Difference between revisions of "Fibroblastic/myofibroblastic tumours"
m (→Microscopic) |
(split out) |
||
| (116 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
This article covers '''fibroblastic/myofibroblastic tumours'''. These tumours fit into the larger category of [[soft tissue lesions]]. | This article covers '''fibroblastic/myofibroblastic tumours'''. These tumours fit into the larger category of [[soft tissue lesions]]. | ||
=List of tumours= | |||
===Benign=== | ===Benign=== | ||
WHO classification:<ref name=Ref_WMSP601>{{Ref WMSP|601}}</ref> | WHO classification:<ref name=Ref_WMSP601>{{Ref WMSP|601}}</ref> | ||
*[[Nodular fasciitis]]. | *[[Nodular fasciitis]]. | ||
*Proliferative fasciitis. | *[[Proliferative fasciitis]]. | ||
*Proliferative myositis. | *[[Proliferative myositis]]. | ||
*[[Myositis ossificans]]. | *[[Myositis ossificans]]. | ||
*Ischemic fasciitis. | *Ischemic fasciitis. | ||
*Elastofibroma. | *[[Elastofibroma]]. | ||
*Myofibroma. | *[[Myofibroma]]. | ||
*Fibromatosis coli | *Fibromatosis colli. <!-- NOT 'coli' --> | ||
*Inclusion body fibromatosis. | *Inclusion body fibromatosis. | ||
*Fibroma of tendon sheath. | *Fibroma of tendon sheath. | ||
*Calcifying aponeurotic fibroma. | *Calcifying aponeurotic fibroma. | ||
* | *[[Angiomyofibroblastoma]]. | ||
*Cellular angiofibroma. | *[[Cellular angiofibroma]]. | ||
*Nuchal-type fibroma. | *Nuchal-type fibroma. | ||
*Gardner fibroma. | *Gardner fibroma. | ||
| Line 25: | Line 25: | ||
*Fibrous hamartoma of infancy. | *Fibrous hamartoma of infancy. | ||
*Juvenile hyaline fibromatosis. | *Juvenile hyaline fibromatosis. | ||
*Desmoplastic fibroblastoma. | *[[Desmoplastic fibroblastoma]]. | ||
*Mammary-type myofibroblastoma. | *Mammary-type myofibroblastoma. | ||
| Line 32: | Line 32: | ||
*Superfical fibromatosis. | *Superfical fibromatosis. | ||
*[[Desmoid-type fibromatosis]]. | *[[Desmoid-type fibromatosis]]. | ||
*Lipofibromatosis. | *[[Lipofibromatosis]]. | ||
===Occasionally metastasizing=== | ===Occasionally metastasizing=== | ||
| Line 38: | Line 38: | ||
*[[Solitary fibrous tumour]]. | *[[Solitary fibrous tumour]]. | ||
*[[Inflammatory myofibroblastic tumour]]. | *[[Inflammatory myofibroblastic tumour]]. | ||
*Low-grade myofibroblastic sarcoma. | *[[Low-grade myofibroblastic sarcoma]]. | ||
*Myxoinflammatory fibroblastic sarcoma. | *Myxoinflammatory fibroblastic sarcoma. | ||
*[[Infantile fibrosarcoma]]. | *[[Infantile fibrosarcoma]]. | ||
| Line 49: | Line 49: | ||
*Sclerosing epithelioid fibrosarcoma. | *Sclerosing epithelioid fibrosarcoma. | ||
== | =Non-malignant= | ||
==Proliferative fasciitis== | |||
===General=== | ===General=== | ||
* | *Benign. | ||
* | *May mimic a sarcoma.<ref name=pmid1058047>{{Cite journal | last1 = Chung | first1 = EB. | last2 = Enzinger | first2 = FM. | title = Proliferative fasciitis. | journal = Cancer | volume = 36 | issue = 4 | pages = 1450-8 | month = Oct | year = 1975 | doi = | PMID = 1058047 }}</ref> | ||
Clinical: | |||
*Solid subcutaneous nodule. | |||
*Rapid growth. | |||
*May be painful. | |||
===Gross=== | |||
*Classically upper and lower extremities.<ref name=pmid1058047/> | |||
*Poorly demarcated. | |||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name= | Features:<ref name=pmid1566969>{{Cite journal | last1 = Meis | first1 = JM. | last2 = Enzinger | first2 = FM. | title = Proliferative fasciitis and myositis of childhood. | journal = Am J Surg Pathol | volume = 16 | issue = 4 | pages = 364-72 | month = Apr | year = 1992 | doi = | PMID = 1566969 }}</ref> | ||
* | *Large polygonal (ganglion-like) and/or spindled cells with: | ||
** | **[[Vesicular nuclei|Vesicular (clear) nuclei]]. | ||
** | **Prominent nucleoli. | ||
*+/-Binucleation. | |||
*Loose myxoid stroma. | |||
*+/- | *Frequent typical mitoses. | ||
* | **'''No''' atypical mitoses. | ||
* | |||
* | |||
* | |||
DDx: | DDx: | ||
*[[ | *[[Inflammatory myofibroblastic tumour]].<ref name=pmid17938159>{{Cite journal | last1 = Gleason | first1 = BC. | last2 = Hornick | first2 = JL. | title = Inflammatory myofibroblastic tumours: where are we now? | journal = J Clin Pathol | volume = 61 | issue = 4 | pages = 428-37 | month = Apr | year = 2008 | doi = 10.1136/jcp.2007.049387 | PMID = 17938159 }}</ref> | ||
*[ | |||
*[ | Images: | ||
*[http://www.medicine.virginia.edu/clinical/departments/pathology/Case%20Studies/known-pathology-cases/95_4-page Proliferative fasciitis - several images (virginia.edu)]. | |||
*[http://www.surgicalpathologyatlas.com/glfusion/mediagallery/media.php?f=0&sort=0&s=20090721114221299 Proliferative fasciitis (surgicalpathologyatlas.com)]. | |||
==Proliferative myositis== | |||
===General=== | |||
*Benign. | |||
*Possible arise from pericytes.<ref name=pmid2058761/> | |||
===Microscopic=== | |||
