Difference between revisions of "Plasma cell neoplasms"
Jump to navigation
Jump to search
m (→Microscopic) |
|||
| (12 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
'''Plasma cell neoplasms''' arise from [[plasma cell]]s. They are encountered by anatomical pathologists on occasion. | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
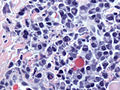
| Image = Plasma cell neoplasm -- very high mag.jpg | |||
| Width = | |||
| Caption = Plasma cell neoplasm. [[H&E stain]] | |||
| Synonyms = | |||
| Micro = dyscohesive plasmacytoid cells (abundant cytoplasm, eccentrically placed nucleus), often prominent perinuclear hof, +/-nucleoli, +/-Russell bodies, +/-Dutcher bodies | |||
| Subtypes = | |||
| LMDDx = [[lymphoplasmacytic lymphoma]], [[neuroendocrine carcinoma]], poorly differentiated carcinoma, others | |||
| Stains = | |||
| IHC = [[CD138]] +ve, CD56 +ve, CD45 -ve/+ve, CD79a +ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[bone]] - [[bone marrow]] | |||
| Assdx = [[renal failure]], [[myeloma cast nephropathy]] | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = | |||
| Bloodwork = +/-[[anemia]], +/-hypercalcemia | |||
| Rads = +/-lytic bone lesions | |||
| Endoscopy = | |||
| Prognosis = poor | |||
| Other = | |||
| ClinDDx = [[metastatic disease]] | |||
| Tx = | |||
}} | |||
'''Plasma cell neoplasms''' arise from [[plasma cell]]s. They are encountered by anatomical pathologists on occasion. | |||
''Plasma cell myeloma'', and ''plasmacytoma'' (solitary myeloma)<ref name=Ref_PCPBoD8_324>{{Ref PCPBoD8|324}}</ref> redirect to this article. | |||
==General== | ==General== | ||
| Line 41: | Line 72: | ||
*Russell bodies: | *Russell bodies: | ||
**Eosinophilic, large (10-15 micrometres), homogenous immunoglobulin-containing inclusions. | **Eosinophilic, large (10-15 micrometres), homogenous immunoglobulin-containing inclusions. | ||
*Dutcher bodies - intranuclear crystalline rods. | *Dutcher bodies - intranuclear crystalline rods. | ||
**Dutcher bodies are ''PAS stain'' +ve.<ref>URL: [http://www.thefreelibrary.com/Dutcher+bodies+in+chronic+synovitis-a083551789 http://www.thefreelibrary.com/Dutcher+bodies+in+chronic+synovitis-a083551789]. Accessed on: 4 August 2010.</ref> | **Dutcher bodies are ''PAS stain'' +ve.<ref>URL: [http://www.thefreelibrary.com/Dutcher+bodies+in+chronic+synovitis-a083551789 http://www.thefreelibrary.com/Dutcher+bodies+in+chronic+synovitis-a083551789]. Accessed on: 4 August 2010.</ref> | ||
*Prominent ''perinuclear hof'' - cytoplasmic crescent shaped lucency adjacent to the nuclear membrane (due to large Golgi apparatus); nucleus has a [http://en.wikipedia.org/wiki/Bib_%28garment%29 "bib"]. | *Prominent ''perinuclear hof'' - cytoplasmic crescent shaped lucency adjacent to the nuclear membrane (due to large Golgi apparatus); nucleus has a [http://en.wikipedia.org/wiki/Bib_%28garment%29 "bib"]. | ||
DDx: | DDx: | ||
| Line 57: | Line 81: | ||
*[[Lymphoplasmacytic lymphoma]] ([[AKA]] Waldenström's macroglobulinemia). | *[[Lymphoplasmacytic lymphoma]] ([[AKA]] Waldenström's macroglobulinemia). | ||
*[[Syphilis]]. | *[[Syphilis]]. | ||
