Difference between revisions of "Intracranial hematomas"
Jump to navigation
Jump to search
m (→See also) |
|||
| (27 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
'''Intracranial | '''Intracranial [[hematoma]]s''', also '''intracranial hemorrhage''', are bad stuff that keep neurosurgeons busy. They are usually diagnosed by imaging (CT head). | ||
Not much bleeding is needed to cause death. In a person without atrophy (to provide space for the blood) ~75 ml is considered enough if it is acute.<ref>McAuliffe. 15 October 2010.</ref> | Not much bleeding is needed to cause death. In a person without atrophy (to provide space for the blood) ~75 ml is considered enough if it is acute.<ref>McAuliffe. 15 October 2010.</ref> | ||
| Line 30: | Line 30: | ||
==Cerebral venous thrombosis== | ==Cerebral venous thrombosis== | ||
:See also: ''[[Thrombosis]]''. | |||
===General=== | ===General=== | ||
*Extremely rare. | *Extremely rare. | ||
| Line 42: | Line 43: | ||
*Congested appearance. | *Congested appearance. | ||
== | ==Epidural hematoma== | ||
*[[AKA]] ''epidural hemorrhage'' | |||
===General=== | ===General=== | ||
*Extradural hemorrhage. | |||
*Patient may have lucid interval.<ref name=pmid8319240>{{cite journal |author=Erşahin Y, Mutluer S, Güzelbag E |title=Extradural hematoma: analysis of 146 cases |journal=Childs Nerv Syst |volume=9 |issue=2 |pages=96–9 |year=1993 |month=April |pmid=8319240 |doi= |url=}}</ref> | |||
*Classically due to an injury of the ''middle meningeal artery''. | |||
*Usually due to trauma. | |||
*Generally considered artefactual in the context of [[fire deaths]].<ref name=pmid2309533>{{Cite journal | last1 = Ritter | first1 = C. | title = [A heat gelatinized subdural hematoma in a burned cadaver as an indication of a vital accident]. | journal = Z Rechtsmed | volume = 103 | issue = 3 | pages = 227-30 | month = | year = 1990 | doi = | PMID = 2309533 }}</ref> | |||
===Gross=== | |||
*Blood outside of the dura. | |||
Radiology: | |||
*Biconvex. | |||
===Microscopic=== | |||
Features: | |||
*+/-Extravasated [[red blood cell]]s. | |||
*+/-Hemosiderin-laden macrophages. | |||
==Subdural hematoma== | |||
*[[AKA]] ''subdural hemorrhage''. | |||
*Abbreviated ''SDH''. | |||
===General=== | |||
Where/what: | |||
*Bridging veins in subdural space between the dura and arachnoid mater - injured.<ref name=pmid2058082>{{cite journal |author=Crooks DA |title=Pathogenesis and biomechanics of traumatic intracranial haemorrhages |journal=Virchows Arch A Pathol Anat Histopathol |volume=418 |issue=6 |pages=479–83 |year=1991 |pmid=2058082 |doi= |url=}}</ref> | |||
Why? | |||
*+/-Trauma. | |||
*Elderly, esp. those with cerebral atrophy.<ref>{{Ref PCPBoD8|663}}</ref> | |||
Recurrance risks: | |||
*[[Diabetes mellitus]].<ref name=pmid22653496>{{Cite journal | last1 = Chon | first1 = KH. | last2 = Lee | first2 = JM. | last3 = Koh | first3 = EJ. | last4 = Choi | first4 = HY. | title = Independent predictors for recurrence of chronic subdural hematoma. | journal = Acta Neurochir (Wien) | volume = 154 | issue = 9 | pages = 1541-8 | month = Sep | year = 2012 | doi = 10.1007/s00701-012-1399-9 | PMID = 22653496 }}</ref> | |||
===Gross=== | |||
*Blood in the subdural potential space. | |||
*Crescentic shape. | |||
===Microscopic=== | |||
Features: | |||
*Blood in subdural (potential) space. | |||