Features:<ref name=pmid2058761>{{Cite journal | last1 = el-Jabbour | first1 = JN. | last2 = Bennett | first2 = MH. | last3 = Burke | first3 = MM. | last4 = Lessells | first4 = A. | last5 = O'Halloran | first5 = A. | title = Proliferative myositis. An immunohistochemical and ultrastructural study. | journal = Am J Surg Pathol | volume = 15 | issue = 7 | pages = 654-9 | month = Jul | year = 1991 | doi = | PMID = 2058761 }}</ref><ref name=pmid1586481>{{Cite journal | last1 = Lundgren | first1 = L. | last2 = Kindblom | first2 = LG. | last3 = Willems | first3 = J. | last4 = Falkmer | first4 = U. | last5 = Angervall | first5 = L. | title = Proliferative myositis and fasciitis. A light and electron microscopic, cytologic, DNA-cytometric and immunohistochemical study. | journal = APMIS | volume = 100 | issue = 5 | pages = 437-48 | month = May | year = 1992 | doi = | PMID = 1586481 }}</ref> | |||
*Large ganglion-like cells. | |||
**Cells have single prominent nucleolus. | |||
*Spindle cells. | |||
*+/-Binucleation. | |||
*Mitotic activity. | |||
**No atypical mitoses. | |||
Image: | |||
*[http://commons.wikimedia.org/wiki/File:Proliferative_myositis_%28HE%29.jpg Proliferative myositis (WC)]. | |||
===IHC=== | |||
Features:<ref name=pmid2058761/> | |||
*Vimentin +ve. | |||
*SMA +ve. | |||
*Desmin +ve/-ve. | |||
Others:<ref name=pmid2058761/> | |||
*Factor XIIIa -ve. | |||
*S100 -ve. | |||
*CAM5.2 -ve. | |||
*NSE -ve. | |||
==Elastofibroma== | |||
{{Main|Elastofibroma}} | |||
==Nodular fasciitis== | ==Nodular fasciitis== | ||
{{Main|Nodular fasciitis}} | |||
==Desmoid-type fibromatosis== | |||
*[[AKA]] ''desmoid tumour''. | |||
*[[AKA]] ''desmoid fibromatosis''. | |||
{{Main|Desmoid-type fibromatosis}} | |||
==Lipofibromatosis== | |||
*[[AKA]] infantile subcutaneous fibromatosis. | |||
===General=== | ===General=== | ||
* | *Childhood. | ||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name= | Features:<ref name=Ref_WMSP609>{{Ref WMSP|609}}</ref> | ||
* | *Fibroblastic cells surrounding adipocytes. | ||
Image: | |||
*[http://cases.edinburgh-dermatopathology.org.uk/#2.0 Lipofibromatosis (edinburgh-dermatopathology.org.uk)]. | |||
* | ===IHC=== | ||
Features:<ref name=Ref_WMSP609>{{Ref WMSP|609}}</ref> | |||
*CD34 +ve. | |||
*BCL2 +ve. | |||
*S100 +ve. | |||
*CD99 +ve. | |||
*Actin +ve. | |||
*EMA +ve. | |||
==Desmoplastic fibroblastoma== | |||
*AKA ''collagenous fibroma''.<ref name=pmid18271804>{{Cite journal | last1 = Watanabe | first1 = H. | last2 = Ishida | first2 = Y. | last3 = Nagashima | first3 = K. | last4 = Makino | first4 = T. | last5 = Norisugi | first5 = O. | last6 = Shimizu | first6 = T. | title = Desmoplastic fibroblastoma (collagenous fibroma). | journal = J Dermatol | volume = 35 | issue = 2 | pages = 93-7 | month = Feb | year = 2008 | doi = 10.1111/j.1346-8138.2008.00421.x | PMID = 18271804 }}</ref> | |||
*'''Not''' to be confused with ''[[desmoplastic fibroma]]''. | |||
===General=== | |||
*Benign lesion. | |||
Epidemiology: | |||
* | *May be on the lip. | ||
*Male:female ~= 5:1.<ref name=pmid15547225/> | |||
*Age - typically 40s & 50s.<ref name=pmid15547225/> | |||
===Gross=== | |||
* | *Classically found in the shoulder region. | ||
* | |||
* | DDx - shoulder region: | ||
*[[Desmoplastic fibroblastoma]]. | |||
*[[Elastofibroma]]. | |||
===Microscopic=== | |||
Features:<ref name=pmid9670823/><ref name=Ref_Sternberg4_161>{{Ref Sternberg4|161}}</ref> | |||
*Spindle cells ''or'' stellate cells without nuclear atypia. | |||
*Acellular stroma with abundant collagen - '''key feature'''. | |||
*+/-Myxoid areas. | |||
*+/-Rare mitoses. | |||
DDx:<ref name=pmid9670823/> | |||
*[[Fibromatosis]]. | |||
*[[Low-grade fibromyxoid sarcoma]]. | |||
Images: | Images: | ||
*[http:// | *[http://www.webpathology.com/image.asp?case=458&n=1 Desmoplastic fibroblastoma (webpathology.com)]. | ||
*[http:// | *[http://www.ajronline.org/content/183/6/1766/F3.expansion Desmoplastic fibroblastoma (ajronline.org)].<ref name=pmid15547225>{{Cite journal | last1 = Walker | first1 = KR. | last2 = Bui-Mansfield | first2 = LT. | last3 = Gering | first3 = SA. | last4 = Ranlett | first4 = RD. | title = Collagenous fibroma (desmoplastic fibroblastoma) of the shoulder. | journal = AJR Am J Roentgenol | volume = 183 | issue = 6 | pages = 1766 | month = Dec | year = 2004 | doi = | PMID = 15547225 }}</ref> | ||
===IHC=== | ===IHC=== | ||
Features:<ref name=pmid9670823>{{Cite journal | last1 = Miettinen | first1 = M. | last2 = Fetsch | first2 = JF. | title = Collagenous fibroma (desmoplastic fibroblastoma): a clinicopathologic analysis of 63 cases of a distinctive soft tissue lesion with stellate-shaped fibroblasts. | journal = Hum Pathol | volume = 29 | issue = 7 | pages = 676-82 | month = Jul | year = 1998 | doi = | PMID = 9670823 }}</ref> | |||
