Difference between revisions of "Intraoperative consultation"
Jump to navigation
Jump to search
| (44 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
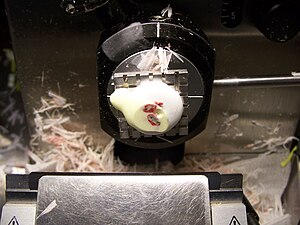
'''Intraoperative consultation''', also '''quick section''' and '''frozen section''', is when a surgeon requests an opinion during an operation so that they can appropriately manage a patient. It is abbreviated '''IC'''. | [[Image:Tissue for frozen section in cryostat.JPG|thumb|right|Tissue within a cryostat, as seen during an intraoperative consultation. (WC/000jaw)]] | ||
'''Intraoperative consultation''', also '''quick section''' and '''frozen section''', is when a surgeon requests an opinion during an operation so that they can appropriately manage a patient. It is abbreviated '''IC'''. Frozen section is often abbreviated '''FS'''. | |||
==Why | ==Why intraoperative consultations are done== | ||
Reasons why IC are done:<ref>{{Cite journal | last1 = Zarbo | first1 = RJ. | last2 = Schmidt | first2 = WA. | last3 = Bachner | first3 = P. | last4 = Howanitz | first4 = PJ. | last5 = Meier | first5 = FA. | last6 = Schifman | first6 = RB. | last7 = Boone | first7 = DJ. | last8 = Herron | first8 = RM. | title = Indications and immediate patient outcomes of pathology intraoperative consultations. College of American Pathologists/Centers for Disease Control and Prevention Outcomes Working Group Study. | journal = Arch Pathol Lab Med | volume = 120 | issue = 1 | pages = 19-25 | month = Jan | year = 1996 | doi = | PMID = 8554440 }} | Reasons why IC are done:<ref name=pmid8554440>{{Cite journal | last1 = Zarbo | first1 = RJ. | last2 = Schmidt | first2 = WA. | last3 = Bachner | first3 = P. | last4 = Howanitz | first4 = PJ. | last5 = Meier | first5 = FA. | last6 = Schifman | first6 = RB. | last7 = Boone | first7 = DJ. | last8 = Herron | first8 = RM. | title = Indications and immediate patient outcomes of pathology intraoperative consultations. College of American Pathologists/Centers for Disease Control and Prevention Outcomes Working Group Study. | journal = Arch Pathol Lab Med | volume = 120 | issue = 1 | pages = 19-25 | month = Jan | year = 1996 | doi = | PMID = 8554440 }} | ||
</ref> | </ref> | ||
#Determine diagnosis & appropriate extent of operation ~ 50%. | #Determine diagnosis & appropriate extent of operation ~ 50%. | ||
#Margins status | #[[Margins|Margin]] status ~ 15%. | ||
#Triage tissue ~ 10%. | #Triage tissue ~ 10%. | ||
#Inform family ~ 8%. | #Inform family ~ 8%. † | ||
#Sufficient tissue? ~ 8%. | #Sufficient tissue? ~ 8%. | ||
#Treatment planning, e.g. insert a portacath ~ 3%. | |||
Note: | |||
*† Some don't consider this a good reason for an IC.<ref>{{Ref BITFS|5}}</ref> | |||
===Why intraoperative consultations may be refused=== | |||
*Tissue is the issue - not enough of it. | |||
*Infectious case and no back-up cryostat. | |||
*Management - it won't make a difference. | |||
**Diagnosis won't make a difference. | |||
**Cannot make the diagnosis. | |||
***Bone tumours. | |||
==Frozen section permanent section concordance == | ==Frozen section permanent section concordance == | ||
{{Main|Quality}} | {{Main|Quality}} | ||
Categories by ADASP:<ref>URL: [http://www.adasp.org/papers/position/QualityAssurance.htm http://www.adasp.org/papers/position/QualityAssurance.htm]. Accessed on: 2 March 2012.</ref> | Categories by the ''Association of Directors of | ||
