Yolk sac tumour
Jump to navigation
Jump to search
Yolk sac tumour is an uncommon germ cell tumour that primarily afflicts infants and young boys.
| Yolk sac tumour | |
|---|---|
| Diagnosis in short | |
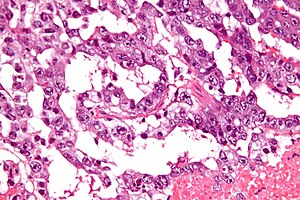 Yolk sac tumour. H&E stain. | |
|
| |
| LM | Schiller-Duval bodies (glomerulerus-like structures), variable architecture - usually reticular or microcystic |
| LM DDx | embryonal carcinoma, mixed germ cell tumour |
| IHC | AFP +ve, glypican 3 +ve, OCT3 -ve, CK19 +ve |
| Gross | white/yellow mucinous infiltrative mass |
| Grossing notes | orchiectomy grossing |
| Staging | testicular cancer staging |
| Site | testis, other |
|
| |
| Prevalence | rare |
| Blood work | alpha-fetoprotein (AFP) elevated |
| Prognosis | poor |
| Clin. DDx | other germ cell tumours |
It may be seen as part of mixed germ cell tumour. It is abbreviated YST.
It may be referred to as endodermal sinus tumour.
General
- Rare in pure form.
- Aggressive - especially extragonadal tumours.[1]
Epidemiology:
- Most common GCT in infants and young boys.
- Bimodal age distribution:[1]
- <4 years.
- 10-30 years.
Clinical:
- Elevated AFP.
Gross
- White/yellow mucinous infiltrative mass.[2]
Microscopic
Classic feature:[2]
- Schiller-Duval bodies.
- Look like glomerulus - central blood vessel surrounded by epithelial-like cells a space and more epithelial-like cells
- Architecure - variable.
- Reticular - most common according to WMSP.[3]
- Microcystic.
- Lace-like pattern.
- Endodermal sinus-like - has Schiller-Duval bodies.
- Solid.
- Papillary.
- Glandular.
- Alveolar.
- Enteric.
- Polyvesicular vitelline.
- Hepatoid.
- +/-Eosinophilic hyaline globules (contain alpha-fetoprotein).
Notes:
- Has a loose stroma/vaguely discohesive -- unlike embryonal carcinoma.
- How to remember patterns REMember PlS GAP EH (or REM PS GAPEH) = reticular, endodermal sinus, microcystic, papillary, solid, glandular, alveolar, polyvesicular vitelline, enteric, hepatoid.
- Yolk sac tumours in adults are essentially always a component of a mixed germ cell tumour, i.e. if one sees a pure yolk sac tumour in an adult, it is probably under sampled.[4]
Variants:
- Hepatoid pattern.[5]
- Vaguely resembles liver.
- Hyaline globules (light red well-circumscribed globs).
- Bile canaculi.
- Vaguely resembles liver.
- Solid pattern.[6]
- Vaguely resembles seminoma.
DDx:
- Embryonal carcinoma - more nuclear atypia, nuclei usually overlap and classically vesicular.
- Mixed germ cell tumour.
Images
Case 1
Case 2
Case 3
www images
IHC
ISUP consensus paper by Ulbright et al.:[8]
- OCT3 -ve.
- Positive in seminoma and embryonal carcinoma.
- Alpha-fetoprotein (abbreviated AFP) +ve.
- Glypican 3 +ve.
- More sensitive than AFP.[9]
Others:
- CK19 +ve.[10]
- Seminoma -ve, embryonal carcinoma -ve, GCNIS (ITGCN) -ve, normal testis -ve.
- Cytokeratin +ve.[citation needed]
- CD30 -ve.
- Positive in embryonal carcinoma.[11]
- OCT3/4 -ve.
- Alpha-1-antitrypsin +ve (abbreviated A1A).[12]
- CDX2 +ve in 8 of 20 cases with YST (versus glypican-3).[13]
See also
References
- ↑ 1.0 1.1 Shah, JP.; Kumar, S.; Bryant, CS.; Ali-Fehmi, R.; Malone, JM.; Deppe, G.; Morris, RT. (Dec 2008). "A population-based analysis of 788 cases of yolk sac tumors: A comparison of males and females.". Int J Cancer 123 (11): 2671-5. doi:10.1002/ijc.23792. PMID 18767035.
- ↑ 2.0 2.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 510. ISBN 978-1416054542.
- ↑ Humphrey, Peter A; Dehner, Louis P; Pfeifer, John D (2008). The Washington Manual of Surgical Pathology (1st ed.). Lippincott Williams & Wilkins. pp. 369. ISBN 978-0781765275.
- ↑ Talerman, A. (Jul 1975). "The incidence of yolk sac tumor (endodermal sinus tumor) elements in germ cell tumors of the testis in adults.". Cancer 36 (1): 211-5. PMID 1203848.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=6. Accessed on: March 8, 2010.
- ↑ URL: http://webpathology.com/image.asp?case=34&n=8. Accessed on: March 8, 2010.
- ↑ Sesterhenn, IA.; Davis, CJ.. "Pathology of germ cell tumors of the testis.". Cancer Control 11 (6): 374-87. PMID 15625525.
- ↑ Ulbright TM, Tickoo SK, Berney DM, Srigley JR (August 2014). "Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): e50–9. doi:10.1097/PAS.0000000000000233. PMID 24832161.
- ↑ Emerson, RE.; Ulbright, TM. (Jun 2010). "Intratubular germ cell neoplasia of the testis and its associated cancers: the use of novel biomarkers.". Pathology 42 (4): 344-55. doi:10.3109/00313021003767355. PMID 20438407.
- ↑ Bremmer, F.; Ströbel, P.; Hubertus, H.; Strecker, J.; Gaisa, N.; Strauß, A.; Schweyer, S.; Radzun, H-J. et al. (2015). [www.diagnosticpathology.org/content/10/1/7Cached "CK19 is a sensitive marker for yolk sac tumours of the testis."]. Diagnostic Pathology 10 (7). doi:10.1186/s13000-015-0243-y. www.diagnosticpathology.org/content/10/1/7Cached.
- ↑ Gopalan, A.; Dhall, D.; Olgac, S.; Fine, SW.; Korkola, JE.; Houldsworth, J.; Chaganti, RS.; Bosl, GJ. et al. (Aug 2009). "Testicular mixed germ cell tumors: a morphological and immunohistochemical study using stem cell markers, OCT3/4, SOX2 and GDF3, with emphasis on morphologically difficult-to-classify areas.". Mod Pathol 22 (8): 1066-74. doi:10.1038/modpathol.2009.66. PMID 19396148.
- ↑ Beilby, JO.; Horne, CH.; Milne, GD.; Parkinson, C. (May 1979). "Alpha-fetoprotein, alpha-1-antitrypsin, and transferrin in gonadal yolk-sac tumours.". J Clin Pathol 32 (5): 455-61. PMID 89123.
- ↑ Bing, Z.; Pasha, T.; Tomaszewski, JE.; Zhang, P. (Oct 2009). "CDX2 expression in yolk sac component of testicular germ cell tumors.". Int J Surg Pathol 17 (5): 373-7. doi:10.1177/1066896909338598. PMID 19578052.