Microsatellite instability in colorectal cancer
Jump to navigation
Jump to search
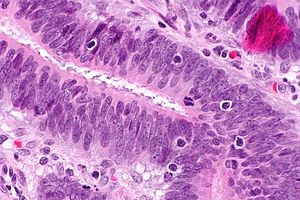
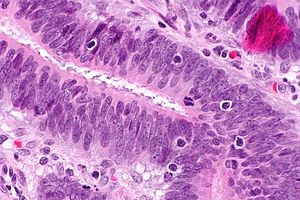
Intratumoural lymphocytic response in colorectal carcinoma, as may be seen in microsatellite instability. H&E stain. (WC)
Microsatellite instability in colorectal cancer, often abbreviated MSI, is recognized as an important predictor of outcome in colorectal adenocarcinoma, and may be seen in the context of Lynch syndrome.
General
- Can be sporadic, i.e. non-syndromic.[1]
- Strong association with Lynch syndrome.[2][1]
Features:[3]
- Prognosis: slightly better than other CRC without MSI.
- Treatment implication: different response to chemotherapy.
When to test
- National Comprehensive Cancer Network (NCCN) in the USA recommends testing all individual with colorectal cancer that are under the age of 70 years.[4]
- A draft document (written in 2015) from CAP, ASCO and others suggests testing all colorectal cancer cases for MSI.[5]
- In Canada, the guidelines vary by the province.[6] Some use the Bethesda criteria (see below) and others have their own set of criteria.
Bethesda criteria of 2004 for MSI testing
MSI testing should be done if any of the following apply:[7]
- Colorectal cancer in patient <50 years old.
- Colorectal cancer with MSI-H histology <60 years old.
- MSI-H histology (any of the following): mucinous differentiation, signet ring differentiation, medullary growth pattern, TILs, Crohn's like reaction.
- Regardless of age - any of the following:
- HNPCC-associated tumours.†
- Synchronous colorectal cancer.
- Metachronous colorectal cancer.
- Colorectal cancer in an individual with:
- One or more first degree relatives with a HNPCC-related tumour diagnosed when <50 years old.
- Two or more first- or second degree relatives with HNPCC-related tumours (diagnosed at any age).
Notes:
- Formally known as Revised Bethesda Guidelines for Hereditary Nonpolyposis Colorectal Cancer (Lynch Syndrome) and Microsatellite Instability.
- †Includes: colorectum, endometrium, stomach, ovary, pancreas, ureter and renal pelvis, biliary tract and brain (usu. glioblastoma), sebaceous gland adenomas and keratoacanthoma in Muir-Torre syndrome and small bowel carcinoma.[7]
MSI classification
MSI associated cancers can be classified into:[8][9]
- MSI-H >= 30% of loci have abnormality.
- MSI-L <30% of loci have abnormality.
Note:
- In the context of no chemotherapy, individuals with MSI-H tumours have a superior outcome to those with MSI-L tumours.[10]
- With chemotherapy the outcomes are similar.
Gross
Features:[3]
- Location: proximal colon, i.e. right-sided, predominance.
Microscopic
Features:[3]
- Lymphocytic infiltrate - see intratumoural lymphocytic response.
- Large peritumoural collections of lymphocytes - see peritumoural lymphocytic response.
- Pushing border.[11]
- Histomorphology:
- Poorly differentiated.
- Mucinous.
- Signet ring.
- Medullary.[12]
Molecular
Commonly associated abnormalities in the genes:
- MLH1.
- PMS2.
- MSH2.
- MSH6.
Less common abnormalities:
- PMS1.
- MLH3.
- MSH3.
IHC
Immunostains are commonly done for:
- MLH1.
- PMS2.
- MSH2.
- MSH6.
IHC interpretation:
- Loss of nuclear staining in nuclei of the tumour implies a mutation.
- Nuclear staining = normal.
- Patchy MSH6 is considered normal.[citation needed]
MSI staining loss patterns:[13]
- MLH1 and PMS2 are often lost together, as MLH1 loss results in PMS2 loss.
- MSH2 and MSH6 are often lost together, as MSH2 loss results in MSH6 loss.
Implication of MSI staining loss patterns:
- PMS2 & MSH6 can be used as a screen.[13]
Etiology/significance loss of staining
- MSH2 mutations (IHC stain -ve) - often associated with a germline mutation,[14] while mutations in MLH1 are usually sporatic.[15]
- PMS2 mutations (IHC stain -ve) - often associated with a germline mutation.[16]
How to remember the more important MSI stuff:
- The MSHs are paired together.
