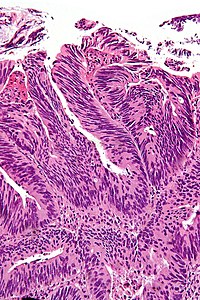
Surgical margins
The surgical margins, often simply referred to as margins, are the set of surfaces that were cut by the surgeon in order to remove the specimen from the body. The distance between the tumour and the margin is called the surgical clearance, a term that may be used interchangeably with the term surgical margin.[1] Margins are important as an incompletely removed disease process may lead to re-occurrence.
Most often, positive margins, i.e. surgical margins with disease present or "very close", are non-optimal. For example, in locally advanced rectal cancer, in one study,[2] five year survival was found to be 60%, 31% and 0% for R0 (no tumour at the margin), R1 (microscopic tumour at the margin), and R2 (macroscopic tumour at the margin) resections respectively.
What defines a positive surgical margin is dependent on the tumour and its biology; definitions of positive margin are dependent on the anatomical site.
Types of margins
- En face (formally en face margin).
- Sample the complete surface.
- No information about the distance between the margin and lesion can be obtained (from the glass slide).
- On edge (formally on edge margin), AKA perpendicular margin, as the cut to prepare the tissue for microscopic examination is perpendicular to the cut from the surgeon.
- Sample a subset of the surface.
- The distance between the margin and lesion can be measured (on the glass slide).
Adequate margin
- What constitutes an adequate margin is dependent on the tumour type, as different tumours have different behaviours.
Adequate margins by tumour
| Tumour | Adequate pathologic margin | Adequate clinical margin | System |
|---|---|---|---|
| Colorectal carcinoma | >=1 mm;[3][4][5] circumferential margin (esp. in rectal carcinoma) most important[6] | 1 cm[7] | Gastrointestinal pathology |
| Vulvar carcinoma | 0.8 cm (fixed)[8] | 1.0 cm (fresh)[8] | Gynecologic pathology |
| Malignant melanoma | same as clinical (interesting is that CAP says "no minimum safe distance established"[9]) | Dermatopathology | |
| Ductal carcinoma in situ | > 2mm[15]; if < 1 mm patient benefits from radiation[16] | Breast pathology | |
| Invasive breast carcinoma | cannot be at margin - no consensus beyond that;[17] no statistical difference between 1 and 2 mm margins for Stage I & II tumours[18] | Breast pathology | |
| Sarcoma | >= 1 cm[19] | Sarcoma | |
| Prostate carcinoma | tumour not touching ink - "close" margins have a higher biochemical recurrence[20] | Genitourinary pathology | |
| Renal cell carcinoma | tumour not touching ink; positive margins get clinical follow-up as recurrences are uncommon[21] | Genitourinary pathology | |
| Squamous cell carcinoma of the skin | 4 mm, 6 mm for high risk[22] | Dermatopathology | |
| Urothelial carcinoma | tumour not touching ink[23] | Genitourinary pathology |
Sign out
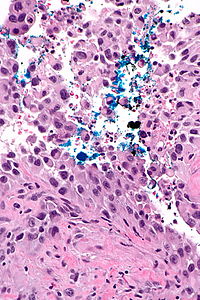
Stray ink versus true positive
True positive
COMMENT: Ink is seen very focally on a fragment of tumour in A21-1. Inspection of the tissue block shows ink on the surface of the tissue fragment with the positive margin; this essentially excludes that what is interpreted as a positive margin could represent stray ink.
Stray ink
COMMENT: The margin assessment is suboptimal as the specimen was cut prior to inking. Ink on tumour in this context may represent stray ink on tumour or a true positive margin. Ink is focally present on tumour in this case and it is favoured to represent stray ink, as the quantity of ink is minimal; however, margin positivity cannot be completely excluded.
See also
References
- ↑ Ng, IO.; Luk, IS.; Yuen, ST.; Lau, PW.; Pritchett, CJ.; Ng, M.; Poon, GP.; Ho, J. (Mar 1993). "Surgical lateral clearance in resected rectal carcinomas. A multivariate analysis of clinicopathologic features.". Cancer 71 (6): 1972-6. PMID 8443747.
- ↑ Larsen SG, Wiig JN, Dueland S, Giercksky KE (April 2008). "Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer". Eur J Surg Oncol 34 (4): 410–7. doi:10.1016/j.ejso.2007.05.012. PMID 17614249.
- ↑ Petersen, VC.; Baxter, KJ.; Love, SB.; Shepherd, NA. (Jul 2002). "Identification of objective pathological prognostic determinants and models of prognosis in Dukes' B colon cancer.". Gut 51 (1): 65-9. PMC 1773289. PMID 12077094. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1773289/.
- ↑ Fitzgerald, TL.; Brinkley, J.; Zervos, EE. (Nov 2011). "Pushing the envelope beyond a centimeter in rectal cancer: oncologic implications of close, but negative margins.". J Am Coll Surg 213 (5): 589-95. doi:10.1016/j.jamcollsurg.2011.07.020. PMID 21856181.
- ↑ Quirke, P.; Durdey, P.; Dixon, MF.; Williams, NS. (Nov 1986). "Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision.". Lancet 2 (8514): 996-9. PMID 2430152.
- ↑ Adam, IJ.; Mohamdee, MO.; Martin, IG.; Scott, N.; Finan, PJ.; Johnston, D.; Dixon, MF.; Quirke, P. (Sep 1994). "Role of circumferential margin involvement in the local recurrence of rectal cancer.". Lancet 344 (8924): 707-11. PMID 7915774.
