Difference between revisions of "Surgical margins"
(tweak) |
|||
| (68 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
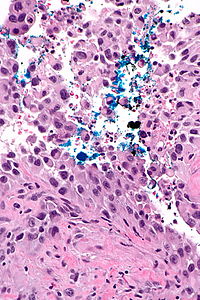
The '''surgical margins''', often simply referred to as '''margins''', are the set of surfaces that were cut by the surgeon in order to remove the specimen from the body. The distance between the tumour and the margin is | [[Image:Urothelial_carcinoma_positive_margin_-_alt_--_high_mag.jpg|thumb|right|200px|A positive surgical margin ([[ink]] on tumour) in [[urothelial carcinoma]]. [[H&E stain]].]] | ||
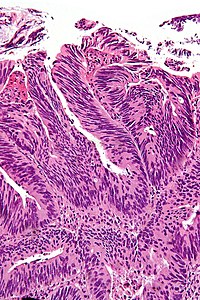
[[Image:Positive_margin_with_cautery_artefact_-_adenocarcinoma_-_high_mag.jpg|right|thumb|200px|A positive surgical margin (tumour with [[cautery artifact]]) in [[colorectal carcinoma]]. [[H&E stain]].]] | |||
The '''surgical margins''', often simply referred to as '''margins''', are the set of surfaces that were cut by the surgeon in order to remove the specimen from the body. The distance between the tumour and the margin is called the '''surgical clearance''', a term that may be used interchangeably with the term ''surgical margin''.<ref name=pmid8443747>{{Cite journal | last1 = Ng | first1 = IO. | last2 = Luk | first2 = IS. | last3 = Yuen | first3 = ST. | last4 = Lau | first4 = PW. | last5 = Pritchett | first5 = CJ. | last6 = Ng | first6 = M. | last7 = Poon | first7 = GP. | last8 = Ho | first8 = J. | title = Surgical lateral clearance in resected rectal carcinomas. A multivariate analysis of clinicopathologic features. | journal = Cancer | volume = 71 | issue = 6 | pages = 1972-6 | month = Mar | year = 1993 | doi = | PMID = 8443747 }}</ref> Margins are important as an incompletely removed disease process may lead to re-occurrence. | |||
What defines a positive surgical margin is dependent on the tumour and its biology; the definitions for a positive margin are often dependent on (1) the anatomical [[site]] of the tumour and (2) the tumour type. | |||
==Significance== | |||
Most often, positive margins, i.e. surgical margins with disease present ''or'' "very close", are non-optimal. For example, in locally advanced [[rectal cancer]], in one study,<ref name=pmid17614249>{{cite journal |author=Larsen SG, Wiig JN, Dueland S, Giercksky KE |title=Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer |journal=Eur J Surg Oncol |volume=34 |issue=4 |pages=410–7 |year=2008 |month=April |pmid=17614249 |doi=10.1016/j.ejso.2007.05.012 |url=}}</ref> five year survival was found to be 60%, 31% and 0% for R0 (no tumour at the margin), R1 (microscopic tumour at the margin), and R2 (macroscopic tumour at the margin) resections respectively. | |||
==Types of margins== | ==Types of margins== | ||
*''En face''. | *''En face'' (formally ''en face margin''). | ||
**Sample the complete surface. | **Sample the complete surface. | ||
**No information about the distance between the margin and lesion can be obtained. | **No information about the distance between the margin and lesion can be obtained at microscopy, i.e. from the glass slide. | ||
*''On edge'', [[AKA]] ''perpendicular margin'', as the cut to prepare the tissue for microscopic examination is perpendicular to the cut from the surgeon. | *''On edge'' (formally ''on edge margin''), [[AKA]] ''perpendicular margin'', as the cut to prepare the tissue for microscopic examination is perpendicular to the cut from the surgeon. | ||
**Sample a subset of the surface. | **Sample a subset of the surface. | ||
**The distance between the margin and lesion can be measured. | **The distance between the margin and lesion can be measured at microscopy, i.e. on the glass slide. | ||
Note: | |||
*It should ''always'' be clear from the ''[[Principles of grossing|gross description]]'' which type of margin was taken; this is especially important for cases that were not [[submitted in total]]. | |||
==Positive margin definition== | |||
Unfortunately, there is no universal definition for ''positive margin''. | |||
