Difference between revisions of "Embryonal carcinoma"
Jump to navigation
Jump to search
| (10 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
| Width = | | Width = | ||
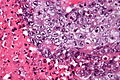
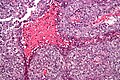
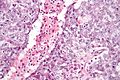
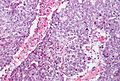
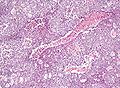
| Caption = Embryonal carcinoma. [[H&E stain]]. | | Caption = Embryonal carcinoma. [[H&E stain]]. | ||
| Micro = vesicular nuclei, nuclear overlap, necrosis (common), mitoses, variable architecture (tubulopapillary, glandular, solid, embryoid bodies) | | Micro = [[vesicular nuclei]], nuclear overlap, necrosis (common), mitoses, variable architecture (tubulopapillary, glandular, solid, embryoid bodies) | ||
| Subtypes = | | Subtypes = | ||
| LMDDx = [[seminoma]], [[mixed germ cell tumour]], [[yolk sac tumour]], other carcinomas | | LMDDx = [[seminoma]], [[mixed germ cell tumour]], [[yolk sac tumour]], other carcinomas | ||
| Line 13: | Line 13: | ||
| IF = | | IF = | ||
| Gross = | | Gross = | ||
| Grossing = | | Grossing = [[orchiectomy grossing]] | ||
| Staging = [[testicular cancer staging]] | |||
| Site = [[testis]], [[ovary]], [[mediastinum]] | | Site = [[testis]], [[ovary]], [[mediastinum]] | ||
| Assdx = | | Assdx = | ||
| Line 20: | Line 21: | ||
| Signs = testicular mass, pelvic mass | | Signs = testicular mass, pelvic mass | ||
| Symptoms = | | Symptoms = | ||
| Prevalence = | | Prevalence = pure embryonal uncommon | ||
| Bloodwork = | | Bloodwork = | ||
| Rads = | | Rads = | ||
| Line 26: | Line 27: | ||
| Prognosis = | | Prognosis = | ||
| Other = | | Other = | ||
| ClinDDx = | | ClinDDx = typically other [[testicle|testicular tumours]] | ||
}} | }} | ||
'''Embryonal carcinoma''' is a type of [[germ cell tumour]]. It is commonly as a component of [[mixed germ cell tumour]]s. | '''Embryonal carcinoma''' is a type of [[germ cell tumour]]. It is commonly as a component of [[mixed germ cell tumour]]s. | ||
| Line 33: | Line 34: | ||
*Affects young adults. | *Affects young adults. | ||
**May be seen in women. | **May be seen in women. | ||
*Usually a component of a [[mixed germ cell tumour]] - in the [[testicle]] 85% of cases are mixed, only 15% are pure.<ref name=pmid24503753/> | |||
==Gross== | ==Gross== | ||
| Line 41: | Line 43: | ||
Features:<ref name=Ref_GUP549>{{Ref GUP|549}}</ref> | Features:<ref name=Ref_GUP549>{{Ref GUP|549}}</ref> | ||
#Nucleoli - '''key feature'''. | #Nucleoli - '''key feature'''. | ||
#Vesicular nuclei (clear, empty appearing nuclei) - '''key feature'''. | #[[Vesicular nuclei]] (clear, empty appearing nuclei) - '''key feature'''. | ||
#Nuclei overlap. | #Nuclei overlap. | ||
#[[Necrosis]] - common. | #[[Necrosis]] - common. | ||
| Line 47: | Line 49: | ||
#Indistinct cell borders | #Indistinct cell borders | ||
#Mitoses - common. | #Mitoses - common. | ||
#Variable architecture: | #Variable architecture:<ref name=pmid24503753>{{Cite journal | last1 = Kao | first1 = CS. | last2 = Ulbright | first2 = TM. | last3 = Young | first3 = RH. | last4 = Idrees | first4 = MT. | title = Testicular embryonal carcinoma: a morphologic study of 180 cases highlighting unusual and unemphasized aspects. | journal = Am J Surg Pathol | volume = 38 | issue = 5 | pages = 689-97 | month = May | year = 2014 | doi = 10.1097/PAS.0000000000000171 | PMID = 24503753 }}</ref> | ||
