Intraoperative consultation
Jump to navigation
Jump to search
Intraoperative consultation, also quick section and frozen section, is when a surgeon requests an opinion during an operation so that they can appropriately manage a patient. It is abbreviated IC. Frozen section is often abbreviated FS.
Why intraoperative consultations are done
Reasons why IC are done:[1]
- Determine diagnosis & appropriate extent of operation ~ 50%.
- Margin status ~ 15%.
- Triage tissue ~ 10%.
- Inform family ~ 8%. †
- Sufficient tissue? ~ 8%.
- Treatment planning, e.g. insert a portacath ~ 3%.
Note:
- † Some don't consider this a good reason for an IC.[2]
Why intraoperative consultations may be refused
- Tissue is the issue - not enough of it.
- Infectious case and no back-up cryostat.
- Management - it won't make a difference.
- Diagnosis won't make a difference.
- Cannot make the diagnosis.
- Bone tumours.
Frozen section permanent section concordance
Main article: Quality
Categories by the Association of Directors of Anatomic and Surgical Pathology (ADASP):[3]
- Agreement
- Deferral - appropriate.
- Deferral – inappropriate
- Recommendation <=10% threshold.
- Disagreement – Minor.
- Disagreement – Major.
- Recommendation <=3% threshold.
Common specimens
Table of common FS specimens
| Specimen | Indication | Subspecialty |
|---|---|---|
| Pelvic mass | diagnosis | gynecologic pathology |
| Ovarian mass | diagnosis | gynecologic pathology |
| Uterine mass | diagnosis | gynecologic pathology |
| Sentinel lymph node | staging in vulvar melanoma | gynecologic pathology |
| Squamous cell carcinoma | margins | head and neck pathology |
| Whipple procedure | margins | gastrointestinal pathology |
| Liver resection (usu. metastatic disease) | margins | gastrointestinal pathology |
| Lower anterior resection | distal margin | gastrointestinal pathology |
| Cystectomy/cystoprostatectomy | ureteral margins | genitourinary pathology |
| Pneumonectomy (usu. cancer) | bronchus margin, lymph nodes for staging | pulmonary pathology |
| Brain tumour | diagnosis | neuropathology |
| Spinal tumour | diagnosis | neuropathology |
| Thyroid nodule | diagnosis | endocrine pathology |
| Prosthetic joint | query prosthetic joint infection | joint pathology |
| Parathyroid gland | identify parathyroid gland | endocrine pathology |
List of specimens
Gynecologic
- Pelvic mass - diagnosis (benign/borderline/malignant).
- Ovarian mass - diagnosis (benign/borderline/malignant).
- Uterine mass - diagnosis (benign/borderline/malignant).
- Sentinel lymph node - staging.
- Vulvar melanoma.
Head and neck
- Squamous cell carcinoma - margins.
Gastrointestinal tract
- Whipple procedure - margins.
- Liver resection - margins.
- Lower anterior resection - distal margin.
Genitourinary tract
- Cystoprostatectomy/cystectomy - ureteral margins.
Pulmonary
- Pneumonectomy:
- Bronchus - margins.
- Lymph nodes - staging.
Neurologic
- Brain tumour - diagnosis.
- Spinal tumour - diagnosis.
Thyroid gland
- Thyroid nodule - diagnosis.
Prosthetic joint
- Query prosthetic joint infection.
Surgeon-pathologist dialog
It should include:
Specific specimens - checklists
Ovarian mass
- Covers adnexal mass and pelvic mass.
Checklist
General:
- Specimen integrity: fragmented/intact/ruptured.
- Dimensions: ___ x ___ x ___ cm.
- Mass: ___ grams.
- Surface involvement: absent/present.
- Consistency: solid/cystic/solid and cystic.
Cystic:
- Type: unilocular, multilocular.
- Cyst content: mucinous/serous/hemorrhagic/purulent/chylous/other. ‡
- Papillary excrescences: absent/present.
- Necrosis: absent/present.
- Hair: absent/present.
Sections:
- Sample morphologically distinct areas - esp. solid areas, papillary excrescences.
Notes:
- ‡ Mucinous versus serous:
- Serous: low viscosity (flows with ease threw the grates typically seen at the bottom of sinks[5]).
- Mucinous: high viscosity (jello-like consistency).
