Difference between revisions of "Oligodendroglioma"
Jensflorian (talk | contribs) (→Microscopic: DDx intraop) |
|||
| (25 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
| Image = Oligodendroglioma1_high_mag.jpg | | Image = Oligodendroglioma1_high_mag.jpg | ||
| Width = | | Width = | ||
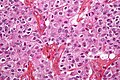
| Caption = Oligodendroglioma. [[H&E stain]]. | | Caption = Oligodendroglioma,IDH mutant and 1p/19q codeleted. [[H&E stain]]. | ||
| Synonyms = | | Synonyms = | ||
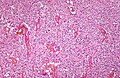
| Micro = highly cellular lesion composed of cells resembling ''fried eggs'' (oligodendrocytes) with a round nucleus (important), distinct cell borders, +/-clear cytoplasm - useful feature (if present), acutely branched capillary sized vessels ("chicken-wire" like appearance), calcifications | | Micro = highly cellular lesion composed of cells resembling ''fried eggs'' (oligodendrocytes) with a round nucleus (important), distinct cell borders, +/-clear cytoplasm - useful feature (if present), acutely branched capillary sized vessels ("chicken-wire" like appearance), calcifications | ||
| Line 11: | Line 11: | ||
| IHC = | | IHC = | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = +/-loss of 1p and 19q (common) | ||
| IF = | | IF = | ||
| Gross = | | Gross = | ||
| Grossing = | | Grossing = | ||
| Site = [[neuropathology tumours]] - | | Site = [[neuropathology tumours]] - cerebral hemispheres, posterior fossa (rare), spinal cord (very rare) | ||
| Assdx = | | Assdx = | ||
| Syndromes = | | Syndromes = | ||
| Line 23: | Line 23: | ||
| Prevalence = | | Prevalence = | ||
| Bloodwork = | | Bloodwork = | ||
| Rads = | | Rads = intra-axial mass, +/-calcifications (best seen on CT), nonenhancing or enhancing | ||
| Endoscopy = | | Endoscopy = | ||
| Prognosis = moderate - dependent on grade | | Prognosis = moderate - dependent on grade | ||
| Line 30: | Line 30: | ||
| Tx = | | Tx = | ||
}} | }} | ||
'''Oligodendroglioma''' is [[CNS tumour]] that is typically in the | '''Oligodendroglioma, IDH mutant and 1p/19q codeleted''' is [[CNS tumour]] that is typically in the cerebral hemispheres. Molecular analysis of IDH1/2 hotspots and LOH1p/19q testing is required for diagnosis. | ||
==General== | ==General== | ||
*Do ''not'' arise from | *Do ''not'' arise from [[oligodendrocyte]]s, although tumor cells look very similiar.<ref>{{Cite journal | last1 = Hartmann | first1 = C. | last2 = von Deimling | first2 = A. | title = Molecular pathology of oligodendroglial tumors. | journal = Recent Results Cancer Res | volume = 171 | issue = | pages = 25-49 | month = | year = 2009 | doi = 10.1007/978-3-540-31206-2_2 | PMID = 19322536 }}</ref> | ||
**Arise from ''glial precursor cells''. | **Arise from ''glial precursor cells''. | ||
Prognosis by flavours (average survival):<ref name=Ref_PSNP98>{{Ref PSNP|98}}</ref> | |||
* | *WHO CNS grade 2: 10-15 years. | ||
* | *WHO CNS grade 3: 3-5 years. | ||
Oligodendrogliomas account for approx 5% of all [[glioma]]s. | |||
* Numbers may be higher when stringent classifiation criteria are not applied. | |||
* Peak incidence: 40-45 years. | |||
* First description of the tumor in 1926. | |||
The fifth edition of WHO classification recognizes two tumor subtypes: | |||
*Oligodendroglioma, IDH-mutant and 1p/19q-codeleted, WHO CNS Grade 2 (ICD-O: 9450/3). | |||
*Oligodendroglioma, IDH-mutant and 1p/19q-codeleted, WHO CNS Grade 3 (ICD-O: 9451/3). | |||