===Images=== | |||
=====Case===== | |||
<gallery> | |||
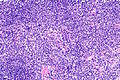
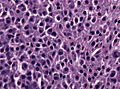
Image: Plasma cell neoplasm -- low mag.jpg | PCN - low mag. | |||
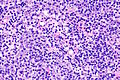
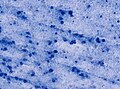
Image: Plasma cell neoplasm -- intermed mag.jpg | PCN - intermed. mag. | |||
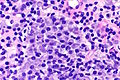
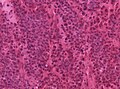
Image: Plasma cell neoplasm -- high mag.jpg | PCN - high mag. | |||
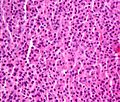
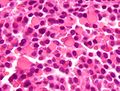
Image: Plasma cell neoplasm -- very high mag.jpg | PCN - very high mag. | |||
</gallery> | |||
=====Other cases===== | |||
<gallery> | |||
Image:Plasmacytoma1.jpg | Plasmacytoma. (WC) | |||
File:Plasmocytoma HE high mag.jpg | Skull base plasmacytoma, higher magnification (WC/jensflorian) | |||
File:Plasmocytoma_frozen_HE_x200.jpg | Plasmacytoma smear (WC/jensflorian) | |||
File:Plasmocytoma_smear_mann_x200.jpg | Leptomeningeal plasmacytoma, frozen section (WC/jensflorian) | |||
</gallery> | |||
=====www===== | |||
*[http://ashimagebank.hematologylibrary.org/cgi/content/full/2004/0126/100984 Various images (hematologylibrary.org)]. | |||
*[http://path.upmc.edu/cases/case515/images/fig05.jpg Multiple myeloma (upmc.edu)].<ref>URL: [http://path.upmc.edu/cases/case515.html http://path.upmc.edu/cases/case515.html]. Accessed on: 25 January 2012.</ref> | |||
====Russell bodies==== | |||
<gallery> | |||
Image:Russell_bodies_2_high_mag_mini.jpg | Russell bodies. (WC) | |||
</gallery> | |||
=====www===== | |||
*[http://www.healthsystem.virginia.edu/internet/hematology/hessimages/russell-bodies-website-arrow.jpg Russell bodies (healthsystem.virginia.edu)]. | |||
*[http://www.pathguy.com/lectures/russ2.jpg Russell bodies - several in one cell (pathguy.com)]. | |||
====Dutcher bodies==== | |||
<gallery> | |||
Image: Dutcher and Russell bodies.jpg | Dutcher bodies and Russell bodies. (WC/Gabriel Caponetti) | |||
</gallery> | |||
==IHC== | ==IHC== | ||
*[[CD138]] +ve. | |||
*[[CD56]] +ve.<ref>URL: [http://www.ncbi.nlm.nih.gov/omim/116930 http://www.ncbi.nlm.nih.gov/omim/116930]. Accessed on: 31 August 2010.</ref> | |||
**Also +ve in NK/T cell lymphomas. | |||
*Kappa -- usu. slightly stronger than lambda. | *Kappa -- usu. slightly stronger than lambda. | ||
*Lambda. | *Lambda. | ||
*CD57. | *CD57. | ||
**Also +ve in [[T-cell large granular lymphocytic leukemia]].<ref>URL: [http://www.nature.com/bmt/journal/v33/n1/full/1704298a.html http://www.nature.com/bmt/journal/v33/n1/full/1704298a.html]. Accessed on: 31 August 2010.</ref> | **Also +ve in [[T-cell large granular lymphocytic leukemia]].<ref>URL: [http://www.nature.com/bmt/journal/v33/n1/full/1704298a.html http://www.nature.com/bmt/journal/v33/n1/full/1704298a.html]. Accessed on: 31 August 2010.</ref> | ||
* | *CD38 +ve.<ref>{{Cite journal | last1 = Tamamori | first1 = T. | last2 = Nakayama | first2 = F. | last3 = Sugimoto | first3 = H. | last4 = Fenxiang | first4 = J. | last5 = Iwatsuki | first5 = K. | last6 = Takigawa | first6 = M. | title = Extramedullary plasmacytoma: cytological and genotypic studies. | journal = Br J Dermatol | volume = 129 | issue = 4 | pages = 468-72 | month = Oct | year = 1993 | doi = | PMID = 8217765 }}</ref> | ||