*Beta-catenin -ve.<ref name=pmid18544056>{{Cite journal | last1 = Takahara | first1 = M. | last2 = Ichikawa | first2 = R. | last3 = Oda | first3 = Y. | last4 = Uchi | first4 = H. | last5 = Takeuchi | first5 = S. | last6 = Moroi | first6 = Y. | last7 = Kiryu | first7 = H. | last8 = Furue | first8 = M. | title = Desmoplastic fibroblastoma: a case presenting as a protruding nodule in the dermis. | journal = J Cutan Pathol | volume = 35 Suppl 1 | issue = | pages = 70-3 | month = Oct | year = 2008 | doi = 10.1111/j.1600-0560.2007.00964.x | PMID = 18544056 }} | |||
</ref> | |||
**+ve in [[desmoid-type fibromatosis]]. | |||
*Desmin -ve. | |||
*S-100 -ve. | |||
*CD34 -ve. | *CD34 -ve. | ||
* | *MSA +ve (focal). | ||
*SMA | *alpha-SMA +ve (focal). | ||
===Molecular=== | ===Molecular=== | ||
* | *llq12 breakpoint described as being characteristic -- possibly the ''FOSL1 gene''.<ref name=pmid22411068>{{Cite journal | last1 = Macchia | first1 = G. | last2 = Trombetta | first2 = D. | last3 = Möller | first3 = E. | last4 = Mertens | first4 = F. | last5 = Storlazzi | first5 = CT. | last6 = Debiec-Rychter | first6 = M. | last7 = Sciot | first7 = R. | last8 = Nord | first8 = KH. | title = FOSL1 as a candidate target gene for 11q12 rearrangements in desmoplastic fibroblastoma. | journal = Lab Invest | volume = 92 | issue = 5 | pages = 735-43 | month = May | year = 2012 | doi = 10.1038/labinvest.2012.46 | PMID = 22411068 }}</ref> | ||
== | ==Calcifying fibrous tumour== | ||
===General=== | ===General=== | ||
*Rare. | |||
*Benign. | *Benign. | ||
===Microscopic=== | ===Microscopic=== | ||
Features:<ref name= | Features:<ref name=pmid16858502>{{cite journal |author=Attila T, Chen D, Gardiner GW, Ptak TW, Marcon NE |title=Gastric calcifying fibrous tumor |journal=Can. J. Gastroenterol. |volume=20 |issue=7 |pages=487–9 |year=2006 |month=July |pmid=16858502 |pmc=2659917 |doi= |url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659917/}}</ref> | ||
* | *Submucosal circumscribed fibrocollagenous nodule. | ||
* | *Psammomatous calcifications. | ||
*Focal plasma cells at the periphery. | |||
* | |||
==Myofibroma== | |||
{{Main|Myofibroma}} | |||
==Cellular angiofibroma== | |||
===General=== | |||
*[ | *Rare. | ||
*Benign. | |||
*Probably related to [[spindle cell lipoma]] and [[mammary-type myofibroblastoma]].<ref name=pmid20852591>{{Cite journal | last1 = Flucke | first1 = U. | last2 = van Krieken | first2 = JH. | last3 = Mentzel | first3 = T. | title = Cellular angiofibroma: analysis of 25 cases emphasizing its relationship to spindle cell lipoma and mammary-type myofibroblastoma. | journal = Mod Pathol | volume = 24 | issue = 1 | pages = 82-9 | month = Jan | year = 2011 | doi = 10.1038/modpathol.2010.170 | PMID = 20852591 }}</ref> | |||
*Predominantly female. | |||
===Gross=== | |||
Features:<ref name=pmid20852591/> | |||
*Superficial. | |||
*Well-circumscribed. | |||
Classic location: | |||
*Vulva.<ref name=pmid20852591/> | |||
===Microscopic=== | |||
Features:<ref name=pmid20852591/> | |||
*Spindle cell lesion. | |||
*Many small-to-medium blood vessls. | |||
===IHC=== | ===IHC=== | ||
Features:<ref name= | Features:<ref name=pmid20852591/> | ||
* | *CD34 ~50% of cases. | ||
*SMA | *SMA ~41% of cases. | ||
*CD99 -ve. | |||
*EMA -ve. | |||
== | =Occasionally metastasizing= | ||
* | ==Inflammatory myofibroblastic tumour== | ||
*[[AKA]] inflammatory pseudotumour, AKA inflammatory fibrosarcoma,<ref name=Ref_WMSP610>{{Ref WMSP|610}}</ref> AKA plasma cell granuloma.<ref>URL: [http://www.uptodate.com/contents/inflammatory-myofibroblastic-tumor-plasma-cell-granuloma-of-the-lung http://www.uptodate.com/contents/inflammatory-myofibroblastic-tumor-plasma-cell-granuloma-of-the-lung]. Accessed on: 27 November 2011.</ref><ref name=pmid21772725>{{Cite journal | last1 = Manohar | first1 = B. | last2 = Bhuvaneshwari | first2 = S. | title = Plasma cell granuloma of gingiva. | journal = J Indian Soc Periodontol | volume = 15 | issue = 1 | pages = 64-6 | month = Jan | year = 2011 | doi = 10.4103/0972-124X.82275 | PMID = 21772725 }}</ref> | |||
{{Main|Inflammatory myofibroblastic tumour}} | |||
== | ==Low-grade myofibroblastic sarcoma== | ||
===General=== | ===General=== | ||
* | *Rare ~ 100 cases in the literature. | ||
* | *Usu. oral cavity or extremities.<ref name=pmid21868549/> | ||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
* | *Spindle cells in the storiform pattern<ref name=pmid21868549/> ''or'' in fasicles. | ||
*Rare mitoses. | |||
Images: | Images: | ||
*[http:// | *[http://path.upmc.edu/cases/case673.html Low-grade myofibroblastic sarcoma - several images (upmc.edu)]. | ||
*[ | |||
*[ | DDx: | ||
*Atypical [[leiomyoma]]. | |||
*[[GIST]]. | |||
*[[Leiomyosarcoma]]. | |||
===IHC=== | ===IHC=== | ||
*CD34 | *SMA +ve. | ||
* | *CD34 -ve. | ||
* | *CD117 -ve.<ref name=pmid21868549/> | ||
