Difference between revisions of "Parathyroid glands"
Jump to navigation
Jump to search
| Line 273: | Line 273: | ||
Features:<ref>{{Ref PBoD8|1128}}</ref> | Features:<ref>{{Ref PBoD8|1128}}</ref> | ||
*Histologically normal parathyroid cells. | *Histologically normal parathyroid cells. | ||
**Cytologic features not reliable for diagnosis. | **Cytologic features '''not''' reliable for diagnosis. | ||
*Fibrous capsule. | *Fibrous capsule. | ||
*Invasion of surrounding tissue - '''key feature'''. | *Invasion of surrounding tissue - '''key feature'''. | ||
| Line 285: | Line 285: | ||
===IHC=== | ===IHC=== | ||
*Ki-67 >6% of cells positive - | *Ki-67 >6% of cells positive - supports diagnosis.<ref name=pmid7860042>{{Cite journal | last1 = Abbona | first1 = GC. | last2 = Papotti | first2 = M. | last3 = Gasparri | first3 = G. | last4 = Bussolati | first4 = G. | title = Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining. | journal = Hum Pathol | volume = 26 | issue = 2 | pages = 135-8 | month = Feb | year = 1995 | doi = | PMID = 7860042 }}</ref> | ||
**Parathyroid adenomas and hyperplasias ~ 3%. | **Parathyroid adenomas and hyperplasias ~ 3%. | ||
Revision as of 18:59, 8 September 2015
The parathyroid glands are an endocrine organ that is important in calcium regulation. They often make an appearance in the context of thyroid surgery.
They produce parathyroid hormone (PTH). PTH acts to increase serum calcium and is important in the regulation of the calcium balance.
Clinical
Hyperparathyroidism
- Definition: increased secretion of parathyroid hormone (PTH).[1]
What PTH does:[1]
- Increase serum calcium.
- Decrease serum phosphate.
Classification
- Primary.
- Secondary.
- Tertiary.
Overview in a table
| Type | PTH | Calcium | Common causes |
|---|---|---|---|
| Primary hyperparathyroidism | high | high | parathyroid adenoma (~85-90% of cases), parathyroid hyperplasia (~10-15% of cases) |
| Secondary hyperparathyroidism | high | low or normal | chronic renal failure, vitamin D deficiency[2] |
| Tertiary hyperparathyroidism | high | high | persistent hyperparathyroidism after renal transplant[3] |
Hypercalcemia DDx
Mnemonic GRIMED:[4]
- Granulomatous disease (tuberculosis, sarcoidosis).
- Renal disease.
- Immobility.
- Malignancy (esp. squamous cell carcinoma, plasmacytoma).
- Endocrine (primary hyperparathyroidism, tertiary hyperparathyroidism, familial hypocalciuric hypercalcemia (FHH)).
- Drugs (thiazides ... others).
Note:
- Hyperparathyroidism and FHH are assoc. with an increased PTH.[5]
- Other causes are assoc. with a decreased PTH.
Primary hyperparathyroidism
Cause:[6]
- Parathyroid adenoma ~90%.
- Parathyroid hyperplasia ~10%.
- Parathyroid carcinoma ~1%.
Familial causes of primary hyperparathyroidism:
- MEN 1.
- MEN 2A.
- Familial hypocalciuric hypercalcemia.
- Autosomal dominant.
- CASR (calcium sensing receptor) gene defect.[7]
Classic manifestations moans, stones, bones, (abdominal) groans, psychiatric overtones.[8][9]
- Moans = bone pain.
- Stones = nephrolithiasis (kidney stones).
- Bones = bone pathology, e.g. osteitis fibrosa cystica.[10]
- Groans = constipation.
- Psychiatric overtones = CNS pathology.
- Can include: lethargy, fatigue, depression, memory loss, psychosis, ataxia, delirium, and coma.
Hypoparathyroidism
- Rare vis-à-vis hyperparathyroidism.
