Difference between revisions of "Leiomyoma"
(→Microscopic: +lipoleiomyosarcoma) |
|||
| (19 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Lipoleiomyoma2.jpg | |||
| Width = | |||
| Caption = Lipoleiomyoma. [[H&E stain]]. | |||
| Micro = spindle cells arranged in fascicles, +/-nuclear atypia, rare mitoses (allowable mitotic rate dependent on specific site) | |||
| Subtypes = lipoleiomyoma, hypercellular leiomyoma, atypical leiomyoma (symplastic leiomyoma), benign metastasizing leiomyoma | |||
| LMDDx = [[leiomyosarcoma]], [[STUMP]], [[dermatomyofibroma]], [[adenomatoid tumour]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = well-circumscribed, whorled appearance, firm | |||
| Grossing = | |||
| Site = [[skin]], [[uterus]], others | |||
| Assdx = | |||
| Syndromes = [[hereditary leiomyomatosis and renal cell cancer]] (cutaneous & uterine leiomyomas) | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = skin: [[painful skin lesion|pain]], uterus: bulky | |||
| Prevalence = very common - esp. uterine | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = benign | |||
| Other = | |||
| ClinDDx = | |||
}} | |||
A '''leiomyoma''' is a very common benign [[smooth muscle tumours|tumour of smooth muscle]]. Leiomyomas fit into the ''[[soft tissue lesions|soft tissue]]'' group of lesions. They are extremely common in the [[uterus]]. They may also be seen in the [[skin]]. | A '''leiomyoma''' is a very common benign [[smooth muscle tumours|tumour of smooth muscle]]. Leiomyomas fit into the ''[[soft tissue lesions|soft tissue]]'' group of lesions. They are extremely common in the [[uterus]]. They may also be seen in the [[skin]]. | ||
| Line 5: | Line 34: | ||
===Cutaneous leiomyomas=== | ===Cutaneous leiomyomas=== | ||
*May be part of '' | *May be part of ''[[hereditary leiomyomatosis and renal cell cancer]]'' (HLRCC).<ref>URL: [http://www.ncbi.nlm.nih.gov/books/NBK1252/ http://www.ncbi.nlm.nih.gov/books/NBK1252/]. Accessed on: 2 September 2011.</ref><ref>URL: [http://ccr.cancer.gov/staff/gallery.asp?profileid=12822 http://ccr.cancer.gov/staff/gallery.asp?profileid=12822]. Accessed on: 2 September 2011.</ref> | ||
*[[Painful skin lesion]]. | |||
===Uterine leiomyoma=== | ===Uterine leiomyoma=== | ||
| Line 11: | Line 41: | ||
*Often called "fibroids". | *Often called "fibroids". | ||
*Extremely common... 40% of women by age 40. | *Extremely common... 40% of women by age 40. | ||
*Can be a cause of [[AUB]] (abnormal uterine bleeding). | *Can be a cause of [[AUB]] ([[abnormal uterine bleeding]]). | ||
*Large & multiple leiomyomas are associated with infertility. | *Large & multiple leiomyomas are associated with infertility. | ||
*May be part of ''[[hereditary leiomyomatosis and renal cell cancer]]'' (HLRCC). | |||
**In one series, 68% with HLRCC were diagnosed at age <=30 years.<ref name=pmid16597677>{{Cite journal | last1 = Pithukpakorn | first1 = M. | last2 = Wei | first2 = MH. | last3 = Toure | first3 = O. | last4 = Steinbach | first4 = PJ. | last5 = Glenn | first5 = GM. | last6 = Zbar | first6 = B. | last7 = Linehan | first7 = WM. | last8 = Toro | first8 = JR. | title = Fumarate hydratase enzyme activity in lymphoblastoid cells and fibroblasts of individuals in families with hereditary leiomyomatosis and renal cell cancer. | journal = J Med Genet | volume = 43 | issue = 9 | pages = 755-62 | month = Sep | year = 2006 | doi = 10.1136/jmg.2006.041087 | PMID = 16597677 }} | |||
</ref> | |||
===Colonic leiomyoma=== | |||
{{Main|Colonic leiomyoma}} | |||
===Renal leiomyoma=== | |||
{{Main|Renal leiomyoma}} | |||
==Gross== | ==Gross== | ||
| Line 39: | Line 78: | ||
Note: | Note: | ||
*Leiomyosarcoma is diagnosed if | *Leiomyosarcoma is diagnosed if 2 of 3 are present: (1) high mitotic rate (dependent on site), (2) marked nuclear atypia (seen at low power), (3) [[necrosis]]. | ||
DDx: | DDx: | ||