#* | #*Solid (predominant in ~55% of cases). | ||
#*Glandular. | #*Glandular (predominant in ~17% of cases). | ||
#* | #*Papillary (predominant in ~11% of cases). | ||
#*Nested. | |||
#*Micropapillary. | |||
#*Anastomosing glandular. | |||
#*Sieve-like glandular. | |||
#*Pseudopapillary. | |||
#*Blastocyst-like. | |||
#*Embryoid bodies - ball of cells in surrounded by empty space on three sides. | #*Embryoid bodies - ball of cells in surrounded by empty space on three sides. | ||
Notes: | Notes: | ||
*Cytoplasmic staining variable (eosinophilic to basophilic). | *Cytoplasmic staining variable (eosinophilic to basophilic). | ||
*[[Syncytiotrophoblasts]] commonly seen (~40-50% of cases<ref name=pmid24503753/>). | |||
DDx: | DDx: | ||
*[[Mixed germ cell tumour]]. | *[[Mixed germ cell tumour]]. | ||
*[[Yolk sac tumour]]. | *[[Yolk sac tumour]]. | ||
*[[Seminoma]]. | |||
===Images=== | ===Images=== | ||
| Line 72: | Line 82: | ||
==IHC== | ==IHC== | ||
===ISUP consensus=== | |||
General panel:<ref name=pmid24832161>{{cite journal |author=Ulbright TM, Tickoo SK, Berney DM, Srigley JR |title=Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference |journal=Am. J. Surg. Pathol. |volume=38 |issue=8 |pages=e50–9 |year=2014 |month=August |pmid=24832161 |doi=10.1097/PAS.0000000000000233 |url=}}</ref> | |||
*OCT4 +ve. | *OCT4 +ve. | ||
**Choriocarcinoma, yolk sac tumour and spermatocytic seminoma all -ve. | **Choriocarcinoma, yolk sac tumour and spermatocytic seminoma all -ve. | ||
| Line 80: | Line 91: | ||
**+ve in [[seminoma]]. | **+ve in [[seminoma]]. | ||
Additional notes | ===Additional notes=== | ||
*CK19 -ve.<ref>{{Cite journal | last1 = Bremmer | first1 = F. | last2 = Ströbel | first2 = P. | last3 = Hubertus | first3 = H. | last4 = Strecker | first4 = J. | last5 = Gaisa | first5 = N. | last6 = Strauß | first6 = A. | last7 = Schweyer | first7 = S. | last8 = Radzun | first8 = H-J. | last9 = Behnes | first9 = C-L | title = CK19 is a sensitive marker for yolk sac tumours of the testis. | journal = Diagnostic Pathology | volume = 10 | issue = 7 | pages = | month = | year = 2015 | doi = 10.1186/s13000-015-0243-y | PMID = | url = www.diagnosticpathology.org/content/10/1/7Cached }}</ref> | |||
**[[Yolk sac tumour]] +ve, seminoma -ve, [[GCNIS]] (ITGCN) -ve, normal testis -ve. | |||
*AE1/AE3 +ve. | *AE1/AE3 +ve. | ||
*OCT3/4 +ve.<ref name=pmid18045648>{{Cite journal | last1 = Iczkowski | first1 = KA. | last2 = Butler | first2 = SL. | last3 = Shanks | first3 = JH. | last4 = Hossain | first4 = D. | last5 = Schall | first5 = A. | last6 = Meiers | first6 = I. | last7 = Zhou | first7 = M. | last8 = Torkko | first8 = KC. | last9 = Kim | first9 = SJ. | title = Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors. | journal = Hum Pathol | volume = 39 | issue = 2 | pages = 275-81 | month = Feb | year = 2008 | doi = 10.1016/j.humpath.2007.07.002 | PMID = 18045648 }}</ref> | *OCT3/4 +ve.<ref name=pmid18045648>{{Cite journal | last1 = Iczkowski | first1 = KA. | last2 = Butler | first2 = SL. | last3 = Shanks | first3 = JH. | last4 = Hossain | first4 = D. | last5 = Schall | first5 = A. | last6 = Meiers | first6 = I. | last7 = Zhou | first7 = M. | last8 = Torkko | first8 = KC. | last9 = Kim | first9 = SJ. | title = Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors. | journal = Hum Pathol | volume = 39 | issue = 2 | pages = 275-81 | month = Feb | year = 2008 | doi = 10.1016/j.humpath.2007.07.002 | PMID = 18045648 }}</ref> | ||
