Dermatologic neoplasms
This article deals with dermatologic neoplasms. It includes dermatologic cancer, which can be deadly. Collectively, dermatologic cancers are the most common form of cancer.
An introduction to dermatopathy is found in the dermatopathology article. Non-malignant disease is covered in the non-malignant skin disease article.
The Big Three malignant
Basal cell carcinoma
Squamous cell carcinoma of the skin
- Abbreviated skin SCC, SCC of the skin, and SCC of skin.
General
Precursor:[1]
- Actinic keratosis (solar keratosis).
- Clinical: yellow-brown scaly, patches, sandpaper sensation.
Risk factors:[1]
- Sun exposure.
- Immune suppression (e.g. organ transplant recipients).
Notes:
- Keratoacanthoma.
- Some don't believe this entity exists.
- These people sign this entity as low grade squamous cell carcinoma, keratoacanthoma type.[2]
- Some don't believe this entity exists.
Microscopic
High risk features - for SCC of the skin:[3]
- Primary site is ear or lip.†
- Clark level IV/V = reticular dermis or deeper.
- >=2 mm thickness -- measured from granular layer (stratum granulosum) or ulcer base to deepest aspect.
- Lymphovascular invasion.
- Perineural invasion.
- Poorly differentiated.
Note:
- † The words used are "hair-bearing lip" - but there is considerable confusion about this as the AJCC manual contradicts itself.[4]
DDx:
- Inverted follicular keratosis.
- Bowen disease.
- Malignant melanoma.
- Paget disease of the breast.
- Eccrine carcinoma
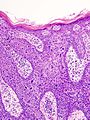
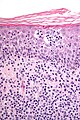
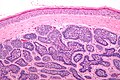
Bowen disease
Bowen disease is squamous cell carcinoma in situ of the skin.
- Its histomorphologic appearance may be similar to Paget disease of the breast/Extramammary Paget disease, Toker cell hyperplasia and melanoma.
- IHC is used to separate the entities definitively.
Histologic DDx of Bowen disease:
- Benign Toker cell hyperplasia.
- Malignant melanoma.
- Paget disease of the breast.
- Eccrine carcinoma.
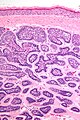
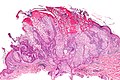
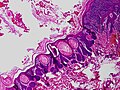
Images
IHC
Bowen's disease panel:
- CK5/6 +ve.[5]
- Usu. -ve in Paget disease of the breast/Extramammary Paget disease.
- S100 -ve, HMB-45 -ve.
- Both typically +ve in melanoma.
- CEA -ve[6] (+ve in Paget disease of the breast/Extramammary Paget disease, -ve in Toker cells).
- CK7 -ve.
- Toker cells CK7 +ve.[7]
Sign-out
Invasive SCC
SKIN, SITE, BIOPSY: - MODERATELY-DIFFERENTIATED INVASIVE SQUAMOUS CELL CARCINOMA, SEE COMMENT. - NEGATIVE FOR LYMPHOVASCULAR INVASION. - NEGATIVE FOR PERINEURAL INVASION. COMMENT: The nearest margin (lateral margin) is 1 mm. The tumour is 9 mm in maximal dimension.
SKIN LESION, SITE, EXCISION: - INVASIVE SQUAMOUS CELL CARCINOMA, MODERATELY-DIFFERENTIATED. -- TUMOUR GREATEST DIMENSION: ___ CM. -- TUMOUR THICKNESS: ___ MM. -- LATERAL MARGINS: NEGATIVE FOR IN SITU CARCINOMA AND INVASIVE CARCINOMA. -- DEEP MARGIN: NEGATIVE FOR INVASIVE CARCINOMA. -- NEAREST MARGIN: 1 MM, LATERAL MARGIN. -- NEGATIVE FOR LYMPHOVASCULAR INVASION. -- NEGATIVE FOR PERINEURAL INVASION. - EXTENSIVE SOLAR ELASTOSIS.