- MSH (Mount Sinai Hospital) is where they started it in the city.
- PMS sucks... it's with the other one (MLH).
- The higher numbers in the pairings (PMS2, MSH6) are the screening tests (High Screen Pass).
- The 2s (MSH2, PMS2) are associated with germline mutations (Four legs good two legs bad!).
See also
References
- ↑ 1.0 1.1 Heinimann, K. (2013). "Toward a Molecular Classification of Colorectal Cancer: The Role of Microsatellite Instability Status.". Front Oncol 3: 272. doi:10.3389/fonc.2013.00272. PMID 24199172.
- ↑ Mensenkamp, AR.; Vogelaar, IP.; van Zelst-Stams, WA.; Goossens, M.; Ouchene, H.; Hendriks-Cornelissen, SJ.; Kwint, MP.; Hoogerbrugge, N. et al. (Dec 2013). "Somatic mutations in MLH1 and MSH2 are a Frequent Cause of Mismatch-repair Deficiency in Lynch Syndrome-like Tumors.". Gastroenterology. doi:10.1053/j.gastro.2013.12.002. PMID 24333619.
- ↑ 3.0 3.1 3.2 Boland CR, Goel A (June 2010). "Microsatellite instability in colorectal cancer". Gastroenterology 138 (6): 2073–2087.e3. doi:10.1053/j.gastro.2009.12.064. PMID 20420947.
- ↑ URL: http://www.medscape.com/viewarticle/821981. Accessed on: 12 January 2016.
- ↑ URL: http://www.amp.org/committees/clinical_practice/documents/20150327CRCMMDraftRecommendationsforOCP-UPDATEDfinaldraft_001.pdf. Accessed on: 12 January 2016.
- ↑ URL: http://www.ncbi.nlm.nih.gov/books/NBK321468/. Accessed on: 12 January 2016.
- ↑ 7.0 7.1 Umar, A.; Boland, CR.; Terdiman, JP.; Syngal, S.; de la Chapelle, A.; Rüschoff, J.; Fishel, R.; Lindor, NM. et al. (Feb 2004). "Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability.". J Natl Cancer Inst 96 (4): 261-8. PMID 14970275.
- ↑ Lawes DA, Pearson T, Sengupta S, Boulos PB (August 2005). "The role of MLH1, MSH2 and MSH6 in the development of multiple colorectal cancers". Br. J. Cancer 93 (4): 472–7. doi:10.1038/sj.bjc.6602708. PMC 2361590. PMID 16106253. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2361590/.
- ↑ Guidoboni M, Gafà R, Viel A, et al. (July 2001). "Microsatellite instability and high content of activated cytotoxic lymphocytes identify colon cancer patients with a favorable prognosis". Am. J. Pathol. 159 (1): 297–304. PMC 1850401. PMID 11438476. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1850401/.
- ↑ Ribic, CM.; Sargent, DJ.; Moore, MJ.; Thibodeau, SN.; French, AJ.; Goldberg, RM.; Hamilton, SR.; Laurent-Puig, P. et al. (Jul 2003). "Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer.". N Engl J Med 349 (3): 247-57. doi:10.1056/NEJMoa022289. PMID 12867608.
- ↑ Pollet, A. 18 October 2010.
- ↑ Truta B, Chen YY, Blanco AM, et al. (2008). "Tumor histology helps to identify Lynch syndrome among colorectal cancer patients". Fam. Cancer 7 (3): 267–74. doi:10.1007/s10689-008-9186-8. PMID 18283560.
- ↑ 13.0 13.1 Hall, G.; Clarkson, A.; Shi, A.; Langford, E.; Leung, H.; Eckstein, RP.; Gill, AJ. (2010). "Immunohistochemistry for PMS2 and MSH6 alone can replace a four antibody panel for mismatch repair deficiency screening in colorectal adenocarcinoma.". Pathology 42 (5): 409-13. doi:10.3109/00313025.2010.493871. PMID 20632815.
- ↑ Mangold E, Pagenstecher C, Friedl W, et al. (December 2005). "Tumours from MSH2 mutation carriers show loss of MSH2 expression but many tumours from MLH1 mutation carriers exhibit weak positive MLH1 staining". J. Pathol. 207 (4): 385–95. doi:10.1002/path.1858. PMID 16216036.
- ↑ A. Pollett. 2010.
- ↑ Vaughn CP, Robles J, Swensen JJ, et al. (May 2010). "Clinical analysis of PMS2: mutation detection and avoidance of pseudogenes". Hum. Mutat. 31 (5): 588–93. doi:10.1002/humu.21230. PMID 20205264.