Difference between revisions of "Squamous cell carcinoma of the lung"
Jump to navigation
Jump to search
(→IHC) |
|||
| (9 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Lung squamous carcinoma -- intermed mag.jpg | ||
| Width = | | Width = | ||
| Caption = Squamous cell carcinoma of the lung. [[ | | Caption = Squamous cell carcinoma of the lung. [[H&E stain]]. | ||
| Synonyms = squamous carcinoma of the lung | | Synonyms = squamous carcinoma of the lung | ||
| Micro = | | Micro = | ||
| Line 9: | Line 9: | ||
| LMDDx = [[lung adenocarcinoma]], [[non-small cell lung carcinoma]], metastatic [[squamous cell carcinoma]], others | | LMDDx = [[lung adenocarcinoma]], [[non-small cell lung carcinoma]], metastatic [[squamous cell carcinoma]], others | ||
| Stains = | | Stains = | ||
| IHC = p40 +ve, p63 +ve, TTF-1 -ve, CK7 -ve | | IHC = [[p40]] +ve, [[p63]] +ve, [[TTF-1]] -ve, CK7 -ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| Line 15: | Line 15: | ||
| Gross = | | Gross = | ||
| Grossing = | | Grossing = | ||
| Staging = [[lung cancer staging]] | |||
| Site = [[lung]] - see [[lung tumours]] | | Site = [[lung]] - see [[lung tumours]] | ||
| Assdx = | | Assdx = | ||
| Line 58: | Line 59: | ||
*+/-Small nucleolus. | *+/-Small nucleolus. | ||
*Intracellular bridges - classic. | *Intracellular bridges - classic. | ||
Note: | |||
*[[Lymphovascular invasion]] (LVI) is relatively common in small tumours. In one series of NSLC tumours less than 2 cm the prevalence of LVI was 16%.<ref>{{cite journal |author=Tao H, Hayashi T, Sano F, ''et al.'' |title=Prognostic impact of lymphovascular invasion compared with that of visceral pleural invasion in patients with pN0 non-small-cell lung cancer and a tumor diameter of 2 cm or smaller |journal=J. Surg. Res. |volume=185 |issue=1 |pages=250–4 |year=2013 |month=November |pmid=23830361 |doi=10.1016/j.jss.2013.05.104 |url=}}</ref> | |||
**Unlike in [[lung adenocarcinoma]], LVI in lung SCC does ''not'' seem to increase the risk of distant metastases and death.<ref name=pmid22617241>{{cite journal |author=Higgins KA, Chino JP, Ready N, ''et al.'' |title=Lymphovascular invasion in non-small-cell lung cancer: implications for staging and adjuvant therapy |journal=J Thorac Oncol |volume=7 |issue=7 |pages=1141–7 |year=2012 |month=July |pmid=22617241 |doi=10.1097/JTO.0b013e3182519a42 |url=}}</ref> | |||
DDx: | DDx: | ||
| Line 65: | Line 70: | ||
*[[Small cell carcinoma of the lung]] - for ''basaloid squamous cell carcinoma''. | *[[Small cell carcinoma of the lung]] - for ''basaloid squamous cell carcinoma''. | ||
===Grading=== | |||
There is no consensus on how grading of lung SCC should be done; however, a three tiered system is suggested in the CAP protocol,<ref name=cap_protocol_v3400>URL: [http://www.cap.org/ShowProperty?nodePath=/UCMCon/Contribution%20Folders/WebContent/pdf/cp-lung-16protocol-3400.pdf http://www.cap.org/ShowProperty?nodePath=/UCMCon/Contribution%20Folders/WebContent/pdf/cp-lung-16protocol-3400.pdf]. Version: 3.4.0.0. Accessed on: 23 March 2016.</ref> and some older data is suggestive that such a system for lung SCC can be predictive.<ref name=pmid7092385>{{Cite journal | last1 = Chung | first1 = CK. | last2 = Zaino | first2 = R. | last3 = Stryker | first3 = JA. | last4 = O'Neill | first4 = M. | last5 = DeMuth | first5 = WE. | title = Carcinoma of the lung: evaluation of histological grade and factors influencing prognosis. | journal = Ann Thorac Surg | volume = 33 | issue = 6 | pages = 599-604 | month = Jun | year = 1982 | doi = | PMID = 7092385 }}</ref> | |||
