Difference between revisions of "Lymph node pathology"
Jump to navigation
Jump to search
(touch) |
|||
| Line 200: | Line 200: | ||
===IHC=== | ===IHC=== | ||
Screening panel: | Screening panel: | ||
*CD3. | *[[CD3]]. | ||
*CD5. | *[[CD5]]. | ||
*CD10. | *CD10. | ||
*CD20. | *[[CD20]]. | ||
*CD30. | *CD30. | ||
*CD15. | *CD15. | ||
Revision as of 15:45, 5 March 2017
This article deals with non-haematologic malignant, i.e. metastases, and non-malignant lymph node pathology. An introduction to the lymph node is in the lymph nodes article.
Haematologic malignancies (in lymph nodes) are dealt with in other articles - see haematopathology and lymphoma.
Overview
Clinical:
- Lymphadenopathy.
Differential diagnosis:[1]
- Infectious - fungal, mycobacterial, viral, protozoal (Toxoplasma), bacterial (Chlamydia, Rickettsia, Bartonella)).
- Neoplastic - lymphoma, carcinoma.
- Endocrine - hyperthyroidism.
- Trauma.
- Autoimmune - SLE, RA, dermatomyositis.
- Inflammatory - drugs (phenytoin).
- Idiopathic - sarcoidosis.
Overview in a table
| Entity | Key feature | Other findings | IHC | DDx | Image |
|---|---|---|---|---|---|
| Non-specific reactive follicular hyperplasia (NSRFH) | large spaced cortical follicles | tingible body macrophages, normal dark/light GC pattern | BCL2 -ve | infection (Toxoplasmosis, HIV/AIDS), Hodgkin's lymphoma | image ? |
| Lymph node metastasis | foreign cell population, usu. in subcapsular sinuses | +/-nuclear atypia, +/-malignant architecture | dependent on tumour type (see IHC) | dependent on morphology, endometriosis (mimics adenocarcinoma), ectopic decidua (mimics SCC) | |
| Progressive transformation of germinal centers | large (atypical) germinal centers | poorly demarcated germinal center (GC)/mantle zone interfaces, expanded mantle zone | IHC to r/o nodular lymphocyte predominant Hodgkin lymphoma (NLPHL) | NLPHL, follicular hyperplasia | |
| Toxoplasmosis | large follicles; epithelioid cells perifollicular & intrafollicular | reactive GCs, monocytoid cell clusters, epithelioid cells | IHC for toxoplasma | NSRFH, HIV/AIDS, Hodgkin's lymphoma | |
| Kikuchi disease (histiocystic necrotizing lymphadenitis) | No PMNs | histiocytes, necrosis | IHC for large cell lymphoma (CD30 + others) | SLE (has (blue) hematoxylin bodies in necrotic areas), large cell lymphomas | |
| Cat-scratch disease | PMNs in necrotic area | "stellate" (or serpentine) shaped microabscesses, granulomas | B. henselae, Dieterle stain | HIV/AIDS, NSRFH | |
| Dermatopathic lymphadenopathy | melanin-laden histiocytes | histiocytosis | S-100+ve (interdigitating dendritic cells), CD1a+ve (Langerhans cells) | cutaneous T-cell lymphoma | |
| Kimura disease | eosinophils | angiolymphoid proliferation (thick-walled blood vessels with hobnail endothelial cells) | IHC ? | Langerhans cell histiocytosis, drug reaction, angiolymphoid hyperplasia with eosinophilia | |
| Langerhans cell histiocytosis | abundant histiocytes with reniform nuclei | often prominent eosinophilia | S-100+, CD1a+ | Kimura disease (eosinophilia), Rosai-Dorfman disease | |
| Rosai-Dorfman disease | sinus histiocytosis | emperipolesis (intact cell within a macrophage) | S-100+, CD1a- | Langerhans cell histiocytosis | |
| Systemic lupus erythematosus lymphadenopathy | (blue) hematoxylin bodies | necrosis, no PMNs | IHC for large cell lymphoma (CD30 + others) | Kikuchi disease, large cell lymphomas | |