- Classically iatrogenic, i.e. the surgeon removing 'em.[5]
Other causes:[11]
- Autoimmune hypoparathyroidism.
- Autosomal dominat hypoparathyroidism.
- Familial isolated hypoparathyroidism.
- Congenital absence (DiGeorge syndrome).
- Drugs - proton pump inhibitors.[12][13]
Normal parathyroid glands
- The cytology is dealt with in normal parathyroid cytology.
General
- Identification of normal can be tricky.
Gross
- No distinctive features - surgeons thus send 'em to pathologists.
Microscopic
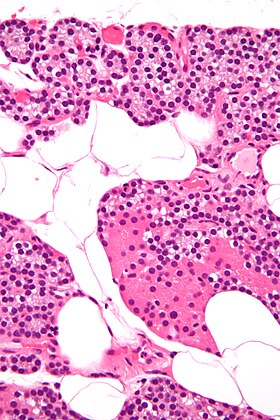
Features:[14]
- Low power:
- May vaguely resemble lymphoid tissue - may have hyperchromatic cytoplasm.
- Does not have follicular centres like a lymph node.
- May form gland-like structure and vaguely resemble the thyroid at low power.
- Cytoplasm may be clear[15] - key feature.
- Surrounded by a thin fibrous capsule.
- May vaguely resemble lymphoid tissue - may have hyperchromatic cytoplasm.
- High power:
- Mixed cell population:[16]
- Chief cells - predominant cell type, small, cytoplasm has variable staining (hyperchromatic-clear-eosinophilic).
- Oxyphil cells (acid staining cells[17]) - abundant cytoplasm.
- Adipocytes - dependent on age, body habitus, PT hormone, size of gland.[18]
- Increased with age, may be used to help differentiate from thyroid - key feature.
- Mixed cell population:[16]
Images
www:
Parathyroid cell types
| Name | Staining (cytoplasm) | Quantity of cells | Cytoplasm (quantity) | Function |
| (parathyroid) chief cells | intense hyperchromatic to eosinophilic (see note) | abundant | moderate | manufacture parathyroid hormone (PTH) |
| oxyphil cells | moderate/light hyperchromatic to eosinophilic | rare | abundant | ? |
Notes:
- Cytoplasmic staining varies considerably on H&E preparations - it may vary from hyperchromatic[19] to clear to eosinophilic.[20]
- Chief cells tend to stain more intensely than oxyphil cells.
Thyroid versus parathyroid
- Parathyroid cytoplasm:
- Hyperchromatic.
See: Parathyroid image (okstate.edu).
Parathyroid versus lymphoid tissue
- Parathyroid:
- No germinal centres.
- Gland-like/follicular-like arrangement may be present but usually much smaller than normal thyroid follicles.
- May be confused with thyroid microfollicules.
- Occasional cell with rim of clear cytoplasm (oxyphil?).
- Nuclei are different:
- Slightly larger than in lymphocytes (1.2-1.5x the size)
- Stippled chromatin (unlike lymphocytes).
Images:
Specific entities
Parathyroid hyperplasia
General
- Chief cell hyperplasia - associated with MEN 1, MEN 2A.[22]
- Parathyroid hyperplasia - classically assoc. with renal failure.
Gross
- Classically all parathyroid glands are involved; however, some may be spared making it difficult to differentiate this from parathyroid adenoma.[23]
Microscopic
Features:[23]
- Classically have abundant adipose tissue.
- +/-Water-clear cells ("water-clear cell hyperplasia").
Note:
- Generally, it is impossible to discern between parathyroid adenomas and parathyroid hyperplasias by histology alone.[24]
- One requires information of the size of the other glands to make the diagnosis.
DDx:
- Parathyroid adenoma - classically have a rim of normal parathyroid gland around it.
Parathyroid adenoma
General
MEN 1:
- Parathyroid adenoma.
- Pancreatic neuroendocrine tumour.