The grading system loosely defined by the CAP protocol (version 3.4.0.0):<ref name=cap_protocol_v3400/> | |||
*Grade 1 (well differentiated) - extensive keratinization. | |||
*Grade 2 (moderately differentiated) - some keratinization. | |||
*Grade 3 (poorly differentiated) - no/little keratinization. | |||
===Images=== | |||
<gallery> | |||
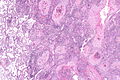
Image: Lung squamous carcinoma -- very low mag.jpg | Lung SCC - very low mag. (WC) | |||
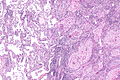
Image: Lung squamous carcinoma -- low mag.jpg | Lung SCC - low mag. (WC) | |||
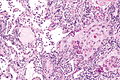
Image: Lung squamous carcinoma -- intermed mag.jpg | Lung SCC - intermed. mag. (WC) | |||
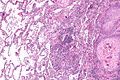
Image: Lung squamous carcinoma -- high mag.jpg | Lung SCC - high mag. (WC) | |||
Image: Lung squamous carcinoma - alt -- low mag.jpg | Lung SCC - low mag. (WC) | |||
Image: Lung squamous carcinoma - alt -- intermed mag.jpg | Lung SCC - intermed. mag. (WC) | |||
</gallery> | |||
====Cytology==== | |||
<gallery> | |||
Image: Squamous carcinoma lung cytology.gif | Lung SCC - cytology. (WC) | |||
</gallery> | |||
==IHC== | ==IHC== | ||
| Line 81: | Line 104: | ||
**Positive in [[adenocarcinoma of the lung]]. | **Positive in [[adenocarcinoma of the lung]]. | ||
SCC versus adenocarcinoma | ===SCC versus adenocarcinoma=== | ||
*p40 +ve. | *p40 +ve. | ||
*CK5/6 +ve. | *CK5/6 +ve. | ||
*TTF-1 -ve. | *TTF-1 -ve. | ||
*[[Napsin]] -ve. | *[[Napsin]] -ve. | ||
===Lung SCC versus metastatic bladder urothelial carcinoma=== | |||
As per Gruver ''et al.'':<ref name=pmid23106579>{{Cite journal | last1 = Gruver | first1 = AM. | last2 = Amin | first2 = MB. | last3 = Luthringer | first3 = DJ. | last4 = Westfall | first4 = D. | last5 = Arora | first5 = K. | last6 = Farver | first6 = CF. | last7 = Osunkoya | first7 = AO. | last8 = McKenney | first8 = JK. | last9 = Hansel | first9 = DE. | title = Selective immunohistochemical markers to distinguish between metastatic high-grade urothelial carcinoma and primary poorly differentiated invasive squamous cell carcinoma of the lung. | journal = Arch Pathol Lab Med | volume = 136 | issue = 11 | pages = 1339-46 | month = Nov | year = 2012 | doi = 10.5858/arpa.2011-0575-OA | PMID = 23106579 }}</ref> | |||
{| class="wikitable sortable" | |||
! IHC | |||
! Lung <Br>SCC | |||
! Bladder <br>[[urothelial carcinoma|UCC]] | |||
|- | |||
| CK7 | |||
| 33% +ve | |||
| 100% +ve | |||
|- | |||
| CK20 | |||
| 7% +ve | |||
| 54% +ve | |||
|- | |||
| GATA-3 | |||
| 23% +ve | |||
| 78% +ve | |||
|- | |||
| Desmoglein-3 | |||
| 87% +ve | |||
| 11% +ve | |||
|- | |||
| CK14 | |||
| 77% +ve | |||
| 32% +ve | |||
|- | |||
| Uroplakin III | |||
| 0% +ve | |||
| 14% +ve | |||
|} | |||
==Sign out== | ==Sign out== | ||
<pre> | |||