*D2-40 -ve.<ref name=pmid18045648/> | *D2-40 -ve.<ref name=pmid18045648/> | ||
**Iczkowski ''et al.'' suggest it is useful for discriminating from [[seminoma]]. This is somewhat disputed by Lau ''et al.''<ref name=pmid17277761>{{Cite journal | last1 = Lau | first1 = SK. | last2 = Weiss | first2 = LM. | last3 = Chu | first3 = PG. | title = D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30. | journal = Mod Pathol | volume = 20 | issue = 3 | pages = 320-5 | month = Mar | year = 2007 | doi = 10.1038/modpathol.3800749 | PMID = 17277761 }}</ref> | **Iczkowski ''et al.'' suggest it is useful for discriminating from [[seminoma]]. This is somewhat disputed by Lau ''et al.''<ref name=pmid17277761>{{Cite journal | last1 = Lau | first1 = SK. | last2 = Weiss | first2 = LM. | last3 = Chu | first3 = PG. | title = D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30. | journal = Mod Pathol | volume = 20 | issue = 3 | pages = 320-5 | month = Mar | year = 2007 | doi = 10.1038/modpathol.3800749 | PMID = 17277761 }}</ref> | ||
*PLAP +ve.<ref name=pmid6209917>{{Cite journal | last1 = Jacobsen | first1 = GK. | last2 = Nørgaard-Pedersen | first2 = B. | title = Placental alkaline phosphatase in testicular germ cell tumours and in carcinoma-in-situ of the testis. An immunohistochemical study. | journal = Acta Pathol Microbiol Immunol Scand A | volume = 92 | issue = 5 | pages = 323-9 | month = Sep | year = 1984 | doi = | PMID = 6209917 }}</ref> | *[[PLAP]] +ve.<ref name=pmid6209917>{{Cite journal | last1 = Jacobsen | first1 = GK. | last2 = Nørgaard-Pedersen | first2 = B. | title = Placental alkaline phosphatase in testicular germ cell tumours and in carcinoma-in-situ of the testis. An immunohistochemical study. | journal = Acta Pathol Microbiol Immunol Scand A | volume = 92 | issue = 5 | pages = 323-9 | month = Sep | year = 1984 | doi = | PMID = 6209917 }}</ref> | ||
==See also== | ==See also== | ||
Revision as of 20:57, 26 April 2016
| Embryonal carcinoma | |
|---|---|
| Diagnosis in short | |
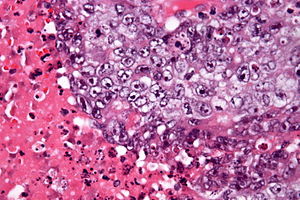 Embryonal carcinoma. H&E stain. | |
|
| |
| LM | vesicular nuclei, nuclear overlap, necrosis (common), mitoses, variable architecture (tubulopapillary, glandular, solid, embryoid bodies) |
| LM DDx | seminoma, mixed germ cell tumour, yolk sac tumour, other carcinomas |
| IHC | OCT3 +ve, CD30 +ve, AE1/AE3 +ve, CD117 -ve |
| Grossing notes | orchiectomy grossing |
| Staging | testicular cancer staging |
| Site | testis, ovary, mediastinum |
|
| |
| Signs | testicular mass, pelvic mass |
| Prevalence | pure embryonal uncommon |
| Clin. DDx | typically other testicular tumours |
Embryonal carcinoma is a type of germ cell tumour. It is commonly as a component of mixed germ cell tumours.
General
- Affects young adults.
- May be seen in women.
