Difference between revisions of "Clear cell renal cell carcinoma"
(→Gross) |
m (benign clear cell clusters) |
||
| (30 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
| Width = | | Width = | ||
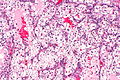
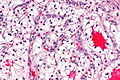
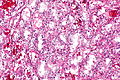
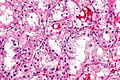
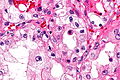
| Caption = Clear cell renal cell carcinoma. [[H&E stain]]. | | Caption = Clear cell renal cell carcinoma. [[H&E stain]]. | ||
| Micro = solid or [[trabecular]] pattern, polygonal cells usually with clear cytoplasm, central nucleus, delicate branching vasculature (chicken wire-like), +/-hyaline bodies | | Synonyms = conventional renal cell carcinoma | ||
| Subtypes = | | Micro = solid or [[trabecular]] pattern, polygonal cells usually with clear cytoplasm (may be eosinophilic - esp. in high grade tumours), central nucleus, delicate branching vasculature (chicken wire-like), +/-hyaline bodies | ||
| Subtypes = | |||
| LMDDx = [[chromophobe renal cell carcinoma]], [[clear cell papillary renal cell carcinoma]], [[Xp11.2 translocation carcinoma]], [[adrenocortical carcinoma]], [[alveolar soft part sarcoma]] | | LMDDx = [[chromophobe renal cell carcinoma]], [[clear cell papillary renal cell carcinoma]], [[Xp11.2 translocation carcinoma]], [[adrenocortical carcinoma]], [[alveolar soft part sarcoma]] | ||
| Stains = [[Hale's colloidal iron stain]] -ve | | Stains = [[Hale's colloidal iron stain]] -ve | ||
| IHC = CK7 -ve, CK20 -ve, TFE3 -ve | | IHC = [[CA9]] +ve, CK7 -ve, CK20 -ve, TFE3 -ve, PAX8 +ve, vimentin +ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| IF = | | IF = | ||
| Gross = | | Gross = golden/yellow colour, +/-hemorrhagic, +/-cystic, +/-[[necrosis]] | ||
| Grossing = | | Grossing = [[total nephrectomy for tumour grossing]], [[partial nephrectomy grossing]] | ||
| Staging = [[kidney cancer staging]] | |||
| Site = [[kidney]] - see [[kidney tumours]] | | Site = [[kidney]] - see [[kidney tumours]] | ||
| Assdx = | | Assdx = | ||
| Line 27: | Line 29: | ||
| Other = | | Other = | ||
| ClinDDx = other [[renal tumours]] | | ClinDDx = other [[renal tumours]] | ||
| Tx = surgery, targeted therapies, other drugs | |||
}} | }} | ||
'''Clear cell renal cell carcinoma''', abbreviated | '''Clear cell renal cell carcinoma''', abbreviated '''CCRCC''', is the most common type of [[renal cell carcinoma]]. | ||
It is also known as '''conventional renal cell carcinoma''' (abbreviated '''CRCC'''). | |||
==General== | ==General== | ||
| Line 35: | Line 40: | ||
*Familial clear cell renal cell carcinoma<ref name=pmid23972705>{{Cite journal | last1 = Keefe | first1 = SM. | last2 = Nathanson | first2 = KL. | last3 = Rathmell | first3 = WK. | title = The molecular biology of renal cell carcinoma. | journal = Semin Oncol | volume = 40 | issue = 4 | pages = 421-8 | month = Aug | year = 2013 | doi = 10.1053/j.seminoncol.2013.05.006 | PMID = 23972705 }}</ref> - usually VHL gene mutation.<ref name=pmid17205537>{{Cite journal | last1 = Foster | first1 = RE. | last2 = Abdulrahman | first2 = M. | last3 = Morris | first3 = MR. | last4 = Prigmore | first4 = E. | last5 = Gribble | first5 = S. | last6 = Ng | first6 = B. | last7 = Gentle | first7 = D. | last8 = Ready | first8 = S. | last9 = Weston | first9 = PM. | title = Characterization of a 3;6 translocation associated with renal cell carcinoma. | journal = Genes Chromosomes Cancer | volume = 46 | issue = 4 | pages = 311-7 | month = Apr | year = 2007 | doi = 10.1002/gcc.20403 | PMID = 17205537 }}</ref> | *Familial clear cell renal cell carcinoma<ref name=pmid23972705>{{Cite journal | last1 = Keefe | first1 = SM. | last2 = Nathanson | first2 = KL. | last3 = Rathmell | first3 = WK. | title = The molecular biology of renal cell carcinoma. | journal = Semin Oncol | volume = 40 | issue = 4 | pages = 421-8 | month = Aug | year = 2013 | doi = 10.1053/j.seminoncol.2013.05.006 | PMID = 23972705 }}</ref> - usually VHL gene mutation.