Anatomic and Surgical Pathology'' (ADASP):<ref name=adasp>URL: [http://www.adasp.org/papers/position/QualityAssurance.htm http://www.adasp.org/papers/position/QualityAssurance.htm]. Accessed on: 2 March 2012.</ref> | |||
*Agreement | *Agreement | ||
*Deferral - appropriate. | *Deferral - appropriate. | ||
| Line 23: | Line 37: | ||
==Common specimens== | ==Common specimens== | ||
Gynecologic | ===Table of common FS specimens=== | ||
*Pelvic mass - diagnosis. | {| class="wikitable sortable" | ||
*Ovarian mass - diagnosis. | ! Specimen | ||
*Uterine mass - diagnosis. | ! Indication | ||
*Sentinel lymph node - staging. | ! Subspecialty | ||
|- | |||
| Pelvic mass | |||
| diagnosis | |||
| [[gynecologic pathology]] | |||
|- | |||
| Ovarian mass | |||
| diagnosis | |||
| [[gynecologic pathology]] | |||
|- | |||
| Uterine mass | |||
| diagnosis | |||
| [[gynecologic pathology]] | |||
|- | |||
| [[Sentinel lymph node]] | |||
| staging in [[vulva]]r melanoma | |||
| [[gynecologic pathology]] | |||
|- | |||
| [[Squamous cell carcinoma]] | |||
| [[margins]] | |||
| [[head and neck pathology]] | |||
|- | |||
| [[Whipple procedure]] | |||
| margins | |||
| [[gastrointestinal pathology]] | |||
|- | |||
| Liver resection (usu. metastatic disease) | |||
| margins | |||
| gastrointestinal pathology | |||
|- | |||
| Lower anterior resection | |||
| distal margin | |||
| gastrointestinal pathology | |||
|- | |||
| Cystectomy/cystoprostatectomy | |||
| ureteral margins | |||
| [[genitourinary pathology]] | |||
|- | |||
| Pneumonectomy (usu. cancer) | |||
| bronchus margin, [[lymph nodes]] for staging | |||
| [[pulmonary pathology]] | |||
|- | |||
| [[Brain tumour]] | |||
| diagnosis | |||
| [[neuropathology]] | |||
|- | |||
| Spinal tumour | |||
| diagnosis | |||
| [[neuropathology]] | |||
|- | |||
| Thyroid nodule | |||
| diagnosis | |||
| [[endocrine pathology]] | |||
|- | |||
| Prosthetic joint | |||
| query [[prosthetic joint infection]] | |||
| [[joints|joint pathology]] | |||
|- | |||
| Parathyroid gland | |||
| identify parathyroid gland | |||
| [[endocrine pathology]] | |||
|} | |||
===List of specimens=== | |||
====Gynecologic==== | |||
*Pelvic mass - diagnosis (benign/borderline/malignant). | |||
*Ovarian mass - diagnosis (benign/borderline/malignant). | |||
*Uterine mass - diagnosis (benign/borderline/malignant). | |||
*[[Sentinel lymph node]] - staging. | |||
**[[Vulva]]r melanoma. | **[[Vulva]]r melanoma. | ||
Head and neck | ====Head and neck==== | ||
*Squamous cell carcinoma - margins. | *Squamous cell carcinoma - margins. | ||
*Thyroid nodule - diagnosis. | |||
*Parathyroid - confirm it is parathyroid. | |||
Gastrointestinal tract | ====Gastrointestinal tract==== | ||
*Whipple procedure - margins. | *Whipple procedure - margins. | ||
*Liver resection - margins. | *Liver resection - margins. | ||
*Lower anterior resection - distal margin. | *Lower anterior resection - distal margin. | ||
Genitourinary tract | ====Genitourinary tract==== | ||
* | *Cystoprostatectomy/cystectomy - ureteral margins. | ||
Pulmonary | ====Pulmonary==== | ||
*Pneumonectomy: | *Pneumonectomy: | ||
**Bronchus - margins. | **Bronchus - margins. | ||
**Lymph nodes - staging. | **[[Lymph nodes]] - staging. | ||
Neurologic | ====Neurologic==== | ||
*Brain tumour - diagnosis. | *[[Brain tumour]] - diagnosis. | ||
*Spinal tumour - diagnosis. | *Spinal tumour - diagnosis. | ||
Thyroid gland: | ====Prosthetic joint==== | ||
* | *Query [[prosthetic joint infection]]. | ||
==Surgeon-pathologist dialog== | |||
