Difference between revisions of "Head and neck cytopathology"
Jump to navigation
Jump to search
(→Normal) |
(+image) |
||
| (9 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
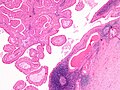
[[Image:Pleomorphic adenoma - cytology -- high mag.jpg|right|thumb|[[Micrograph]] showing a pleomorphic adenoma. [[Pap stain]].]] | |||
'''Head and neck cytopathology''' is a small part of cytopathology. Non-cytopathology head & neck pathology is dealt with in the ''[[head and neck pathology]]'' article. | '''Head and neck cytopathology''' is a small part of cytopathology. Non-cytopathology head & neck pathology is dealt with in the ''[[head and neck pathology]]'' article. | ||
| Line 6: | Line 7: | ||
=Proposed Milan system for reporting salivary gland cytopathology= | =Proposed Milan system for reporting salivary gland cytopathology= | ||
:''Milan system'' | :''Milan system'' and ''Milan classification'' redirect here. | ||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 21: | Line 22: | ||
| | | | ||
|- | |- | ||
| | | Atypia of undetermined significance (AUS) | ||
| repeat FNA | | repeat FNA | ||
| use should be minimized <br>- like [[FLUS]] and [[ASCUS]] | | use should be minimized <br>- like [[FLUS]] and [[ASCUS]] | ||
| Line 27: | Line 28: | ||
| Neoplasm | | Neoplasm | ||
| excision | | excision | ||
| subdivided into: (a) benign (b) | | subdivided into: (a) benign (b) salivary gland neoplasm of uncertain malignant potential (SUMP) | ||
|- | |- | ||
| Suspicious for malignancy | | Suspicious for malignancy | ||
| Line 57: | Line 58: | ||
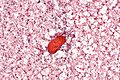
[[Skeletal muscle]]: | [[Skeletal muscle]]: | ||
*Round red staining globs +/-apparent striations | *Round red staining globs +/-apparent striations. | ||
*Nuclei more at edges (peripheral). | |||
===Images=== | ===Images=== | ||
| Line 152: | Line 154: | ||
*Squamous carcinoma. | *Squamous carcinoma. | ||
*Mucoepidermoid carcinoma. | *Mucoepidermoid carcinoma. | ||
==Crystals in salivary gland specimens== | |||
===General=== | |||
*Uncommon in general. | |||
**Typical location is: parotid (>85% salivary gland specimens with crystals<ref name=pmid33296146>{{cite journal |authors=Sun T, Faquin WC, Torous VF |title=Crystalloids in FNA specimens of salivary gland lesions: A retrospective study in a single large institute |journal=Cancer Cytopathol |volume=129 |issue=6 |pages=432–438 |date=June 2021 |pmid=33296146 |doi=10.1002/cncy.22395 |url=}}</ref>). | |||
*May be seen in the context of any diagnostic category (non-diagnostic, benign, neoplastic, malignant). | |||
**Approximately 40% of cases with crystals are benign or non-diagnositic.<ref name=pmid33296146/> | |||
**Approximately 10% of cases with crystals are suspicious or malignant.<ref name=pmid33296146/> | |||
DDx: | |||
*Amylase crystalloids ~ 75%. | |||
*Tyrosine crystalloids ~ 11%. | |||
*Collagenous crystalloids ~ 3%. | |||
*Undetermined type ~ 11%. | |||
===Cytology=== | |||
Features:<ref name=pmid33296146/><ref>{{cite journal |authors=Kishore M, Kaushal M, Dogra S |title=Crystalloids in salivary gland lesion: A diagnostic clue |journal=J Lab Physicians |volume=11 |issue=1 |pages=100–101 |date=2019 |pmid=30983813 |pmc=6437830 |doi=10.4103/JLP.JLP_120_18 |url=}}</ref> | |||