<ref name=pmid17205537>{{Cite journal | last1 = Foster | first1 = RE. | last2 = Abdulrahman | first2 = M. | last3 = Morris | first3 = MR. | last4 = Prigmore | first4 = E. | last5 = Gribble | first5 = S. | last6 = Ng | first6 = B. | last7 = Gentle | first7 = D. | last8 = Ready | first8 = S. | last9 = Weston | first9 = PM. | title = Characterization of a 3;6 translocation associated with renal cell carcinoma. | journal = Genes Chromosomes Cancer | volume = 46 | issue = 4 | pages = 311-7 | month = Apr | year = 2007 | doi = 10.1002/gcc.20403 | PMID = 17205537 }}</ref> | ||
**VHL gene not mutated in all cases.<ref name=pmid10807693>{{Cite journal | last1 = Woodward | first1 = ER. | last2 = Clifford | first2 = SC. | last3 = Astuti | first3 = D. | last4 = Affara | first4 = NA. | last5 = Maher | first5 = ER. | title = Familial clear cell renal cell carcinoma (FCRC): clinical features and mutation analysis of the VHL, MET, and CUL2 candidate genes. | journal = J Med Genet | volume = 37 | issue = 5 | pages = 348-53 | month = May | year = 2000 | doi = | PMID = 10807693 }}</ref> | **VHL gene not mutated in all cases.<ref name=pmid10807693>{{Cite journal | last1 = Woodward | first1 = ER. | last2 = Clifford | first2 = SC. | last3 = Astuti | first3 = D. | last4 = Affara | first4 = NA. | last5 = Maher | first5 = ER. | title = Familial clear cell renal cell carcinoma (FCRC): clinical features and mutation analysis of the VHL, MET, and CUL2 candidate genes. | journal = J Med Genet | volume = 37 | issue = 5 | pages = 348-53 | month = May | year = 2000 | doi = | PMID = 10807693 }}</ref> | ||
Treatment: | |||
*Surgery. | |||
*Various drugs. | |||
*Targeted therapies. | |||
**[[Tyrosine kinase inhibitors]] (e.g. [[sunitinib]], sorafenib).<ref name=pmid25467013>{{Cite journal | last1 = Elaidi | first1 = R. | last2 = Harbaoui | first2 = A. | last3 = Beuselinck | first3 = B. | last4 = Eymard | first4 = JC. | last5 = Bamias | first5 = A. | last6 = De Guillebon | first6 = E. | last7 = Porta | first7 = C. | last8 = Vano | first8 = Y. | last9 = Linassier | first9 = C. | title = Outcomes from second-line therapy in long-term responders to first-line tyrosine kinase inhibitor in clear-cell metastatic renal cell carcinoma. | journal = Ann Oncol | volume = 26 | issue = 2 | pages = 378-85 | month = Feb | year = 2015 | doi = 10.1093/annonc/mdu552 | PMID = 25467013 }}</ref><ref name=pmid21484781>{{Cite journal | last1 = Verma | first1 = J. | last2 = Jonasch | first2 = E. | last3 = Allen | first3 = P. | last4 = Tannir | first4 = N. | last5 = Mahajan | first5 = A. | title = Impact of tyrosine kinase inhibitors on the incidence of brain metastasis in metastatic renal cell carcinoma. | journal = Cancer | volume = 117 | issue = 21 | pages = 4958-65 | month = Nov | year = 2011 | doi = 10.1002/cncr.26138 | PMID = 21484781 }}</ref> | |||
**Anti-VEGF antibodies (e.g. bevacizumab).<ref name=pmid21330923>{{Cite journal | last1 = Singer | first1 = EA. | last2 = Gupta | first2 = GN. | last3 = Srinivasan | first3 = R. | title = Update on targeted therapies for clear cell renal cell carcinoma. | journal = Curr Opin Oncol | volume = 23 | issue = 3 | pages = 283-9 | month = May | year = 2011 | doi = 10.1097/CCO.0b013e32834479c0 | PMID = 21330923 }}</ref> | |||
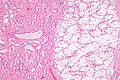
==Gross== | ==Gross== | ||
Features: | Features: | ||
* | *Golden/yellow colour. | ||
*+/-Haemorrhage (common). | *+/-Haemorrhage (common). | ||
