Difference between revisions of "Intracystic papillary carcinoma of the breast"
Jump to navigation
Jump to search
(redirect) |
m (touch) |
||
| (4 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Breast PapillaryCarcinomaEncysted PA.JPG | |||
| Width = | |||
| Caption = Intracystic Papillary Breast Carcinoma. [[H&E stain]]. | |||
| Synonyms = | |||
| Micro = Papillary lesion within a cyst | |||
| Subtypes = | |||
| LMDDx = [[Intraductal papilloma]], papillary [[DCIS]], [[Invasive papillary breast carcinoma]] | |||
| Stains = | |||
| IHC = | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[breast]] | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = +/-bloody discharge from nipple | |||
| Symptoms = | |||
| Prevalence = Rare | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = very good | |||
| Other = | |||
| ClinDDx = other breast tumours | |||
| Tx = surgical | |||
}} | |||
'''Intracystic papillary carcinoma of the breast''', also known as '''encapsulated papillary carcinoma of the breast''' (abbreviated '''EPC'''), is an uncommon type of [[breast cancer]] with a very good prognosis. | |||
It should not be confused with the ''[[invasive papillary carcinoma of the breast]]'', a more aggressive tumour of the breast. | |||
==General== | |||
*Very good prognosis<ref name=pmid21753694>{{Cite journal | last1 = Rakha | first1 = EA. | last2 = Gandhi | first2 = N. | last3 = Climent | first3 = F. | last4 = van Deurzen | first4 = CH. | last5 = Haider | first5 = SA. | last6 = Dunk | first6 = L. | last7 = Lee | first7 = AH. | last8 = Macmillan | first8 = D. | last9 = Ellis | first9 = IO. | title = Encapsulated papillary carcinoma of the breast: an invasive tumor with excellent prognosis. | journal = Am J Surg Pathol | volume = 35 | issue = 8 | pages = 1093-103 | month = Aug | year = 2011 | doi = 10.1097/PAS.0b013e31821b3f65 | PMID = 21753694 }}</ref> - it is similar to [[DCIS]]. | |||
*Classically menopausal women. | |||
*~30% present with bloody discharge.<ref name=pmid21057133>{{Cite journal | last1 = Rodríguez | first1 = MC. | last2 = Secades | first2 = AL. | last3 = Angulo | first3 = JM. | title = Best cases from the AFIP: intracystic papillary carcinoma of the breast. | journal = Radiographics | volume = 30 | issue = 7 | pages = 2021-7 | month = Nov | year = 2010 | doi = 10.1148/rg.307105003 | PMID = 21057133 | URL = http://radiographics.rsnajnls.org/cgi/pmidlookup?view=long&pmid=21057133 }}</ref> | |||
==Microscopic== | |||
Features: | |||
*Lesion confined to a cyst. | |||
**May have a thick fibrous capsule | |||
**The involved space is ''not'' lined by myoepithelial cells. | |||
*The cyst contains an abnormal epithelial proliferation with cribriform, solid or papillary architecture. | |||
**Loss of myoepithelial cells within the epithelial proliferation is a '''key feature'''. | |||
**Scattered large cells with pale eosinophilic cytoplasm may be observed<ref>{{Cite journal | last1 = Collins | first1 = LC. | last2 = Schnitt | first2 = SJ. | title = Papillary lesions of the breast: selected diagnostic and management issues. | journal = Histopathology | volume = 52 | issue = 1 | pages = 20-9 | month = Jan | year = 2008 | doi = 10.1111/j.1365-2559.2007.02898.x | PMID = 18171414 }} | |||
</ref>. | |||