- ↑ Rutkowski, A.; Bujko, K.; Nowacki, MP.; Chmielik, E.; Nasierowska-Guttmejer, A.; Wojnar, A. (Nov 2008). "Distal bowel surgical margin shorter than 1 cm after preoperative radiation for rectal cancer: is it safe?". Ann Surg Oncol 15 (11): 3124-31. doi:10.1245/s10434-008-0125-6. PMID 18766404.
- ↑ 8.0 8.1 Palaia, I.; Bellati, F.; Calcagno, M.; Musella, A.; Perniola, G.; Panici, PB. (Aug 2011). "Invasive vulvar carcinoma and the question of the surgical margin.". Int J Gynaecol Obstet 114 (2): 120-3. doi:10.1016/j.ijgo.2011.02.012. PMID 21669423.
- ↑ URL: http://www.cap.org/apps/docs/committees/cancer/cancer_protocols/2012/SkinMelanoma_12protocol.pdf. Accessed on: 19 August 2012.
- ↑ Kunishige, JH.; Brodland, DG.; Zitelli, JA. (Mar 2012). "Surgical margins for melanoma in situ.". J Am Acad Dermatol 66 (3): 438-44. doi:10.1016/j.jaad.2011.06.019. PMID 22196979.
- ↑ Möller, MG.; Pappas-Politis, E.; Zager, JS.; Santiago, LA.; Yu, D.; Prakash, A.; Kinal, A.; Clark, GS. et al. (Jun 2009). "Surgical management of melanoma-in-situ using a staged marginal and central excision technique.". Ann Surg Oncol 16 (6): 1526-36. doi:10.1245/s10434-008-0239-x. PMID 19050971.
- ↑ Cohn-Cedermark, G.; Rutqvist, LE.; Andersson, R.; Breivald, M.; Ingvar, C.; Johansson, H.; Jönsson, PE.; Krysander, L. et al. (Oct 2000). "Long term results of a randomized study by the Swedish Melanoma Study Group on 2-cm versus 5-cm resection margins for patients with cutaneous melanoma with a tumor thickness of 0.8-2.0 mm.". Cancer 89 (7): 1495-501. PMID 11013363.
- ↑ Veronesi, U.; Cascinelli, N. (Apr 1991). "Narrow excision (1-cm margin). A safe procedure for thin cutaneous melanoma.". Arch Surg 126 (4): 438-41. PMID 2009058.
- ↑ Balch, CM.; Soong, SJ.; Smith, T.; Ross, MI.; Urist, MM.; Karakousis, CP.; Temple, WJ.; Mihm, MC. et al. (Mar 2001). "Long-term results of a prospective surgical trial comparing 2 cm vs. 4 cm excision margins for 740 patients with 1-4 mm melanomas.". Ann Surg Oncol 8 (2): 101-8. PMID 11258773.
- ↑ Dunne, C.; Burke, JP.; Morrow, M.; Kell, MR. (Apr 2009). "Effect of margin status on local recurrence after breast conservation and radiation therapy for ductal carcinoma in situ.". J Clin Oncol 27 (10): 1615-20. doi:10.1200/JCO.2008.17.5182. PMID 19255332.
- ↑ Silverstein, MJ.; Lagios, MD.; Groshen, S.; Waisman, JR.; Lewinsky, BS.; Martino, S.; Gamagami, P.; Colburn, WJ. (May 1999). "The influence of margin width on local control of ductal carcinoma in situ of the breast.". N Engl J Med 340 (19): 1455-61. doi:10.1056/NEJM199905133401902. PMID 10320383.
- ↑ Singletary, SE. (Nov 2002). "Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy.". Am J Surg 184 (5): 383-93. PMID 12433599.
- ↑ Hardy, K.; Fradette, K.; Gheorghe, R.; Lucman, L.; Latosinsky, S. (Nov 2008). "The impact of margin status on local recurrence following breast conserving therapy for invasive carcinoma in Manitoba.". J Surg Oncol 98 (6): 399-402. doi:10.1002/jso.21126. PMID 18767118.
- ↑ Baldini, EH.; Goldberg, J.; Jenner, C.; Manola, JB.; Demetri, GD.; Fletcher, CD.; Singer, S. (Oct 1999). "Long-term outcomes after function-sparing surgery without radiotherapy for soft tissue sarcoma of the extremities and trunk.". J Clin Oncol 17 (10): 3252-9. PMID 10506627.
- ↑ Lu, J.; Wirth, GJ.; Wu, S.; Chen, J.; Dahl, DM.; Olumi, AF.; Young, RH.; McDougal, WS. et al. (Jul 2012). "A close surgical margin after radical prostatectomy is an independent predictor of recurrence.". J Urol 188 (1): 91-7. doi:10.1016/j.juro.2012.02.2565. PMID 22578729.
- ↑ Marszalek, M.; Carini, M.; Chlosta, P.; Jeschke, K.; Kirkali, Z.; Knüchel, R.; Madersbacher, S.; Patard, JJ. et al. (Apr 2012). "Positive surgical margins after nephron-sparing surgery.". Eur Urol 61 (4): 757-63. doi:10.1016/j.eururo.2011.11.028. PMID 22136987.
- ↑ Brodland, DG.; Zitelli, JA. (Aug 1992). "Surgical margins for excision of primary cutaneous squamous cell carcinoma.". J Am Acad Dermatol 27 (2 Pt 1): 241-8. PMID 1430364.
- ↑ Dotan, ZA.; Kavanagh, K.; Yossepowitch, O.; Kaag, M.; Olgac, S.; Donat, M.; Herr, HW. (Dec 2007). "Positive surgical margins in soft tissue following radical cystectomy for bladder cancer and cancer specific survival.". J Urol 178 (6): 2308-12; discussion 2313. doi:10.1016/j.juro.2007.08.023. PMID 17936804.