*+/-Necrosis (common in large tumours). | *+/-Necrosis (common in large tumours). | ||
| Line 55: | Line 67: | ||
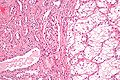
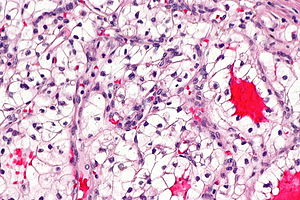
==Microscopic== | ==Microscopic== | ||
Features:<ref name=Ref_PBoD1017-8>{{Ref PBoD|1017-8}}</ref> | Features:<ref name=Ref_PBoD1017-8>{{Ref PBoD|1017-8}}</ref> | ||
*Clear cytoplasm. | |||
**May have eosinophilic cytoplasm (in high-grade tumours) - usually focal. | |||
*Delicate branching vasculature - '''key feature'''. | |||
**Often called "chicken wire-like" vasculature. | |||
*Solid or [[trabecular]] pattern. | *Solid or [[trabecular]] pattern. | ||
*Polygonal cells. | *Polygonal cells. | ||
*Central nucleus. | *Central nucleus. | ||
*+/-[[Renal cell carcinoma with rhabdoid morphology|Rhabdoid cells]]: | |||
*+/-Rhabdoid cells: | |||
**Eccentric nucleus. | **Eccentric nucleus. | ||
**Abundant eosinophilic | **Abundant eosinophilic cytoplasm. | ||
Notes: | Notes: | ||
| Line 72: | Line 85: | ||
**Not common in papillary RCC. | **Not common in papillary RCC. | ||
*Clear cytoplasm - due to lipid content. | *Clear cytoplasm - due to lipid content. | ||
*[[Necrosis]] is independent predictor of outcome - if present in a significant quantity:<ref name=pmid25474516>{{Cite journal | last1 = Renshaw | first1 = AA. | last2 = Cheville | first2 = JC. | title = Quantitative tumour necrosis is an independent predictor of overall survival in clear cell renal cell carcinoma. | journal = Pathology | volume = 47 | issue = 1 | pages = 34-7 | month = Jan | year = 2015 | doi = 10.1097/PAT.0000000000000193 | PMID = 25474516 }}</ref> | |||
**>30% is significant for pT3a tumours. | |||
**>20% is significant for pT1-2 pN0 tumours. | |||
DDx: | DDx: | ||
| Line 80: | Line 96: | ||
**EMA -ve, CKs mostly -ve, inhibin +ve (neg. in RCC).<ref name=Ref_GUP285>{{Ref GUP|285}}</ref> | **EMA -ve, CKs mostly -ve, inhibin +ve (neg. in RCC).<ref name=Ref_GUP285>{{Ref GUP|285}}</ref> | ||
*[[Alveolar soft part sarcoma]]. | *[[Alveolar soft part sarcoma]]. | ||
*[[Adrenal gland]], normal. | *[[Adrenal gland]], normal cortex - wispy, vacuolated. | ||
*[[Epithelioid angiomyolipoma]]. | *[[Epithelioid angiomyolipoma]]. | ||
*[[Benign clear cell clusters of the kidney]]. | |||
===Images=== | ===Images=== | ||
| Line 114: | Line 131: | ||
*CD10 +ve. | *CD10 +ve. | ||
*Vimentin +ve. | *Vimentin +ve. | ||
*CK7 -ve. | *CK7 -ve. | ||
**Strong CK7 staining is more in keeping with [[clear cell papillary renal cell carcinoma]]<ref name=pmid26457355>{{Cite journal | last1 = Williamson | first1 = SR. | last2 = Gupta | first2 = NS. | last3 = Eble | first3 = JN. | last4 = Rogers | first4 = CG. | last5 = Michalowski | first5 = S. | last6 = Zhang | first6 = S. | last7 = Wang | first7 = M. | last8 = Grignon | first8 = DJ. | last9 = Cheng | first9 = L. | title = Clear Cell Renal Cell Carcinoma With Borderline Features of Clear Cell Papillary Renal Cell Carcinoma: Combined Morphologic, Immunohistochemical, and Cytogenetic Analysis. | journal = Am J Surg Pathol | volume = 39 | issue = 11 | pages = 1502-10 | month = Nov | year = 2015 | doi = 10.1097/PAS.0000000000000514 | PMID = 26457355 }}</ref> or the evolving entity of [[TCEB1-mutated renal cell carcinoma]]. | |||
*CK20 -ve. | *CK20 -ve. | ||