Definitionally, there is agreement that "tumour touching the edge of the specimen" is a ''positive margin''.<ref name=pmid26028131>{{cite journal |authors=Chagpar AB, Killelea BK, Tsangaris TN, Butler M, Stavris K, Li F, Yao X, Bossuyt V, Harigopal M, Lannin DR, Pusztai L, Horowitz NR |title=A Randomized, Controlled Trial of Cavity Shave Margins in Breast Cancer |journal=N Engl J Med |volume=373 |issue=6 |pages=503–10 |date=August 2015 |pmid=26028131 |pmc=5584380 |doi=10.1056/NEJMoa1504473 |url=}}</ref><ref name=pmid16509840/> | |||
It may be useful to differentiate ''pathologic margin [status]'' (tumour touching inked margin) and ''oncologic margin [status]'' (tumour sufficiently clear of margin to not significantly affect the prognosis). Oncologists, surgeons and patients really only care about ''oncologic margin [status]'' for relatively obvious reasons. | |||
Perhaps confusing is that: ''a [pathologically] clear margin'' may be defined as being ''[oncologically] a positive margin'', e.g. tumour ''not'' touching the ink of an inked margin - but less than 1 mm from the ink - may be a "positive margin".<ref name=pmid16509840>{{cite journal |authors=Scopa CD, Aroukatos P, Tsamandas AC, Aletra C |title=Evaluation of margin status in lumpectomy specimens and residual breast carcinoma |journal=Breast J |volume=12 |issue=2 |pages=150–3 |date=2006 |pmid=16509840 |doi=10.1111/j.1075-122X.2006.00223.x |url=}}</ref> | |||
==Adequate margin== | ==Adequate margin== | ||
*What constitutes an adequate margin is dependent on the tumour type, as different tumours have different behaviours. | *What constitutes an adequate margin is dependent on the tumour type, as different tumours have different behaviours. | ||
===Adequate margins by tumour=== | |||
{| class="wikitable sortable" | |||
!Tumour | |||
!Adequate pathologic margin | |||
!Adequate clinical margin | |||
!System | |||
|- | |||
| [[Colorectal carcinoma]] | |||
| >1 mm;<ref name=pmid37722286>{{cite journal |authors=Smith HG, Schlesinger NH, Qvortrup C, Chiranth D, Lundon D, Ben-Yaacov A, Caballero C, Suppan I, Kok JH, Holmberg CJ, Mohan H, Montagna G, Santrac N, Sayyed R, Schrage Y, Sgarbura O, Ceelen W, Lorenzon L, Brandl A |title=Variations in the definition and perceived importance of positive resection margins in patients with colorectal cancer - an EYSAC international survey |journal=Eur J Surg Oncol |volume=49 |issue=11 |pages=107072 |date=November 2023 |pmid=37722286 |doi=10.1016/j.ejso.2023.107072 |url=}}</ref> circumferential margin (esp. in rectal carcinoma) most important<ref name=pmid7915774>{{Cite journal | last1 = Adam | first1 = IJ. | last2 = Mohamdee | first2 = MO. | last3 = Martin | first3 = IG. | last4 = Scott | first4 = N. | last5 = Finan | first5 = PJ. | last6 = Johnston | first6 = D. | last7 = Dixon | first7 = MF. | last8 = Quirke | first8 = P. | title = Role of circumferential margin involvement in the local recurrence of rectal cancer. | journal = Lancet | volume = 344 | issue = 8924 | pages = 707-11 | month = Sep | year = 1994 | doi = | PMID = 7915774 }}</ref> | |||
| 1 cm<ref name=pmid18766404>{{Cite journal | last1 = Rutkowski | first1 = A. | last2 = Bujko | first2 = K. | last3 = Nowacki | first3 = MP. | last4 = Chmielik | first4 = E. | last5 = Nasierowska-Guttmejer | first5 = A. | last6 = Wojnar | first6 = A. | title = Distal bowel surgical margin shorter than 1 cm after preoperative radiation for rectal cancer: is it safe? | journal = Ann Surg Oncol | volume = 15 | issue = 11 | pages = 3124-31 | month = Nov | year = 2008 | doi = 10.1245/s10434-008-0125-6 | PMID = 18766404 }}</ref> | |||
| [[Gastrointestinal pathology]] | |||
|- | |||
|[[Vulvar carcinoma]] | |||
| 0.8 cm (fixed)<ref name=pmid21669423/> | |||
| 1.0 cm (fresh)<ref name=pmid21669423>{{Cite journal | last1 = Palaia | first1 = I. | last2 = Bellati | first2 = F. | last3 = Calcagno | first3 = M. | last4 = Musella | first4 = A. | last5 = Perniola | first5 = G. | last6 = Panici | first6 = PB. | title = Invasive vulvar carcinoma and the question of the surgical margin. | journal = Int J Gynaecol Obstet | volume = 114 | issue = 2 | pages = 120-3 | month = Aug | year = 2011 | doi = 10.1016/j.ijgo.2011.02.012 | PMID = 21669423 }}</ref> | |||
| [[Gynecologic pathology]] | |||
