Difference between revisions of "Invasive ductal carcinoma of the breast"
m (mamma) |
m (wikify sub-types) |
||
| (2 intermediate revisions by the same user not shown) | |||
| Line 31: | Line 31: | ||
| Tx = | | Tx = | ||
}} | }} | ||
'''Invasive ductal carcinoma of the breast''', also '''breast invasive ductal carcinoma''', is the most common form of [[invasive breast cancer]]. It | '''Invasive ductal carcinoma of the breast''', also '''breast invasive ductal carcinoma''', is the most common form of [[invasive breast cancer]]. It may arise from [[ductal carcinoma in situ]]. | ||
It is also known as '''NST''' (No Specific Type). | It is also known as breast carcinoma of '''NST''' (No Specific/Special Type). Some pathologists prefer this terminology as the sub-typing of breast carcinoma essentially involves exclusion of special types, identified by certain characteristic features. It is also a more appropriate term for high grade tumours which typically lack any acinar or ductal differentiation. | ||
In the context of the [[breast]], the meaning of '''[[invasive ductal carcinoma]]''' is clear; if the context is ''not'' the breast, it may refer to other (unrelated) cancers. | Generically, it may be referred to as ''invasive mammary carcinoma''. In the context of the [[breast]], the meaning of '''[[invasive ductal carcinoma]]''' is clear; if the context is ''not'' the breast, it may refer to other (unrelated) cancers. | ||
==General== | ==General== | ||
*Most common type of [[invasive breast cancer]]. | *Most common type of [[invasive breast cancer]]. | ||
The WHO bluebook classifies certain breast carcinomas as 'special' types, if they show certain characteristic histological features. These special types are sometimes loosely included in the loose label of invasive ductal carcinoma to distinguish them from invasive lobular carcinoma. These include (see individual pages for specific features): | |||
*[[Tubular carcinoma of the breast|Tubular carcinoma]] | |||
*[[Invasive_cribriform_carcinoma_of_the_breast|Cribriform carcinoma]] | |||
*[[Apocrine carcinoma of the breast|Apocrine carcinoma]] | |||
*[[Mucinous breast carcinoma|Mucinous carcinoma]] | |||
*[[Invasive_micropapillary_carcinoma_of_the_breast|Micropapillary]]/[[Invasive_papillary_carcinoma_of_the_breast|papillary]] carcinoma | |||
*[[Medullary breast carcinoma|Medullary-like carcinoma]] | |||
*[[Metaplastic breast carcinoma|Metaplastic carcinoma]] | |||
If a >90% of a tumour is composed of a 'special type', it is considered pure and labelled as in the list above. If one of the special types accounts for 50%, then is is classed as a mixed tumour, e.g. invasive carcinoma of mixed mucinous and no special type. All other tumours are classed as invasive carcinoma of no special type. | |||
Molecular sub-typing through gene expression analysis suggests that are at least 5 distinct types. | |||
==Gross== | ==Gross== | ||
| Line 48: | Line 61: | ||
==Microscopic== | ==Microscopic== | ||
The histological features are highly variable. They are typically graded using the modified Bloom-Richardson grading system, sometimes toponymously referred to as the Nottingham grading system. This has 3 components: tubule formation, nuclear pleomorphism and a mitotic count. Each of the 3 components is scored between 1 and 3 with a final score out of 9. | |||
*Atypical cells: | *Atypical cells: | ||
**Usually >2x [[RBC]] diameter | **Usually >2x [[RBC]] diameter, but may be bland, especially in tubular carcinomas | ||
**Nucleoli common. | **Nucleoli common. | ||
**Forming ducts ''or'' sheets. | **Forming ducts ''or'' sheets. | ||
| Line 70: | Line 84: | ||
*p63 -ve. | *p63 -ve. | ||
Prognostic markers | Prognostic markers are performed to guide treatment | ||
*ER | *ER - about 75% are positive (typically assessed using the Allred/Quick score) | ||
*PR + | *PR staining is more variable, but ER-/PR+ tumours are rare (<1%), so some question the value of PR staining | ||
*HER2 - | *HER2 - about 15-20% are positive | ||
*Ki67 - this correlates with prognosis, but lack of standardisation in quantification hampers more widespread use | |||
Invasive lobular carcinoma versus invasive ductal carcinoma:<ref name=pmid22595945>{{Cite journal | last1 = de Deus Moura | first1 = R. | last2 = Wludarski | first2 = SC. | last3 = Carvalho | first3 = FM. | last4 = Bacchi | first4 = CE. | title = Immunohistochemistry applied to the differential diagnosis between ductal and lobular carcinoma of the breast. | journal = Appl Immunohistochem Mol Morphol | volume = 21 | issue = 1 | pages = 1-12 | month = Jan | year = 2013 | doi = 10.1097/PAI.0b013e318255bafa | PMID = 22595945 }}</ref> | Invasive lobular carcinoma versus invasive ductal carcinoma:<ref name=pmid22595945>{{Cite journal | last1 = de Deus Moura | first1 = R. | last2 = Wludarski | first2 = SC. | last3 = Carvalho | first3 = FM. | last4 = Bacchi | first4 = CE. | title = Immunohistochemistry applied to the differential diagnosis between ductal and lobular carcinoma of the breast. | journal = Appl Immunohistochem Mol Morphol | volume = 21 | issue = 1 | pages = 1-12 | month = Jan | year = 2013 | doi = 10.1097/PAI.0b013e318255bafa | PMID = 22595945 }}</ref> | ||
*E-cadherin - | *E-cadherin typically shows strong membranous positivity in invasive ductal/NST carcinoma | ||
*However, up to 3-5% may be negative, especially higher grade tumours | |||