- Pituitary adenoma.
MEN 2A:
- Parathyroid adenoma.
- Medullary thyroid carcinoma.
- Pheochromocytoma.
Subtypes
Histologic subtyping:[25]
- Chief cell parathyroid adenoma.
- Common.
- Oxyphil parathyroid adenoma.
- Uncommon.[26]
- Mixed.
Microscopic
Features - general:
- Classically have a rim of normal parathyroid gland around it.[24]
Note:
- Generally, it is impossible to discern between parathyroid adenomas and parathyroid hyperplasias by histology alone.[24]
- One requires information of the size of the other glands to make the diagnosis.
Chief cell parathyroid adenoma
Features:[6]
- Chief cells - key feature:
- Small central nucleus.
- Round with stippled chromatin - important.
- Moderate cytoplasm.
- Small central nucleus.
- +/-Scattered oxyphil cells:
- Large cells.
- Abundant cytoplasm.
- Architecture:
- Nests.
- Circular formations - often around capillaries (perivascular pseudorosettes).
Images
Oxyphil parathyroid adenoma
Features:[6]
- Oxyphil cells:
- Large cells.
- Abundant cytoplasm.
DDx:
- Hürthle cell adenoma of the thyroid gland.
Image:
Sign out
Note:
- One should not say "negative for malignancy".
Parathyroid Gland, Excision: - Chief cell parathyroid adenoma with adjacent residual parathyroid.
Parathyroid Gland (Submitted as "Right Superior Parathyroid Adenoma"), Excision: - Parathyroid adenoma with adjacent residual parathyroid.
Block letters
PARATHRYOID GLAND, EXCISION: - CHIEF CELL PARATHYROID ADENOMA.
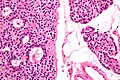
Parathyroid carcinoma
General
- Extremely rare.
Microscopic
Features:[28]
- Histologically normal parathyroid cells.
- Cytologic features not reliable for diagnosis.
- Fibrous capsule.
- Invasion of surrounding tissue - key feature.
- +/-Metastasis - diagnostic feature.
Note:
- Diagnosis of parathyroid carcinoma is like that of malignant pheochromocytoma - cytology useless, tissue invasion and metastases are the key features.
Image:
IHC
- Ki-67 >6% of cells positive - supports diagnosis.[29]
- Parathyroid adenomas and hyperplasias ~ 3%.
See also
References
- ↑ 1.0 1.1 URL: http://emedicine.medscape.com/article/127351-overview. Accessed on: 24 January 2013.
- ↑ URL: http://emedicine.medscape.com/article/127351-overview#aw2aab6b5. Accessed on: 24 January 2013.
- ↑ URL: http://emedicine.medscape.com/article/127351-overview#aw2aab6b6. Accessed on: 24 January 2013.
- ↑ Shiau, Carolyn; Toren, Andrew (2006). Toronto Notes 2006: Comprehensive Medical Reference (Review for MCCQE 1 and USMLE Step 2) (22nd edition (2006) ed.). Toronto Notes for Medical Students, Inc.. pp. Emerg.. ISBN 978-0968592861.
- ↑ 5.0 5.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1129. ISBN 978-1416031215.
Cite error: Invalid
<ref>tag; name "Ref_PBoD8_1129" defined multiple times with different content - ↑ 6.0 6.1 6.2 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1127. ISBN 978-1416031215.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) 601199
- ↑ Lienert, D.; Rege, S. (Feb 2008). "Moans, stones, groans, bones and psychiatric overtones: lithium-induced hyperparathyroidism.". Aust N Z J Psychiatry 42 (2): 171-3. PMID 18350681.
- ↑ URL: http://www.usmleforum.com/files/forum/2010/1/505388.php. Accessed on: 4 December 2011.