| Castleman disease, hyaline vascular variant | thick mantle cell layer with laminar appearance ("onion skin" layering) | hyaline (pink crap), lollipops (large vessels into GC), no mitoses in GC | IHC - to r/o mantle cell lymphoma | mantle cell lymphoma, HIV/AIDS | |
| Castleman disease, plasma cell variant | thick mantle cell layer | sinus perserved, interfollicular plasma cells, mitoses in GC | HHV-8 | HIV/AIDS | image ? |
| Intranodal palisaded myofibroblastoma | spindle cells with nuclear palisading | RBC extravasation, fibrillary bodies with a central vessel "amianthoid fibers" | SMA+, cyclin D1+ | schwannoma |
Follicular lymphoma vs. reactive follicular hyperplasia
Factors to consider:[2]
| Reactive follicular hyperplasia |
Follicular lymphoma | |
|---|---|---|
| Follicle location | cortex | cortex and medulla |
| Germinal center edge | sharp/well-demarcated | poorly demarcated |
| Germinal center density | well spaced, sinuses open | crowded, sinuses effaced/ compressed to nothingness |
| Tingible body macrophages |
common | uncommon |
| Germinal center light/dark pattern |
normal | abnormal |
Lymph node metastasis
Main article: Lymph node metastasis
Kaposi sarcoma
Main article: Kaposi sarcoma
- One of the few non-lymphoid primary lymph node tumours.[3]
Melanocytic nevi
Main article: Melanocytic lesions
- Benign melanocytic nevi can be found in lymph nodes.[3]
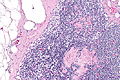
Progressive transformation of germinal centers
Main article: Progressive transformation of germinal centers
- Abbreviated as PTGC.
Reactive follicular hyperplasia
General
- Many causes - including: bacteria, viruses, chemicals, drugs, allergens.
- In only approximately 10% can definitive cause be identified.[4]
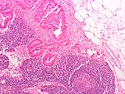
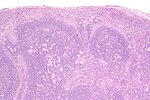
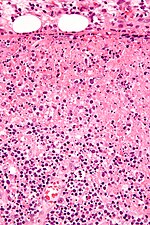
Microscopic
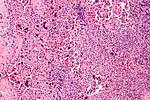
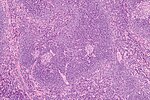
Features:[5]
- Enlarged follicles, follicle size variation - key feature with:
- Large germinal centers (pale on H&E).
- Mitoses common.
- Variable lymphocyte morphology.
- Tingible-body macrophage (large, pale cells with junk in the cytoplasm).
- Germinal centers (GCs) have a crisp/sharp edge.
- Normal dark/light variation of GCs; superficial aspect light, deeper aspect darker.
- Rim of small (inactive) lymphocytes.
- Large germinal centers (pale on H&E).
DDx:
- Hodgkin lymphoma - with rare Reed-Sternberg cells.
- Non-Hodgkin lymphoma.
- T-cell/histiocyte-rich large B cell lymphoma.
Image: Normal lymph node (umdnj.edu).
IHC
Screening panel:
Others:
- BCL2 -ve.
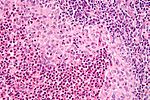
Diffuse paracortical hyperplasia
General
- Benign.
Microscopic
Features:[5]
- Interfollicular areas enlarged - key feature.
- T cell population increased.
- Plasma cells.
- Macrophages.
- Large Reed-Sternberg-like cells.
Sinus histiocytosis
- Should not be confused with sinus histiocytosis with massive lymphadenopathy, also known as Rosai-Dorfman disease.
Main article: Sinus histiocytosis
Kikuchi disease
Main article: Kikuchi disease
Systemic lupus erythematosus lymphadenopathy
Main article: Systemic lupus erythematosus lymphadenopathy
Castleman disease
Main article: Castleman disease
Cat-scratch disease
- AKA cat scratch fever.
