Mixed germ cell tumour
Jump to navigation
Jump to search
| Mixed germ cell tumour | |
|---|---|
| Diagnosis in short | |
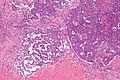
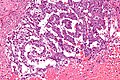
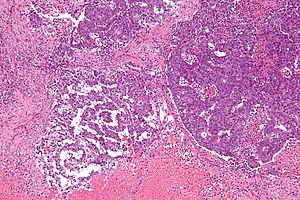 Mixed germ cell tumour. H&E stain. | |
|
| |
| LM | depends on the components |
| LM DDx | other germ cell tumours |
| IHC | variable |
| Gross | heterogeneous appearance, typically solid and cystic |
| Grossing notes | Orchiectomy grossing |
| Staging | Testicular cancer staging |
| Site | ovary, testis, mediastinum, other |
|
| |
| Signs | mass lesion |
| Prevalence | most common germ cell tumour |
| Blood work | +/-AFP elevated, +/-beta-hCG elevated, +/-LDH elevated |
| Prognosis | worse than seminoma/dysgerminoma |
| Clin. DDx | gonads: germ cell tumours, other tumours |
Mixed germ cell tumour, abbreviated MGCT, is a lesion composed of different germ cell tumours. Most germ cell tumours are mixed.
General
- 60% of GCTs are mixed. †
Common combinations:
- Teratoma + embryonal carcinoma + endodermal sinus tumour (yolk sac tumour) (TEE).
- Seminoma + embryonal (SE).
- Teratoma + embryonal +(TE).
Memory device: TEE + all combinations have embryonal carcinoma.
Note:
- † Numbers vary between sources. One series suggests it is almost 70%.[1]
- There has been in increase in MGCTs over the past 20 years that is probably due to changes how in how GCTs are classified.[2]
Gross
- Heterogeneous appearance - distinctive regions that look different from one another.
- Typically solid and cystic.
Images
Microscopic
Features:
- Depends on the components.
- Classic appearances:
- Seminoma: fried egg-like" cells with lymphocytes.
- Yolk sac tumour: edematous appearing/paucicellular regions, Schiller-Duval bodies.
- Embryonal carcinoma: moderate-to-marked nuclear atypia with overlapping nuclei and usu. necrosis.
- Teratoma: cysts with GI like epithelium, cysts with squamous epithelium & keratin (skin), immature cartilage, others.
- Choriocarcinoma: hemorrhagic, multinucleated cells (syncytiotrophoblasts) and cells with pale cytoplasm (cytotrophoblasts).
Notes:
- If one cannot identify the component... it is probably yolk sac as this has so many different patterns.
Images
www:
- Mixed germ cell tumour - several images (upmc.edu).
- Mixed germ cell tumour - several cases (upmc.edu).
IHC
- Immunostains are useful for differentiating components, e.g. yolk sac tumour versus embryonal carcinoma.
Looking for elements
- Beta-hCG +ve - if syncytiotrophoblasts are present.
- AFP +ve (or Glypican 3 +ve) - a yolk sac tumour component is present.
- GFAP +ve - if neuroepithelium is present.
A panel:
- CD30 +ve -- embryonal carcinoma.
- OCT4 +ve -- seminoma.
- D2-40 +ve -- seminoma, useful for LVI.
- Pankeratin +ve -- embryonal carcinoma.
- CEA-M.
- EMA +ve -- metastatic carcinoma.[3]
- Vimentin.
- Glypican 3 +ve -- yolk sac tumour.
- Others: A1A +ve -- yolk sac tumour, AFP +ve -- yolk sac tumour.
Sign out
TESTIS, RIGHT, ORCHIECTOMY: - MALIGNANT MIXED GERM CELL TUMOUR, pT1 pNx: -- 80% OF TUMOUR TERATOMA. -- 20% OF TUMOUR SEMINOMA. -- PLEASE SEE TUMOUR SUMMARY.
See also
References
- ↑ Mosharafa, AA.; Foster, RS.; Leibovich, BC.; Ulbright, TM.; Bihrle, R.; Einhorn, LH.; Donohue, JP. (Apr 2004). "Histology in mixed germ cell tumors. Is there a favorite pairing?". J Urol 171 (4): 1471-3. doi:10.1097/01.ju.0000116841.30826.85. PMID 15017200.
- ↑ Trabert, B.; Stang, A.; Cook, MB.; Rusner, C.; McGlynn, KA. (Aug 2011). "Impact of classification of mixed germ-cell tumours on incidence trends of non-seminoma.". Int J Androl 34 (4 Pt 2): e274-7. doi:10.1111/j.1365-2605.2011.01187.x. PMID 21623833.
- ↑ Shek, TW.; Yuen, ST.; Luk, IS.; Wong, MP. (Mar 1996). "Germ cell tumour as a diagnostic pitfall of metastatic carcinoma.". J Clin Pathol 49 (3): 223-5. PMID 8675733.