It should include: | |||
# Identification: | |||
#* [[Pathology]] is calling - Dr. X is speaking. | |||
#* Patient identifiers - full name. | |||
#* Part(s) submitted. | |||
# [[Diagnosis]]. | |||
# Repeat of diagnosis from surgeon (known as ''read-back confirmation''<ref name=pmid22032564>{{Cite journal | last1 = Nakhleh | first1 = RE. | title = Quality in surgical pathology communication and reporting. | journal = Arch Pathol Lab Med | volume = 135 | issue = 11 | pages = 1394-7 | month = Nov | year = 2011 | doi = 10.5858/arpa.2011-0192-RA | PMID = 22032564 | URL = http://www.archivesofpathology.org/doi/full/10.5858/arpa.2011-0192-RA }}</ref>). | |||
# Additional requests? | |||
==Specific specimens - checklists== | |||
===Ovarian mass=== | |||
:Covers ''adnexal mass'' and ''pelvic mass''. | |||
====Checklist==== | |||
General: | |||
*Specimen integrity: fragmented/intact/ruptured. | |||
*Dimensions: ___ x ___ x ___ cm. | |||
*Mass: ___ grams. | |||
*Surface involvement: absent/present. | |||
*Consistency: solid/cystic/solid and cystic. | |||
Cystic: | |||
*Type: unilocular, multilocular. | |||
*Cyst content: mucinous/serous/hemorrhagic/purulent/chylous/other. ‡ | |||
*Papillary excrescences: absent/present. | |||
*Necrosis: absent/present. | |||
*Hair: absent/present. | |||
Sections: | |||
*Sample morphologically distinct areas - esp. solid areas, papillary excrescences. | |||
Notes: | |||
*‡ Mucinous versus serous: | |||
**Serous: low viscosity (flows with ease threw the grates typically seen at the bottom of sinks<ref>{{Ref BITFS|33}}</ref>). | |||
**Mucinous: high viscosity (jello-like consistency). | |||
====DDx==== | |||
{| class="wikitable sortable" | |||
! Feature | |||
! Dx/DDx | |||
! Notes | |||
|- | |||
| Unilocular cysts | |||
| follicular cyst, epithelial cyst, very rarely [[granulosa cell tumour]] (not typically diagnosed at FS) | |||
| no excrescences or solid areas dx = "simple cyst"; "shag carpet" appearance = serous borderline tumour | |||
|- | |||
| Sebaceous material ''or'' hair | |||
| [[teratoma]] | |||
| ''Rokitansky nodule'' present -> submit section; neuroepithelium = fleshy appearance on gross;<ref>{{Ref BITFS|34}}</ref> | |||
''immature teratoma'' not typically diagnosed at FS | |||
|- | |||
| Chocolate cyst | |||
| [[endometriosis]] | |||
| solid elements (fibrosis vs. clear cell & endometrioid carcinoma | |||
|} | |||
===Endometrial carcinoma=== | |||
===General=== | |||
*Diagnosis usually known before the surgery. | |||
*The IC revolves around whether the lesion has a "high risk" of [[lymph node metastasis]]. | |||
Factors that increase the risk of lymph node metastases:<ref>{{Ref BITFS|43}}</ref> | |||
*Histology: | |||
**Serous or clear cell. | |||
**FIGO grade 3. | |||
*Staging parameters - involvement of: | |||
**Outer half of the myometrium. | |||
**Uterine cervix. | |||
**Adnexa. | |||
===Checklist=== | |||
Gross assessment: | |||
*Uterine cervix involvement (rare). | |||
*Adnexal involvement (rare). | |||
*Myometrial involvement - after sectioning bivalving and sectioning (with a 5 mm interval). | |||
===Parathyroid gland and thyroid gland=== | |||
{{Main|Parathyroid gland}} | |||
Possibilities: | |||
*Parathyroid gland: | |||
**Benign parathyroid gland. | |||
**[[Parathyroid adenoma]]. † | |||
**[[Parathyroid hyperplasia]]. † | |||
**[[Parathyroid carcinoma]]. | |||
*Thyroid gland. | |||