*Glut-1 >85% of CCRCC (membranous pattern).<ref name=pmid17638658>{{Cite journal | last1 = Ozcan | first1 = A. | last2 = Shen | first2 = SS. | last3 = Zhai | first3 = QJ. | last4 = Truong | first4 = LD. | title = Expression of GLUT1 in primary renal tumors: morphologic and biologic implications. | journal = Am J Clin Pathol | volume = 128 | issue = 2 | pages = 245-54 | month = Aug | year = 2007 | doi = 10.1309/HV6NJVRQKK4QHM9F | PMID = 17638658 }}</ref> | *Glut-1 >85% of CCRCC (membranous pattern).<ref name=pmid17638658>{{Cite journal | last1 = Ozcan | first1 = A. | last2 = Shen | first2 = SS. | last3 = Zhai | first3 = QJ. | last4 = Truong | first4 = LD. | title = Expression of GLUT1 in primary renal tumors: morphologic and biologic implications. | journal = Am J Clin Pathol | volume = 128 | issue = 2 | pages = 245-54 | month = Aug | year = 2007 | doi = 10.1309/HV6NJVRQKK4QHM9F | PMID = 17638658 }}</ref> | ||
*E-cadherin +ve - usually weak, often -ve in higher stage tumours.<ref name=pmid23939157>{{Cite journal | last1 = Hu | first1 = H. | last2 = Chen | first2 = JW. | last3 = Xu | first3 = KX. | last4 = Wang | first4 = D. | last5 = Wang | first5 = Y. | last6 = Wang | first6 = GW. | last7 = Zhang | first7 = SY. | last8 = Wang | first8 = XF. | title = [Expressions of CMTM8 and E-cadherin in primary and metastatic clear cell renal cell carcinoma]. | journal = Beijing Da Xue Xue Bao | volume = 45 | issue = 4 | pages = 537-41 | month = Aug | year = 2013 | doi = | PMID = 23939157 }}</ref> | |||
*CAIX (also CA9) +ve. | |||
A panel to confirm the diagnosis: | A panel to confirm the diagnosis: | ||
| Line 124: | Line 144: | ||
ISUP recommends:<ref name=pmid25025364 >{{cite journal |author=Amin MB, Epstein JI, Ulbright TM, ''et al.'' |title=Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference |journal=Am. J. Surg. Pathol. |volume=38 |issue=8 |pages=1017–22 |year=2014 |month=August |pmid=25025364 |doi=10.1097/PAS.0000000000000254 |url=}}</ref> | ISUP recommends:<ref name=pmid25025364 >{{cite journal |author=Amin MB, Epstein JI, Ulbright TM, ''et al.'' |title=Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference |journal=Am. J. Surg. Pathol. |volume=38 |issue=8 |pages=1017–22 |year=2014 |month=August |pmid=25025364 |doi=10.1097/PAS.0000000000000254 |url=}}</ref> | ||
*CD117 -ve (+ve in ChRCC). | *CD117 -ve (+ve in ChRCC). | ||
* | **Aguilar-León ''et al.'' found ~8% of CCRCC are CD117 +ve.<ref name=pmid25643775>{{Cite journal | last1 = Aguilar-León | first1 = D. | last2 = Del Ángel-Millán | first2 = G. | last3 = Zepeda-Quiroz | first3 = I. | last4 = Soria-Céspedes | first4 = D. | title = [Immunohistochemical Expression of CD117 (c-kit) in 75 Renal Cell Tumors]. | journal = Gac Med Mex | volume = 150 Suppl 2 | issue = | pages = 156-60 | month = Dec | year = 2014 | doi = | PMID = 25643775 }}</ref> | ||
*CK7 -ve (+ve in ChRCC). | **Liu ''et al.'' found ~80% of ChRCC are CD117 +ve.<ref name=pmid17683191/> | ||
*CA9 ([[carbonic anhydrase 9]]) +ve (membranous).<ref name=pmid21677535>{{cite journal |author=Al-Ahmadie HA, Alden D, Fine SW, ''et al.'' |title=Role of immunohistochemistry in the evaluation of needle core biopsies in adult renal cortical tumors: an ex vivo study |journal=Am. J. Surg. Pathol. |volume=35 |issue=7 |pages=949–61 |year=2011 |month=July |pmid=21677535 |doi=10.1097/PAS.0b013e31821e25cd |url=}}</ref> | |||
*[[CK7]] -ve (+ve in ChRCC). | |||
May also be useful: | |||
*Vimentin +ve. | *Vimentin +ve. | ||
**-ve in ChRCC. | **-ve in ChRCC.<ref name=pmid17683191>{{Cite journal | last1 = Liu | first1 = L. | last2 = Qian | first2 = J. | last3 = Singh | first3 = H. | last4 = Meiers | first4 = I. | last5 = Zhou | first5 = X. | last6 = Bostwick | first6 = DG. | title = Immunohistochemical analysis of chromophobe renal cell carcinoma, renal oncocytoma, and clear cell carcinoma: an optimal and practical panel for differential diagnosis. | journal = Arch Pathol Lab Med | volume = 131 | issue = 8 | pages = 1290-7 | month = Aug | year = 2007 | doi = 10.1043/1543-2165(2007)131[1290:IAOCRC]2.0.CO;2 | PMID = 17683191 }}</ref> | ||
===CCRCC versus [[CCPRCC]]=== | ===CCRCC versus [[CCPRCC]]=== | ||