The terminology anaplastic oligodendroglioma or oligoastrocytoma is depreceated. <ref>{{Cite journal | last1 = Louis | first1 = DN. | last2 = Perry | first2 = A. | last3 = Reifenberger | first3 = G. | last4 = von Deimling | first4 = A. | last5 = Figarella-Branger | first5 = D. | last6 = Cavenee | first6 = WK. | last7 = Ohgaki | first7 = H. | last8 = Wiestler | first8 = OD. | last9 = Kleihues | first9 = P. | title = The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. | journal = Acta Neuropathol | volume = 131 | issue = 6 | pages = 803-20 | month = Jun | year = 2016 | doi = 10.1007/s00401-016-1545-1 | PMID = 27157931 }}</ref> | |||
==Gross/radiologic== | |||
* | Location: | ||
* | *Cerebral hemispheres - most often (50-60%) frontal lobe, followed by parietal and temporal lobes.<ref name=Ref_PSNP94>{{Ref PSNP|94}}</ref> | ||
*Posterior fossa (rare). | |||
*Intramedullary spinal cord (very rare). | |||
Radiologic features:<ref name=Ref_PSNP94>{{Ref PSNP|94}}</ref> | |||
*Intra-axial mass. | |||
*+/-Calcifications (best seen on CT). | |||
*Nonenhancing or enhancing. | |||
*Occasionally well-circumscribed. | |||
*Widespread dissemination in a gliomatosis cerebri fashion is very rare (DDx: Diffuse leptomeningeal glioneuronal tumour). | |||
Clinical symptoms: | |||
*Seizures (2/3 of all cases). | |||
*Intracranial pressure. | |||
*Focal neurologic decifits. | |||
*Cognitive changes. | |||
*Incidental finding in 10%. | |||
==Microscopic== | ==Microscopic== | ||
Features: | Features: | ||
*Diffusely growing tumor. | |||
*Highly cellular lesion composed of: | *Highly cellular lesion composed of: | ||
**Cells resembling ''fried eggs'' (oligodendrocytes) with: | **Cells resembling ''fried eggs'' (oligodendrocytes) with: | ||
| Line 56: | Line 84: | ||
***Abundant, delicate appearing; may vaguely resemble a paraganglioma at low power. | ***Abundant, delicate appearing; may vaguely resemble a paraganglioma at low power. | ||
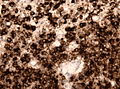
*Calcifications - important feature.<ref>URL: [http://www.emedicine.com/radio/topic481.htm http://www.emedicine.com/radio/topic481.htm].</ref> | *Calcifications - important feature.<ref>URL: [http://www.emedicine.com/radio/topic481.htm http://www.emedicine.com/radio/topic481.htm].</ref> | ||
*Perifocal edema uncommon. | |||
*Few tumors may exhibit [[eosinophilic granular body|eosinophilic granular bodies]]. | |||
*Some tumors may show a [[Polar Spongioblastoma|Spongioblastoma]]-like growth pattern. | |||
Anaplastic (grade 3) criteria:<ref>{{Cite journal | last1 = Giannini | first1 = C. | last2 = Scheithauer | first2 = BW. | last3 = Weaver | first3 = AL. | last4 = Burger | first4 = PC. | last5 = Kros | first5 = JM. | last6 = Mork | first6 = S. | last7 = Graeber | first7 = MB. | last8 = Bauserman | first8 = S. | last9 = Buckner | first9 = JC. | title = Oligodendrogliomas: reproducibility and prognostic value of histologic diagnosis and grading. | journal = J Neuropathol Exp Neurol | volume = 60 | issue = 3 | pages = 248-62 | month = Mar | year = 2001 | doi = | PMID = 11245209 }}</ref> | |||
*"Significant" or "brisk" mitotic activity. | |||
**That means for most neuropathologists >= 6 mitoses per 10 HPF. | |||
*Microvacular proliferation. | |||
*Necrosis. | |||
*Rarely multnucleated cells. | |||
Note: | Note: | ||
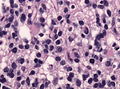
*Tumour cells may be plasmacytoid, i.e. have a [[plasma cell]]-like appearance.<ref name=pmid17284109>{{Cite journal | last1 = Aldape | first1 = K. | last2 = Burger | first2 = PC. | last3 = Perry | first3 = A. | title = Clinicopathologic aspects of 1p/19q loss and the diagnosis of oligodendroglioma. | journal = Arch Pathol Lab Med | volume = 131 | issue = 2 | pages = 242-51 | month = Feb | year = 2007 | doi = 10.1043/1543-2165(2007)131[242:CAOQLA]2.0.CO;2 | PMID = 17284109 | URL = http://www.archivesofpathology.org/doi/full/10.1043/1543-2165(2007)131%5B242:CAOQLA%5D2.0.CO;2 }}</ref> | * The clear cytoplasm around the nucleus is a fixation artefact and not seen in smear, frozen sections or rapid fixation. | ||