Lung, Right Upper Lobe, Core Biopsy: | |||
- SQUAMOUS CELL CARCINOMA. | |||
COMMENT: | |||
The tumour stains as follows: | |||
POSITIVE: p40, CK5/6. | |||
NEGATIVE: TTF-1, napsin. | |||
</pre> | |||
===Block letters=== | |||
<pre> | <pre> | ||
LUNG, RIGHT UPPER LOBE, BIOPSY: | LUNG, RIGHT UPPER LOBE, BIOPSY: | ||
Latest revision as of 17:22, 20 December 2016
| Squamous cell carcinoma of the lung | |
|---|---|
| Diagnosis in short | |
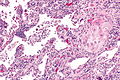
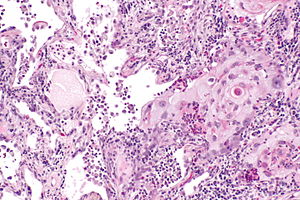 Squamous cell carcinoma of the lung. H&E stain. | |
|
| |
| Synonyms | squamous carcinoma of the lung |
| LM DDx | lung adenocarcinoma, non-small cell lung carcinoma, metastatic squamous cell carcinoma, others |
| IHC | p40 +ve, p63 +ve, TTF-1 -ve, CK7 -ve |
| Staging | lung cancer staging |
| Site | lung - see lung tumours |
|
| |
| Clinical history | smoking |
| Symptoms | +/-hemoptysis |
| Prevalence | common |
| Blood work | serum calcium elevated |
| Radiology | typically a mass assoc. with a large airway, +/-spiculated, +/-cavitation |
| Prognosis | usually poor |
| Clin. DDx | other lung tumours - esp. small cell carcinoma of the lung |
| Treatment | surgical resection if possible |
Squamous cell carcinoma of the lung, also lung squamous cell carcinoma, is a common malignant lung tumour that is associated with smoking.
It is also known as squamous carcinoma of the lung and lung squamous carcinoma.
Squamous cell carcinoma can be abbreviated SCC; however, this can be confusing as small cell carcinoma is sometimes abbreviated as such.
General
- Strong association with smoking.
- May be treated with surgery.
Clinical:
- May be associated with elevated serum calcium.[1]
- +/-Hemoptysis.
Gross
- Lung mass - usually centrally located, i.e. associated with a large airway.
Image
Microscopic
Features:
- Central nucleus.
- Dense appearing cytoplasm, usu. eosinophilic.
- +/-Small nucleolus.
- Intracellular bridges - classic.
Note:
- Lymphovascular invasion (LVI) is relatively common in small tumours. In one series of NSLC tumours less than 2 cm the prevalence of LVI was 16%.[2]
- Unlike in lung adenocarcinoma, LVI in lung SCC does not seem to increase the risk of distant metastases and death.[3]
DDx:
- Metastatic squamous cell carcinoma.
- Adenocarcinoma of the lung.
- Non-small cell lung carcinoma - diagnosis should be avoided if possible.
- Small cell carcinoma of the lung - for basaloid squamous cell carcinoma.
Grading
There is no consensus on how grading of lung SCC should be done; however, a three tiered system is suggested in the CAP protocol,[4] and some older data is suggestive that such a system for lung SCC can be predictive.[5]
The grading system loosely defined by the CAP protocol (version 3.4.0.0):[4]
- Grade 1 (well differentiated) - extensive keratinization.
- Grade 2 (moderately differentiated) - some keratinization.
- Grade 3 (poorly differentiated) - no/little keratinization.
Images
Cytology
IHC
- p40 +ve.[6]
- p63 +ve -- less specific.
- Calponin -ve.
- CK5/6 +ve.
Others:[7]
- CK7 -ve.
- CK20 -ve.
- TTF-1 -ve.
- Positive in adenocarcinoma of the lung.
SCC versus adenocarcinoma
- p40 +ve.
- CK5/6 +ve.
- TTF-1 -ve.
- Napsin -ve.