**Thyroid usually follicular - though parathyroid occasionally is pseudofollicular. | |||
**Thyroid often has birefringent (calcium oxalate) crystals (60 of 80 cases) whereas parathyroid less often does (2 or 20 cases).<ref name=pmid24618617>{{cite journal |authors=Wong KS, Lewis JS, Gottipati S, Chernock RD |title=Utility of birefringent crystal identification by polarized light microscopy in distinguishing thyroid from parathyroid tissue on intraoperative frozen sections |journal=Am J Surg Pathol |volume=38 |issue=9 |pages=1212–9 |date=September 2014 |pmid=24618617 |doi=10.1097/PAS.0000000000000204 |url=}}</ref> | |||
*[[Lymph node]]. | |||
*Fibroadipose tissue. | |||
*[[Paraganglioma]]. | |||
Notes: | |||
* † It is ''not'' possible to determine which one without history ''or'' all parathyroid glands. | |||
* Surgeons are pretty good at identifying parathyroid tissue ~ 94% accurate in one series.<ref name=pmid16360503>{{Cite journal | last1 = Dewan | first1 = AK. | last2 = Kapadia | first2 = SB. | last3 = Hollenbeak | first3 = CS. | last4 = Stack | first4 = BC. | title = Is routine frozen section necessary for parathyroid surgery? | journal = Otolaryngol Head Neck Surg | volume = 133 | issue = 6 | pages = 857-62 | month = Dec | year = 2005 | doi = 10.1016/j.otohns.2005.05.001 | PMID = 16360503 }}</ref> | |||
====Checklist==== | |||
*Weight. | |||
*Dimensions. | |||
*Appearance. | |||
====Sign out==== | |||
<pre> | |||
Query Parathyroid Gland: | |||
- Hypercellular parathyroid tissue. | |||
</pre> | |||
<pre> | |||
QUERY PARATHYROID GLAND: | |||
- PARATHYROID GLAND. | |||
</pre> | |||
===Whipple specimen=== | |||
====Sign out==== | |||
<pre> | |||
BILE DUCT MARGIN: | |||
- NEGATIVE FOR MALIGNANCY. | |||
</pre> | |||
===Skin specimens=== | |||
{{Main|Oriented skin ellipse grossing}} | |||
{{Main|Unoriented skin ellipse grossing}} | |||
{{Main|Grossing separately received oriented margins for a skin ellipse}} | |||
[[Cut-up]] at frozen section depends on how the specimen is received and its size. | |||
* | *Small skin specimens: the standard grossing procedure for fixed specimens. | ||
*Large skin specimens: inking is typically as per the routine process. It is useful to mark non-margin if the nearest margin is taken [[en face margin|en face]]. | |||
*Oriented margins should be grossed in a way that allows orientation by [[ink]]. Ideally, ink should allow one to identify the different specimens. See ''[[Grossing separately received oriented margins for a skin ellipse|grossing separately received oriented margins for a skin ellipse]]''. | |||
==See also== | ==See also== | ||
| Line 60: | Line 270: | ||
==References== | ==References== | ||
{{Reflist| | {{Reflist|2}} | ||
[[Category:Basics]] | [[Category:Basics]] | ||
Latest revision as of 16:15, 15 December 2023
Intraoperative consultation, also quick section and frozen section, is when a surgeon requests an opinion during an operation so that they can appropriately manage a patient. It is abbreviated IC. Frozen section is often abbreviated FS.
Why intraoperative consultations are done
Reasons why IC are done:[1]
- Determine diagnosis & appropriate extent of operation ~ 50%.
- Margin status ~ 15%.
- Triage tissue ~ 10%.
- Inform family ~ 8%. †
- Sufficient tissue? ~ 8%.
- Treatment planning, e.g. insert a portacath ~ 3%.
Note:
- † Some don't consider this a good reason for an IC.[2]
Why intraoperative consultations may be refused
- Tissue is the issue - not enough of it.
- Infectious case and no back-up cryostat.
- Management - it won't make a difference.