[[ISUP]] recommends:<ref name=pmid25025364/> | [[ISUP]] recommends:<ref name=pmid25025364/> | ||
* | *CA9 +ve (strong membranous). | ||
*CK7 -ve. | *CK7 -ve. | ||
**Usually +ve in [[clear cell papillary renal cell carcinoma]]. | |||
*AMACR -ve. | *AMACR -ve. | ||
| Line 165: | Line 186: | ||
<pre> | <pre> | ||
Kidney Mass, Left, Core Biopsy: | Kidney Mass, Left, Core Biopsy: | ||
- CLEAR CELL RENAL CELL CARCINOMA, preliminary nucleolar grade 2 (see comment) | - CLEAR CELL RENAL CELL CARCINOMA, preliminary ISUP nucleolar grade 2 (see comment). | ||
- No renal parenchyma identified | - No renal parenchyma identified. | ||
Comment: | Comment: | ||
| Line 177: | Line 198: | ||
*The surgeon wants the diagnosis and margin status; thus, these are included in the diagnosis line with the tumour stage. | *The surgeon wants the diagnosis and margin status; thus, these are included in the diagnosis line with the tumour stage. | ||
<pre> | |||
Left Kidney, Radical Nephrectomy: | |||
- CLEAR CELL RENAL CELL CARCINOMA. | |||
-- Margins clear. | |||
-- Please see synoptic report. | |||
</pre> | |||
====Block letters==== | |||
<pre> | <pre> | ||
KIDNEY, LEFT, NEPHRECTOMY: | KIDNEY, LEFT, NEPHRECTOMY: | ||
| Line 204: | Line 233: | ||
The sections show a tumour with a chicken wire-like vasculature composed of clear cells with basally stratified nuclei. Hemosiderin-laden macrophages are present. Necrosis is present. Abundant hyaline globules are present. | The sections show a tumour with a chicken wire-like vasculature composed of clear cells with basally stratified nuclei. Hemosiderin-laden macrophages are present. Necrosis is present. Abundant hyaline globules are present. | ||
There is no perinuclear clearing. The cytoplasm is not | There is no perinuclear clearing. The cytoplasm is not wispy. Papillae are not evident. | ||
Rare, small nucleoli are visible with the 10x objective. The tumour nuclei are approximately 15 micrometers. | Rare, small nucleoli are visible with the 10x objective. The tumour nuclei are approximately 15 micrometers. | ||
| Line 215: | Line 244: | ||
==See also== | ==See also== | ||
*[[Kidney tumours]]. | *[[Kidney tumours]]. | ||
*[[TCEB1-mutated renal cell carcinoma]]. | |||
*[[Renal cell carcinoma with rhabdoid morphology]]. | |||
==References== | ==References== | ||
Latest revision as of 16:14, 22 January 2024
| Clear cell renal cell carcinoma | |
|---|---|
| Diagnosis in short | |
 Clear cell renal cell carcinoma. H&E stain. | |
|
| |
| Synonyms | conventional renal cell carcinoma |
|
| |
| LM | solid or trabecular pattern, polygonal cells usually with clear cytoplasm (may be eosinophilic - esp. in high grade tumours), central nucleus, delicate branching vasculature (chicken wire-like), +/-hyaline bodies |
| LM DDx | chromophobe renal cell carcinoma, clear cell papillary renal cell carcinoma, Xp11.2 translocation carcinoma, adrenocortical carcinoma, alveolar soft part sarcoma |
| Stains | Hale's colloidal iron stain -ve |
| IHC | CA9 +ve, CK7 -ve, CK20 -ve, TFE3 -ve, PAX8 +ve, vimentin +ve |
| Gross | golden/yellow colour, +/-hemorrhagic, +/-cystic, +/-necrosis |
| Grossing notes | total nephrectomy for tumour grossing, partial nephrectomy grossing |
| Staging | kidney cancer staging |
| Site | kidney - see kidney tumours |
|
| |
| Syndromes | von Hippel-Lindau syndrome, familial clear cell renal cell carcinoma |
|
| |
| Signs | +/-hematuria, +/-abdominal mass |
| Prevalence | common |
| Radiology | renal mass |
| Prognosis | good-to-poor - dependent on stage and grade |
| Clin. DDx | other renal tumours |
| Treatment | surgery, targeted therapies, other drugs |
Clear cell renal cell carcinoma, abbreviated CCRCC, is the most common type of renal cell carcinoma.