*H-caldesmon -ve.<ref name=pmid21868549>{{Cite journal | last1 = Miyazawa | first1 = M. | last2 = Naritaka | first2 = Y. | last3 = Miyaki | first3 = A. | last4 = Asaka | first4 = S. | last5 = Isohata | first5 = N. | last6 = Yamaguchi | first6 = K. | last7 = Murayama | first7 = M. | last8 = Shimakawa | first8 = T. | last9 = Katsube | first9 = T. | title = A low-grade myofibroblastic sarcoma in the abdominal cavity. | journal = Anticancer Res | volume = 31 | issue = 9 | pages = 2989-94 | month = Sep | year = 2011 | doi = | PMID = }}</ref> | |||
==Congenital-infantile fibrosarcoma== | |||
:Should not be confused with ''[[adult fibrosarcoma]]''. | |||
===General=== | |||
*Locally aggressive. | |||
===Microscopic=== | |||
Features:<ref name=pmid7839472>{{Cite journal | last1 = Corsi | first1 = A. | last2 = Boldrini | first2 = R. | last3 = Bosman | first3 = C. | title = Congenital-infantile fibrosarcoma: study of two cases and review of the literature. | journal = Tumori | volume = 80 | issue = 5 | pages = 392-400 | month = Oct | year = 1994 | doi = | PMID = 7839472 }}</ref> | |||
*Spindle cell lesion. | |||
===Molecular=== | |||
Characteristic [[translocation]]:<ref name=pmid11242790 >{{Cite journal | last1 = Sheng | first1 = WQ. | last2 = Hisaoka | first2 = M. | last3 = Okamoto | first3 = S. | last4 = Tanaka | first4 = A. | last5 = Meis-Kindblom | first5 = JM. | last6 = Kindblom | first6 = LG. | last7 = Ishida | first7 = T. | last8 = Nojima | first8 = T. | last9 = Hashimoto | first9 = H. | title = Congenital-infantile fibrosarcoma. A clinicopathologic study of 10 cases and molecular detection of the ETV6-NTRK3 fusion transcripts using paraffin-embedded tissues. | journal = Am J Clin Pathol | volume = 115 | issue = 3 | pages = 348-55 | month = Mar | year = 2001 | doi = 10.1309/3H24-E7T7-V37G-AKKQ | PMID = 11242790 }}</ref> | |||
*t(12;15)(p13;q25). | |||
**Gene fusion ETV6-[[NTRK3]]. | |||
***Same translocation in [[mesoblastic nephroma]]. | |||
==Solitary fibrous tumour== | |||
{{Main|Solitary fibrous tumour}} | |||
==Hemangiopericytoma== | ==Hemangiopericytoma== | ||
===General=== | ===General=== | ||
*Grouped with ''solitary fibrous tumour'' in the WHO classification; | *Grouped with ''[[solitary fibrous tumour]]'' in the WHO classification; share same genetic NAB2-STAT6 fusion.<ref name=Ref_WMSP609>{{Ref WMSP|609}}</ref><ref>{{Cite journal | last1 = Schweizer | first1 = L. | last2 = Koelsche | first2 = C. | last3 = Sahm | first3 = F. | last4 = Piro | first4 = RM. | last5 = Capper | first5 = D. | last6 = Reuss | first6 = DE. | last7 = Pusch | first7 = S. | last8 = Habel | first8 = A. | last9 = Meyer | first9 = J. | title = Meningeal hemangiopericytoma and solitary fibrous tumors carry the NAB2-STAT6 fusion and can be diagnosed by nuclear expression of STAT6 protein. | journal = Acta Neuropathol | volume = 125 | issue = 5 | pages = 651-8 | month = May | year = 2013 | doi = 10.1007/s00401-013-1117-6 | PMID = 23575898 }}</ref> | ||
* | |||
*Thought to arise from the ''pericyte'', a connective tissue cell of small vessels that is thought to be involved in flow regulation while others consider a fibroblastic nature.<ref>{{Cite journal | last1 = Gengler | first1 = C. | last2 = Guillou | first2 = L. | title = Solitary fibrous tumour and haemangiopericytoma: evolution of a concept. | journal = Histopathology | volume = 48 | issue = 1 | pages = 63-74 | month = Jan | year = 2006 | doi = 10.1111/j.1365-2559.2005.02290.x | PMID = 16359538 }}</ref> | |||
*Hematologic spread most common - to lungs.<ref name=emed1255879ov>URL: [http://emedicine.medscape.com/article/1255879-overview http://emedicine.medscape.com/article/1255879-overview]. Accessed on: 2 May 2010.</ref> | *Hematologic spread most common - to lungs.<ref name=emed1255879ov>URL: [http://emedicine.medscape.com/article/1255879-overview http://emedicine.medscape.com/article/1255879-overview]. Accessed on: 2 May 2010.</ref> | ||
*Oncogenic osteomalacia - assoc. with hemangiopericytoma.<ref name=emed1255879ov>URL: [http://emedicine.medscape.com/article/1255879-overview http://emedicine.medscape.com/article/1255879-overview]. Accessed on: 2 May 2010.</ref> | *[[Oncogenic osteomalacia]] - assoc. with hemangiopericytoma.<ref name=emed1255879ov>URL: [http://emedicine.medscape.com/article/1255879-overview http://emedicine.medscape.com/article/1255879-overview]. Accessed on: 2 May 2010.</ref> | ||
*WHO grade II hemangiopericytoma (ICD-O: 9150/1), WHO grade III anaplastic hemangiopericytoma (ICD-O: 9150/3) | |||
====Presentation==== | ====Presentation==== | ||
*Usually painless mass, slow enlargement. | *Usually painless mass, slow enlargement. | ||
*May profusely bleed during resection. | |||
*May invade bone. | |||
====Histology==== | |||
*high cellular density. | |||
*indistinct cell borders. | |||
*random tumor cell orientation. | |||
*little fibrosis. | |||