SKIN, SITE, BIOPSY: - INVASIVE SQUAMOUS CELL CARCINOMA, SEE TUMOUR SUMMARY. TUMOUR SUMMARY: Histologic type: squamous cell carcinoma, type not otherwise specified. Histologic grade: moderately differentiated. Greatest dimension: ___ cm. Tumour thickness: ___ mm. Peripheral margin: negative for invasive carcinoma and in situ carcinoma. Deep margin (invasive component): negative for invasive carcinoma. Closest margin: deep margin, ___ mm. Lymphovascular invasion: not identified. Perineural invasion: not identified.
Bowen's disease
SKIN LESION, RIGHT EAR, BIOPSY: - SQUAMOUS CELL CARCINOMA IN SITU (BOWEN'S DISEASE), INCOMPLETELY EXCISED. COMMENT: Complete excision of the lesion is recommended.
SKIN LESION, CHEST, EXCISIONAL BIOPSY: - SQUAMOUS CELL CARCINOMA IN SITU (BOWEN'S DISEASE), COMPLETELY EXCISED. - SOLAR ELASTOSIS, MILD.
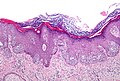
Micro
The sections show hair bearing skin. The squamous epithelium has full thickness changes including an increased nuclear-cytoplasmic ratio, loss of polarity, and nuclear hyperchromasia. Mitoses are seen in the upper third of the epithelium. Nucleoli are not apparent. No atypical cells are seen in the dermis. Parakeratosis overlies the abnormal keratinocytes. Solar elastosis is present. No melanocytic nests are identified.
Melanoma
- Known as the great mimicker in pathology; it may look like many things.
Less common malignant
Dermatofibrosarcoma protuberans
- Abbreviated DFSP.
Cutaneous B-cell lymphoma
- Abbreviated CBCL.
General
- CBCL is less common than cutaneous T-cell lymphoma (CTCL).[8]
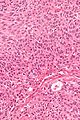
Microscopic
Features:
- Dermal lymphoid infiltrate.
- "Grenz zone" - space between the epidermis and the dermal infiltrate - key feature.
IHC
- B cell and T cell markers.
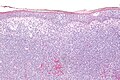
Cutaneous T-cell lymphoma
- Abbreviated CTCL.
General
- Mycosis fungoides - is a subtype (???).
- CTCL is more common than cutaneous B-cell lymphoma (CBCL).[9][10]
Stages - like Kaposi sarcoma:
- Patch.
- Plaque.
- Nodular.
Microscopic
- Atypical lymphocytes:
- Have folded "cerebriform" nuclei; Sezary-Lutzner cells.[11]
- Grouping:
- Nests in the epidermis - known as "Pautrier microabscesses".
- Single lymphocytes in epidermis - without accompanying edema.
- Short linear arrays of lymphocytes along the basal layer of the epidermis; "epidermotropism".[11]
DDx:
Images
www:
IHC
Key stain:
- CD4 +ve.[12]
Other stains:
- CD3 +ve.
- CD8 -ve.
- CD20 -ve (to r/o significant B cell population).
- CD30 -ve.
- CD5 +ve.
- CD7 -ve (often lost first in T cell lymphomas).
- Ki-67 high.
- CD56 -ve.
Merkel cell carcinoma
Eccrine carcinoma
General
- Arises from the proximal sweat duct.
Microscopic
Features:
- Pleomorphic nuclei with nucleoli.
- Duct-like structures - key feature.
- Extends from dermis into epidermis (follows path of a benign sweat duct).
Notes:
- May resemble Extramammary Paget's disease/Paget's disease of the breast.
Kaposi sarcoma
- See Kaposi sarcoma.
Sebaceous carcinoma
Microcystic adnexal carcinoma
Trichilemmal carcinoma
General
- Super rare.
- Not well-described.
Microscopic
Features:[13]
- Clear (glycogen-rich) cytoplasm in center of lesion.
- Peripheral palisading at edge of lesion - root sheath differentiation (hair follicle).
- Contiguous with hair follicle or assoc. with trichilemmoma.
DDx:
- Squamous cell carcinoma, clear cell variant.
- Basal cell carcinoma, clear cell variant.
- Trichilemmoma.
Lymphomatoid papulosis
General
- Rare.