* Tumour cells may be plasmacytoid, i.e. have a [[plasma cell]]-like appearance.<ref name=pmid17284109>{{Cite journal | last1 = Aldape | first1 = K. | last2 = Burger | first2 = PC. | last3 = Perry | first3 = A. | title = Clinicopathologic aspects of 1p/19q loss and the diagnosis of oligodendroglioma. | journal = Arch Pathol Lab Med | volume = 131 | issue = 2 | pages = 242-51 | month = Feb | year = 2007 | doi = 10.1043/1543-2165(2007)131[242:CAOQLA]2.0.CO;2 | PMID = 17284109 | URL = http://www.archivesofpathology.org/doi/full/10.1043/1543-2165(2007)131%5B242:CAOQLA%5D2.0.CO;2 }}</ref> | |||
**Also called minigemistocytes. | |||
* | **The are usually strong GFAP+ve. | ||
** | *Few neural tumours have round nuclei - DDx in intraoperative specimen: | ||
*Few neural tumours have round nuclei - DDx: | |||
**Oligodendroglioma. | **Oligodendroglioma. | ||
**[[Lymphoma]]. | **[[Lymphoma]]. | ||
| Line 75: | Line 110: | ||
Image:Oligodendroglioma1_high_mag.jpg | Oligodendroglioma high mag. (WC) | Image:Oligodendroglioma1_high_mag.jpg | Oligodendroglioma high mag. (WC) | ||
Image:Oligodendroglioma1_low_mag.jpg | Oligodendroglioma low mag. (WC) | Image:Oligodendroglioma1_low_mag.jpg | Oligodendroglioma low mag. (WC) | ||
File:Oligodendroglioma_discrete_invasion_HE.jpg | Discrete invasion in a oligodendroglioma. (WC/jensflorian) | |||
File:Anaplastic_oligodendroglioma_minigemistocytes.jpg | Minigemistocytes and mitoses. (WC/jensflorian) | |||
MAP2_anaplastic_oligodendroglioma.jpg | Perinuclear [[MAP2]] immunoreactivity in oligodendroglioma. (WC/jensflorian) | |||
File:IDH1_R132H_in_anaplastic_ologodendroglioma.jpg | Demonstration of [[IDH-1|IDH1 R132H]] mutation in oligodendroglioma. (WC/jensflorian) | |||
</gallery> | </gallery> | ||
www: | www: | ||
*[http://path.upmc.edu/cases/case713.html Oligodendroglioma - several images (upmc.edu)]. | *[http://path.upmc.edu/cases/case713.html Oligodendroglioma - several images (upmc.edu)]. | ||
| Line 82: | Line 122: | ||
===Histologic grading=== | ===Histologic grading=== | ||
Come in two flavours: | Come in two flavours: | ||
# WHO grade | # WHO CNS grade 2 | ||
#*This is most oligodendrogliomas. | #*This is most oligodendrogliomas. | ||
# WHO grade | #*Without genetic testing for [[IDH-1]]/2 and LOH 1p/19q, the tumor is called Oligodendroglioma, NOS. | ||
# WHO CNS grade 3 | |||
#*Features for calling high grade:<ref name=Ref_PSNP98>{{Ref PSNP|98}}</ref> | #*Features for calling high grade:<ref name=Ref_PSNP98>{{Ref PSNP|98}}</ref> | ||
#**Endothelial hypertrophy. | #**Endothelial hypertrophy. | ||
#***Plump/large endothelial cells. | #***Plump/large endothelial cells. | ||
#**Necrosis. | #**Necrosis. | ||
#**High mitotic rate (6 mitoses/10 HPF for | #**High mitotic rate (6 or more mitoses/10 HPF of 0.55mm²). | ||
#*Without genetic testing for [[IDH-1]]/2 and LOH 1p/19q, the tumor is called Anaplastic oligodendroglioma, NOS. | |||
==IHC== | ==IHC== | ||
Features: | Features: | ||
* | *[[MAP2]] +ve.<reF name=pmid12025943>{{cite journal |author=Suzuki SO, Kitai R, Llena J, Lee SC, Goldman JE, Shafit-Zagardo B |title=MAP-2e, a novel MAP-2 isoform, is expressed in gliomas and delineates tumor architecture and patterns of infiltration |journal=J. Neuropathol. Exp. Neurol. |volume=61 |issue=5 |pages=403–12 |year=2002 |month=May |pmid=12025943 |doi= |url=}}</ref> | ||
*GFAP | *GFAP +ve (variable). | ||
**Some subtypes +ve - should not be used to distinguish.<ref name=Ref_PSNP>{{Ref PSNP|98}}</ref> | **Some subtypes +ve - should not be used to distinguish.<ref name=Ref_PSNP>{{Ref PSNP|98}}</ref> | ||
*EMA +ve. | *EMA +ve. | ||
*IDH-1 | *IDH-1 (R132H) +ve (approx 85%). | ||