| Line 46: | Line 85: | ||
*Dermatomyofibroma.<ref name=Ref_Derm533>{{Ref Derm|533}}</ref> | *Dermatomyofibroma.<ref name=Ref_Derm533>{{Ref Derm|533}}</ref> | ||
*[[Myopericytoma]] / [[myofibroma]]. | *[[Myopericytoma]] / [[myofibroma]]. | ||
*[[Adenomatoid tumour]] - esp. for lipoleiomyoma. | |||
*[[Smooth muscle tumour of uncertain malignant potential]] (STUMP) - do not fulfill criteria for leiomyosarcoma. | |||
*[[Epstein-Barr virus-associated smooth muscle tumour]] - very rare. | |||
===Variants=== | ===Variants=== | ||
| Line 55: | Line 97: | ||
<gallery> | <gallery> | ||
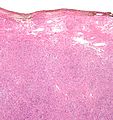
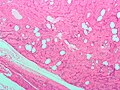
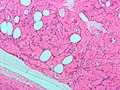
Image:Atypical_leiomyoma_low_mag.jpg | Atypical leiomyoma - low mag. (WC/Nephron) | |||
Image:Atypical_leiomyoma_intermed_mag.jpg | Atypical leiomyoma - intermed. mag. (WC/Nephron) | Image:Atypical_leiomyoma_intermed_mag.jpg | Atypical leiomyoma - intermed. mag. (WC/Nephron) | ||
Image:Atypical_leiomyoma_high_mag.jpg | Atypical leiomyoma - high mag. (WC/Nephron) | Image:Atypical_leiomyoma_high_mag.jpg | Atypical leiomyoma - high mag. (WC/Nephron) | ||
Image:Lipoleiomyoma1.jpg | Lipoleiomyoma - low mag. (WC/Nephron) | Image:Lipoleiomyoma1.jpg | Lipoleiomyoma - low mag. (WC/Nephron) | ||
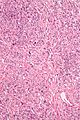
Image:Lipoleiomyoma2.jpg | Lipoleiomyoma - high mag. (WC/Nephron) | |||
</gallery> | </gallery> | ||
| Line 82: | Line 126: | ||
===Micro=== | ===Micro=== | ||
The section shows unremarkable hair-bearing skin with a well-circumscribed subcutaneous lesion with a fascicular architecture. The lesion has no nuclear atypia and no mitotic activity is identified. At the periphery of the lesion is a medium-sized muscular artery from which the lesion appears to arise. | The section shows unremarkable hair-bearing skin with a well-circumscribed subcutaneous lesion with a fascicular architecture. The lesion has no nuclear atypia and no mitotic activity is identified. At the periphery of the lesion is a medium-sized muscular artery from which the lesion appears to arise. | ||
====Alternate==== | |||
The sections show a spindle cell lesion with a fascicular architecture. Focal hyaline | |||
change is seen. No nuclear atypia is apparent. Mitotic activity is not readily identified. No necrosis is identified. The lesion extends to the edge of the tissue fragments. | |||
==See also== | ==See also== | ||
Latest revision as of 15:39, 13 May 2016
| Leiomyoma | |
|---|---|
| Diagnosis in short | |
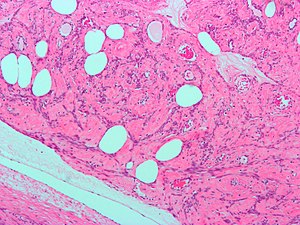 Lipoleiomyoma. H&E stain. | |
|
| |
| LM | spindle cells arranged in fascicles, +/-nuclear atypia, rare mitoses (allowable mitotic rate dependent on specific site) |
| Subtypes | lipoleiomyoma, hypercellular leiomyoma, atypical leiomyoma (symplastic leiomyoma), benign metastasizing leiomyoma |
| LM DDx | leiomyosarcoma, STUMP, dermatomyofibroma, adenomatoid tumour |
| Gross | well-circumscribed, whorled appearance, firm |
| Site | skin, uterus, others |
|
| |
| Syndromes | hereditary leiomyomatosis and renal cell cancer (cutaneous & uterine leiomyomas) |
|
| |
| Symptoms | skin: pain, uterus: bulky |
| Prevalence | very common - esp. uterine |
| Prognosis | benign |
A leiomyoma is a very common benign tumour of smooth muscle. Leiomyomas fit into the soft tissue group of lesions. They are extremely common in the uterus. They may also be seen in the skin.
General
- Benign.
Cutaneous leiomyomas
- May be part of hereditary leiomyomatosis and renal cell cancer (HLRCC).[1][2]
- Painful skin lesion.
Uterine leiomyoma
- Often called "fibroids".
- Extremely common... 40% of women by age 40.
- Can be a cause of AUB (abnormal uterine bleeding).
- Large & multiple leiomyomas are associated with infertility.
- May be part of hereditary leiomyomatosis and renal cell cancer (HLRCC).