*plenty reticulin. | |||
*vascular with slit-like channels ("staghorn-like vessels"). | |||
====IHC==== | |||
* Vimentin +ve. | |||
* CD34 +ve (often patchy, used to differentiate from SFT). | |||
* [[STAT6]] nuclear +ve. | |||
* EMA +/-ve. | |||
===Radiology=== | ===Radiology=== | ||
| Line 203: | Line 321: | ||
*Hypervascular lesion - '''key diagnostic feature'''.<ref name=enzinger>Enzinger & Weiss's Soft Tissue Tumors. 4th Ed. PP.1007-13. ISBN 0-323-01200-0.</ref> | *Hypervascular lesion - '''key diagnostic feature'''.<ref name=enzinger>Enzinger & Weiss's Soft Tissue Tumors. 4th Ed. PP.1007-13. ISBN 0-323-01200-0.</ref> | ||
**Abundant thin-walled branching small vessels of variable size. | **Abundant thin-walled branching small vessels of variable size. | ||
***May be described as "staghorn vessels" or "antler-like" vasculature. | ***May be described as "[[staghorn vessels]]" or "antler-like" vasculature. | ||
***Cells may "onion-skin" around thin blood vessels. | ***Cells may "onion-skin" around thin blood vessels. | ||
*Spindle or ovoid shaped cells in nests or sheets. | *Spindle or ovoid shaped cells in nests or sheets. | ||
DDx: | DDx: | ||
*Other vascular tumours. | *Other [[vascular tumours]]. | ||
*Vascular malformations. | *[[Vascular malformations]]. | ||
*[[Synovial sarcoma]]. | *[[Synovial sarcoma]]. | ||
*[[Dermatofibroma]]. (???) | *[[Dermatofibroma]]. (???) | ||
| Line 227: | Line 345: | ||
*S100 -ve. | *S100 -ve. | ||
== | ===Images=== | ||
<gallery> | |||
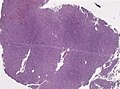
Image:Neuropathology_case_VI_02.jpg | Anaplastic hemangiopericytoma, low mag. (WC/jensflorian) | |||
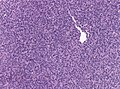
Image:Neuropathology_case_VI_03.jpg | Anaplastic hemangiopericytoma, intermed mag. (WC/jensflorian) | |||
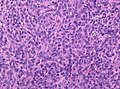
Image:Neuropathology_case_VI_04.jpg | Anaplastic hemangiopericytoma, high mag. (WC/jensflorian) | |||
Image:Neuropathology_case_VI_01.jpg | Anaplastic hemangiopericytoma, [[STAT6]] immunostaining. (WC/jensflorian) | |||
</gallery> | |||
</ | |||
=Malignant= | |||
==Low-grade fibromyxoid sarcoma== | ==Low-grade fibromyxoid sarcoma== | ||
*[[AKA]] ''hyalinizing spindle cell tumour''. | *[[AKA]] ''hyalinizing spindle cell tumour''. | ||
*Should '''not''' be confused with ''[[myxofibrosarcoma]]''. | |||
* | *Abbreviated ''LGFMS''. | ||
{{Main|Low-grade fibromyxoid sarcoma}} | |||
* | |||
==Adult fibrosarcoma== | ==Adult fibrosarcoma== | ||
| Line 289: | Line 372: | ||
Feature:<ref name=Ref_WMSP611>{{Ref WMSP|611}}</ref> | Feature:<ref name=Ref_WMSP611>{{Ref WMSP|611}}</ref> | ||
*Spindle cell lesion. | *Spindle cell lesion. | ||
*Herring bone pattern - '''key feature'''. | *[[Herring bone pattern]] - '''key feature'''. | ||
*Mitoses. | *Mitoses. | ||
| Line 298: | Line 381: | ||
DDx: | DDx: | ||
*[[ | *[[Dermatofibrosarcoma protuberans]] (DFSP) - t(17;22) COLA1/PDGFB. | ||
*Congenital-infantile fibrosarcoma - t(12;15) ETV6/NTRK3. | *[[Congenital-infantile fibrosarcoma]] - t(12;15) ETV6/NTRK3. | ||
*[[Solitary fibrous tumour]]. | *[[Solitary fibrous tumour]]. | ||
*[[Synovial sarcoma]] - t(X;18) SYT/SSX. | *[[Synovial sarcoma]] - t(X;18) SYT/SSX. | ||
| Line 312: | Line 395: | ||
*SMA. | *SMA. | ||
== | ==Myxofibrosarcoma== | ||
*Should '''not''' be confused with ''[[low-grade fibromyxoid sarcoma]]''.<ref name=pmid8650138>{{Cite journal | last1 = Mentzel | first1 = T. | last2 = Katenkamp | first2 = D. | last3 = Fletcher | first3 = CD. | title = [Low malignancy myxofibrosarcoma versus low malignancy fibromyxoid sarcoma. Distinct entities with similar names but different clinical course]. | journal = Pathologe | volume = 17 | issue = 2 | pages = 116-21 | month = Mar | year = 1996 | doi = | PMID = 8650138 }}</ref> | |||
*[[AKA]] ''myxoid malignant fibrous histiocytoma'' or ''myxoid MFH''.<ref>{{Cite journal | last1 = Fujimura | first1 = T. | last2 = Okuyama | first2 = R. | last3 = Terui | first3 = T. | last4 = Okuno | first4 = K. | last5 = Masu | first5 = A. | last6 = Masu | first6 = T. | last7 = Chiba | first7 = S. | last8 = Kunii | first8 = T. | last9 = Tagami | first9 = H. | title = Myxofibrosarcoma (myxoid malignant fibrous histiocytoma) showing cutaneous presentation: report of two cases. | journal = J Cutan Pathol | volume = 32 | issue = 7 | pages = 512-5 | month = Aug | year = 2005 | doi = 10.1111/j.0303-6987.2005.00368.x | PMID = 16008697 }}</ref> | |||
{{Main|Myxofibrosarcoma}} | |||
* | |||
=See also= | |||
*[[Soft tissue lesions]]. | *[[Soft tissue lesions]]. | ||
=References= | |||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Soft tissue lesions]] | [[Category:Soft tissue lesions]] | ||
Latest revision as of 18:58, 24 March 2019
This article covers fibroblastic/myofibroblastic tumours. These tumours fit into the larger category of soft tissue lesions.