* | **18% +ve in one series of children,<ref name=pmid24805856>{{Cite journal | last1 = Rodriguez | first1 = FJ. | last2 = Tihan | first2 = T. | last3 = Lin | first3 = D. | last4 = McDonald | first4 = W. | last5 = Nigro | first5 = J. | last6 = Feuerstein | first6 = B. | last7 = Jackson | first7 = S. | last8 = Cohen | first8 = K. | last9 = Burger | first9 = PC. | title = Clinicopathologic features of pediatric oligodendrogliomas: a series of 50 patients. | journal = Am J Surg Pathol | volume = 38 | issue = 8 | pages = 1058-70 | month = Aug | year = 2014 | doi = 10.1097/PAS.0000000000000221 | PMID = 24805856 }}</ref> 23% +ve in another series.<ref name=pmid23361281>{{Cite journal | last1 = Sipayya | first1 = V. | last2 = Sharma | first2 = I. | last3 = Sharma | first3 = KC. | last4 = Singh | first4 = A. | title = Immunohistochemical expression of IDH1 in gliomas: a tissue microarray-based approach. | journal = J Cancer Res Ther | volume = 8 | issue = 4 | pages = 598-601 | month = | year = | doi = 10.4103/0973-1482.106567 | PMID = 23361281 }}</ref> | ||
**Useful for differentiating ''astrocytoma'' vs. ''oligodendroglioma''. | *ATRX +ve (nuclear retention). | ||
*Ki-67. | **Useful for differentiating ''astrocytoma'' vs. ''oligodendroglioma''.<ref>{{Cite journal | last1 = Reuss | first1 = DE. | last2 = Sahm | first2 = F. | last3 = Schrimpf | first3 = D. | last4 = Wiestler | first4 = B. | last5 = Capper | first5 = D. | last6 = Koelsche | first6 = C. | last7 = Schweizer | first7 = L. | last8 = Korshunov | first8 = A. | last9 = Jones | first9 = DT. | title = ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an "integrated" diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma. | journal = Acta Neuropathol | volume = 129 | issue = 1 | pages = 133-46 | month = Jan | year = 2015 | doi = 10.1007/s00401-014-1370-3 | PMID = 25427834 }}</ref> | ||
*H3K27me3 -ve (nuclear loss).<ref>{{Cite journal | last1 = Filipski | first1 = K. | last2 = Braun | first2 = Y. | last3 = Zinke | first3 = J. | last4 = Roller | first4 = B. | last5 = Baumgarten | first5 = P. | last6 = Wagner | first6 = M. | last7 = Senft | first7 = C. | last8 = Zeiner | first8 = PS. | last9 = Ronellenfitsch | first9 = MW. | title = Lack of H3K27 trimethylation is associated with 1p/19q codeletion in diffuse gliomas. | journal = Acta Neuropathol | volume = | issue = | pages = | month = May | year = 2019 | doi = 10.1007/s00401-019-02025-9 | PMID = 31065834 }}</ref> | |||
*SOX10 +ve (up to 80%).<ref>{{Cite journal | last1 = Bannykh | first1 = SI. | last2 = Stolt | first2 = CC. | last3 = Kim | first3 = J. | last4 = Perry | first4 = A. | last5 = Wegner | first5 = M. | title = Oligodendroglial-specific transcriptional factor SOX10 is ubiquitously expressed in human gliomas. | journal = J Neurooncol | volume = 76 | issue = 2 | pages = 115-27 | month = Jan | year = 2006 | doi = 10.1007/s11060-005-5533-x | PMID = 16205963 }}</ref> | |||
*Olig2 +ve. | |||
*H3 K27me3 nuclear loss in most cases. | |||
*NOGO-A often +ve. | |||
*p53 -ve or low expressed. | |||
*Ki-67 (usu. >5% in CNS grade 2). | |||
*May have neuronal "islands" (Synapto +ve, NeuN +ve). | |||
==Molecular pathology== | ==Molecular pathology== | ||
Combined losses of 1p and 19q both and presence of IDH1 mutation in codon 132 or IDH2 mutation in codon 172 is required for final diagnosis and is prognostic and therapeutic relevant:<ref name=pmid18565359>{{cite journal |author=Fontaine D, Vandenbos F, Lebrun C, Paquis V, Frenay M |title=[Diagnostic and prognostic values of 1p and 19q deletions in adult gliomas: critical review of the literature and implications in daily clinical practice] |language=French |journal=Rev. Neurol. (Paris) |volume=164 |issue=6-7 |pages=595–604 |year=2008 |pmid=18565359 |doi=10.1016/j.neurol.2008.04.002 |url=}}</ref><ref>{{Cite journal | last1 = Wiestler | first1 = B. | last2 = Capper | first2 = D. | last3 = Hovestadt | first3 = V. | last4 = Sill | first4 = M. | last5 = Jones | first5 = DT. | last6 = Hartmann | first6 = C. | last7 = Felsberg | first7 = J. | last8 = Platten | first8 = M. | last9 = Feiden | first9 = W. | title = Assessing CpG island methylator phenotype, 1p/19q codeletion, and MGMT promoter methylation from epigenome-wide data in the biomarker cohort of the NOA-04 trial. | journal = Neuro Oncol | volume = 16 | issue = 12 | pages = 1630-8 | month = Dec | year = 2014 | doi = 10.1093/neuonc/nou138 | PMID = 25028501 }}</ref><ref>{{Cite journal | last1 = Cairncross | first1 = G. | last2 = Wang | first2 = M. | last3 = Shaw | first3 = E. | last4 = Jenkins | first4 = R. | last5 = Brachman | first5 = D. | last6 = Buckner | first6 = J. | last7 = Fink | first7 = K. | last8 = Souhami | first8 = L. | last9 = Laperriere | first9 = N. | title = Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. | journal = J Clin Oncol | volume = 31 | issue = 3 | pages = 337-43 | month = Jan | year = 2013 | doi = 10.1200/JCO.2012.43.2674 | PMID = 23071247 }}</ref> | |||
*Greater chemosensitivity | *Greater chemosensitivity to PCV regimen.<ref>{{Cite journal | last1 = Cairncross | first1 = G. | last2 = Wang | first2 = M. | last3 = Shaw | first3 = E. | last4 = Jenkins | first4 = R. | last5 = Brachman | first5 = D. | last6 = Buckner | first6 = J. | last7 = Fink | first7 = K. | last8 = Souhami | first8 = L. | last9 = Laperriere | first9 = N. | title = Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. | journal = J Clin Oncol | volume = 31 | issue = 3 | pages = 337-43 | month = Jan | year = 2013 | doi = 10.1200/JCO.2012.43.2674 | PMID = 23071247 }}</ref> | ||
*Better prognosis. | *Better prognosis compared to astrocytic tumors.<ref>{{Cite journal | last1 = Mur | first1 = P. | last2 = Mollejo | first2 = M. | last3 = Ruano | first3 = Y. | last4 = de Lope | first4 = ÁR. | last5 = Fiaño | first5 = C. | last6 = García | first6 = JF. | last7 = Castresana | first7 = JS. | last8 = Hernández-Laín | first8 = A. | last9 = Rey | first9 = JA. | title = Codeletion of 1p and 19q determines distinct gene methylation and expression profiles in IDH-mutated oligodendroglial tumors. | journal = Acta Neuropathol | volume = 126 | issue = 2 | pages = 277-89 | month = Aug | year = 2013 | doi = 10.1007/s00401-013-1130-9 | PMID = 23689617 }}</ref> | ||
*TERT promotor mutation present. | |||
*CDKN2A homozygoud deletion in <10% of grade 3 tumours. | |||
Note: If molecular testing fails, cases should be classified as Oligodendroglioma, NOS. | |||
DDx: | |||
*[[Neurocytoma]] also have perinuclear clearing and well-defined cellular borders. | |||
**Pineocytomatous/neurocytic rosettes = (irregular) rosette with a large meshwork of fibers (neuropil) at the centre. | |||
*Clear cell [[ependymoma]]. | |||
*[[Dysembryoplastic neuroepithelial tumour]]. | |||
*Oligodendroglial-like cells in [[Pilocytic astrocytoma]]. | |||
*Clear cell [[meningioma]]. (EMA +ve) | |||
*Clear cell renal carcinoma. (Pan-CK +ve) | |||
*Demyelinisation. | |||
* [[Astrocytoma]] | |||
** [[IDH-1]] mutant, but non-codeleted tumors with oligodendrogliom histologye are no longer classified as oligodendrogliomas on molecular basis. These tumors are classified as IDH-mutant astrocytoma. | |||
* Diffuse leptomeningeal glioneuronal tumour (1p/19q codeletion present, but IDH wildtype) | |||
Note: | |||
*Consider Glioblastoma with oligo features when tumor is IDH1/2 wildtype and has no LOH 1p/19q and no ATRX loss. | |||
*Dual-genotype astrocytoma/oligodendroglioma are very rare. | |||
==See also== | ==See also== | ||
| Line 116: | Line 187: | ||
[[Category:Neuropathology tumours]] | [[Category:Neuropathology tumours]] | ||
[[Category:Diagnosis]] | [[Category:Diagnosis]] | ||