Lung SCC versus metastatic bladder urothelial carcinoma
As per Gruver et al.:[8]
| IHC | Lung SCC |
Bladder UCC |
|---|---|---|
| CK7 | 33% +ve | 100% +ve |
| CK20 | 7% +ve | 54% +ve |
| GATA-3 | 23% +ve | 78% +ve |
| Desmoglein-3 | 87% +ve | 11% +ve |
| CK14 | 77% +ve | 32% +ve |
| Uroplakin III | 0% +ve | 14% +ve |
Sign out
Lung, Right Upper Lobe, Core Biopsy: - SQUAMOUS CELL CARCINOMA. COMMENT: The tumour stains as follows: POSITIVE: p40, CK5/6. NEGATIVE: TTF-1, napsin.
Block letters
LUNG, RIGHT UPPER LOBE, BIOPSY: - INVASIVE SQUAMOUS CELL CARCINOMA. COMMENT: The tumour stains as follows: POSITIVE: p40, CK5/6. NEGATIVE: TTF-1, napsin.
Resection
LUNG, RIGHT UPPER LOBE, LOBECTOMY: - SQUAMOUS CELL CARCINOMA, MODERATELY DIFFERENTIATED, pT2b, pN0. -- MARGINS NEGATIVE. -- PLEASE SEE TUMOUR SUMMARY.
See also
References
- ↑ Campbell, JH.; Ralston, S.; Boyle, IT.; Banham, SW. (May 1991). "Symptomatic hypercalcaemia in lung cancer.". Respir Med 85 (3): 223-7. PMID 1831917.
- ↑ Tao H, Hayashi T, Sano F, et al. (November 2013). "Prognostic impact of lymphovascular invasion compared with that of visceral pleural invasion in patients with pN0 non-small-cell lung cancer and a tumor diameter of 2 cm or smaller". J. Surg. Res. 185 (1): 250–4. doi:10.1016/j.jss.2013.05.104. PMID 23830361.
- ↑ Higgins KA, Chino JP, Ready N, et al. (July 2012). "Lymphovascular invasion in non-small-cell lung cancer: implications for staging and adjuvant therapy". J Thorac Oncol 7 (7): 1141–7. doi:10.1097/JTO.0b013e3182519a42. PMID 22617241.
- ↑ 4.0 4.1 URL: http://www.cap.org/ShowProperty?nodePath=/UCMCon/Contribution%20Folders/WebContent/pdf/cp-lung-16protocol-3400.pdf. Version: 3.4.0.0. Accessed on: 23 March 2016.
- ↑ Chung, CK.; Zaino, R.; Stryker, JA.; O'Neill, M.; DeMuth, WE. (Jun 1982). "Carcinoma of the lung: evaluation of histological grade and factors influencing prognosis.". Ann Thorac Surg 33 (6): 599-604. PMID 7092385.
- ↑ Bishop, JA.; Teruya-Feldstein, J.; Westra, WH.; Pelosi, G.; Travis, WD.; Rekhtman, N. (Mar 2012). "p40 (ΔNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma.". Mod Pathol 25 (3): 405-15. doi:10.1038/modpathol.2011.173. PMID 22056955.
- ↑ Montezuma, D.; Azevedo, R.; Lopes, P.; Vieira, R.; Cunha, AL.; Henrique, R. (Dec 2013). "A panel of four immunohistochemical markers (CK7, CK20, TTF-1, and p63) allows accurate diagnosis of primary and metastatic lung carcinoma on biopsy specimens.". Virchows Arch 463 (6): 749-54. doi:10.1007/s00428-013-1488-z. PMID 24126803.
- ↑ Gruver, AM.; Amin, MB.; Luthringer, DJ.; Westfall, D.; Arora, K.; Farver, CF.; Osunkoya, AO.; McKenney, JK. et al. (Nov 2012). "Selective immunohistochemical markers to distinguish between metastatic high-grade urothelial carcinoma and primary poorly differentiated invasive squamous cell carcinoma of the lung.". Arch Pathol Lab Med 136 (11): 1339-46. doi:10.5858/arpa.2011-0575-OA. PMID 23106579.