|- | |||
|[[Malignant melanoma]] | |||
| same as clinical (interesting is that CAP says "no minimum safe distance established"<ref>URL: [http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/SkinMelanoma_12protocol.pdf http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/SkinMelanoma_12protocol.pdf]. Accessed on: 19 August 2012.</ref>) | |||
| | |||
*[[MIS]]: 5 mm<ref name=pmid22196979>{{Cite journal | last1 = Kunishige | first1 = JH. | last2 = Brodland | first2 = DG. | last3 = Zitelli | first3 = JA. | title = Surgical margins for melanoma in situ. | journal = J Am Acad Dermatol | volume = 66 | issue = 3 | pages = 438-44 | month = Mar | year = 2012 | doi = 10.1016/j.jaad.2011.06.019 | PMID = 22196979 }}</ref> considered inadequate by some<ref name=pmid19050971>{{Cite journal | last1 = Möller | first1 = MG. | last2 = Pappas-Politis | first2 = E. | last3 = Zager | first3 = JS. | last4 = Santiago | first4 = LA. | last5 = Yu | first5 = D. | last6 = Prakash | first6 = A. | last7 = Kinal | first7 = A. | last8 = Clark | first8 = GS. | last9 = Zhu | first9 = W. | title = Surgical management of melanoma-in-situ using a staged marginal and central excision technique. | journal = Ann Surg Oncol | volume = 16 | issue = 6 | pages = 1526-36 | month = Jun | year = 2009 | doi = 10.1245/s10434-008-0239-x | PMID = 19050971 }}</ref> | |||
*<2 mm invasion: 10 mm<ref name=pmid11013363>{{Cite journal | last1 = Cohn-Cedermark | first1 = G. | last2 = Rutqvist | first2 = LE. | last3 = Andersson | first3 = R. | last4 = Breivald | first4 = M. | last5 = Ingvar | first5 = C. | last6 = Johansson | first6 = H. | last7 = Jönsson | first7 = PE. | last8 = Krysander | first8 = L. | last9 = Lindholm | first9 = C. | title = Long term results of a randomized study by the Swedish Melanoma Study Group on 2-cm versus 5-cm resection margins for patients with cutaneous melanoma with a tumor thickness of 0.8-2.0 mm. | journal = Cancer | volume = 89 | issue = 7 | pages = 1495-501 | month = Oct | year = 2000 | doi = | PMID = 11013363 }}</ref><ref name=pmid2009058>{{Cite journal | last1 = Veronesi | first1 = U. | last2 = Cascinelli | first2 = N. | title = Narrow excision (1-cm margin). A safe procedure for thin cutaneous melanoma. | journal = Arch Surg | volume = 126 | issue = 4 | pages = 438-41 | month = Apr | year = 1991 | doi = | PMID = 2009058 }}</ref> | |||
*>=2 mm invasion: 20 mm<ref name=pmid11258773>{{Cite journal | last1 = Balch | first1 = CM. | last2 = Soong | first2 = SJ. | last3 = Smith | first3 = T. | last4 = Ross | first4 = MI. | last5 = Urist | first5 = MM. | last6 = Karakousis | first6 = CP. | last7 = Temple | first7 = WJ. | last8 = Mihm | first8 = MC. | last9 = Barnhill | first9 = RL. | title = Long-term results of a prospective surgical trial comparing 2 cm vs. 4 cm excision margins for 740 patients with 1-4 mm melanomas. | journal = Ann Surg Oncol | volume = 8 | issue = 2 | pages = 101-8 | month = Mar | year = 2001 | doi = | PMID = 11258773 }}</ref> | |||
| [[Dermatopathology]] | |||
|- | |||
| [[Ductal carcinoma in situ]] | |||
| [[ink]] cannot be on tumour - consensus of Society of Surgical Oncology-American Society for Radiation Oncology (for low stage tumours)<ref name=pmid24521674>{{Cite journal | last1 = Moran | first1 = MS. | last2 = Schnitt | first2 = SJ. | last3 = Giuliano | first3 = AE. | last4 = Harris | first4 = JR. | last5 = Khan | first5 = SA. | last6 = Horton | first6 = J. | last7 = Klimberg | first7 = S. | last8 = Chavez-MacGregor | first8 = M. | last9 = Freedman | first9 = G. | title = Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. | journal = Int J Radiat Oncol Biol Phys | volume = 88 | issue = 3 | pages = 553-64 | month = Mar | year = 2014 | doi = 10.1016/j.ijrobp.2013.11.012 | PMID = 24521674 }}</ref> | |||
| | |||
| [[Breast pathology]] | |||
|- | |||
| [[Invasive breast cancer|Invasive breast carcinoma]] | |||