[[Category:WHO grade II tumours]] | |||
Latest revision as of 09:32, 6 April 2022
| Oligodendroglioma | |
|---|---|
| Diagnosis in short | |
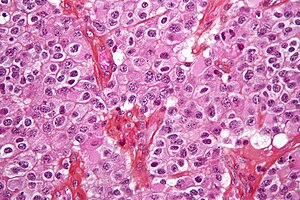 Oligodendroglioma,IDH mutant and 1p/19q codeleted. H&E stain. | |
|
| |
| LM | highly cellular lesion composed of cells resembling fried eggs (oligodendrocytes) with a round nucleus (important), distinct cell borders, +/-clear cytoplasm - useful feature (if present), acutely branched capillary sized vessels ("chicken-wire" like appearance), calcifications |
| LM DDx | neurocytoma, clear cell variant of ependymoma, seminoma / dysgerminoma / germinoma |
| Molecular | +/-loss of 1p and 19q (common) |
| Site | neuropathology tumours - cerebral hemispheres, posterior fossa (rare), spinal cord (very rare) |
|
| |
| Radiology | intra-axial mass, +/-calcifications (best seen on CT), nonenhancing or enhancing |
| Prognosis | moderate - dependent on grade |
Oligodendroglioma, IDH mutant and 1p/19q codeleted is CNS tumour that is typically in the cerebral hemispheres. Molecular analysis of IDH1/2 hotspots and LOH1p/19q testing is required for diagnosis.
General
- Do not arise from oligodendrocytes, although tumor cells look very similiar.[1]
- Arise from glial precursor cells.
Prognosis by flavours (average survival):[2]
- WHO CNS grade 2: 10-15 years.
- WHO CNS grade 3: 3-5 years.
Oligodendrogliomas account for approx 5% of all gliomas.
- Numbers may be higher when stringent classifiation criteria are not applied.
- Peak incidence: 40-45 years.
- First description of the tumor in 1926.
The fifth edition of WHO classification recognizes two tumor subtypes:
- Oligodendroglioma, IDH-mutant and 1p/19q-codeleted, WHO CNS Grade 2 (ICD-O: 9450/3).
- Oligodendroglioma, IDH-mutant and 1p/19q-codeleted, WHO CNS Grade 3 (ICD-O: 9451/3).
The terminology anaplastic oligodendroglioma or oligoastrocytoma is depreceated. [3]
Gross/radiologic
Location:
- Cerebral hemispheres - most often (50-60%) frontal lobe, followed by parietal and temporal lobes.[4]
- Posterior fossa (rare).
- Intramedullary spinal cord (very rare).
Radiologic features:[4]
- Intra-axial mass.
- +/-Calcifications (best seen on CT).
- Nonenhancing or enhancing.
- Occasionally well-circumscribed.
- Widespread dissemination in a gliomatosis cerebri fashion is very rare (DDx: Diffuse leptomeningeal glioneuronal tumour).
Clinical symptoms:
- Seizures (2/3 of all cases).
- Intracranial pressure.
- Focal neurologic decifits.
- Cognitive changes.
- Incidental finding in 10%.
Microscopic
Features:
- Diffusely growing tumor.
- Highly cellular lesion composed of:
- Cells resembling fried eggs (oligodendrocytes) with:
- Round nucleus - key feature.
- Distinct cell borders.
- Moderate-to-marked nuclear atypia.
- Clear cytoplasm - useful feature (if present).
- Some oligodendrogliomas have eosinophilic cytoplasm with focal perinuclear clearing.
- Acutely branched capillary sized vessels - "chicken-wire" like appearance.
- Abundant, delicate appearing; may vaguely resemble a paraganglioma at low power.
- Cells resembling fried eggs (oligodendrocytes) with:
- Calcifications - important feature.[5]
- Perifocal edema uncommon.
- Few tumors may exhibit eosinophilic granular bodies.
- Some tumors may show a Spongioblastoma-like growth pattern.
Anaplastic (grade 3) criteria:[6]
- "Significant" or "brisk" mitotic activity.
- That means for most neuropathologists >= 6 mitoses per 10 HPF.
- Microvacular proliferation.
- Necrosis.
- Rarely multnucleated cells.
Note:
- The clear cytoplasm around the nucleus is a fixation artefact and not seen in smear, frozen sections or rapid fixation.
- Tumour cells may be plasmacytoid, i.e. have a plasma cell-like appearance.[7]
- Also called minigemistocytes.
