- None very good.
- May be indication for transplant.
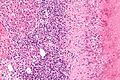
Microscopic
Features:
- Classic: "onion-skinning" - cells layer around the bile ducts; "onion skin" present in approx. 40% of cases.[33]
- Not pathognomonic for PSC[33] - but not too much else looks like this on microscopy (ergo good fellowship exam question).
- +/-Ductopenia.
- +/-Ductal proliferation.
DDx:
- Big.
Images:
Notes:
- PSC often has minimal inflammation.[36]
Staging
Features:[37]
- Stage I - focal portal inflammation, +/- duct abnormalities, no fibrosis.
- Stage II - portal enlargement (fibrosis), +/- inflammation.
- Stage III - bridging fibrosis + necrosis.
- Stage IV - cirrhosis.
Notes:
- Similar to PBC staging.
Hereditary
Caroli disease
General
- Genetic disease.
- Frequently associated with autosomal recessive polycystic kidney disease (ARPKD).[38]
- May be seen in isolation.[39]
Clinical:[40]
- Recurrent cholangitis.
- Recurrent cholelithiasis.
- Cholangiocarcinoma[41] - seen in ~7% of cases.[42]
Note:
- Caroli syndrome = Caroli disease + congenital hepatic fibrosis.[43]
Gross
- Dilated bile ducts.[38]
Microscopic
Features:[40]
- Dilated bile ducts.
- Periductal fibrosis. (???)
- +/-Fibrosis.
Image:
Hereditary hemochromatosis
- For secondary causes see secondary hemochromatosis.
General
Epidemiology:
- Genetic defect - HFE gene.[45]
- Onset in males earlier than females (due to menses).
- Mutation thought to confer survival advantage - several theories (increased resistance to TB, S. typhi vs. decreased iron deficiency/increased iron absorption).[46]
Associated pathology (mnemonic: hemochromatosis can cause deposits anywhere):[47][48]
- Hypogonadism.
- Cirrhosis and HCC.
- Cardiomyopathy - DCM (esp. with his63asp mutation),[49] may be RCM.
- Diabetes mellitus (bronze diabetes).
- Arthropathy.[50]
Pathophysiology:
- Iron overload -> cirrhosis.
Microscopic
Features:
- Periportal iron deposition (early).
- Late stage disease has diffuse iron deposition.
- Brown granular - may vaguely look like lipofuscin on H&E.
Notes:
- Iron in the bile ducts and endothelium used to be though specific of hereditary hemochromatosis.[51]
- It is now thought to just reflect the severity of iron deposition, i.e. if the bile ducts and endothelium have iron - it is severe.
DDx - secondary hemochromatosis:
- Myelodysplastic syndrome.
- Chronic hemolysis.
- Alcoholic liver disease; iron deposition common in cirrhosis.
Images
www:
Stains
Iron stain +ve -- important.
- Light blue haze is not enough.
- Must be separated from siderosis -- iron in Kupffer cells.
Molecular
- PCR - diagnostic - see molecular pathology tests.
Wilson disease
General
Epidemiology:
- Rare autosomal recessive - mutation in copper-transporting adenosine triphosphatase (ATPase) gene (ATP7B).[52][53]
- Heterozygote carrier rate approximately 1/100 persons.[52]
- Young individuals - usually 12-23 years old.
Clinical:
- Kayser-Fleischer rings --> on slit-lamp examination (green eyes).
- May present to psychiatry or appear to be abusing EtOH.
- Serum ceruloplasmin - lower than normal.
Etiology:
- Excess copper -- due to genetic defect.
Microscopic
Features:
- Nothing specific - known as the great mimicker of live pathology.
- Steatosis.
- Portal fibrosis.
Stains
- Copper staining positive - only 15% of cases.
- Other stains: rhodinine (red/orange granules = positive), orecin.
Notes:
- Copper staining is a non-specific finding seen in many liver diseases; it is associated with impaired bile secretion.[54]
Additional testing
- Mass spectrometry - determine portion of copper.
Alpha-1 antitrypsin deficiency
- AKA alpha1-antiprotease inhibitor deficiency.
General
Etiology:
- Genetic defect.
- Prevalence 1 in 2000-5000.[55]
Causes:
- Lung and liver injury.