It is also known as conventional renal cell carcinoma (abbreviated CRCC).
General
- Most common subtype of RCC.
- May be associated with Von Hippel-Lindau syndrome.
- Familial clear cell renal cell carcinoma[1] - usually VHL gene mutation.[2]
- VHL gene not mutated in all cases.[3]
Treatment:
- Surgery.
- Various drugs.
- Targeted therapies.
- Tyrosine kinase inhibitors (e.g. sunitinib, sorafenib).[4][5]
- Anti-VEGF antibodies (e.g. bevacizumab).[6]
Gross
Features:
- Golden/yellow colour.
- +/-Haemorrhage (common).
- +/-Necrosis (common in large tumours).
- +/-Calcification.
- +/-Cysts.
- Usually unifocal. ‡
Note:
- ‡ Approximately 4% of CCRCCs are multifocal (based on a set of 5378 patients).[7]
Image
Microscopic
Features:[8]
- Clear cytoplasm.
- May have eosinophilic cytoplasm (in high-grade tumours) - usually focal.
- Delicate branching vasculature - key feature.
- Often called "chicken wire-like" vasculature.
- Solid or trabecular pattern.
- Polygonal cells.
- Central nucleus.
- +/-Rhabdoid cells:
- Eccentric nucleus.
- Abundant eosinophilic cytoplasm.
Notes:
- Cytoplasm may be eosinophilic.[9]
- This change is typically focal - other areas have a classic appearance.
- Chicken wire-like vasculature present - helps distinguish from other tumours.
- Hyaline bodies common.[10]
- Not common in papillary RCC.
- Clear cytoplasm - due to lipid content.
- Necrosis is independent predictor of outcome - if present in a significant quantity:[11]
- >30% is significant for pT3a tumours.
- >20% is significant for pT1-2 pN0 tumours.
DDx:
- Chromophobe renal cell carcinoma.
- Clear cell papillary renal cell carcinoma.
- Xp11.2 translocation carcinoma.
- Adrenocortical carcinoma (ACC)
- EMA -ve, CKs mostly -ve, inhibin +ve (neg. in RCC).[12]
- Alveolar soft part sarcoma.
- Adrenal gland, normal cortex - wispy, vacuolated.
- Epithelioid angiomyolipoma.
- Benign clear cell clusters of the kidney.
Images
Case 1
Case 2
Case 3
Stains
- Hale's colloidal iron -ve.
- +ve in chromophobe RCC.
Note: Hale's colloidal iron does not stain iron... it stains hemosiderin.[13]
Clear cell vs. chromophobe:
- Chromophobe: "translucent" (NOT quite clear), reticulated, Hale's colloidal iron stain+, CK7+ (cell membrane).
IHC
- CD10 +ve.
- Vimentin +ve.
- CK7 -ve.
- Strong CK7 staining is more in keeping with clear cell papillary renal cell carcinoma[14] or the evolving entity of TCEB1-mutated renal cell carcinoma.
- CK20 -ve.
- Glut-1 >85% of CCRCC (membranous pattern).[15]
- E-cadherin +ve - usually weak, often -ve in higher stage tumours.[16]
- CAIX (also CA9) +ve.
A panel to confirm the diagnosis:
- CK7 (-ve), CD10 (+ve), PAX8 (+ve), vimentin (+ve).
CCRCC versus chromophobe RCC
ISUP recommends:[17]
- CD117 -ve (+ve in ChRCC).
- CA9 (carbonic anhydrase 9) +ve (membranous).[20]
- CK7 -ve (+ve in ChRCC).
May also be useful:
- Vimentin +ve.
- -ve in ChRCC.[19]
CCRCC versus CCPRCC
- CA9 +ve (strong membranous).
- CK7 -ve.
- Usually +ve in clear cell papillary renal cell carcinoma.
- AMACR -ve.