| ink cannot be on tumour - consensus of Society of Surgical Oncology-American Society for Radiation Oncology (for low stage tumours)<ref name=pmid24521674>{{Cite journal | last1 = Moran | first1 = MS. | last2 = Schnitt | first2 = SJ. | last3 = Giuliano | first3 = AE. | last4 = Harris | first4 = JR. | last5 = Khan | first5 = SA. | last6 = Horton | first6 = J. | last7 = Klimberg | first7 = S. | last8 = Chavez-MacGregor | first8 = M. | last9 = Freedman | first9 = G. | title = Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. | journal = Int J Radiat Oncol Biol Phys | volume = 88 | issue = 3 | pages = 553-64 | month = Mar | year = 2014 | doi = 10.1016/j.ijrobp.2013.11.012 | PMID = 24521674 }}</ref> | |||
| | |||
| [[Breast pathology]] | |||
|- | |||
| [[Sarcoma]] | |||
| >= 1 cm<ref name=pmid10506627>{{Cite journal | last1 = Baldini | first1 = EH. | last2 = Goldberg | first2 = J. | last3 = Jenner | first3 = C. | last4 = Manola | first4 = JB. | last5 = Demetri | first5 = GD. | last6 = Fletcher | first6 = CD. | last7 = Singer | first7 = S. | title = Long-term outcomes after function-sparing surgery without radiotherapy for soft tissue sarcoma of the extremities and trunk. | journal = J Clin Oncol | volume = 17 | issue = 10 | pages = 3252-9 | month = Oct | year = 1999 | doi = | PMID = 10506627 }}</ref> | |||
| | |||
| [[Sarcoma]] | |||
|- | |||
| [[Prostate carcinoma]] | |||
| tumour not touching ink - "close" margins have a higher biochemical recurrence<ref name=pmid22578729>{{Cite journal | last1 = Lu | first1 = J. | last2 = Wirth | first2 = GJ. | last3 = Wu | first3 = S. | last4 = Chen | first4 = J. | last5 = Dahl | first5 = DM. | last6 = Olumi | first6 = AF. | last7 = Young | first7 = RH. | last8 = McDougal | first8 = WS. | last9 = Wu | first9 = CL. | title = A close surgical margin after radical prostatectomy is an independent predictor of recurrence. | journal = J Urol | volume = 188 | issue = 1 | pages = 91-7 | month = Jul | year = 2012 | doi = 10.1016/j.juro.2012.02.2565 | PMID = 22578729 }}</ref> | |||
| | |||
| [[Genitourinary pathology]] | |||
|- | |||
| [[Renal cell carcinoma]] | |||
| tumour not touching ink; positive margins get clinical follow-up as recurrences are uncommon<ref name=pmid22136987>{{Cite journal | last1 = Marszalek | first1 = M. | last2 = Carini | first2 = M. | last3 = Chlosta | first3 = P. | last4 = Jeschke | first4 = K. | last5 = Kirkali | first5 = Z. | last6 = Knüchel | first6 = R. | last7 = Madersbacher | first7 = S. | last8 = Patard | first8 = JJ. | last9 = Van Poppel | first9 = H. | title = Positive surgical margins after nephron-sparing surgery. | journal = Eur Urol | volume = 61 | issue = 4 | pages = 757-63 | month = Apr | year = 2012 | doi = 10.1016/j.eururo.2011.11.028 | PMID = 22136987 }}</ref> | |||
| | |||
| [[Genitourinary pathology]] | |||
|- | |||
| [[Squamous cell carcinoma of the skin]] | |||
| | |||
| 4 mm, 6 mm for high risk<ref name=pmid1430364>{{Cite journal | last1 = Brodland | first1 = DG. | last2 = Zitelli | first2 = JA. | title = Surgical margins for excision of primary cutaneous squamous cell carcinoma. | journal = J Am Acad Dermatol | volume = 27 | issue = 2 Pt 1 | pages = 241-8 | month = Aug | year = 1992 | doi = | PMID = 1430364 }}</ref> | |||
| [[Dermatopathology]] | |||
|- | |||
| [[Urothelial carcinoma]] | |||
| tumour not touching ink<ref name=pmid17936804>{{Cite journal | last1 = Dotan | first1 = ZA. | last2 = Kavanagh | first2 = K. | last3 = Yossepowitch | first3 = O. | last4 = Kaag | first4 = M. | last5 = Olgac | first5 = S. | last6 = Donat | first6 = M. | last7 = Herr | first7 = HW. | title = Positive surgical margins in soft tissue following radical cystectomy for bladder cancer and cancer specific survival. | journal = J Urol | volume = 178 | issue = 6 | pages = 2308-12; discussion 2313 | month = Dec | year = 2007 | doi = 10.1016/j.juro.2007.08.023 | PMID = 17936804 }}</ref> | |||
| | |||
| [[Genitourinary pathology]] | |||
|- <!-- | |||
|Tumour | |||
|Pathologic margin | |||
|Clinical margin | |||
|System --> | |||
|} | |||
==Fragmented and incised specimens== | |||
There is limited advice on how to deal with a fragmented or incised specimen. | |||
If the specimen can be "put back together", it is reasonable to assess the margin and comment on the limitation. | |||