- Lung -> panlobular emphysema.
Microscopic
Features:
- Pink globules in zone 1 (periportal).
- Globules not seen in children.
- May not be present in late stage (cirrhotic).
- Best seen on PASD stain.
- Can be seen on H&E -- if one looks carefully.
Note:
- The pink globules may be seen in the context of cirrhosis; cases should be confirmation with IHC.
Images:
Stains
IHC
- A1-AT +ve globules.[57]
Other
Budd-Chiari syndrome
- AKA hepatic vein obstruction.
General
- Hepatic outflow obstruction.
Clinical triad:[58]
- Ascites.
- Abdominal pain.
- Hepatomegaly.
Etiology:
- ~50% have a myeloproliferative disease.[59]
- May be due to mass effect from a tumour.
Clinical DDx:
Microscopic
Features:[60]
- Sinusoidal dilation in zone III (congestion).
- +/-Hepatocyte drop-out.
- +/-Centrilobular fibrosis.
DDx congestion:
- Congestive heart failure (congestive hepatopathy).
- Constrictive pericarditis.
Vanishing bile duct syndrome
General
- Fatal.
DDx:[62]
- Primary biliary cirrhosis.
- Primary sclerosing cholangitis.
- GVHD.[63]
- Drugs.[64]
- Chronic rejection.[61]
Microscopic
Features:[62]
- Loss of intrahepatitic bile ducts - key feature.
- Cholestasis.
Note:
- May occur without fibrosis and inflammation; thus, can be easy to miss.
IHC
- CK7 -ve.
- Marks bile ducts.
Congestive hepatopathy
General
- Liver failure due to (right) heart failure.
- AKA cardiac cirrhosis - a term used by clinicians.
- Generally, it does not satisfy pathologic criteria for cirrhosis.[65]
Gross
- "Nutmeg" liver - yellow spotted appearance.
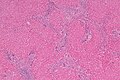
Microscopic
Features:[66]
- Zone III atrophy.
- Portal venule (central vein) distension.
- Perisinusoidal fibrosis - progresses to centrilobular fibrosis and then diffuse fibrosis.
- Dilation of sinusoids in all zone III areas - key feature.[67]
Image: Congestive hepatopathy (WC).
Drug-induced liver disease
- AKA drug-induced liver toxicity.
General
- Drugs can do almost anything; may include: granulomata, bile duct loss, cholestasis, ischemic type injury.
- Effects can be delayed -- temporal relationship not always obvious.
Microscopic
Features:
- Non-specific findings.
- +/-Eosinophils[68] - significant suggestive finding.
- +/-Steatosis - periportal macrovesicular, microvesicular.
- +/-Vanishing bile duct syndrome.
- +/-Granulomas.
Images
Specific patterns
Acute hepatits:
- Related to Rx - most often antibiotics.
Steatohepatitis/steatosis:[69]
- Amiodarone - cardiac arrhythmias.
- Tamoxifen - breast cancer.
- Carbamazepine - seizures.
Specific drugs
Acetaminophen:
- Zone 3 necrosis.
Methotrexate - chronic use:
- Histology:[72]
- Features of steatohepatitis.
- Zone III steatosis.
- Ballooning degeneration.
- Portal inflammation with mixed population (lymphocytes, macrophages, PMNs).
- Nuclear atypia (hyperchromasia, pleomorphism, vacuolation).
- Described as just nuclear size variation by some.[73]
- Features of steatohepatitis.
Focal nodular hyperplasia
- Abbreviated FNH.
General
- Not commonly seen by pathologists, as these are usually distinctive on medical imaging.[74]
- Benign lesions.
- May be seen in the context of hereditary hemorrhagic telangiectasia.[75]
Note:
- Oral contraceptive pill (OCP) use does not appear to be a factor in the growth of these lesions;[76] however, the study claims there is nothing on hepatocellular adenomas -- yet I found a JAMA paper by Rooks et al.[77] on this topic.
Imaging
Gross
Features:[79]
- Well circumscribed, but no capsule.
- Lighter than surrounding parenchyma, may be yellow.
- +/-Stellate central scar with thick vessels.
- Can be identified on medial imaging.