*Amylase crystalloids: rhomboid (or polygonal) +/- "pointy" ends, nonbirefringent. | |||
*Tyrosine crystalloids: floret-like structures, refractile. | |||
*Collagenous crystalloids: needle-shaped, radially arranged. | |||
====Images==== | |||
<gallery> | |||
Image: Amylase crystals - parotid -- intermed mag.jpg | Amylase crystals - parotid - intermed. mag. | |||
Image: Amylase crystals - parotid - alt -- intermed mag.jpg | Amylase crystals - parotid - intermed. mag. | |||
Image: Amylase crystals - parotid -- high mag.jpg | Amylase crystals - parotid - high mag. | |||
Image: Amylase crystals - parotid - alt -- high mag.jpg | Amylase crystals - parotid - high mag. | |||
Image: Amylase crystals - parotid -- very high mag.jpg | Amylase crystals - parotid - very high mag. | |||
Image: Amylase crystals - parotid - alt -- very high mag.jpg | Amylase crystals - parotid - very high mag. | |||
Image: Amylase crystals - parotid - alt2 -- very high mag.jpg | Amylase crystals - parotid - very high mag. | |||
Image: Amylase crystals - parotid -- high mag.gif | Amylase crystals - parotid - animation - high mag. | |||
Image: Amylase crystals - parotid -- very high mag.gif | Amylase crystals - parotid - animation - very high mag. | |||
</gallery> | |||
===Sign out=== | |||
<pre> | |||
Crystalloid material is present and has a rhomboid/polygonal shape with occasional "pointy" ends; this is in keeping with amylase crystals. | |||
</pre> | |||
==Pleomorphic adenoma== | ==Pleomorphic adenoma== | ||
Latest revision as of 16:09, 4 November 2024
Head and neck cytopathology is a small part of cytopathology. Non-cytopathology head & neck pathology is dealt with in the head and neck pathology article.
Thyroid cytopathology is dealt with in the thyroid cytopathology article. An introduction to cytopathology is in the cytopathology article.
Salivary gland cytopathology and salivary gland cytology redirect to here.
Proposed Milan system for reporting salivary gland cytopathology
- Milan system and Milan classification redirect here.
| Category | Typical management | Comments |
|---|---|---|
| Nondiagnostic | repeat FNA | |
| Nonneoplastic | follow-up/discharge | |
| Atypia of undetermined significance (AUS) | repeat FNA | use should be minimized - like FLUS and ASCUS |
| Neoplasm | excision | subdivided into: (a) benign (b) salivary gland neoplasm of uncertain malignant potential (SUMP) |
| Suspicious for malignancy | wide excision +/-lymph nodes (?) | |
| Malignant | wide excision & lymph nodes (?) |
Notes:
- This classification is still evolving.[1] The preliminary version (above) was presented by Dr. William Faquin at USCAP 2016 in Seattle.[2]
- The goal is to complete the reporting system by the summer of 2017.
Normal
Depends on the structure that is needled.
Parotid:[3]
- Acini - small globoid clusters.
- Separated by adipose tissue.
- Granular cytoplasm.
- Nucleus:
- Dispersed chromatin.
- Indistinct nucleolus.
- Low NC ratio cells.
Sticky lymphoid tissue:
- Irregular globs of tissue with small cells.
- Round red staining globs +/-apparent striations.
- Nuclei more at edges (peripheral).