- Benign behaviour.
Microscopic
Features:
- Dermal lymphocytosis.
- No epidermal lymphocytes.
- Focal nuclear atypia.
DDx:
IHC
- CD30 +ve.[14]
Rare malignant
Basosquamous carcinoma
- Should not be confused with basaloid squamous cell carcinoma (AKA squamous cell carcinoma, basaloid variant).
General
- Very rare.
- Largest case series, as of 2000, 35 cases.[15]
- May be considered an aggressive variant of basal cell carcinoma.[15]
- Aggressive behaviour.[16]
Microscopic
Features:
- Has features of both basal cell carcinoma and squamous cell carcinoma.[16]
- BCC component usually predominant.[17]
Note:
- Busam notes that there is disagreement about what defines this tumour;[18] however, he goes on the describe it as a collision tumour.[17]
DDx:
- Basaloid squamous cell carcinoma.
- Basal cell carcinoma with squamous differentiation.
Intermediate
Atypical fibroxanthoma
- Abbreviated AFX.
General
- Typically head & neck region.[19]
- Thought to be related to pleomorphic undifferentiated sarcoma;[20][21] some say it is the same thing.[22]
- Usually benign.
- May metastasize - case report-type of occurrence.[23]
Clinical:
- Rapid growth.
- Elderly.
- Good prognosis.[24]
Microscopic
Features:[25]
- Dermal lesion - key point.
- Marked nuclear atypia.
- Mitoses.
- Mulitnucleated cells.
- Foamy cytoplasm - key feature.
DDx:
- Melanoma.
- Pleomorphic undifferentiated sarcoma (MFH) - deeper than the dermis.
- Leiomyosarcoma.
- Sarcomatoid squamous carcinoma.
Notes:
- No Grenz zone. (???)
Image:
IHC
Features:[25]
- S100 -ve (done to r/o melanoma).
- 34betaE12 -ve.
- p63 -ve (done to exclude SCC)
- Scant staining not considered +ve.
- Desmin -ve (done to r/o leiomyosarcoma).
Sign out
Incompletely excised
SKIN LESION, MID BACK, SHAVE BIOPSY: - ATYPICAL SPINDLE CELL NEOPLASM, SEE MICRO AND COMMENT. COMMENT: The diagnosis of atypical fibroxanthoma (AFX) is favoured. The main differential diagnosis is pleomorphic undifferentiated sarcoma. The extent of the lesion cannot be determined, as it is present at the deep margin. This lesion should be re-excised, as it could represent an aggressive malignancy.
Benign
Syringoma
General
- Benign sweat duct tumour.
- Eccrine differentiation.
- Usually close to lower eyelid.[27]
Microscopic
Features:[28]
- Proliferation of benign ducts with lined by a bilayer (as in normal sweat ducts) with abnormal architecture:
- Tadpole like appearing ducts.
DDx:
- Syringomatous adenomas of nipple (AKA syringoma of the nipple).[29]
- Chondroid syringoma. (???)
Images:
Chondroid syringoma
- Used to be called mixed tumour of skin.[31]
General
- Mixed apocrine & eccrine tumour of skin, usually in the head & neck[31], especially nose and cheek.[32]
- May be in major and minor salivary glands.[32]
Microscopic
Features:
- Mix tumour with:[31]
- Epithelial component:
- Nests of cells with:
- Moderate dull eosinophilic cytoplasm.
- Round/ovoid nuclei with nucleoli.
- Nests of cells with:
- Mesenchymal component - key feature:
- Epithelial component:
Images:
Dermal cylindroma
General
- Benign skin lesion.
- Occasionally malignant.[34]
- Should not be confused with cylindroma (adenoid cystic carcinoma).
- May be related to eccrine spiradenoma.[35][36]
May be familial:[34]
- Familial cylindromatosis (autosomal dominant).
- Brook–Spiegler syndrome.
Gross
- Classically scalp - usually head and neck or face.
Microscopic
Features:[34]
- Nests of cells that fit together like a jigsaw puzzle - the borders of the nests are opposed and undulate.