The ''College of American Pathologists'' synoptic for invasive breast carcinoma (version 4.3.0.1) states:<ref>URL: [https://documents.cap.org/protocols/cp-breast-invasive-resection-19-4301.pdf https://documents.cap.org/protocols/cp-breast-invasive-resection-19-4301.pdf]. Accessed on: 2022 January 12.</ref> | |||
:''If the specimen is received sectioned or fragmented, this should be noted, as this will limit the ability to evaluate the status of margins.'' | |||
==Microscopic== | |||
Features of the true margin: | |||
*Irregular/non-linear appearance. | |||
DDx: | |||
*Cut at the grossing bench (by the pathologist/pathology assistant/pathology resident) post-[[fixation]] - these are usually straight. | |||
*Artifactal cleft/separation. | |||
Note: | |||
*The surgeon's cut is irregular due to loading during extraction and fixation effects. | |||
===Images=== | |||
<gallery> | |||
Image: Surgeons cut at microscopy - extremely low mag.jpg | True margin - surgeon's cut (left of image) - extremely low mag. (WC) | |||
Image: PAs cut at microscopy - extremely low mag.jpg | Pathology assistant's cut (right of image) - extremely low mag. (WC) | |||
</gallery> | |||
==Sign out== | |||
===Stray ink versus true positive=== | |||
====True positive==== | |||
<pre> | |||
COMMENT: | |||
Ink is seen very focally on a fragment of tumour in A21-1. Inspection of | |||
the tissue block shows ink on the surface of the tissue fragment with the | |||
positive margin; this essentially excludes that what is interpreted as a | |||
positive margin could represent stray ink. | |||
</pre> | |||
====Stray ink==== | |||
<pre> | |||
COMMENT: | |||
The margin assessment is suboptimal as the specimen was cut prior to | |||
inking. Ink on tumour in this context may represent stray ink on tumour | |||
or a true positive margin. | |||
Ink is focally present on tumour in this case and it is favoured to | |||
represent stray ink, as the quantity of ink is minimal; however, margin | |||
positivity cannot be completely excluded. | |||
</pre> | |||
===A re-excised (previously) positive margin is negative for tumour=== | |||
It occasionally happens that a re-excised margin specimen is negative for tumour. | |||
<pre> | |||
The lack of tumour in Part B may be explained by either of the following: | |||
(1) There was minimal clearance (<1 mm) in Part A that was not sampled. | |||
(2) The sampling of Part B missed minimal tumour involvement. | |||
</pre> | |||
Note: | |||
*One should review the positive margin call to ensure it isn't an overall. | |||
===Tumour in tip - flipped block=== | |||
<pre> | |||
Lesion, Right Upper Lid, Excision: | |||
- BASAL CELL CARCINOMA, favour clear margin (see comment). | |||
Comment: | |||
Basal cell carcinoma (BCC) is present in the block 3 tip, on the initial cut. The tissue was re-embedded and BCC is seen on the recut. BCC is clear of the inked margin. Thus, the margin is favoured to be clear; however, out-of-plane margin involvement cannot be excluded. | |||
</pre> | |||
===Alternate=== | |||
<pre> | |||
Lesion, Right Lower Eyelid, Excision: | |||
- BASAL CELL CARCINOMA (BCC), cannot exclude positive margin, see comment. | |||
Comment: | |||
BCC was found in block 1 (one of the tips) on the initial cut. | |||
In block 1, BCC is present but distant from the inked margin in the plane | |||
of section. The margin is not completely in the plane of section; thus, | |||
trimming of a negative margin cannot be entirely excluded. As BCC is seen | |||
on both sides of the block, a positive cannot be excluded. | |||
</pre> | |||
==See also== | ==See also== | ||
*[[Basics]]. | *[[Basics]]. | ||
*[[Frozen section]]. | *[[Frozen section]]. | ||
*[[Crush artifact]]. | |||
*[[Marking ink]]. | |||
==References== | ==References== | ||
Latest revision as of 05:38, 9 January 2024
The surgical margins, often simply referred to as margins, are the set of surfaces that were cut by the surgeon in order to remove the specimen from the body. The distance between the tumour and the margin is called the surgical clearance, a term that may be used interchangeably with the term surgical margin.[1] Margins are important as an incompletely removed disease process may lead to re-occurrence.