- Usually a component of a mixed germ cell tumour - in the testicle 85% of cases are mixed, only 15% are pure.[1]
Gross
- Typically a testicular mass.
- May be seen in the mediastinum.[2]
Microscopic
Features:[3]
- Nucleoli - key feature.
- Vesicular nuclei (clear, empty appearing nuclei) - key feature.
- Nuclei overlap.
- Necrosis - common.
- Not commonly present in seminoma.
- Indistinct cell borders
- Mitoses - common.
- Variable architecture:[1]
- Solid (predominant in ~55% of cases).
- Glandular (predominant in ~17% of cases).
- Papillary (predominant in ~11% of cases).
- Nested.
- Micropapillary.
- Anastomosing glandular.
- Sieve-like glandular.
- Pseudopapillary.
- Blastocyst-like.
- Embryoid bodies - ball of cells in surrounded by empty space on three sides.
Notes:
- Cytoplasmic staining variable (eosinophilic to basophilic).
- Syncytiotrophoblasts commonly seen (~40-50% of cases[1]).
DDx:
Images
IHC
ISUP consensus
General panel:[4]
- OCT4 +ve.
- Choriocarcinoma, yolk sac tumour and spermatocytic seminoma all -ve.
- CD30 +ve.
- -ve in seminoma.
- CD117 -ve.[5]
- +ve in seminoma.
Additional notes
- CK19 -ve.[6]
- Yolk sac tumour +ve, seminoma -ve, GCNIS (ITGCN) -ve, normal testis -ve.
- AE1/AE3 +ve.
- OCT3/4 +ve.[7]
- D2-40 -ve.[7]
- PLAP +ve.[8]
See also
References
- ↑ 1.0 1.1 1.2 Kao, CS.; Ulbright, TM.; Young, RH.; Idrees, MT. (May 2014). "Testicular embryonal carcinoma: a morphologic study of 180 cases highlighting unusual and unemphasized aspects.". Am J Surg Pathol 38 (5): 689-97. doi:10.1097/PAS.0000000000000171. PMID 24503753.
- ↑ Yalçın, B.; Demir, HA.; Tanyel, FC.; Akçören, Z.; Varan, A.; Akyüz, C.; Kutluk, T.; Büyükpamukçu, M. (Oct 2012). "Mediastinal germ cell tumors in childhood.". Pediatr Hematol Oncol 29 (7): 633-42. doi:10.3109/08880018.2012.713084. PMID 22877235.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 549. ISBN 978-0443066771.
- ↑ Ulbright TM, Tickoo SK, Berney DM, Srigley JR (August 2014). "Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): e50–9. doi:10.1097/PAS.0000000000000233. PMID 24832161.
- ↑ 5.0 5.1 Lau, SK.; Weiss, LM.; Chu, PG. (Mar 2007). "D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30.". Mod Pathol 20 (3): 320-5. doi:10.1038/modpathol.3800749. PMID 17277761.
- ↑ Bremmer, F.; Ströbel, P.; Hubertus, H.; Strecker, J.; Gaisa, N.; Strauß, A.; Schweyer, S.; Radzun, H-J. et al. (2015). [www.diagnosticpathology.org/content/10/1/7Cached "CK19 is a sensitive marker for yolk sac tumours of the testis."]. Diagnostic Pathology 10 (7). doi:10.1186/s13000-015-0243-y. www.diagnosticpathology.org/content/10/1/7Cached.
- ↑ 7.0 7.1 Iczkowski, KA.; Butler, SL.; Shanks, JH.; Hossain, D.; Schall, A.; Meiers, I.; Zhou, M.; Torkko, KC. et al. (Feb 2008). "Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors.". Hum Pathol 39 (2): 275-81. doi:10.1016/j.humpath.2007.07.002. PMID 18045648.
- ↑ Jacobsen, GK.; Nørgaard-Pedersen, B. (Sep 1984). "Placental alkaline phosphatase in testicular germ cell tumours and in carcinoma-in-situ of the testis. An immunohistochemical study.". Acta Pathol Microbiol Immunol Scand A 92 (5): 323-9. PMID 6209917.