- Basaloid cells with scant cytoplasm and dark nuclei palisade around the edge of the nests.
- Larger cells with moderate eosinophilic cytoplasm and lighter staining nuclei are at the centre of the nests.
- Cells nests surrounded by a band of hyaline (i.e. glassy, eosinophilic, acellular) material ~ 2X thickness of a basilar cell - key feature.
- This is basement membrane.
DDx:
Images
www:
Stains
- PAS +ve (basement membrane).[34]
Keratoacanthoma
Sebaceous adenoma
General
- Seen in Muir-Torre syndrome - a variant of Lynch syndrome (hereditary non-polyposis colon cancer).
Notes:
- Sebaceous lesions (from benign to malignant): sebaceous hyperplasia, sebaceous adenoma, sebaceoma, sebaceous carcinoma.
Microscopic
Features:
- Abnormal sebaceous glands (pale fluffy cytoplasm):
- Increased basal epithelium.
- Multiple dilated glands - opening to the surface.
Images
www:
Trichilemmoma
- May be spelled tricholemmoma.
General
- Benign neoplasm with features of the pilosebaceous follicular epithelium.[37]
- Associated with nevus sebaceous.[38]
- Muliple trichilemmomas associated with Cowden syndrome.[39]
Microscopic
Features:[39]
- Superficial dermal lesion contiguous with the epidermis:
- Core of lesion:
- Cuboidal cells with round nuclei, eosinophilic-clear cytoplasm.
- Periphery of lesion:
- Surrounded by hyaline band.
- Peripheral palisading.
- Core of lesion:
DDx:
Images:
- Trichilemmoma - low mag. (cancer.gov).[40]
- Trichilemmoma - high mag. (cancer.gov).[40]
- Trichilemmoma (jhmi.edu).[41]
- Trichilemmoma - low mag. (flickr.com/Irlam).
- Trichilemmoma - intermed. mag. (flickr.com/Irlam).
- Trichilemmoma - high mag. (flickr.com/Irlam).
Eccrine poroma
General
- Benign tumour arising from the distal sweat duct.
- Erythematous - gross.
Microscopic
Features:[42]
- Broad sheets of basaloid cells - attached to the epidermis - containing ductal structures - key feature.
- Biphasic stroma:
- Edematous stroma.
- Sclerotic stroma.
- Moderate nuclear pleomorphism.
- +/-Occasional mitoses.
Notes:
- Area above gland appears crusted.
DDx:
Images:
Nodular hidradenoma
General
- Benign adnexal tumour.[44]
Typical locations:[43]
- Scalp.
- Face.
- Trunk, anterior.
Microscopic
Features:[44]
- Well-circumscribed dermal lesions with:
- Back-to-back nests with a whorled appearance.
- Spaces between cells.
- Nuclei ovoid and centrally placed in the cell.
- No nucleolus.
- Cystic spaces with degenerated cells.
DDx:
Images
IHC
Features:[44]
- CAM5.2 +ve.
- AE1/AE3 +ve.
- EMA +ve.
- S100 -ve.
- Desmin -ve.
Trichoblastoma
Trichofolliculoma
General
- Benign.
Microscopic
Features:[45]
- Irregular hair follicle (basilar nest of cells with an acellular hair shaft) with:
- Smaller satellites (follicles) consisting of well-circumscribed basilar cells.
Note:
- Lack artificial clefting between the (basilar) nests and stroma (seen in BCC).
- Surrounding stroma does not have a basophilic tingle (seen in BCC).
DDx:
Images
www:
Apocrine carcinoma of the skin
General
Microscopic
Features:[46]
- Nests.
- Apocrine snouts - "decapitation secretion"
DDx:
Images
Stains
Features:[46]
- PAS +ve.
- PASD +ve.
IHC
- GCDFP-15 (gross cystic disease fluid protein-15) +ve.[46]
Dermatomyofibroma
- Should not be confused with dermatofibroma.
- Abbreviated DMF.
General
- Uncommon.
Microscopic
Features:[47]
- Poorly formed fasicles parallel to the skin surface, usu. restricted to the superficial dermis.