- ↑ França, TC.; Griz, L.; Pinho, J.; Diniz, ET.; Andrade, LD.; Lucena, CS.; Beserra, SR.; Asano, NM. et al. (Apr 2011). "Bisphosphonates can reduce bone hunger after parathyroidectomy in patients with primary hyperparathyroidism and osteitis fibrosa cystica.". Rev Bras Reumatol 51 (2): 131-7. PMID 21584419.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1130. ISBN 978-1416031215.
- ↑ Deroux, A.; Khouri, C.; Chabre, O.; Bouillet, L.; Casez, O. (Oct 2014). "Severe acute neurological symptoms related to proton pump inhibitors induced hypomagnesemia responsible for profound hypoparathyroidism with hypocalcemia.". Clin Res Hepatol Gastroenterol 38 (5): e103-5. doi:10.1016/j.clinre.2014.03.005. PMID 24736034.
- ↑ Toh, JW.; Ong, E.; Wilson, R. (Aug 2014). "Hypomagnesaemia associated with long-term use of proton pump inhibitors.". Gastroenterol Rep (Oxf). doi:10.1093/gastro/gou054. PMID 25138239.
- ↑ http://www.medicalhistology.us/twiki/pub/Main/ChapterFourteenSlides/b56b_parathyroid_40x_he_labeled.jpg
- ↑ http://pathology.mc.duke.edu/research/Histo_course/parathyroid2.jpg
- ↑ http://www.bu.edu/histology/p/15002loa.htm
- ↑ http://dictionary.reference.com/search?q=oxyphil%20cell
- ↑ Iwasaki, A.; Shan, L.; Kawano, I.; Nakamura, M.; Utsuno, H.; Kobayashi, A.; Kuma, K.; Kakudo, K. (Jul 1995). "Quantitative analysis of stromal fat content of human parathyroid glands associated with thyroid diseases using computer image analysis.". Pathol Int 45 (7): 483-6. PMID 7551007.
- ↑ http://www.deltagen.com/target/histologyatlas/atlas_files/endocrine/parathyroid_and_thyroid_glands_20x.jpg
- ↑ http://instruction.cvhs.okstate.edu/Histology/HistologyReference/hrendo.htm
- ↑ Johnson, SJ.; Sheffield, EA.; McNicol, AM. (Apr 2005). "Best practice no 183. Examination of parathyroid gland specimens.". J Clin Pathol 58 (4): 338-42. doi:10.1136/jcp.2002.002550. PMC 1770637. PMID 15790694. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770637/.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970475-2. Accessed on: 29 July 2010.
- ↑ 23.0 23.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1128. ISBN 978-1416031215.
- ↑ 24.0 24.1 24.2 Taxy, J.; Husain, A; Montag, A. (2009). Biopsy Interpretation: The Frozen Section (1st ed.). Lippincott Williams & Wilkins. pp. 191. ISBN 978-0781767798.
- ↑ Moran, CA.; Suster, S. (Nov 2005). "Primary parathyroid tumors of the mediastinum: a clinicopathologic and immunohistochemical study of 17 cases.". Am J Clin Pathol 124 (5): 749-54. doi:10.1309/WJEL-N05L-9A06-9DU0. PMID 16203274.
- ↑ Fleischer, J.; Becker, C.; Hamele-Bena, D.; Breen, TL.; Silverberg, SJ. (Dec 2004). "Oxyphil parathyroid adenoma: a malignant presentation of a benign disease.". J Clin Endocrinol Metab 89 (12): 5948-51. doi:10.1210/jc.2004-1597. PMID 15579742.
- ↑ URL: http://library.med.utah.edu/WebPath/EXAM/IMGQUIZ/enfrm.html. Accessed on: 6 December 2010.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1128. ISBN 978-1416031215.
- ↑ Abbona, GC.; Papotti, M.; Gasparri, G.; Bussolati, G. (Feb 1995). "Proliferative activity in parathyroid tumors as detected by Ki-67 immunostaining.". Hum Pathol 26 (2): 135-8. PMID 7860042.