Mucoepidermoid carcinoma
(Redirected from MEC)
Jump to navigation
Jump to search
| Mucoepidermoid carcinoma | |
|---|---|
| Diagnosis in short | |
 Mucoepidermoid carcinoma. H&E stain. | |
|
| |
| LM | mucous cells (abundant fluffy cytoplasm and large mucin vacuoles - nucleus distorted by mucin vacuole, cells may be scarce); epidermoid cells (non-keratinized, polygonal squamoid cell with clear or oncocytic cytoplasm); architecture - cystic (low grade) or solid (high grade) |
| LM DDx | squamous cell carcinoma of the head and neck, adenosquamous carcinoma, pleomorphic adenoma |
| Stains | mucous cells: alcian blue stain +ve, mucicarmine stain +ve |
| Molecular | t(11;19)(q21;p13) |
| Gross | solid, cystic or both |
| Site | salivary gland, classically parotid gland |
|
| |
| Signs | mass lesion |
| Prevalence | most common malignant salivary gland tumour, generally uncommon |
Mucoepidermoid carcinoma, abbreviated MEC, the is the most common malignant neoplasm of the salivary gland.
General
- Most common malignant neoplasm of salivary gland in all age groups.[1][2]
- Female:male ~= 3:2.
- Site: parotid > submandibular.
Gross
- Cystic or solid, usually a mix of both.
Note:
- May mimic a benign cystic lesion grossly.
- Unicystic mucoepidermoid carcinoma is rare.[3]
Microscopic
Features:
- Architecture:[4]
- Cystic (low grade).
- Solid (high grade).
- Mucous cells with abundant fluffy cytoplasm and large mucin vacuoles - key feature.
- Nucleus distorted by mucin vacuole.
- Mucous cell may be scarce - more difficult to diagnose.
- Epidermoid cells:
Notes:
- The classic description - composed of 3 cell types: epidermoid, intermediate, and mucin producing.[5]
- "Intermediate cells" are described in textbooks. Weinreb thinks they are a pretty much a myth.[6]
- Mucin vacuoles may be rare; in a superficial glance -- it may mimic squamous cell carcinoma.
- The thought of high-grade MEC should prompt consideration of squamous cell carcinoma.
DDx:[7]
- Squamous cell carcinoma of the skin - 75% of metastases to the parotid region are from the skin.[8]
- Squamous cell carcinoma of the head and neck.
- Adenosquamous carcinoma.
- Pleomorphic adenoma.[9]
Images
www:
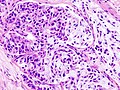
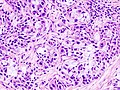
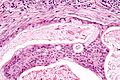