- Moderate cellular density - less cellular than DFSP.
- Eosinophilic cytoplasm.
DDx:
Images:
IHC
Features:[47]
- CD10 +ve.
- Vimentin +ve.
Others:[47]
- CD34 -ve.
- Factor XIIIa -ve.
- S-100 -ve.
Papillary eccrine adenoma
- Abbreviated PEA.
General
- Uncommon.
- Benign.[48]
Treatment:
- Excision.[49]
Gross
- Central location.
Note:
- The digital papillary adenoma is considered malignant; the AFIP says these are best classified as adenocarcinomas, i.e. digital papillary adenocarcinoma.[50]
Microscopic
- Well-circumscribed lesions consisting of multiple cystic spaces lined by a bilayered epithelium with:
- Papillary projections into the lumen.
- Amorphous eosinophilic material in the cystic spaces.
- Surrounded by a fibrous stroma.[53]
Note:
- May appear to have more than two cell layers.
DDx:
- Digital papillary adenocarcinoma - location important.
- Tubular apocrine adenoma (tubulopapillary hidradenoma[54]) - a related tumour.[55]
Image:
IHC
Outer layer of epithelium:[53]
- SMA-alpha +ve.
- Keratin 14 +ve.
Inner layer of epithelium:[53]
- Keratin 8 +ve.
Other stains:[52]
- Vimentin +ve.
- CEA +ve.
- EMA +ve.
- S-100 +ve.
Sign out
SKIN LESION, LEFT PARIETAL SCALP, BIOPSY: - PAPILLARY ECCRINE ADENOMA.
Micro
The sections show a well-circumscribed multi-locular superficial dermal lesion with a bilayered epithelium and intracystic papillary projections. The cystic spaces contain amorphous eosinophilic material. The cystic component is surrounded by a dense fibrous stroma with a mixed inflammatory infiltrate, consisting primary of plasma cells and lymphocytes.
There is no significant nuclear atypia and no mitotic activity is appreciated. The overlying epidermis matures appropriately. A granular layer is present.
See also
References
- ↑ 1.0 1.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1180. ISBN 978-1416031215.
- ↑ RS. 17 May 2010.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/SkinSquamousCell_11protocol.pdf. Accessed on: 29 March 2012.
- ↑ Buethe, D.; Warner, C.; Miedler, J.; Cockerell, CJ. (2011). "Focus Issue on Squamous Cell Carcinoma: Practical Concerns Regarding the 7th Edition AJCC Staging Guidelines.". J Skin Cancer 2011: 156391. doi:10.1155/2011/156391. PMC 2990020. PMID 21151529. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2990020/.
- ↑ RS. May 2010.
- ↑ URL: http://emedicine.medscape.com/article/1101235-workup#a0721. Accessed on: 2 September 2011.
- ↑ Nofech-Mozes, S.; Hanna, W.. "Toker cells revisited.". Breast J 15 (4): 394-8. doi:10.1111/j.1524-4741.2009.00743.x. PMID 19601945.
- ↑ URL: http://emedicine.medscape.com/article/1099540-overview. Accessed on: 24 August 2010.
- ↑ URL: http://emedicine.medscape.com/article/1099540-overview. Accessed on: 24 August 2010.
- ↑ URL: http://emedicine.medscape.com/article/1098342-overview. Accessed on: 24 August 2010.
- ↑ 11.0 11.1 Klatt, Edward C. (2006). Robbins and Cotran Atlas of Pathology (1st ed.). Saunders. pp. 385. ISBN 978-1416002741.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1185. ISBN 978-1416031215.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 399-400. ISBN 978-0443066542.
- ↑ URL: http://path.upmc.edu/cases/case513/dx.html. Accessed on: 25 January 2012.
- ↑ 15.0 15.1 Martin, RC.; Edwards, MJ.; Cawte, TG.; Sewell, CL.; McMasters, KM. (Mar 2000). "Basosquamous carcinoma: analysis of prognostic factors influencing recurrence.". Cancer 88 (6): 1365-9. PMID 10717618.