***These cells are so-called globoid cells or clear cells and are immunoreactive for [[GCDFP-15]]. | |||
***They should not be mistaken for myoepithelial cells. | |||
**Neoplastic epithelial cells: | |||
***[[Nuclear atypia]] - including: nucleoli, [[nuclear pleomorphism]]. | |||
Notes: | |||
*Many potential pitfalls with papillary breast lesions on needle core biopsy. | |||
**Complete excision is recommended.<ref name=pmid22244207>{{Cite journal | last1 = Rizzo | first1 = M. | last2 = Linebarger | first2 = J. | last3 = Lowe | first3 = MC. | last4 = Pan | first4 = L. | last5 = Gabram | first5 = SG. | last6 = Vasquez | first6 = L. | last7 = Cohen | first7 = MA. | last8 = Mosunjac | first8 = M. | title = Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up. | journal = J Am Coll Surg | volume = 214 | issue = 3 | pages = 280-7 | month = Mar | year = 2012 | doi = 10.1016/j.jamcollsurg.2011.12.005 | PMID = 22244207 }}</ref> | |||
*Adequately and carefully sample the specimen to exclude an invasive component. | |||
*Report only the size of the invasive component (if present) to prevent over-estimation of tumor stage. | |||
DDx:<ref name=pmid18171414>{{Cite journal | last1 = Collins | first1 = LC. | last2 = Schnitt | first2 = SJ. | title = Papillary lesions of the breast: selected diagnostic and management issues. | journal = Histopathology | volume = 52 | issue = 1 | pages = 20-9 | month = Jan | year = 2008 | doi = 10.1111/j.1365-2559.2007.02898.x | PMID = 18171414 }} | |||
</ref><ref>{{Cite journal | last1 = Pathmanathan | first1 = N. | last2 = Albertini | first2 = AF. | last3 = Provan | first3 = PJ. | last4 = Milliken | first4 = JS. | last5 = Salisbury | first5 = EL. | last6 = Bilous | first6 = AM. | last7 = Byth | first7 = K. | last8 = Balleine | first8 = RL. | title = Diagnostic evaluation of papillary lesions of the breast on core biopsy. | journal = Mod Pathol | volume = 23 | issue = 7 | pages = 1021-8 | month = Jul | year = 2010 | doi = 10.1038/modpathol.2010.81 | PMID = 20473278 }}</ref>: | |||
*[[Intraductal papilloma]]. | |||
**Absent or scant stroma favors papillary carcinoma over papilloma. | |||
**Is there a single cell or dual cell population in the lesion? | |||
***ER staining will be heterologous in a benign lesion. | |||
***Myoepithelial markers (calponin/p63/SMA +ve)s hould be positive in a benign lesion. | |||
*[[Papillary ductal carcinoma in situ]]. | |||
**Papillary DCIS shows myoepithelial cells (calponin/p63/SMA +ve) at the periphery of the involved spaces | |||
**But papillary DCIS should be negative for myoepithelial cells within the focus of DCIS | |||
**Papillary intracystic carcinoma does not show myoepithelial cells at the periphery of the involved spaces | |||
*[[Invasive papillary carcinoma of the breast]]. | |||
**Similar architecture but no cystic space, frankly invasive. | |||
**Very rare. | |||
*Invasive carcinoma arising in association with papillary intracystic carcinoma | |||
**Epithelial entrapment in the encysting fibrous tissue should not be interpreted as invasion. | |||
**Carcinoma must be seen in the breast tissue outside the encysting fibrous tissue. | |||
**Infiltrating carcinoma is usually of the 'no special type' variety. | |||
*[[Adenoid cystic carcinoma of the breast]] | |||
**The solid variant looks basaloid - solid adenoid cystic carcinoma or a 'basal-like' carcinoma should be considered in these cases. | |||
===Images=== | |||
<gallery> | |||
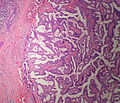
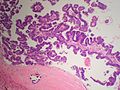