List of tumours
Benign
WHO classification:[1]
- Nodular fasciitis.
- Proliferative fasciitis.
- Proliferative myositis.
- Myositis ossificans.
- Ischemic fasciitis.
- Elastofibroma.
- Myofibroma.
- Fibromatosis colli.
- Inclusion body fibromatosis.
- Fibroma of tendon sheath.
- Calcifying aponeurotic fibroma.
- Angiomyofibroblastoma.
- Cellular angiofibroma.
- Nuchal-type fibroma.
- Gardner fibroma.
- Calcifying fibrous tumour.
- Giant cell angiofibroma.
- Fibrous hamartoma of infancy.
- Juvenile hyaline fibromatosis.
- Desmoplastic fibroblastoma.
- Mammary-type myofibroblastoma.
Locally aggressive
WHO classification:[1]
- Superfical fibromatosis.
- Desmoid-type fibromatosis.
- Lipofibromatosis.
Occasionally metastasizing
WHO classification:[2]
- Solitary fibrous tumour.
- Inflammatory myofibroblastic tumour.
- Low-grade myofibroblastic sarcoma.
- Myxoinflammatory fibroblastic sarcoma.
- Infantile fibrosarcoma.
Malignant
WHO classification:[2]
- Adult fibrosarcoma.
- Myxofibrosarcoma.
- Low-grade fibromyxoid sarcoma (hyalinizing spindle cell tumour).
- Sclerosing epithelioid fibrosarcoma.
Non-malignant
Proliferative fasciitis
General
- Benign.
- May mimic a sarcoma.[3]
Clinical:
- Solid subcutaneous nodule.
- Rapid growth.
- May be painful.
Gross
- Classically upper and lower extremities.[3]
- Poorly demarcated.
Microscopic
Features:[4]
- Large polygonal (ganglion-like) and/or spindled cells with:
- Vesicular (clear) nuclei.
- Prominent nucleoli.
- +/-Binucleation.
- Loose myxoid stroma.
- Frequent typical mitoses.
- No atypical mitoses.
DDx:
Images:
- Proliferative fasciitis - several images (virginia.edu).
- Proliferative fasciitis (surgicalpathologyatlas.com).
Proliferative myositis
General
- Benign.
- Possible arise from pericytes.[6]
Microscopic
- Large ganglion-like cells.
- Cells have single prominent nucleolus.
- Spindle cells.
- +/-Binucleation.
- Mitotic activity.
- No atypical mitoses.
Image:
IHC
Features:[6]
- Vimentin +ve.
- SMA +ve.
- Desmin +ve/-ve.
Others:[6]
- Factor XIIIa -ve.
- S100 -ve.
- CAM5.2 -ve.
- NSE -ve.
Elastofibroma
Nodular fasciitis
Desmoid-type fibromatosis
Lipofibromatosis
- AKA infantile subcutaneous fibromatosis.
General
- Childhood.
Microscopic
Features:[8]
- Fibroblastic cells surrounding adipocytes.
Image:
IHC
Features:[8]
- CD34 +ve.
- BCL2 +ve.
- S100 +ve.
- CD99 +ve.
- Actin +ve.
- EMA +ve.
Desmoplastic fibroblastoma
- AKA collagenous fibroma.[9]
- Not to be confused with desmoplastic fibroma.
General
- Benign lesion.
Epidemiology:
Gross
- Classically found in the shoulder region.
DDx - shoulder region:
Microscopic
- Spindle cells or stellate cells without nuclear atypia.
- Acellular stroma with abundant collagen - key feature.
- +/-Myxoid areas.
- +/-Rare mitoses.
DDx:[11]
Images:
IHC
Features:[11]
- Beta-catenin -ve.[13]
- +ve in desmoid-type fibromatosis.
- Desmin -ve.
- S-100 -ve.
- CD34 -ve.
- MSA +ve (focal).
- alpha-SMA +ve (focal).
Molecular
- llq12 breakpoint described as being characteristic -- possibly the FOSL1 gene.[14]
Calcifying fibrous tumour
General
- Rare.
- Benign.
Microscopic
Features:[15]
- Submucosal circumscribed fibrocollagenous nodule.
- Psammomatous calcifications.
- Focal plasma cells at the periphery.
Myofibroma
Cellular angiofibroma
General
- Rare.
- Benign.
- Probably related to spindle cell lipoma and mammary-type myofibroblastoma.[16]
- Predominantly female.
Gross
Features:[16]
- Superficial.
- Well-circumscribed.
Classic location:
- Vulva.[16]
Microscopic
Features:[16]
- Spindle cell lesion.
- Many small-to-medium blood vessls.
IHC
Features:[16]
- CD34 ~50% of cases.
- SMA ~41% of cases.
- CD99 -ve.
- EMA -ve.
Occasionally metastasizing
Inflammatory myofibroblastic tumour
- AKA inflammatory pseudotumour, AKA inflammatory fibrosarcoma,[17] AKA plasma cell granuloma.[18][19]
Low-grade myofibroblastic sarcoma
General
- Rare ~ 100 cases in the literature.
- Usu. oral cavity or extremities.[20]
Microscopic
Features:
- Spindle cells in the storiform pattern[20] or in fasicles.