*Invasive lobular carcinoma is typically negative, but up to 15% may show some staining (though typically weak/incomplete) | |||
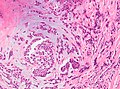
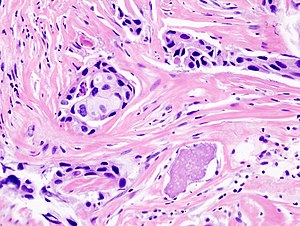
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
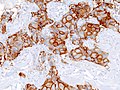
Image:Breast invasive scirrhous carcinoma histopathology (2) HER2 expression.JPG|IDC HER2 positive. | Image:Breast invasive scirrhous carcinoma histopathology (2) HER2 expression.JPG|IDC HER2 positive. | ||
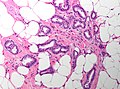
Image:18S08891_tubular_carcinoma_x20a.jpg | Tubular carcinoma - medium mag. (WC) | |||
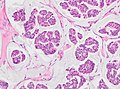
Image:Breast mucinous carcinoma.jpg|Mucinous carcinoma - medium mag. (WC) | |||
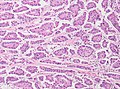
Image:Breast micropapillary carcinoma.jpg|Micropapillary carcinoma - medium mag. (WC) | |||
Image:Breast apocrine carcinoma.jpg|Apocrine carcinoma - medium mag. (WC) | |||
Image:Breast metaplastic carcinoma.jpg|Metaplastic carcinoma - medium mag. (WC) | |||
</gallery> | </gallery> | ||
Latest revision as of 21:29, 29 September 2018
| Invasive ductal carcinoma of the breast | |
|---|---|
| Diagnosis in short | |
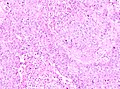
 Invasive ductal carcinoma. H&E stain. | |
| LM DDx | DCIS, invasive lobular carcinoma |
| EM | usu. ER and PR +ve, usu. HER2 -ve, mammaglobin +ve, CK7 +ve, CK20 -ve |
| Grossing notes | breast grossing |
| Staging | breast cancer staging |
| Site | breast |
|
| |
| Signs | +/-palpable breast mass |
| Prevalence | common |
| Prognosis | dependent on stage and grade, good to poor |
| Clin. DDx | other breast tumours |
Invasive ductal carcinoma of the breast, also breast invasive ductal carcinoma, is the most common form of invasive breast cancer. It may arise from ductal carcinoma in situ.
It is also known as breast carcinoma of NST (No Specific/Special Type). Some pathologists prefer this terminology as the sub-typing of breast carcinoma essentially involves exclusion of special types, identified by certain characteristic features. It is also a more appropriate term for high grade tumours which typically lack any acinar or ductal differentiation.
Generically, it may be referred to as invasive mammary carcinoma. In the context of the breast, the meaning of invasive ductal carcinoma is clear; if the context is not the breast, it may refer to other (unrelated) cancers.
General
- Most common type of invasive breast cancer.
The WHO bluebook classifies certain breast carcinomas as 'special' types, if they show certain characteristic histological features. These special types are sometimes loosely included in the loose label of invasive ductal carcinoma to distinguish them from invasive lobular carcinoma. These include (see individual pages for specific features):
- Tubular carcinoma
- Cribriform carcinoma
- Apocrine carcinoma
- Mucinous carcinoma
- Micropapillary/papillary carcinoma
- Medullary-like carcinoma
- Metaplastic carcinoma
If a >90% of a tumour is composed of a 'special type', it is considered pure and labelled as in the list above. If one of the special types accounts for 50%, then is is classed as a mixed tumour, e.g. invasive carcinoma of mixed mucinous and no special type. All other tumours are classed as invasive carcinoma of no special type.
Molecular sub-typing through gene expression analysis suggests that are at least 5 distinct types.
Gross
- White, firm stellate lesion.
Microscopic
The histological features are highly variable. They are typically graded using the modified Bloom-Richardson grading system, sometimes toponymously referred to as the Nottingham grading system. This has 3 components: tubule formation, nuclear pleomorphism and a mitotic count. Each of the 3 components is scored between 1 and 3 with a final score out of 9.
- Atypical cells:
- Usually >2x RBC diameter, but may be bland, especially in tubular carcinomas
- Nucleoli common.
- Forming ducts or sheets.
- +/-Mitoses.
- +/-Necrosis.
- Evidence of invasion:
- Atypical nucleus adjacent to adipocyte - diagnostic.
- "Infiltrative" pattern:
- Small glands of variable size within desmoplastic stroma.
- Glands lined by a single layer of cells.
DDx:
IHC
Myoepithelial markers - diagnostic for invasion:
- SMMS -ve.
- p63 -ve.
Prognostic markers are performed to guide treatment
- ER - about 75% are positive (typically assessed using the Allred/Quick score)
- PR staining is more variable, but ER-/PR+ tumours are rare (<1%), so some question the value of PR staining
- HER2 - about 15-20% are positive
- Ki67 - this correlates with prognosis, but lack of standardisation in quantification hampers more widespread use
Invasive lobular carcinoma versus invasive ductal carcinoma:[1]
- E-cadherin typically shows strong membranous positivity in invasive ductal/NST carcinoma
- However, up to 3-5% may be negative, especially higher grade tumours
- Invasive lobular carcinoma is typically negative, but up to 15% may show some staining (though typically weak/incomplete)
Images
See also
References
- ↑ de Deus Moura, R.; Wludarski, SC.; Carvalho, FM.; Bacchi, CE. (Jan 2013). "Immunohistochemistry applied to the differential diagnosis between ductal and lobular carcinoma of the breast.". Appl Immunohistochem Mol Morphol 21 (1): 1-12. doi:10.1097/PAI.0b013e318255bafa. PMID 22595945.