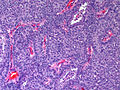
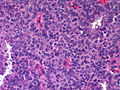
Image:Breast PapillaryCarcinomaEncysted 3 PA.JPG|Breast - Intracystic Papillary Carcinoma - Medium power (SKB) | |||
Image:Breast PapillaryCarcinomaEncysted 2 PA.JPG|Breast - Intracystic Papillary Carcinoma - Medium power (SKB) | |||
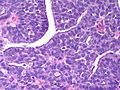
Image:Breast PapillaryCarcinomaEncysted PA.JPG|Breast - Intracystic Papillary Carcinoma - High power (SKB) | |||
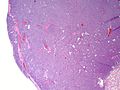
Image:Breast Carcinoma Papillary Intracystic SolidVariant LP CTR.jpg|Breast - Papillary Intracystic Carcinoma, Solid Variant - low power (SKB) | |||
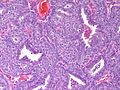
Image:Breast Carcinoma Papillary Intracystic SolidVariant MP2 CTR.jpg|Breast - Papillary Intracystic Carcinoma, Solid Variant - medium power (SKB) | |||
Image:Breast Carcinoma Papillary Intracystic SolidVariant MP CTR.jpg|Breast - Papillary Intracystic Carcinoma, Solid Variant - medium power (SKB) | |||
Image:Breast Carcinoma Papillary Intracystic SolidVariant HP2 CTR.jpg|Breast - Papillary Intracystic Carcinoma, Solid Variant - high power (SKB) | |||
Image:Breast Carcinoma Papillary Intracystic SolidVariant HP CTR.jpg|Breast - Papillary Intracystic Carcinoma, Solid Variant - high power (SKB) | |||
Image:Breast EncystedPapillaryCarcinoma InfiltratingDuctalCarcinoma PA.JPG|Breast - Intracystic papillary adenocarcinoma (top) with associated invasive ductal carcinoma (bottom) (SKB) | |||
</gallery> | |||
==IHC== | |||
*Calponin/p63/SMA/CK5-6. | |||
**Loss of myoepithelial cells within the tumour. | |||
**Loss of myoepithelial cells at the cyst wall. | |||
*ER - Homogeneous staining of the epithelial proliferation. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Diagnosis]] | |||
[[Category:Breast pathology]] | |||
Latest revision as of 05:18, 29 April 2015
| Intracystic papillary carcinoma of the breast | |
|---|---|
| Diagnosis in short | |
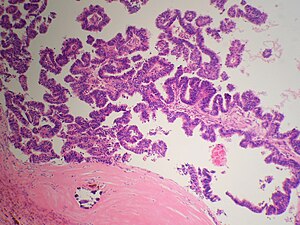 Intracystic Papillary Breast Carcinoma. H&E stain. | |
|
| |
| LM | Papillary lesion within a cyst |
| LM DDx | Intraductal papilloma, papillary DCIS, Invasive papillary breast carcinoma |
| Site | breast |
|
| |
| Signs | +/-bloody discharge from nipple |
| Prevalence | Rare |
| Prognosis | very good |
| Clin. DDx | other breast tumours |
| Treatment | surgical |
Intracystic papillary carcinoma of the breast, also known as encapsulated papillary carcinoma of the breast (abbreviated EPC), is an uncommon type of breast cancer with a very good prognosis.
It should not be confused with the invasive papillary carcinoma of the breast, a more aggressive tumour of the breast.
General
- Very good prognosis[1] - it is similar to DCIS.
- Classically menopausal women.
- ~30% present with bloody discharge.[2]
Microscopic
Features:
- Lesion confined to a cyst.
- May have a thick fibrous capsule
- The involved space is not lined by myoepithelial cells.
- The cyst contains an abnormal epithelial proliferation with cribriform, solid or papillary architecture.
- Loss of myoepithelial cells within the epithelial proliferation is a key feature.
- Scattered large cells with pale eosinophilic cytoplasm may be observed[3].
- These cells are so-called globoid cells or clear cells and are immunoreactive for GCDFP-15.
- They should not be mistaken for myoepithelial cells.