Images
Salivary gland tumours - summary
Benign
| Diagnosis | Architecture | Cytoplasm | Nucleus | Main DDx | Used to diff. from main DDx | Image |
|---|---|---|---|---|---|---|
| Pleomorphic adenoma | Fluffy fibromyxoid material & cells and single (plasmacytoid-like) myoepithelial cells | ? | Myoepithelial cells - plasmacytoid appearance | DDx (?) | ? | |
| Warthin tumour (papillary cystadenoma lymphomatosum) | Sheets of uniformly spaced oncocytes, lymphocytes, necrotic debris | Oncocytes (abundant, granular, eosinophilic tinge), well-defined cell borders | Oncocytes have nucleolus | Acinic cell carcinoma (AcCC), oncocytoma | AcCC: irregular spaced cells, lack well-defined cell borders |
Malignant
| Diagnosis | Architecture | Cytoplasm | Nucleus | Main DDx | Used to diff. from main DDx | Image |
|---|---|---|---|---|---|---|
| Mucoepidermoid carcinoma | Clumps of cells | Abundant whispy cytoplasm | Small oval nucleus, +/-distinct nucleolus | Mucocele ? | Nuclear atypia | |
| Adenoid cystic carcinoma (AdCC) | Circular islands of abundant very small cells | Scant cytoplasm | Small nucleus - may have carrot shape | AcCC | Basement membrane material - PAS-D+ve[4] | |
| Acinic cell carcinoma (AcCC) | 3-D clusters of small cells | Abundant orangeophilic granular cytoplasm | Stippled chromatin | Warthin tumour | AcCC missing lymphocytic background; irreg. spacing of cells |
Salivary gland
Main article: Salivary gland
Sialoadenitis
Main article: Chronic sialadenitis
Cytology
Features:
- Inflammatory cells - lymphocytes, plasma cells - key features.
- +/-Squamous metaplasia.
- +/-Necrotic debris.
- Benign ductal epithelium.
DDx:
- Squamous carcinoma.
- Mucoepidermoid carcinoma.
Crystals in salivary gland specimens
General
- Uncommon in general.
- Typical location is: parotid (>85% salivary gland specimens with crystals[5]).
- May be seen in the context of any diagnostic category (non-diagnostic, benign, neoplastic, malignant).
DDx:
- Amylase crystalloids ~ 75%.
- Tyrosine crystalloids ~ 11%.
- Collagenous crystalloids ~ 3%.
- Undetermined type ~ 11%.
Cytology
- Amylase crystalloids: rhomboid (or polygonal) +/- "pointy" ends, nonbirefringent.
- Tyrosine crystalloids: floret-like structures, refractile.
- Collagenous crystalloids: needle-shaped, radially arranged.
Images
Sign out
Crystalloid material is present and has a rhomboid/polygonal shape with occasional "pointy" ends; this is in keeping with amylase crystals.
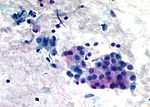
Pleomorphic adenoma
Main article: Pleomorphic adenoma
- Abbreviated PA.
General
- Common benign tumour.
Cytology
- Myoepithelial cells.
- Plasmacytoid-like cells.
- Single cells (very common) or small clumps - oval shape.
- Plasmacytoid-like cells.
- Epithelial cells.
- Chondromyxoid stroma.
- Whispy/fluffy groups of spindle cells that overlap (fibromyxoid tissue) - blue-ish.
DDx:
- Adenoid cystic carcinoma.
- Big circular globs (cysts) - common in AdCC.
Images
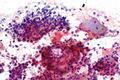
Warthin tumour
- AKA papillary cystadenoma lymphomatosum.
General
- Usual smokers.
- May be bilateral.
Cytology
Features:[9]
- Oncocytes.
- Well-defined cell border.
- Granular cytoplasm.
- Nucleoli.
- Oncocytes are often associated with mast cells, i.e. on "top of" oncocytes.
- Mast cells: very granular dark staining cytoplasm (on smears).
- Lymphocytes.
- Necrotic material (cyst contents).
DDx:
- Acinic cell carcinoma.
- Spacing of tumour in AcCC is more irregular and appear more crowded.
- The cell borders in AcCC is less obvious.
- Oncocytoma.
- Oncocytoma (vis-a-vis Warthin tumour) has more cells, more cytoplasm, more granularity of cytoplasm, more complex architecture.[3]
Images
Oncocytoma
Main article: Oncocytoma of the salivary gland
General
- May be confused with Warthin tumour.
Cytology
Features:
- Oncocytes.
- Well-defined cell border.
- Granular cytoplasm.
- Nucleoli.
Vis-a-vis Warthin tumour:
- Oncocytoma has:[3]
- More cells,
- More cytoplasm,
- More granularity of cytoplasm,
- More complex architecture.