Note: Usually a solitary lesion.[78]
Microscopic
Features:[79]
- Classically a stellate scar that has large arteries with fibromuscular hyperplasia.
- Thin fibrous septa radiate from the central scar - surrounded by lymphocytes & bile ductules.
- Normal hepatocytes between fibrous septae.
- Thin fibrous septa radiate from the central scar - surrounded by lymphocytes & bile ductules.
Practical features:
- Thick walled blood vessels.
- Bile duct of same size not seen.
- Bile ductular proliferation at the edge of the fibrosis tissue.
- Clinical history: it is a focal lesion.
DDx:
- Hepatic adenoma - may be difficult to distinguish, if no scar and no ductal proliferation.[80]
- Cirrhosis - complete nodules
- FNH has incomplete nodules.
Memory device FNH = focal lesion, numerous bile ductules, hyperplasia of arteries.
Images
www:
Nodular regenerative hyperplasia
General
- Associated with renal transplants, bone marrow transplants and vasculitides.[79]
- Can lead to portal hypertension and many of the associated complications.[81]
Etiology
- Arterial hypervascularity secondary to loss of hepatic vein radicles (loss of central venule in hepatic lobule).[79]
ASIDE: radicle = ramulus - smallest branch or vessel or nerve.[82]
Gross
- Diffuse nodularity - whole liver.
Microscopic
Features:[79]
- "Plump" hepatocytes surrounded by atrophic ones.
- No fibrosis.
Sinuosoidal obstruction syndrome
- May be referred to as Hepatic veno-occlusive disease.[83]
General
Clinical DDx:
Microscopic
Features:[60]
- Subendothelial swelling in hepatic venules.
Negatives:
- No thrombosis.
Polycystic kidney disease and the liver
General
Complications of PKD in the liver:[85]
- Infected cyst.
- Cholangiocarcinoma.
- Cholestasis/obstruction due to duct compression.[86]
Cysts:
- Cysts in the liver, like the kidney, are thought to enlarge with age.
Microscopic
Features:[87]
- Von Meyenburg complexes (bile duct hamartoma):
- Cluster of dilated ducts with "altered" bile.
- Surrounded by collagenous stroma.
- Separate from the portal areas.[88]
Images:
Notes:
Peliosis hepatis
General
- Associated with:
- Infections.
- Malignancy.
- Other stuff.
- Rarely biopsied.
Microscopic
Features:
- Cyst lined by endothelium.
- Usu. incomplete.
- Blood.
Total parenteral nutrition
- Abbreviated TPN.
General
- Indication: short gut syndrome, others.
Microscopic
Variable - may range from: steatosis, steatohepatitis, cholestasis, fibrosis and cirrhosis.[91]
- Steatosis (periportal) - early.
- Cholestasis - late.
Giant cell hepatitis
- AKA neonatal giant cell hepatitis.
- See: Giant cell hepatitis.
Hepatic amyloidosis
General
- Diffuse abundant amyloid within the space of Disse is associated with portal hypertension.[94]
Microscopic
Features:
- Amorphous extracellular pink stuff on H&E - see amyloid article.
DDx:
Images:
Stains
- Congo red +ve.
Fulminant hepatic necrosis
General
Etiology:
- Viral, i.e. Hepatitis A, Hepatitis B; Hepatitis C - extremely rare.
- Trauma.
- Shock.
Microscopic
Features:
- Hepatocyte necrosis.
- Bile duct proliferation.
DDx:
Secondary hemochromatosis
- For the hereditary one see hereditary hemochromatosis.
General
- Iron overload secondary to blood transfusions for hereditary or acquired anemia.[95]
- Primary hemochromatosis due to a defect in iron processing - called hereditary hemochromatosis.
- Imaging considered the best test, as iron deposition is patchy.[95]
Selected hereditary causes:[95]
- Thalassemia.
- Sickle cell anemia.
- Hereditary sideroblastic anemia.
Selected acquired causes:[95]
- Myelodysplastic syndromes
- Myelofibrosis
- Aplastic anemia, intractable.
Microscopic
See also
References
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 448. ISBN 978-1416054542.
- ↑ "Terminology of chronic hepatitis, hepatic allograft rejection, and nodular lesions of the liver: summary of recommendations developed by an international working party, supported by the World Congresses of Gastroenterology, Los Angeles, 1994.". Am J Gastroenterol 89 (8 Suppl): S177-81. Aug 1994. PMID 8048409.