* | |||
Others:<ref>URL: [http://e-immunohistochemistry.info/web/Plasmacytoma_plasma_cell_myeloma.htm http://e-immunohistochemistry.info/web/Plasmacytoma_plasma_cell_myeloma.htm]. Accessed on: 9 November 2015.</ref> | |||
*CD79a +ve. | |||
*CD45 -ve/+ve. | |||
*CD10 -ve. | |||
*CD5 -ve. | |||
*Cyclin D1 -ve/+ve. | |||
A panel:<!-- need a good panel - maybe here http://clincancerres.aacrjournals.org/content/15/2/714.full or here http://e-immunohistochemistry.info/web/Plasmacytoma_plasma_cell_myeloma.htm --> | |||
*CD3, CD20, CD56, CD117, CD138, IG-kappa (plasma), IG-lambda (plasma). | |||
==Molecular== | ==Molecular== | ||
Latest revision as of 17:22, 12 December 2016
| Plasma cell neoplasms | |
|---|---|
| Diagnosis in short | |
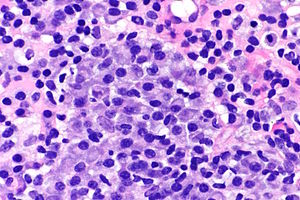 Plasma cell neoplasm. H&E stain | |
|
| |
| LM | dyscohesive plasmacytoid cells (abundant cytoplasm, eccentrically placed nucleus), often prominent perinuclear hof, +/-nucleoli, +/-Russell bodies, +/-Dutcher bodies |
| LM DDx | lymphoplasmacytic lymphoma, neuroendocrine carcinoma, poorly differentiated carcinoma, others |
| IHC | CD138 +ve, CD56 +ve, CD45 -ve/+ve, CD79a +ve |
| Site | bone - bone marrow |
|
| |
| Associated Dx | renal failure, myeloma cast nephropathy |
| Blood work | +/-anemia, +/-hypercalcemia |
| Radiology | +/-lytic bone lesions |
| Prognosis | poor |
| Clin. DDx | metastatic disease |
Plasma cell neoplasms arise from plasma cells. They are encountered by anatomical pathologists on occasion.
Plasma cell myeloma, and plasmacytoma (solitary myeloma)[1] redirect to this article.
General
- Malignancy derived from the plasma cells.
- Prognosis: poor.
- Common primary bone tumour in adults.
Clinical:[2]
- Bence Jones protein (urine).
- Abnormal protein electrophoresis (monoclonal gammopathy, dysproteinemia, paraproteinemia).
Note:
- Plasmacytoma = histology of multiple myeloma; to diagnose multiple myeloma other (non-pathology) criteria are needed.
Classified by site:
- Medullary.
- Extramedullary - usu. upper aerodigestive tract.[3]
Multiple myeloma
Diagnosis requires the following:[4]
- Clonal plasma cells. Must >10% if on bone marrow biopsy.
- Monoclonal protein, i.e. paraprotein, in serum or urine.
- End-organ damage thought to be due to the neoplasm - mnemonic CARL:
- Calcium (in the serum) is elevated.
- Anemia.
- Renal failure.
- Lytic bone lesions.
Note:
- CRAB (calclium, renal failure, anemia, bony lesions) is another mnemonic.[5]
Microscopic
Features (plasmacytoma):
- Abundant eosinophilic cytoplasm.
- Eccentrically placed nucleus.
- Usually with "clock face" morphology.
- "Clock face" morphology = chromatin clumps around the edge of the nucleus, like the numbers on a clock face.
- May have nucleoli.
- Usually with "clock face" morphology.
- Russell bodies:
- Eosinophilic, large (10-15 micrometres), homogenous immunoglobulin-containing inclusions.
- Dutcher bodies - intranuclear crystalline rods.