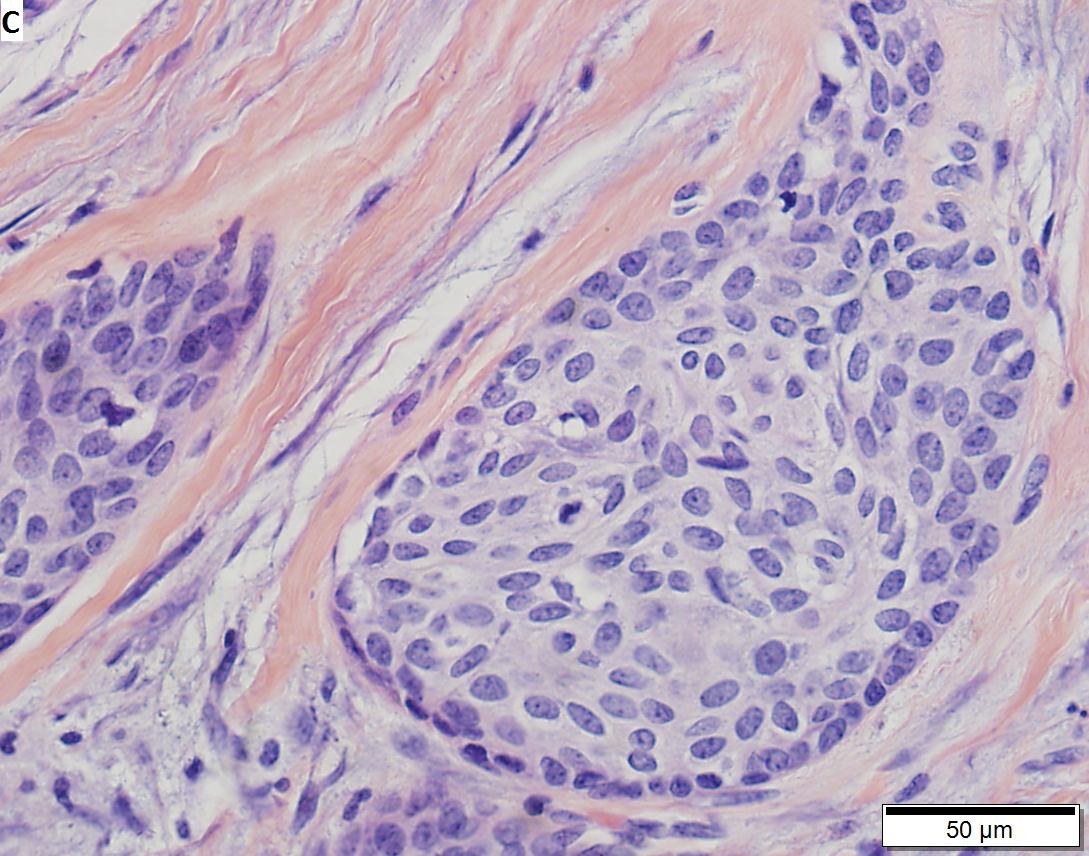
Low grade mucoepidermoid carcinoma in left parotid of 51 year old woman. A. Tumor shows blue squamoud differentiation with cystic dilatation. B This focus shows more obvious cyst formation. C. Squamous component with round to spindled cancer cells; note that currently squamous pearls and high grade squamous cancer elements render the tumor a squamous carcinoma, according to Barnes. D. Glandular cell component.
Subtypes
- Conventional.
- Oncocytic.
- Definition: composed of 50% oncocytes.
- Good outcome.[10]
- Clear cell.
- Unicystic (cystadenocarcinoma).
- Based on the gross. (???)
- Sclerosing MEC +/- eosinophilia.
- Rare.
Grading
General:
Notes:
- Both systems have their pros and cons.
- Weinreb uses the AFIP system with a slight modification.
AFIP
- Low cystic component (<20%) - 2 points.
- Perineural invasion - 2 points.
- Necrosis - 3 points.
- Mitoses > 4 per 10 HPFs (HPF not defined in paper - see HPFitis) - 3 points.
- Anaplasia - 4 points.
Scoring:
- Low grade = 0-4 points.
- Intermediate grade = 5-6 points.
- High grade = 7+ points.
Weinreb modification
Weinreb looks for the following:
- Tumour invades in small nests/islands - 2 points.
- If applicable, the two points are added to the AFIP score.
- The tumour is graded using the AFIP (scoring) cut points -- see above.
Notes:
- It seems pointless to memorize this but it is occasionally asked on exams.
- How to remember: think of the Nottingham grading system (architecture, mitoses, nuclear grade) + necrosis + LVI.
Stains
Mucous cells:
- Alcian blue +ve.
- Mucicarmine +ve.
Notes:
- Above useful for MEC versus squamous cell carcinoma.[13]
IHC
- CK7 +ve.
- CK20 -ve.
- CEA +ve.[14]
Sign out
A. Lymph Node, Deep Lobe of Left Parotid Gland, Excision:
- One lymph node NEGATIVE for malignancy (0/1).
B. Parotid Gland - Left Deep Lobe, Excision:
- MUCOEPIDERMOID CARCINOMA, low (AFIP) grade.
-- Margins clear.
-- Please see synoptic report.
Molecular
- t(11;19)(q21;p13) -- MECT1-MAML2 fusion.[15][16]
- Present in ~65% of MECs.
- Presence assoc. with low-grade MEC (vs. high-grade MEC) & favourable prognosis.
- Not seen in tumours that are in the DDx of MEC.
See also
References
- ↑ URL: http://path.upmc.edu/cases/case715/dx.html. Accessed on: 2 February 2012.