====Images==== | |||
<gallery> | |||
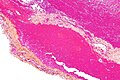
Image:Subdural_hematoma_-_very_low_mag.jpg | SDH - very low mag. (WC) | |||
Image:Subdural_hematoma_-_intermed_low_mag.jpg | SDH - intermed. mag. (WC) | |||
</gallery> | |||
==Subarachnoid hematoma== | |||
*Abbreviated ''SAH''. | *Abbreviated ''SAH''. | ||
*In the [[forensic pathology|forensic]] context ''SAH'' alone is not good enough | *[[AKA]] ''subarachnoid hemorrhage''. | ||
===General=== | |||
*In the [[forensic pathology|forensic]] context ''SAH'' alone is not good enough. | |||
**One needs to determine the cause, e.g. ruptured [[berry aneurysm]] ''or'' laceration of left vertebral artery. | |||
===Traumatic SAH=== | DDx: | ||
*Trauma - most common, see section below. | |||
*Ruptured [[berry aneurysm]] ~80% of non-traumatic SAH.<ref>{{Cite journal | last1 = Ingelmo Ingelmo | first1 = I. | last2 = Fàbregas Julià | first2 = N. | last3 = Rama-Maceiras | first3 = P. | last4 = Hernández-Palazón | first4 = J. | last5 = Rubio Romero | first5 = R. | last6 = Carmona Aurioles | first6 = J. | title = [Subarachnoid hemorrhage: epidemiology, social impact and a multidisciplinary approach]. | journal = Rev Esp Anestesiol Reanim | volume = 57 Suppl 2 | issue = | pages = S4-15 | month = Dec | year = 2010 | doi = | PMID = 21298906 }} | |||
</ref> | |||
*[[Arteriovenous malformation]] and other vascular anomalies. | |||
====Traumatic SAH==== | |||
*May have a characteristic mastoid contusion. | *May have a characteristic mastoid contusion. | ||
**May be associated with vascular [[Ehlers-Danlos syndrome]]. | **May be associated with vascular [[Ehlers-Danlos syndrome]]. | ||
== | ===Gross=== | ||
* | *Blood between pia mater and arachnoid membrane. | ||
*Etiology: fat embolism syndrome | *Typically at the base of the brain. | ||
* | |||
Note: | |||
*Ruptured [[berry aneurysms]] are best found when the brain is fresh; it is hard to dissect away fixed blood. | |||
==Intracerebral hematoma== | |||
*[[AKA]] ''intraparenchymal hemorrhage'', AKA ''intracerebral hemorrhage''. | |||
===General=== | |||
Causes:<ref>{{Ref PCPBoD8|665}}</ref> | |||
*[[Hypertension]] - usually putamen, thalamus, pons, cerebellum - see ''[[hypertension#Intracerebral_hematoma|intracerebral hematoma in hypertension]]''. | |||
*[[Cerebral amyloid angiopathy]] - usually superficial (cortex & subcortical white matter) & frontal lobe or parietal lobe.<ref name=pmid17297004>{{Cite journal | last1 = Haacke | first1 = EM. | last2 = DelProposto | first2 = ZS. | last3 = Chaturvedi | first3 = S. | last4 = Sehgal | first4 = V. | last5 = Tenzer | first5 = M. | last6 = Neelavalli | first6 = J. | last7 = Kido | first7 = D. | title = Imaging cerebral amyloid angiopathy with susceptibility-weighted imaging. | journal = AJNR Am J Neuroradiol | volume = 28 | issue = 2 | pages = 316-7 | month = Feb | year = 2007 | doi = | PMID = 17297004 | URL = http://www.ajnr.org/content/28/2/316.long }}</ref> | |||
*[[Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy]] (CADASIL).<ref name=pmid17135568>{{Cite journal | last1 = Choi | first1 = JC. | last2 = Kang | first2 = SY. | last3 = Kang | first3 = JH. | last4 = Park | first4 = JK. | title = Intracerebral hemorrhages in CADASIL. | journal = Neurology | volume = 67 | issue = 11 | pages = 2042-4 | month = Dec | year = 2006 | doi = 10.1212/01.wnl.0000246601.70918.06 | PMID = 17135568 }}</ref> | |||