- In one series, 68% with HLRCC were diagnosed at age <=30 years.[3]
Colonic leiomyoma
Renal leiomyoma
Gross
- Sharply circumscribed.
- Gray-white.
- Whorled appearance.
Factors that raise concern for leiomyosarcoma:
- Haemorrhage.
- Cystic degeneration.
- Necrosis.
Microscopic
Features:
- Spindle cells arranged in fascicles.
- Fascicular appearance: adjacent groups of cells have their long axis perpendicular to one another; looks somewhat like a braided hair that was cut.
- Whorled arrangement of cells.
- +/-Medium-sized artery seen at the periphery of the lesion.
- Often arise from a muscular artery.
Uncommonly present - see note:
- Necrosis (low power) - suggestive of leiomyosarcoma.
- Hypercellularity.
- Nuclear atypia seen at low power.
- Few mitoses.
Note:
- Leiomyosarcoma is diagnosed if 2 of 3 are present: (1) high mitotic rate (dependent on site), (2) marked nuclear atypia (seen at low power), (3) necrosis.
DDx:
- Leiomyosarcoma.
- Lipoleiomyosarcoma - very rare.[4]
- Dermatomyofibroma.[5]
- Myopericytoma / myofibroma.
- Adenomatoid tumour - esp. for lipoleiomyoma.
- Smooth muscle tumour of uncertain malignant potential (STUMP) - do not fulfill criteria for leiomyosarcoma.
- Epstein-Barr virus-associated smooth muscle tumour - very rare.
Variants
- Lipoleiomyoma - with adipose tissue.
- Hypercellular leiomyoma - hypercellularity assoc. with more mutations.[6]
- Atypical leiomyoma (AKA symplastic leiomyoma) - leiomyoma with nuclear atypia.
- Benign metastasizing leiomyoma.[7]
- This is just what it sounds like. Some believe these are low grade leiomyosarcomas.
IHC
Work-up of suspicious leiomyomas:[8]
- CD10 +ve.
- Ki-67 -ve.
- SMA +ve.
- Desmin +ve.
Other stains:
- H-caldesmon +ve.[9]
Sign out
SKIN LESION, RIGHT LEG, EXCISION: - LEIOMYOMA. - NEGATIVE FOR MALIGNANCY. COMMENT: The lesion stains for desmin and SMA. It is negative for S-100 and has minimal staining with Ki-67.
Micro
The section shows unremarkable hair-bearing skin with a well-circumscribed subcutaneous lesion with a fascicular architecture. The lesion has no nuclear atypia and no mitotic activity is identified. At the periphery of the lesion is a medium-sized muscular artery from which the lesion appears to arise.
Alternate
The sections show a spindle cell lesion with a fascicular architecture. Focal hyaline change is seen. No nuclear atypia is apparent. Mitotic activity is not readily identified. No necrosis is identified. The lesion extends to the edge of the tissue fragments.
See also
References
- ↑ URL: http://www.ncbi.nlm.nih.gov/books/NBK1252/. Accessed on: 2 September 2011.
- ↑ URL: http://ccr.cancer.gov/staff/gallery.asp?profileid=12822. Accessed on: 2 September 2011.
- ↑ Pithukpakorn, M.; Wei, MH.; Toure, O.; Steinbach, PJ.; Glenn, GM.; Zbar, B.; Linehan, WM.; Toro, JR. (Sep 2006). "Fumarate hydratase enzyme activity in lymphoblastoid cells and fibroblasts of individuals in families with hereditary leiomyomatosis and renal cell cancer.". J Med Genet 43 (9): 755-62. doi:10.1136/jmg.2006.041087. PMID 16597677.
- ↑ Folpe, AL.; Weiss, SW. (Jun 2002). "Lipoleiomyosarcoma (well-differentiated liposarcoma with leiomyosarcomatous differentiation): a clinicopathologic study of nine cases including one with dedifferentiation.". Am J Surg Pathol 26 (6): 742-9. PMID 12023578.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 533. ISBN 978-0443066542.
- ↑ http://www3.interscience.wiley.com/journal/119360394/abstract
- ↑ Patton, KT.; Cheng, L.; Papavero, V.; Blum, MG.; Yeldandi, AV.; Adley, BP.; Luan, C.; Diaz, LK. et al. (Jan 2006). "Benign metastasizing leiomyoma: clonality, telomere length and clinicopathologic analysis.". Mod Pathol 19 (1): 130-40. doi:10.1038/modpathol.3800504. PMID 16357844. http://www.nature.com/modpathol/journal/v19/n1/full/3800504a.html.
- ↑ STC. 25 February 2009.
- ↑ Zámecník, M.; Kascák, P. (Jul 2011). "Uterine leiomyoma with amianthoid-like fibers.". Cesk Patol 47 (3): 125-7. PMID 21887931.