- ↑ Bell, RB.; Dierks, EJ.; Homer, L.; Potter, BE. (Jul 2005). "Management and outcome of patients with malignant salivary gland tumors.". J Oral Maxillofac Surg 63 (7): 917-28. PMID 16003616.
- ↑ Qannam A, Bello IO, Al-Kindi M, Al-Hindi M (April 2013). "Unicystic mucoepidermoid carcinoma presenting as a salivary duct cyst". Int J Surg Pathol 21 (2): 181–5. doi:10.1177/1066896912454918. PMID 22843640.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/opaq/PathQuiz/D2A001-PQ01-M.htm. Accessed on: 19 October 2010.
- ↑ Lennerz, JK.; Perry, A.; Mills, JC.; Huettner, PC.; Pfeifer, JD. (Jun 2009). "Mucoepidermoid carcinoma of the cervix: another tumor with the t(11;19)-associated CRTC1-MAML2 gene fusion.". Am J Surg Pathol 33 (6): 835-43. doi:10.1097/PAS.0b013e318190cf5b. PMID 19092631.
- ↑ IW. 10 January 2011.
- ↑ 7.0 7.1 Mokhtari, S.; Mokhtari, S. (2012). "Clinical features and differential diagnoses in laryngeal mucoepidermoid carcinoma.". Clin Med Insights Pathol 5: 1-6. doi:10.4137/CPath.S8435. PMID 22262946.
- ↑ Zanetti, D.; Renaldini, G.; Peretti, G.; Antonelli, AR.. "[Intra-parotid lymph node metastasis of malignant skin neoplasms of the head].". Acta Otorhinolaryngol Ital 9 (4): 381-90. PMID 2694753.
- ↑ Siddiqui, NH.; Wu, SJ. (Apr 2005). "Fine-needle aspiration biopsy of cystic pleomorphic adenoma with adnexa-like differentiation mimicking mucoepidermoid carcinoma: a case report.". Diagn Cytopathol 32 (4): 229-32. doi:10.1002/dc.20215. PMID 15754364.
- ↑ Weinreb I, Seethala RR, Perez-Ordoñez B, Chetty R, Hoschar AP, Hunt JL (March 2009). "Oncocytic mucoepidermoid carcinoma: clinicopathologic description in a series of 12 cases". Am. J. Surg. Pathol. 33 (3): 409–16. doi:10.1097/PAS.0b013e318184b36d. PMID 18971778.
- ↑ Goode RK, Auclair PL, Ellis GL (April 1998). "Mucoepidermoid carcinoma of the major salivary glands: clinical and histopathologic analysis of 234 cases with evaluation of grading criteria". Cancer 82 (7): 1217–24. PMID 9529011.
- ↑ Brandwein MS, Ivanov K, Wallace DI, et al. (July 2001). "Mucoepidermoid carcinoma: a clinicopathologic study of 80 patients with special reference to histological grading". Am. J. Surg. Pathol. 25 (7): 835–45. PMID 11420454.
- ↑ Jastrzebski, A.; Brownstein, S.; Jordan, DR.; Gilberg, SM. (Apr 2012). "Histochemical analysis and immunohistochemical profile of mucoepidermoid carcinoma of the conjunctiva.". Saudi J Ophthalmol 26 (2): 205-10. doi:10.1016/j.sjopt.2012.01.004. PMID 23960993.
- ↑ Hassanin, MB.; Ghosh, L.; Das, AK.; Waterhouse, JP. (May 1989). "Immunohistochemical and fluorescent microscopic study of histogenesis of salivary mucoepidermoid carcinoma.". J Oral Pathol Med 18 (5): 291-8. PMID 2475619.
- ↑ Tonon G, Modi S, Wu L, et al. (February 2003). "t(11;19)(q21;p13) translocation in mucoepidermoid carcinoma creates a novel fusion product that disrupts a Notch signaling pathway". Nat. Genet. 33 (2): 208–13. doi:10.1038/ng1083. PMID 12539049.
- ↑ Seethala RR, Dacic S, Cieply K, Kelly LM, Nikiforova MN (August 2010). "A reappraisal of the MECT1/MAML2 translocation in salivary mucoepidermoid carcinomas". Am. J. Surg. Pathol. 34 (8): 1106–21. doi:10.1097/PAS.0b013e3181de3021. PMID 20588178.