===Gross=== | |||
*Blood within the parenchyma of the brain. | |||
===Microscopic=== | |||
*+/-Hemosiderin-laden macrophages. | |||
==Cerebral fat embolism== | |||
===General=== | |||
*Etiology: trauma. | |||
*May be associated with [[pulmonary fat embolism]]. | |||
===Gross=== | |||
Features:<ref name=pmid7423578>{{Cite journal | last1 = Kamenar | first1 = E. | last2 = Burger | first2 = PC. | title = Cerebral fat embolism: a neuropathological study of a microembolic state. | journal = Stroke | volume = 11 | issue = 5 | pages = 477-84 | month = | year = | doi = | PMID = 7423578 }} | |||
</ref> | |||
*Multiple white matter predominant petechiae. | |||
DDx - medical imaging: | |||
*[[Diffuse axonal injury]]<ref name=pmid22406792>{{Cite journal | last1 = Kumar | first1 = S. | last2 = Gupta | first2 = V. | last3 = Aggarwal | first3 = S. | last4 = Singh | first4 = P. | last5 = Khandelwal | first5 = N. | title = Fat embolism syndrome mimicker of diffuse axonal injury on magnetic resonance imaging. | journal = Neurol India | volume = 60 | issue = 1 | pages = 100-2 | month = | year = | doi = 10.4103/0028-3886.93597 | PMID = 22406792 }}</ref> - severe DAI classically has a corpus callosum injury. | |||
*Herpes simplex encephalitis - temporal lobe hemorrhage. | |||
Images: | |||
*[http://www.duke.edu/~ema5/Golian/Slides/3/fluids-hemo_files/flh212.jpg FE (duke.edu)].<ref>URL: [http://www.duke.edu/~ema5/Golian/Slides/3/fluids-hemo.htm http://www.duke.edu/~ema5/Golian/Slides/3/fluids-hemo.htm]. Accessed on: 25 March 2012.</ref> | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3132375/figure/F2/ Cerebral fat embolism (nih.gov)].<ref>{{Cite journal | last1 = Eriksson | first1 = EA. | last2 = Schultz | first2 = SE. | last3 = Cohle | first3 = SD. | last4 = Post | first4 = KW. | title = Cerebral fat embolism without intracardiac shunt: A novel presentation. | journal = J Emerg Trauma Shock | volume = 4 | issue = 2 | pages = 309-12 | month = Apr | year = 2011 | doi = 10.4103/0974-2700.82233 | PMID = 21769222 | PMC = 3132375}}</ref> | |||
===Microscopic=== | |||
Features:<ref name=pmid7423578/> | |||
*Intravascular fat globules. | |||
==See also== | ==See also== | ||
*[[Cerebral amyloid angiopathy]]. | *[[Cerebral amyloid angiopathy]]. | ||
*[[Duret hematoma]]. | |||
*[[Forensic pathology]]. | *[[Forensic pathology]]. | ||
*[[Hypertension]]. | *[[Hypertension]]. | ||
*[[Neuropathology]]. | *[[Neuropathology]]. | ||
*[[Scalp hematomas]]. | |||
==References== | ==References== | ||
Latest revision as of 07:14, 9 December 2014
Intracranial hematomas, also intracranial hemorrhage, are bad stuff that keep neurosurgeons busy. They are usually diagnosed by imaging (CT head).
Not much bleeding is needed to cause death. In a person without atrophy (to provide space for the blood) ~75 ml is considered enough if it is acute.[1]
Clinical
- Headache.
- Neck stiffness.
- Vomit without diarrhea.
- Changes in level of consciousness.
Classification
By location
- Epidural hemorrhage (extradural hemorrhage).
- Patient may have lucid interval.[2]
- Middle meningeal artery.
- Radiology: biconvex.
- Subdural hemorrhage
- Damaged bridging veins: subdural space between the dura and arachnoid mater.[3]
- Radiology: crescent shape.
- Subarachnoid hemorrhage.