What defines a positive surgical margin is dependent on the tumour and its biology; the definitions for a positive margin are often dependent on (1) the anatomical site of the tumour and (2) the tumour type.
Significance
Most often, positive margins, i.e. surgical margins with disease present or "very close", are non-optimal. For example, in locally advanced rectal cancer, in one study,[2] five year survival was found to be 60%, 31% and 0% for R0 (no tumour at the margin), R1 (microscopic tumour at the margin), and R2 (macroscopic tumour at the margin) resections respectively.
Types of margins
- En face (formally en face margin).
- Sample the complete surface.
- No information about the distance between the margin and lesion can be obtained at microscopy, i.e. from the glass slide.
- On edge (formally on edge margin), AKA perpendicular margin, as the cut to prepare the tissue for microscopic examination is perpendicular to the cut from the surgeon.
- Sample a subset of the surface.
- The distance between the margin and lesion can be measured at microscopy, i.e. on the glass slide.
Note:
- It should always be clear from the gross description which type of margin was taken; this is especially important for cases that were not submitted in total.
Positive margin definition
Unfortunately, there is no universal definition for positive margin.
Definitionally, there is agreement that "tumour touching the edge of the specimen" is a positive margin.[3][4]
It may be useful to differentiate pathologic margin [status] (tumour touching inked margin) and oncologic margin [status] (tumour sufficiently clear of margin to not significantly affect the prognosis). Oncologists, surgeons and patients really only care about oncologic margin [status] for relatively obvious reasons.
Perhaps confusing is that: a [pathologically] clear margin may be defined as being [oncologically] a positive margin, e.g. tumour not touching the ink of an inked margin - but less than 1 mm from the ink - may be a "positive margin".[4]
Adequate margin
- What constitutes an adequate margin is dependent on the tumour type, as different tumours have different behaviours.
Adequate margins by tumour
| Tumour | Adequate pathologic margin | Adequate clinical margin | System |
|---|---|---|---|
| Colorectal carcinoma | >1 mm;[5] circumferential margin (esp. in rectal carcinoma) most important[6] | 1 cm[7] | Gastrointestinal pathology |
| Vulvar carcinoma | 0.8 cm (fixed)[8] | 1.0 cm (fresh)[8] | Gynecologic pathology |
| Malignant melanoma | same as clinical (interesting is that CAP says "no minimum safe distance established"[9]) | Dermatopathology | |
| Ductal carcinoma in situ | ink cannot be on tumour - consensus of Society of Surgical Oncology-American Society for Radiation Oncology (for low stage tumours)[15] | Breast pathology | |
| Invasive breast carcinoma | ink cannot be on tumour - consensus of Society of Surgical Oncology-American Society for Radiation Oncology (for low stage tumours)[15] | Breast pathology | |
| Sarcoma | >= 1 cm[16] | Sarcoma | |
| Prostate carcinoma | tumour not touching ink - "close" margins have a higher biochemical recurrence[17] | Genitourinary pathology | |
| Renal cell carcinoma | tumour not touching ink; positive margins get clinical follow-up as recurrences are uncommon[18] | Genitourinary pathology | |
| Squamous cell carcinoma of the skin | 4 mm, 6 mm for high risk[19] | Dermatopathology | |
| Urothelial carcinoma | tumour not touching ink[20] | Genitourinary pathology |
Fragmented and incised specimens
There is limited advice on how to deal with a fragmented or incised specimen.
If the specimen can be "put back together", it is reasonable to assess the margin and comment on the limitation.
The College of American Pathologists synoptic for invasive breast carcinoma (version 4.3.0.1) states:[21]
- If the specimen is received sectioned or fragmented, this should be noted, as this will limit the ability to evaluate the status of margins.
Microscopic
Features of the true margin:
- Irregular/non-linear appearance.
DDx:
- Cut at the grossing bench (by the pathologist/pathology assistant/pathology resident) post-fixation - these are usually straight.
- Artifactal cleft/separation.
Note:
- The surgeon's cut is irregular due to loading during extraction and fixation effects.