- ↑ URL: http://familydoctor.org/familydoctor/en/diseases-conditions/hepatitis-b.html. Accessed on: 2 May 2012.
- ↑ Jeong SH, Lee HS (2010). "Hepatitis A: clinical manifestations and management". Intervirology 53 (1): 15–9. doi:10.1159/000252779. PMID 20068336.
- ↑ STC. 6 December 2010.
- ↑ Yoon EJ, Hu KQ. Hepatitis C virus (HCV) infection and hepatic steatosis. Int J Med Sci. 2006;3(2):53-6. Epub 2006 Apr 1. PMID 16614743. Avialable at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1415843. Accessed on: September 9, 2009.
- ↑ OA. September 2009.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 448. ISBN 978-1416054542.
- ↑ URL: http://emedicine.medscape.com/article/170539-overview. Accessed on: 3 May 2012.
- ↑ STC. 6 December 2010.
- ↑ STC. 6 December 2010.
- ↑ Jensen K, Gluud C (November 1994). "The Mallory body: theories on development and pathological significance (Part 2 of a literature survey)". Hepatology 20 (5): 1330-42. PMID 7927269.
- ↑ MG. September 2009.
- ↑ MG. 22 September 2009.
- ↑ Farrell, GC. (2002). "Drugs and steatohepatitis.". Semin Liver Dis 22 (2): 185-94. doi:10.1055/s-2002-30106. PMID 12016549.
- ↑ Gramlich, T.; Kleiner, DE.; McCullough, AJ.; Matteoni, CA.; Boparai, N.; Younossi, ZM. (Feb 2004). "Pathologic features associated with fibrosis in nonalcoholic fatty liver disease.". Hum Pathol 35 (2): 196-9. PMID 14991537.
- ↑ Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Am J Gastroenterol. 1999 Sep;94(9):2467-74. PMID 10484010.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 162. ISBN 978-0470519035.
- ↑ Nguyen, DL.; Juran, BD.; Lazaridis, KN. (Oct 2010). "Primary biliary cirrhosis.". Best Pract Res Clin Gastroenterol 24 (5): 647-54. doi:10.1016/j.bpg.2010.07.006. PMID 20955967.
- ↑ Nakanuma, Y.; Harada, K. (Sep 1993). "Florid duct lesion in primary biliary cirrhosis shows highly proliferative activities.". J Hepatol 19 (2): 216-21. PMID 7905494.
- ↑ OA. 11 September 2009.
- ↑ http://dictionary.reference.com/browse/garland
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 163. ISBN 978-0470519035.
- ↑ Vanishing bile duct syndrome and Hodgkin disease: a case series and review of the literature. Pass AK, McLin VA, Rushton JR, Kearney DL, Hastings CA, Margolin JF. J Pediatr Hematol Oncol. 2008 Dec;30(12):976-80. PMID 19131796.
- ↑ PBC. eMedicine.com. URL: http://emedicine.medscape.com/article/171117-diagnosis. Accessed on: 22 September 2009.
- ↑ J Clin Pathol. 1996 July; 49(7): 556-559. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=500569. Accessed on: September 22, 2009.
- ↑ Muratori, P.; Granito, A.; Pappas, G.; Pendino, GM.; Quarneti, C.; Cicola, R.; Menichella, R.; Ferri, S. et al. (Jun 2009). "The serological profile of the autoimmune hepatitis/primary biliary cirrhosis overlap syndrome.". Am J Gastroenterol 104 (6): 1420-5. doi:10.1038/ajg.2009.126. PMID 19491855.
- ↑ URL: http://emedicine.medscape.com/article/181889-overview. Accessed on: 25 January 2012.
- ↑ Khurana V, Singh T. Primary sclerosing cholangitis. eMedicine.com. URL: http://emedicine.medscape.com/article/187724-overview. Accessed on: 29 November 2009.
- ↑ Jesudian, AB.; Jacobson, IM. (2009). "Screening and diagnosis of cholangiocarcinoma in patients with primary sclerosing cholangitis.". Rev Gastroenterol Disord 9 (2): E41-7. PMID 19668124.