- Classically caused by aneuryms:[4]
- Anterior communicating artery (ACA) - most common.
- Middle cerebral artery (MCA) - second most common.
- Classically caused by aneuryms:[4]
- Intracerebral hemorrhage.
- > 60 ml at presentation (assessed via CT scan) assoc. with > 90% 30 day mortality.[5]
By vessel type
- Arterial - common.
- Venous - rare (~3-4 cases/1,000,000 people/year[6]).
Cerebral venous thrombosis
- See also: Thrombosis.
General
- Extremely rare.
- Female > male.
- May be associated with trauma.[7]
- Presentation often mimics subarachnoid haemorrhage.[8]
- Typically involves superior sagittal sinus.[8]
Gross
- Bilateral involvement.
- Congested appearance.
Epidural hematoma
- AKA epidural hemorrhage
General
- Extradural hemorrhage.
- Patient may have lucid interval.[2]
- Classically due to an injury of the middle meningeal artery.
- Usually due to trauma.
- Generally considered artefactual in the context of fire deaths.[11]
Gross
- Blood outside of the dura.
Radiology:
- Biconvex.
Microscopic
Features:
- +/-Extravasated red blood cells.
- +/-Hemosiderin-laden macrophages.
Subdural hematoma
- AKA subdural hemorrhage.
- Abbreviated SDH.
General
Where/what:
- Bridging veins in subdural space between the dura and arachnoid mater - injured.[3]
Why?
- +/-Trauma.
- Elderly, esp. those with cerebral atrophy.[12]
Recurrance risks:
Gross
- Blood in the subdural potential space.
- Crescentic shape.
Microscopic
Features:
- Blood in subdural (potential) space.
Images
Subarachnoid hematoma
- Abbreviated SAH.
- AKA subarachnoid hemorrhage.
General
- In the forensic context SAH alone is not good enough.
- One needs to determine the cause, e.g. ruptured berry aneurysm or laceration of left vertebral artery.
DDx:
- Trauma - most common, see section below.
- Ruptured berry aneurysm ~80% of non-traumatic SAH.[14]
- Arteriovenous malformation and other vascular anomalies.
Traumatic SAH
- May have a characteristic mastoid contusion.
- May be associated with vascular Ehlers-Danlos syndrome.
Gross
- Blood between pia mater and arachnoid membrane.
- Typically at the base of the brain.
Note:
- Ruptured berry aneurysms are best found when the brain is fresh; it is hard to dissect away fixed blood.
Intracerebral hematoma
- AKA intraparenchymal hemorrhage, AKA intracerebral hemorrhage.
General
Causes:[15]
- Hypertension - usually putamen, thalamus, pons, cerebellum - see intracerebral hematoma in hypertension.
- Cerebral amyloid angiopathy - usually superficial (cortex & subcortical white matter) & frontal lobe or parietal lobe.[16]
- Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL).[17]
Gross
- Blood within the parenchyma of the brain.
Microscopic
- +/-Hemosiderin-laden macrophages.
Cerebral fat embolism
General
- Etiology: trauma.
- May be associated with pulmonary fat embolism.
Gross
Features:[18]
- Multiple white matter predominant petechiae.
DDx - medical imaging:
- Diffuse axonal injury[19] - severe DAI classically has a corpus callosum injury.
- Herpes simplex encephalitis - temporal lobe hemorrhage.
Images:
Microscopic
Features:[18]
- Intravascular fat globules.
See also
- Cerebral amyloid angiopathy.
- Duret hematoma.
- Forensic pathology.
- Hypertension.
- Neuropathology.
- Scalp hematomas.
References
- ↑ McAuliffe. 15 October 2010.
- ↑ 2.0 2.1 Erşahin Y, Mutluer S, Güzelbag E (April 1993). "Extradural hematoma: analysis of 146 cases". Childs Nerv Syst 9 (2): 96–9. PMID 8319240.
- ↑ 3.0 3.1 Crooks DA (1991). "Pathogenesis and biomechanics of traumatic intracranial haemorrhages". Virchows Arch A Pathol Anat Histopathol 418 (6): 479–83. PMID 2058082.