- Rare mitoses.
Images:
DDx:
- Atypical leiomyoma.
- GIST.
- Leiomyosarcoma.
IHC
Congenital-infantile fibrosarcoma
- Should not be confused with adult fibrosarcoma.
General
- Locally aggressive.
Microscopic
Features:[21]
- Spindle cell lesion.
Molecular
Characteristic translocation:[22]
- t(12;15)(p13;q25).
- Gene fusion ETV6-NTRK3.
- Same translocation in mesoblastic nephroma.
- Gene fusion ETV6-NTRK3.
Solitary fibrous tumour
Hemangiopericytoma
General
- Grouped with solitary fibrous tumour in the WHO classification; share same genetic NAB2-STAT6 fusion.[8][23]
- Thought to arise from the pericyte, a connective tissue cell of small vessels that is thought to be involved in flow regulation while others consider a fibroblastic nature.[24]
- Hematologic spread most common - to lungs.[25]
- Oncogenic osteomalacia - assoc. with hemangiopericytoma.[25]
- WHO grade II hemangiopericytoma (ICD-O: 9150/1), WHO grade III anaplastic hemangiopericytoma (ICD-O: 9150/3)
Presentation
- Usually painless mass, slow enlargement.
- May profusely bleed during resection.
- May invade bone.
Histology
- high cellular density.
- indistinct cell borders.
- random tumor cell orientation.
- little fibrosis.
- plenty reticulin.
- vascular with slit-like channels ("staghorn-like vessels").
IHC
- Vimentin +ve.
- CD34 +ve (often patchy, used to differentiate from SFT).
- STAT6 nuclear +ve.
- EMA +/-ve.
Radiology
- Intramedullary lytic mass.
- May be well-circumscribed.
- +/-Periosteal reaction.
- +/-Sclerotic border.
May be worked-up with angiography to distinguish from a vascular malformation.[26]
Location
- Usually extremities - femur or proximal tibial.[25]
Microscopic
Features:[26]
- Hypervascular lesion - key diagnostic feature.[27]
- Abundant thin-walled branching small vessels of variable size.
- May be described as "staghorn vessels" or "antler-like" vasculature.
- Cells may "onion-skin" around thin blood vessels.
- Abundant thin-walled branching small vessels of variable size.
- Spindle or ovoid shaped cells in nests or sheets.
DDx:
- Other vascular tumours.
- Vascular malformations.
- Synovial sarcoma.
- Dermatofibroma. (???)
IHC
- Vimentin +ve (usually).
- Desmin -ve (typical).
- Factor VIII -ve (marks endothelium).
- CD34 +ve.
- CD34 usu. -ve in synovial sarcoma.
- CD31 -ve (marks benign endothelium).
- vWF (von Willebrand factor) -ve.
May be in the DDx for meningioma:[28]
- EMA -ve.
- S100 -ve.
Images
Anaplastic hemangiopericytoma, STAT6 immunostaining. (WC/jensflorian)
Malignant
Low-grade fibromyxoid sarcoma
- AKA hyalinizing spindle cell tumour.
- Should not be confused with myxofibrosarcoma.
- Abbreviated LGFMS.
Adult fibrosarcoma
- AKA fibrosarcoma.
- Should not be confused with infantile fibrosarcoma.
General
- Malignant.
- Older adults.
- Locations: head & neck, extremities.
Microscopic
Feature:[29]
- Spindle cell lesion.
- Herring bone pattern - key feature.
- Mitoses.
DDx (herring bone):
- MPNST.
- Synovial sarcoma.
- Fibrosarcoma.
DDx:
- Dermatofibrosarcoma protuberans (DFSP) - t(17;22) COLA1/PDGFB.
- Congenital-infantile fibrosarcoma - t(12;15) ETV6/NTRK3.
- Solitary fibrous tumour.
- Synovial sarcoma - t(X;18) SYT/SSX.
- MPNST.
Images:
IHC
Features:[29]
- Vimentin.
- SMA.
Myxofibrosarcoma
- Should not be confused with low-grade fibromyxoid sarcoma.[30]
- AKA myxoid malignant fibrous histiocytoma or myxoid MFH.[31]
See also
References
- ↑ 1.0 1.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 601. ISBN 978-0781765275.
- ↑ 2.0 2.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 602. ISBN 978-0781765275.
- ↑ 3.0 3.1 Chung, EB.; Enzinger, FM. (Oct 1975). "Proliferative fasciitis.". Cancer 36 (4): 1450-8. PMID 1058047.
- ↑ Meis, JM.; Enzinger, FM. (Apr 1992). "Proliferative fasciitis and myositis of childhood.". Am J Surg Pathol 16 (4): 364-72. PMID 1566969.
- ↑ Gleason, BC.; Hornick, JL. (Apr 2008). "Inflammatory myofibroblastic tumours: where are we now?". J Clin Pathol 61 (4): 428-37. doi:10.1136/jcp.2007.049387. PMID 17938159.
- ↑ 6.0 6.1 6.2 6.3 el-Jabbour, JN.; Bennett, MH.; Burke, MM.; Lessells, A.; O'Halloran, A. (Jul 1991). "Proliferative myositis. An immunohistochemical and ultrastructural study.". Am J Surg Pathol 15 (7): 654-9. PMID 2058761.
- ↑ Lundgren, L.; Kindblom, LG.; Willems, J.; Falkmer, U.; Angervall, L. (May 1992). "Proliferative myositis and fasciitis. A light and electron microscopic, cytologic, DNA-cytometric and immunohistochemical study.". APMIS 100 (5): 437-48. PMID 1586481.
- ↑ 8.0 8.1 8.2 8.3 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 609. ISBN 978-0781765275.
- ↑ Watanabe, H.; Ishida, Y.; Nagashima, K.; Makino, T.; Norisugi, O.; Shimizu, T. (Feb 2008). "Desmoplastic fibroblastoma (collagenous fibroma).". J Dermatol 35 (2): 93-7. doi:10.1111/j.1346-8138.2008.00421.x. PMID 18271804.