- ↑ 16.0 16.1 Bowman, PH.; Ratz, JL.; Knoepp, TG.; Barnes, CJ.; Finley, EM. (Aug 2003). "Basosquamous carcinoma.". Dermatol Surg 29 (8): 830-2; discussion 833. PMID 12859383..
- ↑ 17.0 17.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 397. ISBN 978-0443066542.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 372. ISBN 978-0443066542.
- ↑ URL: http://emedicine.medscape.com/article/1056204-overview. Accessed on 2 September 2011.
- ↑ Withers, AH.; Brougham, ND.; Barber, RM.; Tan, ST. (Jun 2011). "Atypical fibroxanthoma and malignant fibrous histiocytoma.". J Plast Reconstr Aesthet Surg. doi:10.1016/j.bjps.2011.05.004. PMID 21664889.
- ↑ Tchernev, G.; Tronnier, M.; Ananiev, J.; Taneva, T.; Patterson, JW.; Gulubova, M.; Trafeli, JP.; Gegova, A. et al. (Aug 2013). "Atypical fibroxanthoma-a diagnosis of exclusion!". Wien Med Wochenschr 163 (15-16): 380-386. doi:10.1007/s10354-012-0173-1. PMID 23319144.
- ↑ Ghazarian, Danny; 16 September 2011.
- ↑ New, D.; Bahrami, S.; Malone, J.; Callen, JP. (Dec 2010). "Atypical fibroxanthoma with regional lymph node metastasis: report of a case and review of the literature.". Arch Dermatol 146 (12): 1399-404. doi:10.1001/archdermatol.2010.206. PMID 20713774.
- ↑ Beer, TW.; Drury, P.; Heenan, PJ. (Aug 2010). "Atypical fibroxanthoma: a histological and immunohistochemical review of 171 cases.". Am J Dermatopathol 32 (6): 533-40. doi:10.1097/DAD.0b013e3181c80b97. PMID 20526171.
- ↑ 25.0 25.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 521. ISBN 978-0443066542.
- ↑ Vandergriff, TW.; Reed, JA.; Orengo, IF. (2008). "An unusual presentation of atypical fibroxanthoma.". Dermatol Online J 14 (1): 6. PMID 18319023.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1177. ISBN 978-1416031215.
- ↑ URL: http://emedicine.medscape.com/article/1059871-diagnosis. Accessed on: 12 May 2010.
- ↑ Boecker, W.; Junkers, T.; Reusch, M.; Buerger, H.; Korsching, E.; Metze, D.; Decker, T.; Loening, T. et al. (2012). "Origin and differentiation of breast nipple syringoma.". Sci Rep 2: 226. doi:10.1038/srep00226. PMID 22355740.
- ↑ Nosrati, N.; Coleman, NM.; Hsu, S. (2008). "Axillary syringomas.". Dermatol Online J 14 (4): 13. PMID 18627735.
- ↑ 31.0 31.1 31.2 Kumar, B. (Jan 2010). "Chondroid syringoma diagnosed by fine needle aspiration cytology.". Diagn Cytopathol 38 (1): 38-40. doi:10.1002/dc.21159. PMID 19693940.
- ↑ 32.0 32.1 Rauso, R.; Santagata, M.; Tartaro, G.; Filipi, M.; Colella, G.. "Chondroid syringoma: a rare tumor of orofacial region.". Minerva Stomatol 58 (7-8): 383-8. PMID 19633639.
- ↑ 33.0 33.1 URL: http://www.ispub.com/journal/the_internet_journal_of_dermatology/volume_7_number_2_23/article/cutaneous_mixed_tumor.html. Access on: 21 September 2011.
- ↑ 34.0 34.1 34.2 34.3 34.4 Obaidat, NA.; Alsaad, KO.; Ghazarian, D. (Feb 2007). "Skin adnexal neoplasms--part 2: an approach to tumours of cutaneous sweat glands.". J Clin Pathol 60 (2): 145-59. doi:10.1136/jcp.2006.041608. PMC 1860616. PMID 16882695. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860616/.
- ↑ Gerber, JE.; Descalzi, ME. (Feb 1983). "Eccrine spiradenoma and dermal cylindroma.". J Cutan Pathol 10 (1): 73-8. PMID 6302142.