- Diagnosis won't make a difference.
- Cannot make the diagnosis.
- Bone tumours.
Frozen section permanent section concordance
Main article: Quality
Categories by the Association of Directors of Anatomic and Surgical Pathology (ADASP):[3]
- Agreement
- Deferral - appropriate.
- Deferral – inappropriate
- Recommendation <=10% threshold.
- Disagreement – Minor.
- Disagreement – Major.
- Recommendation <=3% threshold.
Common specimens
Table of common FS specimens
| Specimen | Indication | Subspecialty |
|---|---|---|
| Pelvic mass | diagnosis | gynecologic pathology |
| Ovarian mass | diagnosis | gynecologic pathology |
| Uterine mass | diagnosis | gynecologic pathology |
| Sentinel lymph node | staging in vulvar melanoma | gynecologic pathology |
| Squamous cell carcinoma | margins | head and neck pathology |
| Whipple procedure | margins | gastrointestinal pathology |
| Liver resection (usu. metastatic disease) | margins | gastrointestinal pathology |
| Lower anterior resection | distal margin | gastrointestinal pathology |
| Cystectomy/cystoprostatectomy | ureteral margins | genitourinary pathology |
| Pneumonectomy (usu. cancer) | bronchus margin, lymph nodes for staging | pulmonary pathology |
| Brain tumour | diagnosis | neuropathology |
| Spinal tumour | diagnosis | neuropathology |
| Thyroid nodule | diagnosis | endocrine pathology |
| Prosthetic joint | query prosthetic joint infection | joint pathology |
| Parathyroid gland | identify parathyroid gland | endocrine pathology |
List of specimens
Gynecologic
- Pelvic mass - diagnosis (benign/borderline/malignant).
- Ovarian mass - diagnosis (benign/borderline/malignant).
- Uterine mass - diagnosis (benign/borderline/malignant).
- Sentinel lymph node - staging.
- Vulvar melanoma.
Head and neck
- Squamous cell carcinoma - margins.
- Thyroid nodule - diagnosis.
- Parathyroid - confirm it is parathyroid.
Gastrointestinal tract
- Whipple procedure - margins.
- Liver resection - margins.
- Lower anterior resection - distal margin.
Genitourinary tract
- Cystoprostatectomy/cystectomy - ureteral margins.
Pulmonary
- Pneumonectomy:
- Bronchus - margins.
- Lymph nodes - staging.
Neurologic
- Brain tumour - diagnosis.
- Spinal tumour - diagnosis.
Prosthetic joint
- Query prosthetic joint infection.
Surgeon-pathologist dialog
It should include:
- Identification:
- Pathology is calling - Dr. X is speaking.
- Patient identifiers - full name.
- Part(s) submitted.
- Diagnosis.
- Repeat of diagnosis from surgeon (known as read-back confirmation[4]).
- Additional requests?
Specific specimens - checklists
Ovarian mass
- Covers adnexal mass and pelvic mass.
Checklist
General:
- Specimen integrity: fragmented/intact/ruptured.
- Dimensions: ___ x ___ x ___ cm.
- Mass: ___ grams.
- Surface involvement: absent/present.
- Consistency: solid/cystic/solid and cystic.
Cystic:
- Type: unilocular, multilocular.
- Cyst content: mucinous/serous/hemorrhagic/purulent/chylous/other. ‡
- Papillary excrescences: absent/present.
- Necrosis: absent/present.
- Hair: absent/present.
Sections:
- Sample morphologically distinct areas - esp. solid areas, papillary excrescences.
Notes:
- ‡ Mucinous versus serous:
- Serous: low viscosity (flows with ease threw the grates typically seen at the bottom of sinks[5]).
- Mucinous: high viscosity (jello-like consistency).
DDx
| Feature | Dx/DDx | Notes |
|---|---|---|
| Unilocular cysts | follicular cyst, epithelial cyst, very rarely granulosa cell tumour (not typically diagnosed at FS) | no excrescences or solid areas dx = "simple cyst"; "shag carpet" appearance = serous borderline tumour |
| Sebaceous material or hair | teratoma | Rokitansky nodule present -> submit section; neuroepithelium = fleshy appearance on gross;[6]
immature teratoma not typically diagnosed at FS |
| Chocolate cyst | endometriosis | solid elements (fibrosis vs. clear cell & endometrioid carcinoma |
Endometrial carcinoma
General
- Diagnosis usually known before the surgery.