- The are usually strong GFAP+ve.
- Few neural tumours have round nuclei - DDx in intraoperative specimen:
- Oligodendroglioma.
- Lymphoma.
- Clear cell variant of ependymoma.
- Germ cell tumour (germinoma/dysgerminoma/seminoma).
Images
Perinuclear MAP2 immunoreactivity in oligodendroglioma. (WC/jensflorian)
Demonstration of IDH1 R132H mutation in oligodendroglioma. (WC/jensflorian)
www:
- Oligodendroglioma - several images (upmc.edu).
- Oligodendroglioma with plasmacytoid cells (frontalcortex.com).
Histologic grading
Come in two flavours:
- WHO CNS grade 2
- This is most oligodendrogliomas.
- Without genetic testing for IDH-1/2 and LOH 1p/19q, the tumor is called Oligodendroglioma, NOS.
- WHO CNS grade 3
IHC
Features:
- MAP2 +ve.[8]
- GFAP +ve (variable).
- Some subtypes +ve - should not be used to distinguish.[9]
- EMA +ve.
- IDH-1 (R132H) +ve (approx 85%).
- ATRX +ve (nuclear retention).
- Useful for differentiating astrocytoma vs. oligodendroglioma.[12]
- H3K27me3 -ve (nuclear loss).[13]
- SOX10 +ve (up to 80%).[14]
- Olig2 +ve.
- H3 K27me3 nuclear loss in most cases.
- NOGO-A often +ve.
- p53 -ve or low expressed.
- Ki-67 (usu. >5% in CNS grade 2).
- May have neuronal "islands" (Synapto +ve, NeuN +ve).
Molecular pathology
Combined losses of 1p and 19q both and presence of IDH1 mutation in codon 132 or IDH2 mutation in codon 172 is required for final diagnosis and is prognostic and therapeutic relevant:[15][16][17]
- Greater chemosensitivity to PCV regimen.[18]
- Better prognosis compared to astrocytic tumors.[19]
- TERT promotor mutation present.
- CDKN2A homozygoud deletion in <10% of grade 3 tumours.
Note: If molecular testing fails, cases should be classified as Oligodendroglioma, NOS.
DDx:
- Neurocytoma also have perinuclear clearing and well-defined cellular borders.
- Pineocytomatous/neurocytic rosettes = (irregular) rosette with a large meshwork of fibers (neuropil) at the centre.
- Clear cell ependymoma.
- Dysembryoplastic neuroepithelial tumour.
- Oligodendroglial-like cells in Pilocytic astrocytoma.
- Clear cell meningioma. (EMA +ve)
- Clear cell renal carcinoma. (Pan-CK +ve)
- Demyelinisation.
- Astrocytoma
- IDH-1 mutant, but non-codeleted tumors with oligodendrogliom histologye are no longer classified as oligodendrogliomas on molecular basis. These tumors are classified as IDH-mutant astrocytoma.
- Diffuse leptomeningeal glioneuronal tumour (1p/19q codeletion present, but IDH wildtype)
Note:
- Consider Glioblastoma with oligo features when tumor is IDH1/2 wildtype and has no LOH 1p/19q and no ATRX loss.
- Dual-genotype astrocytoma/oligodendroglioma are very rare.
See also
References
- ↑ Hartmann, C.; von Deimling, A. (2009). "Molecular pathology of oligodendroglial tumors.". Recent Results Cancer Res 171: 25-49. doi:10.1007/978-3-540-31206-2_2. PMID 19322536.
- ↑ 2.0 2.1 Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 98. ISBN 978-0443069826.
- ↑ Louis, DN.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, WK.; Ohgaki, H.; Wiestler, OD. et al. (Jun 2016). "The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary.". Acta Neuropathol 131 (6): 803-20. doi:10.1007/s00401-016-1545-1. PMID 27157931.
- ↑ 4.0 4.1 Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 94. ISBN 978-0443069826.
- ↑ URL: http://www.emedicine.com/radio/topic481.htm.
- ↑ Giannini, C.; Scheithauer, BW.; Weaver, AL.; Burger, PC.; Kros, JM.; Mork, S.; Graeber, MB.; Bauserman, S. et al. (Mar 2001). "Oligodendrogliomas: reproducibility and prognostic value of histologic diagnosis and grading.". J Neuropathol Exp Neurol 60 (3): 248-62. PMID 11245209.
- ↑ Aldape, K.; Burger, PC.; Perry, A. (Feb 2007). "Clinicopathologic aspects of 1p/19q loss and the diagnosis of oligodendroglioma.". Arch Pathol Lab Med 131 (2): 242-51. doi:10.1043/1543-2165(2007)131[242:CAOQLA]2.0.CO;2. PMID 17284109.