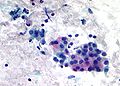
Mucoepidermoid carcinoma
Main article: Mucoepidermoid carcinoma
General
- A challenging FNA diagnosis.[10]
Cytology
Features:
- Sheets of cells.
- Cells have a small oval nucleus with nucleolus.
- Fluffy cytoplasm with a pink tinge (on Pap stain) - key feature.
- Cytoplasm not seen in 3-D clusters - look for single layer of cells.
- Cell borders are often distinct.
DDx:
- Squamous cell carcinoma - extensive keratinization and squamous pearls.[11]
Images
Acinic cell carcinoma
Main article: Acinic cell carcinoma
General
- Uncommon.
Cytology
Features:[12]
- Abundant granular cytoplasm.
- Stippled chromatin.
- +/-Nucleolus.
Notes:
- Often accompanied by stripped nuclei; may mimic lymphocytes (may lead to confusion with Warthin tumour).
- Lack:[3]
- Adipocytes between acini (differentiates from normal).
- Ductal structures (differentiates from normal).
Memory device:
- AcCC - lots of "C"s: lots of cytoplasm, carcinoid-like (stippled chromatin, granular cytoplasm).
Image
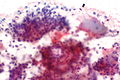
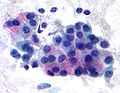
Adenoid cystic carcinoma
General
- Usu. distinctive.
- May be painful due the presence of perineural invasion.
Cytology
Features:
- Solid circular islands that are well-circumscribed.
- Classically forms cystic structures.
- Very cellular.
- Small cells - key feature.
- Nucleus - large relative to cell (high NC ratio)
- Often oval/triangular - may be carrot-shaped.
- +/-Nucleolus. (???)
- Chromatin NOT stippled.
- Scant cytoplasm - key feature.
Notes:
- Memory device: AdCC = lotsa DNA in relation to cell.
Image
Epithelial-myoepithelial carcinoma
Main article: Epithelial-myoepithelial carcinoma
Cytology
Features:
- Single cells/stripped nuclei.
- 3-dimensional clusters.
- Two cell population:
- Dark small cells.
- Light large cells.
Common
Squamous carcinoma
Main article: Squamous cell carcinoma
- AKA squamous cell carcinoma.
Cytopathology
Features:
- Mix of spindle cells/epithelioid cells, present in clusters, +/-small number of single cells.
- Keratinization:
- Orange/red staining on Pap stain.
- Poorly differentiated SCC = not orange/red.
- "Intense" (blue) staining of cells on rapid Romanowsky + pyknotic (small shriveled) nucleus.[13]
- Orange/red staining on Pap stain.
- "Dense" appearing cytoplasm.
- +/-Laminae (layers)/lines in the cytoplasm.
- Nuclear features of malignancy (required for diagnosis):
- Irregular nuclear membrane, e.g. notches, sharp discontinuities.
- Nuclear hyperchromasia - "jet-black" nuclei on Pap stain key feature.
- Increased NC ratio.
- Variation of nuclear size from cell-to-cell.
- Granular chromatin.
Notes:
- One should see abnormal squamous cells to call it SCC.
- Poorly differentiated SCC may look like adenocarcinoma.
Melanoma
Main article: Malignant melanoma
Features:
- Usually mixed population of:
- Spindle cells.
- Often single/detacted cells.
- Epithelioid cells - usually predominant.
- Nucleus typically eccentric.
- Spindle cells.
- Brown granular cytoplasm; usually fine granularity.
- Large red nucleoli (classic finding).
- +/-Intranuclear inclusions.
- +/-Binucleation.
Minimal (for morphologic diagnosis):
- Nuclear features of malignancy in epithelioid cells (with an eccentric nucleus) or spindle cells.
- Brown granular cytoplasm.
Notes:
- IHC stains are needed in many cases (S-100, HMB-45, Melan A).
- The classic appearance of melanoma without pigment is closest to adenocarcinoma (which may have red nucleoli, large cells, abundant cytoplasm, occasional binucleation).
- Differentiating morphologic features: adenocarcinoma - 3-D clusters of cells, no spindle-shaped cells.