Images
Sign out
Stray ink versus true positive
True positive
COMMENT: Ink is seen very focally on a fragment of tumour in A21-1. Inspection of the tissue block shows ink on the surface of the tissue fragment with the positive margin; this essentially excludes that what is interpreted as a positive margin could represent stray ink.
Stray ink
COMMENT: The margin assessment is suboptimal as the specimen was cut prior to inking. Ink on tumour in this context may represent stray ink on tumour or a true positive margin. Ink is focally present on tumour in this case and it is favoured to represent stray ink, as the quantity of ink is minimal; however, margin positivity cannot be completely excluded.
A re-excised (previously) positive margin is negative for tumour
It occasionally happens that a re-excised margin specimen is negative for tumour.
The lack of tumour in Part B may be explained by either of the following: (1) There was minimal clearance (<1 mm) in Part A that was not sampled. (2) The sampling of Part B missed minimal tumour involvement.
Note:
- One should review the positive margin call to ensure it isn't an overall.
Tumour in tip - flipped block
Lesion, Right Upper Lid, Excision:
- BASAL CELL CARCINOMA, favour clear margin (see comment).
Comment:
Basal cell carcinoma (BCC) is present in the block 3 tip, on the initial cut. The tissue was re-embedded and BCC is seen on the recut. BCC is clear of the inked margin. Thus, the margin is favoured to be clear; however, out-of-plane margin involvement cannot be excluded.
Alternate
Lesion, Right Lower Eyelid, Excision:
- BASAL CELL CARCINOMA (BCC), cannot exclude positive margin, see comment.
Comment:
BCC was found in block 1 (one of the tips) on the initial cut.
In block 1, BCC is present but distant from the inked margin in the plane
of section. The margin is not completely in the plane of section; thus,
trimming of a negative margin cannot be entirely excluded. As BCC is seen
on both sides of the block, a positive cannot be excluded.
See also
References
- ↑ Ng, IO.; Luk, IS.; Yuen, ST.; Lau, PW.; Pritchett, CJ.; Ng, M.; Poon, GP.; Ho, J. (Mar 1993). "Surgical lateral clearance in resected rectal carcinomas. A multivariate analysis of clinicopathologic features.". Cancer 71 (6): 1972-6. PMID 8443747.
- ↑ Larsen SG, Wiig JN, Dueland S, Giercksky KE (April 2008). "Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer". Eur J Surg Oncol 34 (4): 410–7. doi:10.1016/j.ejso.2007.05.012. PMID 17614249.
- ↑ Chagpar AB, Killelea BK, Tsangaris TN, Butler M, Stavris K, Li F, Yao X, Bossuyt V, Harigopal M, Lannin DR, Pusztai L, Horowitz NR (August 2015). "A Randomized, Controlled Trial of Cavity Shave Margins in Breast Cancer". N Engl J Med 373 (6): 503–10. doi:10.1056/NEJMoa1504473. PMC 5584380. PMID 26028131. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5584380/.
- ↑ 4.0 4.1 Scopa CD, Aroukatos P, Tsamandas AC, Aletra C (2006). "Evaluation of margin status in lumpectomy specimens and residual breast carcinoma". Breast J 12 (2): 150–3. doi:10.1111/j.1075-122X.2006.00223.x. PMID 16509840.
- ↑ Smith HG, Schlesinger NH, Qvortrup C, Chiranth D, Lundon D, Ben-Yaacov A, Caballero C, Suppan I, Kok JH, Holmberg CJ, Mohan H, Montagna G, Santrac N, Sayyed R, Schrage Y, Sgarbura O, Ceelen W, Lorenzon L, Brandl A (November 2023). "Variations in the definition and perceived importance of positive resection margins in patients with colorectal cancer - an EYSAC international survey". Eur J Surg Oncol 49 (11): 107072. doi:10.1016/j.ejso.2023.107072. PMID 37722286.
- ↑ Adam, IJ.; Mohamdee, MO.; Martin, IG.; Scott, N.; Finan, PJ.; Johnston, D.; Dixon, MF.; Quirke, P. (Sep 1994). "Role of circumferential margin involvement in the local recurrence of rectal cancer.". Lancet 344 (8924): 707-11. PMID 7915774.
- ↑ Rutkowski, A.; Bujko, K.; Nowacki, MP.; Chmielik, E.; Nasierowska-Guttmejer, A.; Wojnar, A. (Nov 2008). "Distal bowel surgical margin shorter than 1 cm after preoperative radiation for rectal cancer: is it safe?". Ann Surg Oncol 15 (11): 3124-31. doi:10.1245/s10434-008-0125-6. PMID 18766404.