- ↑ Terjung, B.; Worman, HJ. (Aug 2001). "Anti-neutrophil antibodies in primary sclerosing cholangitis.". Best Pract Res Clin Gastroenterol 15 (4): 629-42. doi:10.1053/bega.2001.0209. PMID 11492972.
- ↑ Khurana V, Singh T. Primary sclerosing cholangitis. eMedicine.com. URL: http://emedicine.medscape.com/article/187724-diagnosis. Accessed on: 29 November 2009.
- ↑ 33.0 33.1 Steele et al. URL: http://www.medscape.com/viewarticle/552500_6. Accessed on: 29 November 2009.
- ↑ URL: http://trialx.com/curebyte/2011/07/08/clinical-trials-and-images-of-primary-sclerosing-cholangitis/. Accessed on: 1 January 2012.
- ↑ URL: http://www.onmedica.com/NewsArticle.aspx?id=d7f992b5-6dee-46c6-8383-bbdfb4528ccc. Accessed on: 1 January 2011.
- ↑ STC. 9 December 2010.
- ↑ Steele et al. URL: http://www.medscape.com/viewarticle/552500_6. Accessed on: 29 November 2009.
- ↑ 38.0 38.1 Online 'Mendelian Inheritance in Man' (OMIM) 263200
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 600643
- ↑ 40.0 40.1 Yonem, O.; Bayraktar, Y. (Apr 2007). "Clinical characteristics of Caroli's syndrome.". World J Gastroenterol 13 (13): 1934-7. PMID 17461493.
- ↑ Yonem, O.; Bayraktar, Y. (Apr 2007). "Clinical characteristics of Caroli's disease.". World J Gastroenterol 13 (13): 1930-3. PMID 17461492.
- ↑ Karim, AS. (Aug 2004). "Caroli's disease.". Indian Pediatr 41 (8): 848-50. PMID 15347876.
- ↑ Brancatelli, G.; Federle, MP.; Vilgrain, V.; Vullierme, MP.; Marin, D.; Lagalla, R.. "Fibropolycystic liver disease: CT and MR imaging findings.". Radiographics 25 (3): 659-70. doi:10.1148/rg.253045114. PMID 15888616.
- ↑ URL: http://www.meddean.luc.edu/lumen/MedEd/orfpath/develop.htm. Accessed on: 1 December 2011.
- ↑ 45.0 45.1 Online 'Mendelian Inheritance in Man' (OMIM) 613609
- ↑ 46.0 46.1 Weinberg ED (2008). "Survival advantage of the hemochromatosis C282Y mutation". Perspect. Biol. Med. 51 (1): 98-102. doi:10.1353/pbm.2008.0001. PMID 18192769.
- ↑ URL: http://en.wikibooks.org/wiki/USMLE_Step_2_Review. Accessed on: 15 March 2012.
- ↑ Fix, OK.; Kowdley, KV. (Dec 2008). "Hereditary hemochromatosis.". Minerva Med 99 (6): 605-17. PMID 19034258.
- ↑ Mahon, NG.; Coonar, AS.; Jeffery, S.; Coccolo, F.; Akiyu, J.; Zal, B.; Houlston, R.; Levin, GE. et al. (Nov 2000). "Haemochromatosis gene mutations in idiopathic dilated cardiomyopathy.". Heart 84 (5): 541-7. PMID 11040018.
- ↑ von Kempis, J. (Jan 2001). "Arthropathy in hereditary hemochromatosis.". Curr Opin Rheumatol 13 (1): 80-3. PMID 11148720.
- ↑ MG. 17 September 2009.
- ↑ 52.0 52.1 http://emedicine.medscape.com/article/183456-overview
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 606882
- ↑ Miyamura H, Nakanuma Y, Kono N (December 1988). "Survey of copper granules in liver biopsy specimens from various liver abnormalities other than Wilson's disease and biliary diseases". Gastroenterol. Jpn. 23 (6): 633–8. PMID 2464523.
- ↑ Stoller, JK.; Aboussouan, LS. (Sep 2011). "A Review of Alpha-1 Antitrypsin Deficiency.". Am J Respir Crit Care Med. doi:10.1164/rccm.201108-1428CI. PMID 21960536.
