Squamous cell carcinoma
(Redirected from Carcinoma cuniculatum)
Jump to navigation
Jump to search
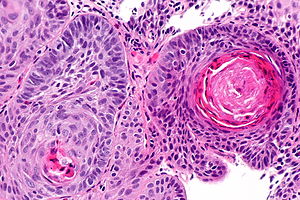
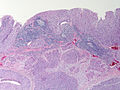
Squamous cell carcinoma. H&E stain. (WC)
This article deal with squamous cell carcinoma, also squamous carcinoma, a very common epithelial derived malignant neoplasm that can arise from many sites. It is commonly abbreviated SCC.
Sites
Skin
Main article: Squamous cell carcinoma of the skin
- A common skin tumour.
Head and neck
Main article: Squamous cell carcinoma of the head and neck
- Most common tumour of the head & neck.
- Tongue squamous cell carcinoma is dealt with separately.
- Nasopharyngeal carcinoma can be considered a variant SCC.
- HPV-associated SCC is dealt with in HPV-associated head and neck squamous cell carcinoma.
Tumour extent
- There is no agreed upon measure of tumour extent (tumour thickness/depth of invasion)[1] - proposed measures:[2]
- "Tumour thickness" = perpendicular distance from mucosal surface to deepest point of invasion.
- "Tumour depth" = perpendicular distance from epithelial basement membrane to deepest point of invasion.
Uterine cervix
Main article: Squamous cell carcinoma of the uterine cervix
- Most common form of cervical cancer.
Vulva
- Most common form of vulvar cancer.
Tumour extent
- No kerinization present: mucosal surface to the deepest point of invasion.
- Kerinization present: bottom of granular layer to the deepest point of invasion.
Lung
Main article: Squamous cell carcinoma of the lung
- A common form of lung cancer that is associated with smoking.
Esophagus
Main article: Squamous cell carcinoma of the esophagus
- Upper and middle esophagus.
Anus
Main article: Anal squamous cell carcinoma
- Most common form of anal cancer.
Other sites
Microscopic
Classification
SCC is subdivided by the WHO into:[5]
- Keratinizing type (KT).
- Worst prognosis.
- More common than non-keratinizing type.[6]
- Undifferentiated type (UT).
- Intermediate prognosis.
- EBV association.
- Non-keratinizing type (NT).
- Good prognosis.
- EBV association.
Features based on classification:[5]
- KT subtype:
- Keratinization & intercellular bridges through-out most of the malignant lesion.
- UT:
- Non-distinct borders/syncytial pattern.
- Nucleoli.
- NT:
- Well-defined cell borders.
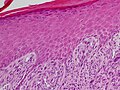
Invasive squamous cell carcinoma
Features:
- Eosinophilia.
- Extra large nuclei/bizarre nuclei.
- Inflammation (lymphocytes, plasma cells).
- Long rete ridges.
- Numerous beeds/blobs of epithelial cells that seem unlikely to be rete ridges.
Pitfalls:
- Tangential cuts.
- If you can trace the squamous cells from a gland to the surface it is less likely to be invasive cancer.
Notes on invasion:
- Nice review paper by Wenig.[7]
- See SCC of the cervix versus CIN III.
Image(s):
Subtypes
There are several subtypes:[8]
- Adenosquamous carcinoma.
- Ancatholytic squamous cell carcinoma.
- Basaloid squamous cell carcinoma - poor prognosis, usu. diagnosed by recognition of typical SCC.
- Carcinoma cuniculatum.
- Verrucous carcinoma - good prognosis, rare.
- Papillary squamous cell carcinoma.
- Lymphoepithelial carcinoma - rare.
- Spindle cell squamous carcinoma - a common spindle cell lesion of the H&N.
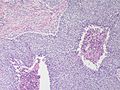
Carcinoma cuniculatum
General
- Rare.
- Good prognosis.[9]
Gross
- Usually lower extremities.
- Classically plantar aspect of foot.[9]
Microscopic
Features:
- Nests squamous epithelium with minimal atypia in the dermis - key feature.
- Hyperkeratosis.
- Parakeratosis.
- Acanthosis.
Verrucous squamous cell carcinoma
- AKA verrucous carcinoma.
Main article: Verrucous carcinoma
Spindle cell squamous carcinoma
General
- Common spindle cell lesion of the head and neck.
Microscopic
Feature:
- Histomorphologic key to the diagnosis: finding a component of conventional squamous cell carcinoma.
- Malignant spindle cell neoplasm.
DDx:
- Spindle cell melanoma.
- Mesenchymal neoplasms - see spindle cell lesions.
Images
IHC
- Typically keratin -ve.
- p63 +ve.
- Soft tissue tumour uncommonly positive.[11]
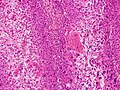
Basaloid squamous cell carcinoma
- Should not be confused with basosquamous carcinoma.