- Dutcher bodies are PAS stain +ve.[6]
- Prominent perinuclear hof - cytoplasmic crescent shaped lucency adjacent to the nuclear membrane (due to large Golgi apparatus); nucleus has a "bib".
DDx:
- Neuroendocrine carcinoma - nucleus often has a plasmacytoid (plasma cell-like) appearance.
- Lymphoplasmacytic lymphoma (AKA Waldenström's macroglobulinemia).
- Syphilis.
Images
Case
Other cases
www
Russell bodies
www
Dutcher bodies
IHC
- CD138 +ve.
- CD56 +ve.[8]
- Also +ve in NK/T cell lymphomas.
- Kappa -- usu. slightly stronger than lambda.
- Lambda.
- CD57.
- Also +ve in T-cell large granular lymphocytic leukemia.[9]
- CD38 +ve.[10]
Others:[11]
- CD79a +ve.
- CD45 -ve/+ve.
- CD10 -ve.
- CD5 -ve.
- Cyclin D1 -ve/+ve.
A panel:
- CD3, CD20, CD56, CD117, CD138, IG-kappa (plasma), IG-lambda (plasma).
Molecular
- t(4;14)(p16.3;q32.3) / IGH–MMSET.[12]
- Associated with poor prognosis.[13]
- 13q deletion.
- Worse prognosis.[1]
- 17q deletion.
- Worse prognosis.[1]
See also
References
- ↑ 1.0 1.1 1.2 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 324. ISBN 978-1416054542.
- ↑ Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 323. ISBN 978-1416054542.
- ↑ Alexiou, C.; Kau, RJ.; Dietzfelbinger, H.; Kremer, M.; Spiess, JC.; Schratzenstaller, B.; Arnold, W. (Jun 1999). "Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts.". Cancer 85 (11): 2305-14. PMID 10357398.
- ↑ Kyle RA, Rajkumar SV (January 2009). "Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma". Leukemia 23 (1): 3–9. doi:10.1038/leu.2008.291. PMC 2627786. PMID 18971951. http://www.nature.com/leu/journal/v23/n1/full/leu2008291a.html.
- ↑ "Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group.". Br J Haematol 121 (5): 749-57. Jun 2003. PMID 12780789.
- ↑ URL: http://www.thefreelibrary.com/Dutcher+bodies+in+chronic+synovitis-a083551789. Accessed on: 4 August 2010.
- ↑ URL: http://path.upmc.edu/cases/case515.html. Accessed on: 25 January 2012.
- ↑ URL: http://www.ncbi.nlm.nih.gov/omim/116930. Accessed on: 31 August 2010.
- ↑ URL: http://www.nature.com/bmt/journal/v33/n1/full/1704298a.html. Accessed on: 31 August 2010.
- ↑ Tamamori, T.; Nakayama, F.; Sugimoto, H.; Fenxiang, J.; Iwatsuki, K.; Takigawa, M. (Oct 1993). "Extramedullary plasmacytoma: cytological and genotypic studies.". Br J Dermatol 129 (4): 468-72. PMID 8217765.
- ↑ URL: http://e-immunohistochemistry.info/web/Plasmacytoma_plasma_cell_myeloma.htm. Accessed on: 9 November 2015.
- ↑ Chesi, M.; Nardini, E.; Lim, RS.; Smith, KD.; Kuehl, WM.; Bergsagel, PL. (Nov 1998). "The t(4;14) translocation in myeloma dysregulates both FGFR3 and a novel gene, MMSET, resulting in IgH/MMSET hybrid transcripts.". Blood 92 (9): 3025-34. PMID 9787135.
- ↑ Keats, JJ.; Reiman, T.; Maxwell, CA.; Taylor, BJ.; Larratt, LM.; Mant, MJ.; Belch, AR.; Pilarski, LM. (Feb 2003). "In multiple myeloma, t(4;14)(p16;q32) is an adverse prognostic factor irrespective of FGFR3 expression.". Blood 101 (4): 1520-9. doi:10.1182/blood-2002-06-1675. PMID 12393535.