- ↑ 56.0 56.1 Qizilbash, A.; Young-Pong, O. (Jun 1983). "Alpha 1 antitrypsin liver disease differential diagnosis of PAS-positive, diastase-resistant globules in liver cells.". Am J Clin Pathol 79 (6): 697-702. PMID 6189389.
- ↑ Theaker, JM.; Fleming, KA. (Jan 1986). "Alpha-1-antitrypsin and the liver: a routine immunohistological screen.". J Clin Pathol 39 (1): 58-62. PMID 3512609.
- ↑ Fox, MA.; Fox, JA.; Davies, MH. (2011). "Budd-Chiari syndrome--a review of the diagnosis and management.". Acute Med 10 (1): 5-9. PMID 21573256.
- ↑ Plessier, A.; Valla, DC. (Aug 2008). "Budd-Chiari syndrome.". Semin Liver Dis 28 (3): 259-69. doi:10.1055/s-0028-1085094. PMID 18814079.
- ↑ 60.0 60.1 60.2 Aydinli, M.; Bayraktar, Y. (May 2007). "Budd-Chiari syndrome: etiology, pathogenesis and diagnosis.". World J Gastroenterol 13 (19): 2693-6. PMID 17569137. http://www.wjgnet.com/1007-9327/full/v13/i19/2693.htm.
- ↑ 61.0 61.1 Inomata, Y.; Tanaka, K. (2001). "Pathogenesis and treatment of bile duct loss after liver transplantation.". J Hepatobiliary Pancreat Surg 8 (4): 316-22. doi:10.1007/s0053410080316. PMID 11521176.
- ↑ 62.0 62.1 Reau, NS.; Jensen, DM. (Feb 2008). "Vanishing bile duct syndrome.". Clin Liver Dis 12 (1): 203-17, x. doi:10.1016/j.cld.2007.11.007. PMID 18242505.
- ↑ Yeh, KH.; Hsieh, HC.; Tang, JL.; Lin, MT.; Yang, CH.; Chen, YC. (Aug 1994). "Severe isolated acute hepatic graft-versus-host disease with vanishing bile duct syndrome.". Bone Marrow Transplant 14 (2): 319-21. PMID 7994249.
- ↑ Chitturi, S.; Farrell, GC. (Apr 2001). "Drug-induced cholestasis.". Semin Gastrointest Dis 12 (2): 113-24. PMID 11352118.
- ↑ URL: http://emedicine.medscape.com/article/151792-overview. Accessed on: 17 June 2010.
- ↑ URL: http://emedicine.medscape.com/article/151792-diagnosis. Accessed on: 17 June 2010.
- ↑ Suggested by OA. September 2009.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 166. ISBN 978-0470519035.
- ↑ Grieco, A.; Forgione, A.; Miele, L.; Vero, V.; Greco, AV.; Gasbarrini, A.; Gasbarrini, G.. "Fatty liver and drugs.". Eur Rev Med Pharmacol Sci 9 (5): 261-3. PMID 16237810.
- ↑ 70.0 70.1 Millea PJ (August 2009). "N-acetylcysteine: multiple clinical applications". Am Fam Physician 80 (3): 265–9. PMID 19621836.
- ↑ URL: http://www.mskcc.org/mskcc/html/69310.cfm. Accessed on: 19 October 2010.
- ↑ Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 715. ISBN 978-0-443-10012-3.
- ↑ MG. 23 September 2009.
- ↑ 74.0 74.1 Brancatelli, G.; Federle, MP.; Grazioli, L.; Blachar, A.; Peterson, MS.; Thaete, L. (Apr 2001). "Focal nodular hyperplasia: CT findings with emphasis on multiphasic helical CT in 78 patients.". Radiology 219 (1): 61-8. PMID 11274535.
- ↑ Khalid SK, Garcia-Tsao G (August 2008). "Hepatic vascular malformations in hereditary hemorrhagic telangiectasia". Semin. Liver Dis. 28 (3): 247–58. doi:10.1055/s-0028-1085093. PMID 18814078.
- ↑ Kapp, N.; Curtis, KM. (Oct 2009). "Hormonal contraceptive use among women with liver tumors: a systematic review.". Contraception 80 (4): 387-90. doi:10.1016/j.contraception.2009.01.021. PMID 19751862.