- ↑ Lee, MW.; Kelly, JW. (Feb 1996). "Dermal cylindroma and eccrine spiradenoma.". Australas J Dermatol 37 (1): 48-9. PMID 8936072.
- ↑ URL: http://emedicine.medscape.com/article/1059940-overview. Accessed on: 2 September 2011.
- ↑ Baykal, C.; Buyukbabani, N.; Yazganoglu, KD.; Saglik, E. (Jan 2006). "[Tumors associated with nevus sebaceous].". J Dtsch Dermatol Ges 4 (1): 28-31. doi:10.1111/j.1610-0387.2006.05855.x. PMID 16503928.
- ↑ 39.0 39.1 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 386. ISBN 978-0443066542.
- ↑ 40.0 40.1 URL: http://ccr.cancer.gov/staff/gallery.asp?profileid=12822. Accessed on: 2 September 2011.
- ↑ URL: http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=667496720. Accessed on: 2 September 2011.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675(06)70190-5. Accessed on: 2 July 2010.
- ↑ 43.0 43.1 Punia, RP.; Garg, S.; Bal, A.; Mohan, H. (2008). "Pigmented nodular hidradenoma masquerading as nodular malignant melanoma.". Dermatol Online J 14 (1): 15. PMID 18319032.
- ↑ 44.0 44.1 44.2 Stratigos, AJ.; Olbricht, S.; Kwan, TH.; Bowers, KE. (Mar 1998). "Nodular hidradenoma. A report of three cases and review of the literature.". Dermatol Surg 24 (3): 387-91. PMID 9537017.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 382. ISBN 978-0443066542.
- ↑ 46.0 46.1 46.2 46.3 46.4 Paties, C.; Taccagni, GL.; Papotti, M.; Valente, G.; Zangrandi, A.; Aloi, F. (Jan 1993). "Apocrine carcinoma of the skin. A clinicopathologic, immunocytochemical, and ultrastructural study.". Cancer 71 (2): 375-81. PMID 7678545.
- ↑ 47.0 47.1 47.2 Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 504. ISBN 978-0443066542.
- ↑ Rulon, DB.; Helwig, EB. (May 1977). "Papillary eccrine adenoma.". Arch Dermatol 113 (5): 596-8. PMID 857729.
- ↑ URL: http://archderm.jamanetwork.com/article.aspx?articleid=541159. Accessed on: 10 December 2012.
- ↑ Duke, WH.; Sherrod, TT.; Lupton, GP. (Jun 2000). "Aggressive digital papillary adenocarcinoma (aggressive digital papillary adenoma and adenocarcinoma revisited).". Am J Surg Pathol 24 (6): 775-84. PMID 10843279.
- ↑ 51.0 51.1 Laxmisha, C.; Thappa, DM.; Jayanthi, S.. "Papillary eccrine adenoma.". Indian J Dermatol Venereol Leprol 70 (6): 370-2. PMID 17642667.
- ↑ 52.0 52.1 Guccion, JG.; Patterson, RH.; Nayar, R.; Saini, NB.. "Papillary eccrine adenoma: an ultrastructural and immunohistochemical study.". Ultrastruct Pathol 22 (3): 263-9. PMID 9793207.
- ↑ 53.0 53.1 53.2 Mizuoka, H.; Senzaki, H.; Shikata, N.; Uemura, Y.; Tsubura, A. (Jan 1998). "Papillary eccrine adenoma: immunohistochemical study and literature review.". J Cutan Pathol 25 (1): 59-64. PMID 9508346.
- ↑ Fox, SB.; Cotton, DW. (Apr 1992). "Tubular apocrine adenoma and papillary eccrine adenoma. Entities or unity?". Am J Dermatopathol 14 (2): 149-54. PMID 1566975.
- ↑ Ishiko, A.; Shimizu, H.; Inamoto, N.; Nakmura, K. (Oct 1993). "Is tubular apocrine adenoma a distinct clinical entity?". Am J Dermatopathol 15 (5): 482-7. PMID 8238787.