DDx
| Feature | Dx/DDx | Notes |
|---|---|---|
| Unilocular cysts | follicular cyst, epithelial cyst, very rarely granulosa cell tumour (not typically diagnosed at FS) | no excrescences or solid areas dx = "simple cyst"; "shag carpet" appearance = serous borderline tumour |
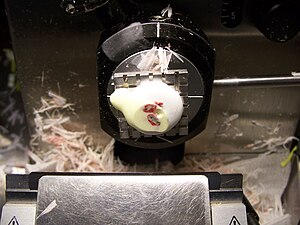
| Sebaceous material or hair | teratoma | Rokitansky nodule present -> submit section; neuroepithelium = fleshy appearance on gross;[6]
immature teratoma not typically diagnosed at FS |
| Chocolate cyst | endometriosis | solid elements (fibrosis vs. clear cell & endometrioid carcinoma |
Endometrial carcinoma
General
- Diagnosis usually known before the surgery.
- The IC revolves around whether the lesion has a "high risk" of lymph node metastasis.
Factors that increase the risk of lymph node metastases:[7]
- Histology:
- Serous or clear cell.
- FIGO grade 3.
- Staging parameters - involvement of:
- Outer half of the myometrium.
- Uterine cervix.
- Adnexa.
Checklist
Gross assessment:
- Uterine cervix involvement (rare).
- Adnexal involvement (rare).
- Myometrial involvement - after sectioning bivalving and sectioning (with a 5 mm interval).
Parathyroid gland
Main article: Parathyroid gland
Possibilities:
- Parathyroid gland:
- Benign parathyroid gland.
- Parathyroid adenoma. †
- Parathyroid hyperplasia. †
- Parathyroid carcinoma.
- Thyroid gland.
- Thyroid usually follicular - though parathyroid occasionally is pseudofollicular.
- Thyroid often has birefringent (calcium oxalate) crystals (60 of 80 cases) whereas parathyroid less often does (2 or 20 cases).[8]
- Lymph node.
- Fibroadipose tissue.
- Paraganglioma.
Notes:
- † It is not possible to determine which one without history or all parathyroid glands.
- Surgeons are pretty good at identifying parathyroid tissue ~ 94% accurate in one series.[9]
Checklist
- Weight.
- Dimensions.
- Appearance.
Sign out
QUERY PARATHYROID GLAND: - PARATHYROID GLAND.
Whipple specimen
Sign out
BILE DUCT MARGIN: - NEGATIVE FOR MALIGNANCY.
Skin specmens
Main article: Oriented skin ellipse grossing
Main article: Unoriented skin ellipse grossing
Cut-up at frozen section depends on how the specimens is received. The standard grossing procedure for fixed specimens can be used if the specimen is small.
See also
References
- ↑ Zarbo, RJ.; Schmidt, WA.; Bachner, P.; Howanitz, PJ.; Meier, FA.; Schifman, RB.; Boone, DJ.; Herron, RM. (Jan 1996). "Indications and immediate patient outcomes of pathology intraoperative consultations. College of American Pathologists/Centers for Disease Control and Prevention Outcomes Working Group Study.". Arch Pathol Lab Med 120 (1): 19-25. PMID 8554440.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 5. ISBN 978-0781767798.
- ↑ URL: http://www.adasp.org/papers/position/QualityAssurance.htm. Accessed on: 2 March 2012.
- ↑ Nakhleh, RE. (Nov 2011). "Quality in surgical pathology communication and reporting.". Arch Pathol Lab Med 135 (11): 1394-7. doi:10.5858/arpa.2011-0192-RA. PMID 22032564.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 33. ISBN 978-0781767798.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 34. ISBN 978-0781767798.
- ↑ Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 43. ISBN 978-0781767798.
- ↑ Wong KS, Lewis JS, Gottipati S, Chernock RD (September 2014). "Utility of birefringent crystal identification by polarized light microscopy in distinguishing thyroid from parathyroid tissue on intraoperative frozen sections". Am J Surg Pathol 38 (9): 1212–9. doi:10.1097/PAS.0000000000000204. PMID 24618617.
- ↑ Dewan, AK.; Kapadia, SB.; Hollenbeak, CS.; Stack, BC. (Dec 2005). "Is routine frozen section necessary for parathyroid surgery?". Otolaryngol Head Neck Surg 133 (6): 857-62. doi:10.1016/j.otohns.2005.05.001. PMID 16360503.