- ↑ Rooks, JB.; Ory, HW.; Ishak, KG.; Strauss, LT.; Greenspan, JR.; Hill, AP.; Tyler, CW. (Aug 1979). "Epidemiology of hepatocellular adenoma. The role of oral contraceptive use.". JAMA 242 (7): 644-8. PMID 221698.
- ↑ 78.0 78.1 http://emedicine.medscape.com/article/368377-overview
- ↑ 79.0 79.1 79.2 79.3 79.4 Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 922. ISBN 0-7216-0187-1.
- ↑ STC. 19 Jan 2009.
- ↑ Bissonnette, J.; Généreux, A.; Côté, J.; Nguyen, B.; Perreault, P.; Bouchard, L.; Pomier-Layrargues, G. (Aug 2012). "Hepatic hemodynamics in 24 patients with nodular regenerative hyperplasia and symptomatic portal hypertension.". J Gastroenterol Hepatol 27 (8): 1336-40. doi:10.1111/j.1440-1746.2012.07168.x. PMID 22554152.
- ↑ Dorland's Medical Dictionary. 30th Ed.
- ↑ DeLeve, LD.; Shulman, HM.; McDonald, GB. (Feb 2002). "Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome (veno-occlusive disease).". Semin Liver Dis 22 (1): 27-42. doi:10.1055/s-2002-23204. PMID 11928077..
- ↑ Helmy, A. (Jan 2006). "Review article: updates in the pathogenesis and therapy of hepatic sinusoidal obstruction syndrome.". Aliment Pharmacol Ther 23 (1): 11-25. doi:10.1111/j.1365-2036.2006.02742.x. PMID 16393276.
- ↑ Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 174-5. ISBN 978-0-443-10012-3.
- ↑ URL: http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=9184868. Accessed on: 23 September 2009.
- ↑ Burt, Alastair D.;Portmann, Bernard C.;Ferrell, Linda D. (2006). MacSween's Pathology of the Liver (5th ed.). Churchill Livingstone. pp. 176. ISBN 978-0-443-10012-3.
- ↑ Meyenburg complex. Stedman's Medical Dictionary. 27th Ed.
- ↑ Bile duct hamartomas--the von Meyenburg complex. Salles VJ, Marotta A, Netto JM, Speranzini MB, Martins MR. Hepatobiliary Pancreat Dis Int. 2007 Feb;6(1):108-9. PMID 17287178.
- ↑ [The von Meyenburg complex] Schwab SA, Bautz W, Uder M, Kuefner MA. Rontgenpraxis. 2008;56(6):241-4. German. PMID 19294869.
- ↑ Guglielmi FW, Boggio-Bertinet D, Federico A, et al. (September 2006). "Total parenteral nutrition-related gastroenterological complications". Dig Liver Dis 38 (9): 623–42. doi:10.1016/j.dld.2006.04.002. PMID 16766237.
- ↑ Li, SJ.; Nussbaum, MS.; McFadden, DW.; Gapen, CL.; Dayal, R.; Fischer, JE. (Aug 1988). "Addition of glucagon to total parenteral nutrition (TPN) prevents hepatic steatosis in rats.". Surgery 104 (2): 350-7. PMID 3135627.
- ↑ Stanko, RT.; Nathan, G.; Mendelow, H.; Adibi, SA. (Jan 1987). "Development of hepatic cholestasis and fibrosis in patients with massive loss of intestine supported by prolonged parenteral nutrition.". Gastroenterology 92 (1): 197-202. PMID 3096806.
- ↑ Bion, E.; Brenard, R.; Pariente, EA.; Lebrec, D.; Degott, C.; Maitre, F.; Benhamou, JP. (Feb 1991). "Sinusoidal portal hypertension in hepatic amyloidosis.". Gut 32 (2): 227-30. PMC 1378815. PMID 1864548. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1378815/.
- ↑ 95.0 95.1 95.2 95.3 Gattermann, N. (Jul 2009). "The treatment of secondary hemochromatosis.". Dtsch Arztebl Int 106 (30): 499-504, I. doi:10.3238/arztebl.2009.0499. PMC 2735704. PMID 19727383. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2735704/.