- ↑ 8.0 8.1 Palaia, I.; Bellati, F.; Calcagno, M.; Musella, A.; Perniola, G.; Panici, PB. (Aug 2011). "Invasive vulvar carcinoma and the question of the surgical margin.". Int J Gynaecol Obstet 114 (2): 120-3. doi:10.1016/j.ijgo.2011.02.012. PMID 21669423.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/SkinMelanoma_12protocol.pdf. Accessed on: 19 August 2012.
- ↑ Kunishige, JH.; Brodland, DG.; Zitelli, JA. (Mar 2012). "Surgical margins for melanoma in situ.". J Am Acad Dermatol 66 (3): 438-44. doi:10.1016/j.jaad.2011.06.019. PMID 22196979.
- ↑ Möller, MG.; Pappas-Politis, E.; Zager, JS.; Santiago, LA.; Yu, D.; Prakash, A.; Kinal, A.; Clark, GS. et al. (Jun 2009). "Surgical management of melanoma-in-situ using a staged marginal and central excision technique.". Ann Surg Oncol 16 (6): 1526-36. doi:10.1245/s10434-008-0239-x. PMID 19050971.
- ↑ Cohn-Cedermark, G.; Rutqvist, LE.; Andersson, R.; Breivald, M.; Ingvar, C.; Johansson, H.; Jönsson, PE.; Krysander, L. et al. (Oct 2000). "Long term results of a randomized study by the Swedish Melanoma Study Group on 2-cm versus 5-cm resection margins for patients with cutaneous melanoma with a tumor thickness of 0.8-2.0 mm.". Cancer 89 (7): 1495-501. PMID 11013363.
- ↑ Veronesi, U.; Cascinelli, N. (Apr 1991). "Narrow excision (1-cm margin). A safe procedure for thin cutaneous melanoma.". Arch Surg 126 (4): 438-41. PMID 2009058.
- ↑ Balch, CM.; Soong, SJ.; Smith, T.; Ross, MI.; Urist, MM.; Karakousis, CP.; Temple, WJ.; Mihm, MC. et al. (Mar 2001). "Long-term results of a prospective surgical trial comparing 2 cm vs. 4 cm excision margins for 740 patients with 1-4 mm melanomas.". Ann Surg Oncol 8 (2): 101-8. PMID 11258773.
- ↑ 15.0 15.1 Moran, MS.; Schnitt, SJ.; Giuliano, AE.; Harris, JR.; Khan, SA.; Horton, J.; Klimberg, S.; Chavez-MacGregor, M. et al. (Mar 2014). "Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer.". Int J Radiat Oncol Biol Phys 88 (3): 553-64. doi:10.1016/j.ijrobp.2013.11.012. PMID 24521674.
- ↑ Baldini, EH.; Goldberg, J.; Jenner, C.; Manola, JB.; Demetri, GD.; Fletcher, CD.; Singer, S. (Oct 1999). "Long-term outcomes after function-sparing surgery without radiotherapy for soft tissue sarcoma of the extremities and trunk.". J Clin Oncol 17 (10): 3252-9. PMID 10506627.
- ↑ Lu, J.; Wirth, GJ.; Wu, S.; Chen, J.; Dahl, DM.; Olumi, AF.; Young, RH.; McDougal, WS. et al. (Jul 2012). "A close surgical margin after radical prostatectomy is an independent predictor of recurrence.". J Urol 188 (1): 91-7. doi:10.1016/j.juro.2012.02.2565. PMID 22578729.
- ↑ Marszalek, M.; Carini, M.; Chlosta, P.; Jeschke, K.; Kirkali, Z.; Knüchel, R.; Madersbacher, S.; Patard, JJ. et al. (Apr 2012). "Positive surgical margins after nephron-sparing surgery.". Eur Urol 61 (4): 757-63. doi:10.1016/j.eururo.2011.11.028. PMID 22136987.
- ↑ Brodland, DG.; Zitelli, JA. (Aug 1992). "Surgical margins for excision of primary cutaneous squamous cell carcinoma.". J Am Acad Dermatol 27 (2 Pt 1): 241-8. PMID 1430364.
- ↑ Dotan, ZA.; Kavanagh, K.; Yossepowitch, O.; Kaag, M.; Olgac, S.; Donat, M.; Herr, HW. (Dec 2007). "Positive surgical margins in soft tissue following radical cystectomy for bladder cancer and cancer specific survival.". J Urol 178 (6): 2308-12; discussion 2313. doi:10.1016/j.juro.2007.08.023. PMID 17936804.
- ↑ URL: https://documents.cap.org/protocols/cp-breast-invasive-resection-19-4301.pdf. Accessed on: 2022 January 12.