- Neoplastic epithelial cells:
- Nuclear atypia - including: nucleoli, nuclear pleomorphism.
Notes:
- Many potential pitfalls with papillary breast lesions on needle core biopsy.
- Complete excision is recommended.[4]
- Adequately and carefully sample the specimen to exclude an invasive component.
- Report only the size of the invasive component (if present) to prevent over-estimation of tumor stage.
- Intraductal papilloma.
- Absent or scant stroma favors papillary carcinoma over papilloma.
- Is there a single cell or dual cell population in the lesion?
- ER staining will be heterologous in a benign lesion.
- Myoepithelial markers (calponin/p63/SMA +ve)s hould be positive in a benign lesion.
- Papillary ductal carcinoma in situ.
- Papillary DCIS shows myoepithelial cells (calponin/p63/SMA +ve) at the periphery of the involved spaces
- But papillary DCIS should be negative for myoepithelial cells within the focus of DCIS
- Papillary intracystic carcinoma does not show myoepithelial cells at the periphery of the involved spaces
- Invasive papillary carcinoma of the breast.
- Similar architecture but no cystic space, frankly invasive.
- Very rare.
- Invasive carcinoma arising in association with papillary intracystic carcinoma
- Epithelial entrapment in the encysting fibrous tissue should not be interpreted as invasion.
- Carcinoma must be seen in the breast tissue outside the encysting fibrous tissue.
- Infiltrating carcinoma is usually of the 'no special type' variety.
- Adenoid cystic carcinoma of the breast
- The solid variant looks basaloid - solid adenoid cystic carcinoma or a 'basal-like' carcinoma should be considered in these cases.
Images
IHC
- Calponin/p63/SMA/CK5-6.
- Loss of myoepithelial cells within the tumour.
- Loss of myoepithelial cells at the cyst wall.
- ER - Homogeneous staining of the epithelial proliferation.
References
- ↑ Rakha, EA.; Gandhi, N.; Climent, F.; van Deurzen, CH.; Haider, SA.; Dunk, L.; Lee, AH.; Macmillan, D. et al. (Aug 2011). "Encapsulated papillary carcinoma of the breast: an invasive tumor with excellent prognosis.". Am J Surg Pathol 35 (8): 1093-103. doi:10.1097/PAS.0b013e31821b3f65. PMID 21753694.
- ↑ Rodríguez, MC.; Secades, AL.; Angulo, JM. (Nov 2010). "Best cases from the AFIP: intracystic papillary carcinoma of the breast.". Radiographics 30 (7): 2021-7. doi:10.1148/rg.307105003. PMID 21057133.
- ↑ Collins, LC.; Schnitt, SJ. (Jan 2008). "Papillary lesions of the breast: selected diagnostic and management issues.". Histopathology 52 (1): 20-9. doi:10.1111/j.1365-2559.2007.02898.x. PMID 18171414.
- ↑ Rizzo, M.; Linebarger, J.; Lowe, MC.; Pan, L.; Gabram, SG.; Vasquez, L.; Cohen, MA.; Mosunjac, M. (Mar 2012). "Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up.". J Am Coll Surg 214 (3): 280-7. doi:10.1016/j.jamcollsurg.2011.12.005. PMID 22244207.
- ↑ Collins, LC.; Schnitt, SJ. (Jan 2008). "Papillary lesions of the breast: selected diagnostic and management issues.". Histopathology 52 (1): 20-9. doi:10.1111/j.1365-2559.2007.02898.x. PMID 18171414.
- ↑ Pathmanathan, N.; Albertini, AF.; Provan, PJ.; Milliken, JS.; Salisbury, EL.; Bilous, AM.; Byth, K.; Balleine, RL. (Jul 2010). "Diagnostic evaluation of papillary lesions of the breast on core biopsy.". Mod Pathol 23 (7): 1021-8. doi:10.1038/modpathol.2010.81. PMID 20473278.