- ↑ Beck J, Rohde S, Berkefeld J, Seifert V, Raabe A (January 2006). "Size and location of ruptured and unruptured intracranial aneurysms measured by 3-dimensional rotational angiography". Surg Neurol 65 (1): 18–25; discussion 25–7. doi:10.1016/j.surneu.2005.05.019. PMID 16378842.
- ↑ URL: http://stroke.ahajournals.org/cgi/content/abstract/24/7/987. Accessed on: 2 September 2010.
- ↑ Agostoni E, Aliprandi A, Longoni M (April 2009). "Cerebral venous thrombosis". Expert Rev Neurother 9 (4): 553–64. doi:10.1586/ern.09.3. PMID 19344306.
- ↑ URL: http://emedicine.medscape.com/article/1162804-overview. Accessed on: 12 October 2010.
- ↑ 8.0 8.1 URL: http://www.jpma.org.pk/full_article_text.php?article_id=932. Accessed on: 12 October 2010.
- ↑ Milandre L, Pellissier JF, Vincentelli F, Khalil R (1990). "Deep cerebral venous system thrombosis in adults". Eur. Neurol. 30 (2): 93–7. PMID 2187698.
- ↑ MSP. 12 October 2010.
- ↑ Ritter, C. (1990). "[A heat gelatinized subdural hematoma in a burned cadaver as an indication of a vital accident].". Z Rechtsmed 103 (3): 227-30. PMID 2309533.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 663. ISBN 978-1416054542.
- ↑ Chon, KH.; Lee, JM.; Koh, EJ.; Choi, HY. (Sep 2012). "Independent predictors for recurrence of chronic subdural hematoma.". Acta Neurochir (Wien) 154 (9): 1541-8. doi:10.1007/s00701-012-1399-9. PMID 22653496.
- ↑ Ingelmo Ingelmo, I.; Fàbregas Julià, N.; Rama-Maceiras, P.; Hernández-Palazón, J.; Rubio Romero, R.; Carmona Aurioles, J. (Dec 2010). "[Subarachnoid hemorrhage: epidemiology, social impact and a multidisciplinary approach].". Rev Esp Anestesiol Reanim 57 Suppl 2: S4-15. PMID 21298906.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 665. ISBN 978-1416054542.
- ↑ Haacke, EM.; DelProposto, ZS.; Chaturvedi, S.; Sehgal, V.; Tenzer, M.; Neelavalli, J.; Kido, D. (Feb 2007). "Imaging cerebral amyloid angiopathy with susceptibility-weighted imaging.". AJNR Am J Neuroradiol 28 (2): 316-7. PMID 17297004.
- ↑ Choi, JC.; Kang, SY.; Kang, JH.; Park, JK. (Dec 2006). "Intracerebral hemorrhages in CADASIL.". Neurology 67 (11): 2042-4. doi:10.1212/01.wnl.0000246601.70918.06. PMID 17135568.
- ↑ 18.0 18.1 Kamenar, E.; Burger, PC.. "Cerebral fat embolism: a neuropathological study of a microembolic state.". Stroke 11 (5): 477-84. PMID 7423578.
- ↑ Kumar, S.; Gupta, V.; Aggarwal, S.; Singh, P.; Khandelwal, N.. "Fat embolism syndrome mimicker of diffuse axonal injury on magnetic resonance imaging.". Neurol India 60 (1): 100-2. doi:10.4103/0028-3886.93597. PMID 22406792.
- ↑ URL: http://www.duke.edu/~ema5/Golian/Slides/3/fluids-hemo.htm. Accessed on: 25 March 2012.
- ↑ Eriksson, EA.; Schultz, SE.; Cohle, SD.; Post, KW. (Apr 2011). "Cerebral fat embolism without intracardiac shunt: A novel presentation.". J Emerg Trauma Shock 4 (2): 309-12. doi:10.4103/0974-2700.82233. PMC 3132375. PMID 21769222. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3132375/.