Others:
- CD10 +ve.
- Usually -ve in clear cell papillary renal cell carcinoma.
CCRCC versus Xp11.2 translocation carcinomas
ISUP recommends:[17]
- Cathepsin K -ve.[21]
- TFE3 -ve.
- TFEB -ve.
Sign out
Biopsy
Kidney Mass, Left, Core Biopsy: - Clear cell renal cell carcinoma - ISUP nucleolar grade 2 (based on biopsy) - No renal parenchyma identified Comment: The quantity of tissue available at microscopy is very limited. Immunostains confirm the morphologic impression (see microscopic).
MDA form
Kidney Mass, Left, Core Biopsy: - CLEAR CELL RENAL CELL CARCINOMA, preliminary ISUP nucleolar grade 2 (see comment). - No renal parenchyma identified. Comment: The quantity of tissue at microscopy is limited, and may not be representative of the lesion identified radiologically.
Resection
Note:
- The surgeon wants the diagnosis and margin status; thus, these are included in the diagnosis line with the tumour stage.
Left Kidney, Radical Nephrectomy:
- CLEAR CELL RENAL CELL CARCINOMA.
-- Margins clear.
-- Please see synoptic report.
Block letters
KIDNEY, LEFT, NEPHRECTOMY: - CLEAR CELL RENAL CELL CARCINOMA, FUHRMAN GRADE 2, pT1a, pNx. -- MARGINS NEGATIVE FOR MALIGNANCY. -- PLEASE SEE TUMOUR SUMMARY.
Adrenal gland present
KIDNEY, RIGHT, RADICAL NEPHRECTOMY: - CLEAR CELL RENAL CELL CARCINOMA, FUHRMAN GRADE 2, pT1a, pNx. -- MARGINS NEGATIVE FOR MALIGNANCY. -- PLEASE SEE TUMOUR SUMMARY. - ADRENAL GLAND WITHIN NORMAL LIMITS.
KIDNEY, RIGHT, RADICAL NEPHRECTOMY: - CLEAR CELL RENAL CELL CARCINOMA, FUHRMAN GRADE 3, pT1b, pNx. -- MARGINS NEGATIVE FOR MALIGNANCY. -- PLEASE SEE TUMOUR SUMMARY. - ADRENAL GLAND WITHIN NORMAL LIMITS.
Micro
The sections show a tumour with a chicken wire-like vasculature composed of clear cells with basally stratified nuclei. Hemosiderin-laden macrophages are present. Necrosis is present. Abundant hyaline globules are present.
There is no perinuclear clearing. The cytoplasm is not wispy. Papillae are not evident.
Rare, small nucleoli are visible with the 10x objective. The tumour nuclei are approximately 15 micrometers.
Alternate
The sections show cohesive mildly atypical clear cells with a columnar morphology. Small cystic spaces are present. The nuclei are basal stratified. Nucleoli are not prominent. Siderophages are present. Blood is present.
No perinuclear halos are apparent. No papillary structures are identified. No definite renal parenchyma is seen.
See also
References
- ↑ Keefe, SM.; Nathanson, KL.; Rathmell, WK. (Aug 2013). "The molecular biology of renal cell carcinoma.". Semin Oncol 40 (4): 421-8. doi:10.1053/j.seminoncol.2013.05.006. PMID 23972705.
- ↑ Foster, RE.; Abdulrahman, M.; Morris, MR.; Prigmore, E.; Gribble, S.; Ng, B.; Gentle, D.; Ready, S. et al. (Apr 2007). "Characterization of a 3;6 translocation associated with renal cell carcinoma.". Genes Chromosomes Cancer 46 (4): 311-7. doi:10.1002/gcc.20403. PMID 17205537.
- ↑ Woodward, ER.; Clifford, SC.; Astuti, D.; Affara, NA.; Maher, ER. (May 2000). "Familial clear cell renal cell carcinoma (FCRC): clinical features and mutation analysis of the VHL, MET, and CUL2 candidate genes.". J Med Genet 37 (5): 348-53. PMID 10807693.
- ↑ Elaidi, R.; Harbaoui, A.; Beuselinck, B.; Eymard, JC.; Bamias, A.; De Guillebon, E.; Porta, C.; Vano, Y. et al. (Feb 2015). "Outcomes from second-line therapy in long-term responders to first-line tyrosine kinase inhibitor in clear-cell metastatic renal cell carcinoma.". Ann Oncol 26 (2): 378-85. doi:10.1093/annonc/mdu552. PMID 25467013.