- ↑ Suzuki SO, Kitai R, Llena J, Lee SC, Goldman JE, Shafit-Zagardo B (May 2002). "MAP-2e, a novel MAP-2 isoform, is expressed in gliomas and delineates tumor architecture and patterns of infiltration". J. Neuropathol. Exp. Neurol. 61 (5): 403–12. PMID 12025943.
- ↑ Perry, Arie; Brat, Daniel J. (2010). Practical Surgical Neuropathology: A Diagnostic Approach: A Volume in the Pattern Recognition series (1st ed.). Churchill Livingstone. pp. 98. ISBN 978-0443069826.
- ↑ Rodriguez, FJ.; Tihan, T.; Lin, D.; McDonald, W.; Nigro, J.; Feuerstein, B.; Jackson, S.; Cohen, K. et al. (Aug 2014). "Clinicopathologic features of pediatric oligodendrogliomas: a series of 50 patients.". Am J Surg Pathol 38 (8): 1058-70. doi:10.1097/PAS.0000000000000221. PMID 24805856.
- ↑ Sipayya, V.; Sharma, I.; Sharma, KC.; Singh, A.. "Immunohistochemical expression of IDH1 in gliomas: a tissue microarray-based approach.". J Cancer Res Ther 8 (4): 598-601. doi:10.4103/0973-1482.106567. PMID 23361281.
- ↑ Reuss, DE.; Sahm, F.; Schrimpf, D.; Wiestler, B.; Capper, D.; Koelsche, C.; Schweizer, L.; Korshunov, A. et al. (Jan 2015). "ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an "integrated" diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma.". Acta Neuropathol 129 (1): 133-46. doi:10.1007/s00401-014-1370-3. PMID 25427834.
- ↑ Filipski, K.; Braun, Y.; Zinke, J.; Roller, B.; Baumgarten, P.; Wagner, M.; Senft, C.; Zeiner, PS. et al. (May 2019). "Lack of H3K27 trimethylation is associated with 1p/19q codeletion in diffuse gliomas.". Acta Neuropathol. doi:10.1007/s00401-019-02025-9. PMID 31065834.
- ↑ Bannykh, SI.; Stolt, CC.; Kim, J.; Perry, A.; Wegner, M. (Jan 2006). "Oligodendroglial-specific transcriptional factor SOX10 is ubiquitously expressed in human gliomas.". J Neurooncol 76 (2): 115-27. doi:10.1007/s11060-005-5533-x. PMID 16205963.
- ↑ Fontaine D, Vandenbos F, Lebrun C, Paquis V, Frenay M (2008). "[Diagnostic and prognostic values of 1p and 19q deletions in adult gliomas: critical review of the literature and implications in daily clinical practice]" (in French). Rev. Neurol. (Paris) 164 (6-7): 595–604. doi:10.1016/j.neurol.2008.04.002. PMID 18565359.
- ↑ Wiestler, B.; Capper, D.; Hovestadt, V.; Sill, M.; Jones, DT.; Hartmann, C.; Felsberg, J.; Platten, M. et al. (Dec 2014). "Assessing CpG island methylator phenotype, 1p/19q codeletion, and MGMT promoter methylation from epigenome-wide data in the biomarker cohort of the NOA-04 trial.". Neuro Oncol 16 (12): 1630-8. doi:10.1093/neuonc/nou138. PMID 25028501.
- ↑ Cairncross, G.; Wang, M.; Shaw, E.; Jenkins, R.; Brachman, D.; Buckner, J.; Fink, K.; Souhami, L. et al. (Jan 2013). "Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402.". J Clin Oncol 31 (3): 337-43. doi:10.1200/JCO.2012.43.2674. PMID 23071247.
- ↑ Cairncross, G.; Wang, M.; Shaw, E.; Jenkins, R.; Brachman, D.; Buckner, J.; Fink, K.; Souhami, L. et al. (Jan 2013). "Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402.". J Clin Oncol 31 (3): 337-43. doi:10.1200/JCO.2012.43.2674. PMID 23071247.
- ↑ Mur, P.; Mollejo, M.; Ruano, Y.; de Lope, ÁR.; Fiaño, C.; García, JF.; Castresana, JS.; Hernández-Laín, A. et al. (Aug 2013). "Codeletion of 1p and 19q determines distinct gene methylation and expression profiles in IDH-mutated oligodendroglial tumors.". Acta Neuropathol 126 (2): 277-89. doi:10.1007/s00401-013-1130-9. PMID 23689617.