Lymph nodes
Normal lymph node
Cytology
- Mixed population of lymphoid cells.
- +/-Lymphoglandular bodies.
Image
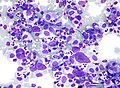
Non-Hodgkin's lymphoma
Cytology
Features:
- Population of monomorphous lymphoid cells - usu. ~2x the size of a RBC.
- Lymphoglandular bodies - blue-grey bodies.
- Often about 1/2 the size of a RBC.
- These may be seen in benign tissue.
- Often about 1/2 the size of a RBC.
Note:
- Small cell lymphomas cannot be diagnosed definitively from cytology.
Image
Hodgkin's lymphoma
Main article: Hodgkin lymphoma
Cytology
Features:
- Reed-Sternberg cell (diagnostic).
- Classically binucleated.
- Huge cell with macronucleus.
- Each nucleus has a huge macronucleolus.
- Macronucleolus approximately the size of a RBC.
- Commonly seen with eosinophils.
Note:
- RSCs are usually found at the edge of smears.[15]
Images
www:
Cystic lesions of the neck
General
- One should never sign-out a cytology specimen as: "branchial cleft cyst" or "thyroglossal duct cyst".
- The proper verbiage is "cystic squamous lesion".
DDx
Lateral:
Medial:
Both:
- Epidermoid cyst.
- Cystic squamous cell carcinoma.
See also
References
- ↑ URL: http://www.cytopathology.org/the-milan-system-for-reporting-salivary-gland-cytopathology/. Accessed on: 31 March 2016.
- ↑ URL: http://www.uscap.org/meetings/detail/2016-annual-meeting/sessions/2334. Accessed on: 13 March 2016.
- ↑ 3.0 3.1 3.2 3.3 Boerner SL. Patterns and pitfalls in fine needle aspiration of salivary gland. Current Diagnostic Pathology. 9:339-354. 2003. URL (abstract only): http://www.journals.elsevierhealth.com/periodicals/ycdip/article/PIIS0968605303000711/abstract.
- ↑ Chen SY (November 1976). "Adenoid cystic carcinoma of minor salivary gland. Histochemical and electron microscopic studies of cystlike space". Oral Surg. Oral Med. Oral Pathol. 42 (5): 606–19. PMID 62333.
- ↑ 5.0 5.1 5.2 5.3 Sun T, Faquin WC, Torous VF (June 2021). "Crystalloids in FNA specimens of salivary gland lesions: A retrospective study in a single large institute". Cancer Cytopathol 129 (6): 432–438. doi:10.1002/cncy.22395. PMID 33296146.
- ↑ Kishore M, Kaushal M, Dogra S (2019). "Crystalloids in salivary gland lesion: A diagnostic clue". J Lab Physicians 11 (1): 100–101. doi:10.4103/JLP.JLP_120_18. PMC 6437830. PMID 30983813. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6437830/.
- ↑ Thompson, Lester D. R. (2006). Head and Neck Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 295-319. ISBN 978-0443069604.
- ↑ SM. 13 January 2010.
- ↑ http://sciencelinks.jp/j-east/article/200123/000020012301A0753392.php
- ↑ Cohen, MB.; Fisher, PE.; Holly, EA.; Ljung, BM.; Löwhagen, T.; Bottles, K.. "Fine needle aspiration biopsy diagnosis of mucoepidermoid carcinoma. Statistical analysis.". Acta Cytol 34 (1): 43-9. PMID 2296840.
- ↑ Sidawy, Mark K.; Ali, Syed Z. (2007). Fine Needle Aspiration Cytology: A Volume in Foundations in Diagnostic Pathology (1st ed.). Churchill Livingstone. pp. 25. ISBN 978-0443067310.
- ↑ SB. 12 January 2010.
- ↑ GS. 24 February 2010.
- ↑ 14.0 14.1 URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-024-M.htm. Accessed on: 9 April 2012.
- ↑ 15.0 15.1 URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-026-M.htm. Accessed on: 9 April 2012.