- ↑ Verma, J.; Jonasch, E.; Allen, P.; Tannir, N.; Mahajan, A. (Nov 2011). "Impact of tyrosine kinase inhibitors on the incidence of brain metastasis in metastatic renal cell carcinoma.". Cancer 117 (21): 4958-65. doi:10.1002/cncr.26138. PMID 21484781.
- ↑ Singer, EA.; Gupta, GN.; Srinivasan, R. (May 2011). "Update on targeted therapies for clear cell renal cell carcinoma.". Curr Opin Oncol 23 (3): 283-9. doi:10.1097/CCO.0b013e32834479c0. PMID 21330923.
- ↑ Siracusano, S.; Novara, G.; Antonelli, A.; Artibani, W.; Bertini, R.; Carini, M.; Carmignani, G.; Ciciliato, S. et al. (Dec 2012). "Prognostic role of tumour multifocality in renal cell carcinoma.". BJU Int 110 (11 Pt B): E443-8. doi:10.1111/j.1464-410X.2012.11121.x. PMID 22502873.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1017-8. ISBN 0-7216-0187-1.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 291. ISBN 978-0781765275.
- ↑ AFIP Renal Tumours Book.
- ↑ Renshaw, AA.; Cheville, JC. (Jan 2015). "Quantitative tumour necrosis is an independent predictor of overall survival in clear cell renal cell carcinoma.". Pathology 47 (1): 34-7. doi:10.1097/PAT.0000000000000193. PMID 25474516.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 285. ISBN 978-0443066771.
- ↑ Latta. 27 January 2009.
- ↑ Williamson, SR.; Gupta, NS.; Eble, JN.; Rogers, CG.; Michalowski, S.; Zhang, S.; Wang, M.; Grignon, DJ. et al. (Nov 2015). "Clear Cell Renal Cell Carcinoma With Borderline Features of Clear Cell Papillary Renal Cell Carcinoma: Combined Morphologic, Immunohistochemical, and Cytogenetic Analysis.". Am J Surg Pathol 39 (11): 1502-10. doi:10.1097/PAS.0000000000000514. PMID 26457355.
- ↑ Ozcan, A.; Shen, SS.; Zhai, QJ.; Truong, LD. (Aug 2007). "Expression of GLUT1 in primary renal tumors: morphologic and biologic implications.". Am J Clin Pathol 128 (2): 245-54. doi:10.1309/HV6NJVRQKK4QHM9F. PMID 17638658.
- ↑ Hu, H.; Chen, JW.; Xu, KX.; Wang, D.; Wang, Y.; Wang, GW.; Zhang, SY.; Wang, XF. (Aug 2013). "[Expressions of CMTM8 and E-cadherin in primary and metastatic clear cell renal cell carcinoma].". Beijing Da Xue Xue Bao 45 (4): 537-41. PMID 23939157.
- ↑ 17.0 17.1 17.2 Amin MB, Epstein JI, Ulbright TM, et al. (August 2014). "Best practices recommendations in the application of immunohistochemistry in urologic pathology: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): 1017–22. doi:10.1097/PAS.0000000000000254. PMID 25025364.
- ↑ Aguilar-León, D.; Del Ángel-Millán, G.; Zepeda-Quiroz, I.; Soria-Céspedes, D. (Dec 2014). "[Immunohistochemical Expression of CD117 (c-kit) in 75 Renal Cell Tumors].". Gac Med Mex 150 Suppl 2: 156-60. PMID 25643775.
- ↑ 19.0 19.1 Liu, L.; Qian, J.; Singh, H.; Meiers, I.; Zhou, X.; Bostwick, DG. (Aug 2007). "Immunohistochemical analysis of chromophobe renal cell carcinoma, renal oncocytoma, and clear cell carcinoma: an optimal and practical panel for differential diagnosis.". Arch Pathol Lab Med 131 (8): 1290-7. doi:10.1043/1543-2165(2007)131[1290:IAOCRC]2.0.CO;2. PMID 17683191.
- ↑ Al-Ahmadie HA, Alden D, Fine SW, et al. (July 2011). "Role of immunohistochemistry in the evaluation of needle core biopsies in adult renal cortical tumors: an ex vivo study". Am. J. Surg. Pathol. 35 (7): 949–61. doi:10.1097/PAS.0b013e31821e25cd. PMID 21677535.
- ↑ Martignoni G, Gobbo S, Camparo P, et al. (October 2011). "Differential expression of cathepsin K in neoplasms harboring TFE3 gene fusions". Mod. Pathol. 24 (10): 1313–9. doi:10.1038/modpathol.2011.93. PMID 21602817.