- ↑ 10.0 10.1 10.2 Walker, KR.; Bui-Mansfield, LT.; Gering, SA.; Ranlett, RD. (Dec 2004). "Collagenous fibroma (desmoplastic fibroblastoma) of the shoulder.". AJR Am J Roentgenol 183 (6): 1766. PMID 15547225.
- ↑ 11.0 11.1 11.2 Miettinen, M.; Fetsch, JF. (Jul 1998). "Collagenous fibroma (desmoplastic fibroblastoma): a clinicopathologic analysis of 63 cases of a distinctive soft tissue lesion with stellate-shaped fibroblasts.". Hum Pathol 29 (7): 676-82. PMID 9670823.
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 161. ISBN 978-0781740517.
- ↑ Takahara, M.; Ichikawa, R.; Oda, Y.; Uchi, H.; Takeuchi, S.; Moroi, Y.; Kiryu, H.; Furue, M. (Oct 2008). "Desmoplastic fibroblastoma: a case presenting as a protruding nodule in the dermis.". J Cutan Pathol 35 Suppl 1: 70-3. doi:10.1111/j.1600-0560.2007.00964.x. PMID 18544056.
- ↑ Macchia, G.; Trombetta, D.; Möller, E.; Mertens, F.; Storlazzi, CT.; Debiec-Rychter, M.; Sciot, R.; Nord, KH. (May 2012). "FOSL1 as a candidate target gene for 11q12 rearrangements in desmoplastic fibroblastoma.". Lab Invest 92 (5): 735-43. doi:10.1038/labinvest.2012.46. PMID 22411068.
- ↑ Attila T, Chen D, Gardiner GW, Ptak TW, Marcon NE (July 2006). "Gastric calcifying fibrous tumor". Can. J. Gastroenterol. 20 (7): 487–9. PMC 2659917. PMID 16858502. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659917/.
- ↑ 16.0 16.1 16.2 16.3 16.4 Flucke, U.; van Krieken, JH.; Mentzel, T. (Jan 2011). "Cellular angiofibroma: analysis of 25 cases emphasizing its relationship to spindle cell lipoma and mammary-type myofibroblastoma.". Mod Pathol 24 (1): 82-9. doi:10.1038/modpathol.2010.170. PMID 20852591.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 610. ISBN 978-0781765275.
- ↑ URL: http://www.uptodate.com/contents/inflammatory-myofibroblastic-tumor-plasma-cell-granuloma-of-the-lung. Accessed on: 27 November 2011.
- ↑ Manohar, B.; Bhuvaneshwari, S. (Jan 2011). "Plasma cell granuloma of gingiva.". J Indian Soc Periodontol 15 (1): 64-6. doi:10.4103/0972-124X.82275. PMID 21772725.
- ↑ 20.0 20.1 20.2 20.3 Miyazawa, M.; Naritaka, Y.; Miyaki, A.; Asaka, S.; Isohata, N.; Yamaguchi, K.; Murayama, M.; Shimakawa, T. et al. (Sep 2011). "A low-grade myofibroblastic sarcoma in the abdominal cavity.". Anticancer Res 31 (9): 2989-94.
- ↑ Corsi, A.; Boldrini, R.; Bosman, C. (Oct 1994). "Congenital-infantile fibrosarcoma: study of two cases and review of the literature.". Tumori 80 (5): 392-400. PMID 7839472.
- ↑ Sheng, WQ.; Hisaoka, M.; Okamoto, S.; Tanaka, A.; Meis-Kindblom, JM.; Kindblom, LG.; Ishida, T.; Nojima, T. et al. (Mar 2001). "Congenital-infantile fibrosarcoma. A clinicopathologic study of 10 cases and molecular detection of the ETV6-NTRK3 fusion transcripts using paraffin-embedded tissues.". Am J Clin Pathol 115 (3): 348-55. doi:10.1309/3H24-E7T7-V37G-AKKQ. PMID 11242790.
- ↑ Schweizer, L.; Koelsche, C.; Sahm, F.; Piro, RM.; Capper, D.; Reuss, DE.; Pusch, S.; Habel, A. et al. (May 2013). "Meningeal hemangiopericytoma and solitary fibrous tumors carry the NAB2-STAT6 fusion and can be diagnosed by nuclear expression of STAT6 protein.". Acta Neuropathol 125 (5): 651-8. doi:10.1007/s00401-013-1117-6. PMID 23575898.
- ↑ Gengler, C.; Guillou, L. (Jan 2006). "Solitary fibrous tumour and haemangiopericytoma: evolution of a concept.". Histopathology 48 (1): 63-74. doi:10.1111/j.1365-2559.2005.02290.x. PMID 16359538.
- ↑ 25.0 25.1 25.2 URL: http://emedicine.medscape.com/article/1255879-overview. Accessed on: 2 May 2010.
- ↑ 26.0 26.1 URL: http://emedicine.medscape.com/article/1255879-diagnosis. Accessed on: 2 May 2010.
- ↑ 27.0 27.1 Enzinger & Weiss's Soft Tissue Tumors. 4th Ed. PP.1007-13. ISBN 0-323-01200-0.
- ↑ Croul, SE. 8 November 2010.
- ↑ 29.0 29.1 Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 611. ISBN 978-0781765275.
- ↑ Mentzel, T.; Katenkamp, D.; Fletcher, CD. (Mar 1996). "[Low malignancy myxofibrosarcoma versus low malignancy fibromyxoid sarcoma. Distinct entities with similar names but different clinical course].". Pathologe 17 (2): 116-21. PMID 8650138.
- ↑ Fujimura, T.; Okuyama, R.; Terui, T.; Okuno, K.; Masu, A.; Masu, T.; Chiba, S.; Kunii, T. et al. (Aug 2005). "Myxofibrosarcoma (myxoid malignant fibrous histiocytoma) showing cutaneous presentation: report of two cases.". J Cutan Pathol 32 (7): 512-5. doi:10.1111/j.0303-6987.2005.00368.x. PMID 16008697.