Main article: Cat scratch disease
Toxoplasma lymphadenitis
Main article: Toxoplasma
General
- Caused by protozoan Toxoplasma gondii.
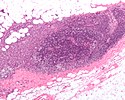
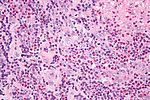
Microscopic
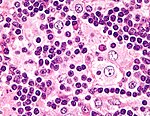
Features:[8]
- Reactive germinal centers (pale areas - larger than usual).
- Often poorly demarcated - due to loose epithelioid cell clusters at germinal center edge - key feature.
- Epithelioid cells - perifollicular & intrafollicular.
- Loose aggregates of histiocytes (do not form round granulomas):
- Abundant pale cytoplasm.
- Nucleoli.
- Loose aggregates of histiocytes (do not form round granulomas):
- Monocytoid cells (monocyte-like cells) - in cortex & paracortex.
- Large cells in islands/sheets key feature with:
- Abundant pale cytoplasm - important.
- Well-defined cell border - important.
- Singular nucleus.
- Cell clusters usually have interspersed neutrophils.
- Large cells in islands/sheets key feature with:
Images:
Notes:
- Monocytoid cells CD68 -ve.
IHC
- IHC for toxoplasmosis.
Dermatopathic lymphadenopathy
Main article: Dermatopathic lymphadenopathy
Kimura lymphadenopathy
Main article: Kimura disease
Rosai-Dorfman disease
- Abbreviated RDD.
- AKA sinus histiocytosis with massive lymphadenopathy, abbreviated SHML.
Main article: Rosai-Dorfman disease
Langerhans cell histiocytosis
Main article: Langerhans cell histiocytosis
Lymph node hyalinization
- AKA hyalinized lymph node.
General
- Benign.
- Associated with aging.[9]
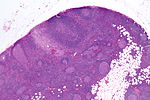
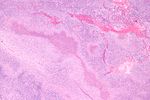
Microscopic
Features:
- Hyaline material (acellular pink stuff on H&E) within a lymph node.
Subdivided into:[9]
- Mediastinal-type.
- Usually in medullary sinus.
- Onion peel-like appearance.
- Pelvic-type hyalinization.
- Discrete round, eosinophilic, glassy appearance at low power, whirled/fibrous at high power.
- +/-Calcification.
DDx:
- Amyloidosis - cotton candy-like appearance, usu. no calcifications.
Images
www:
Sign out
- Not reported.
See also
References
- ↑ URL: http://path.upmc.edu/cases/case289.html. Accessed on: 14 January 2012.
- ↑ DB. 4 August 2010.
- ↑ 3.0 3.1 Bigotti, G.; Coli, A.; Mottolese, M.; Di Filippo, F. (Sep 1991). "Selective location of palisaded myofibroblastoma with amianthoid fibres.". J Clin Pathol 44 (9): 761-4. PMC 496726. PMID 1918406. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC496726/.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 174. ISBN 978-0781775960.
- ↑ 5.0 5.1 Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 179. ISBN 978-0781775960.
- ↑ Kaushik V, Malik TH, Bishop PW, Jones PH (June 2004). "Histiocytic necrotising lymphadenitis (Kikuchi's disease): a rare cause of cervical lymphadenopathy". Surgeon 2 (3): 179–82. PMID 15570824.
- ↑ URL: http://www.mayoclinic.com/health/castleman-disease/DS01000. Accessed on: 17 June 2010.
- ↑ Ioachim, Harry L; Medeiros, L. Jeffrey (2008). Ioachim's Lymph Node Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 113. ISBN 978-0781775960.
- ↑ 9.0 9.1 Taniguchi, I.; Murakami, G.; Sato, A.; Fujiwara, D.; Ichikawa, H.; Yajima, T.; Kohama, G. (Oct 2003). "Lymph node hyalinization in elderly Japanese.". Histol Histopathol 18 (4): 1169-80. PMID 12973685.