General
- May mimic adenoid cystic carcinoma.
- Classically base of tongue.[12]
- Typically poor prognosis.
Microscopic
Features:
- "Basaloid" cells - "blue" at low power.
- Nests.
- Basal pallisading.
- Nests.
- +/-Keratinization - useful.
- +/-Squamous dysplasia in overlying skin.
- Conventional squamous cell carcinoma.
DDx:
Clear cell squamous cell carcinoma
General
- Very rare.[13]
Microscopic
Features:
- Clear cytoplasm.
Images
Lymphoepithelial (squamous cell) carcinoma
- This is discussed in detail in the lymphoepithelioma-like carcinoma (LELC) article.
- In the head and neck this is a separate entity known as nasopharyngeal carcinoma.
General
Microscopic
Features:
- Malignant squamoid cells (eosinophilic cytoplasm, nuclear atypia).
- Abundant mononuclear inflammatory cells (plasma cells, lymphocytes).
Images: see the LELC article.
IHC
Features:[15]
- CK5/6 +ve.
- p63 +ve.
- K903 +ve.
- p16 +ve/-ve -- dependent on site, +ve favours non-lung SCC.[15]
- p40 +ve.
Note:
- Immunostains not particularly helpful for establishing primary site of squamous cell carcinoma. p16 may be helpful but is not definitive for non-lung SCC.[15]
See also
- Adenocarcinoma.
- Pseudoepitheliomatous hyperplasia - can mimic squamous cell carcinoma.
- Basics.
References
- ↑ Pentenero, M.; Gandolfo, S.; Carrozzo, M. (Dec 2005). "Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: a review of the literature.". Head Neck 27 (12): 1080-91. doi:10.1002/hed.20275. PMID 16240329.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/LipOralCav_11protocol.pdf. Accessed on: 3 April 2012.
- ↑ Yoder, BJ.; Rufforny, I.; Massoll, NA.; Wilkinson, EJ. (May 2008). "Stage IA vulvar squamous cell carcinoma: an analysis of tumor invasive characteristics and risk.". Am J Surg Pathol 32 (5): 765-72. doi:10.1097/PAS.0b013e318159a2cb. PMID 18379417.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/Vulva_11protocol.pdf. Accessed on: 3 April 2012.
- ↑ 5.0 5.1 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 975. ISBN 978-0781740517.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/LipOralCav_11protocol.pdf. Accessed on: 3 April 2012.
- ↑ Wenig BM (March 2002). "Squamous cell carcinoma of the upper aerodigestive tract: precursors and problematic variants". Mod. Pathol. 15 (3): 229–54. doi:10.1038/modpathol.3880520. PMID 11904340. http://www.nature.com/modpathol/journal/v15/n3/pdf/3880520a.pdf.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2011/LipOralCav_11protocol.pdf. Accessed on: 3 April 2012.
- ↑ 9.0 9.1 Kruse, AL.; Graetz, KW. (Jul 2009). "Carcinoma cuniculatum: a rare entity in the oral cavity.". J Craniofac Surg 20 (4): 1270-2. doi:10.1097/SCS.0b013e3181ace06b. PMID 19625845.
- ↑ Hall, JM.; Saenger, JS.; Fadare, O. (Mar 2008). "Diagnostic utility of P63 and CD10 in distinguishing cutaneous spindle cell/sarcomatoid squamous cell carcinomas and atypical fibroxanthomas.". Int J Clin Exp Pathol 1 (6): 524-30. PMID 18787630.
- ↑ Jo, VY.; Fletcher, CD. (Nov 2011). "p63 immunohistochemical staining is limited in soft tissue tumors.". Am J Clin Pathol 136 (5): 762-6. doi:10.1309/AJCPXNUC7JZSKWEU. PMID 22031315.
- ↑ URL: http://www.biomedcentral.com/1471-2407/6/146. Accessed on: March 9, 2010.
- ↑ Lawal, AO.; Adisa, AO.; Olajide, MA.; Olusanya, AA. (Jan 2013). "Clear cell variant of squamous cell carcinoma of skin: A report of a case.". J Oral Maxillofac Pathol 17 (1): 110-2. doi:10.4103/0973-029X.110697. PMID 23798842.
- ↑ Skinner, NE.; Horowitz, RI.; Majmudar, B. (Oct 2000). "Lymphoepithelioma-like carcinoma of the uterine cervix.". South Med J 93 (10): 1024-7. PMID 11147469.
- ↑ 15.0 15.1 15.2 Pereira, TC.; Share, SM.; Magalhães, AV.; Silverman, JF. (Jan 2011). "Can we tell the site of origin of metastatic squamous cell carcinoma? An immunohistochemical tissue microarray study of 194 cases.". Appl Immunohistochem Mol Morphol 19 (1): 10-4. doi:10.1097/PAI.0b013e3181ecaf1c. PMID 20823766.