- The IC revolves around whether the lesion has a "high risk" of lymph node metastasis.
Factors that increase the risk of lymph node metastases:[7]
- Histology:
- Serous or clear cell.
- FIGO grade 3.
- Staging parameters - involvement of:
- Outer half of the myometrium.
- Uterine cervix.
- Adnexa.
Checklist
Gross assessment:
- Uterine cervix involvement (rare).
- Adnexal involvement (rare).
- Myometrial involvement - after sectioning bivalving and sectioning (with a 5 mm interval).
Parathyroid gland and thyroid gland
Main article: Parathyroid gland
Possibilities:
- Parathyroid gland:
- Benign parathyroid gland.
- Parathyroid adenoma. †
- Parathyroid hyperplasia. †
- Parathyroid carcinoma.
- Thyroid gland.
- Thyroid usually follicular - though parathyroid occasionally is pseudofollicular.
- Thyroid often has birefringent (calcium oxalate) crystals (60 of 80 cases) whereas parathyroid less often does (2 or 20 cases).[8]
- Lymph node.
- Fibroadipose tissue.
- Paraganglioma.
Notes:
- † It is not possible to determine which one without history or all parathyroid glands.
- Surgeons are pretty good at identifying parathyroid tissue ~ 94% accurate in one series.[9]
Checklist
- Weight.
- Dimensions.
- Appearance.
Sign out
Query Parathyroid Gland: - Hypercellular parathyroid tissue.
QUERY PARATHYROID GLAND: - PARATHYROID GLAND.
Whipple specimen
Sign out
BILE DUCT MARGIN: - NEGATIVE FOR MALIGNANCY.
Skin specimens
Main article: Oriented skin ellipse grossing
Main article: Unoriented skin ellipse grossing
Cut-up at frozen section depends on how the specimen is received and its size.
- Small skin specimens: the standard grossing procedure for fixed specimens.
- Large skin specimens: inking is typically as per the routine process. It is useful to mark non-margin if the nearest margin is taken en face.
- Oriented margins should be grossed in a way that allows orientation by ink. Ideally, ink should allow one to identify the different specimens. See grossing separately received oriented margins for a skin ellipse.
See also
References
- ↑ Zarbo, RJ.; Schmidt, WA.; Bachner, P.; Howanitz, PJ.; Meier, FA.; Schifman, RB.; Boone, DJ.; Herron, RM. (Jan 1996). "Indications and immediate patient outcomes of pathology intraoperative consultations. College of American Pathologists/Centers for Disease Control and Prevention Outcomes Working Group Study.". Arch Pathol Lab Med 120 (1): 19-25. PMID 8554440.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 5. ISBN 978-0781767798.
- ↑ URL: http://www.adasp.org/papers/position/QualityAssurance.htm. Accessed on: 2 March 2012.
- ↑ Nakhleh, RE. (Nov 2011). "Quality in surgical pathology communication and reporting.". Arch Pathol Lab Med 135 (11): 1394-7. doi:10.5858/arpa.2011-0192-RA. PMID 22032564.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 33. ISBN 978-0781767798.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 34. ISBN 978-0781767798.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 43. ISBN 978-0781767798.
- ↑ Wong KS, Lewis JS, Gottipati S, Chernock RD (September 2014). "Utility of birefringent crystal identification by polarized light microscopy in distinguishing thyroid from parathyroid tissue on intraoperative frozen sections". Am J Surg Pathol 38 (9): 1212–9. doi:10.1097/PAS.0000000000000204. PMID 24618617.
- ↑ Dewan, AK.; Kapadia, SB.; Hollenbeak, CS.; Stack, BC. (Dec 2005). "Is routine frozen section necessary for parathyroid surgery?". Otolaryngol Head Neck Surg 133 (6): 857-62. doi:10.1016/j.otohns.2005.05.001. PMID 16360503.