Difference between revisions of "Gallbladder"
(+images) |
|||
| Line 16: | Line 16: | ||
*'''No''' muscularis mucosae. | *'''No''' muscularis mucosae. | ||
*Small amount of lymphocytes in the lamina propria. | *Small amount of lymphocytes in the lamina propria. | ||
Note: | Note: | ||
*As there is no ''muscularis mucosae'', the [[cancer staging]] is different; pT1a is lamina propria invasion. pT1b is muscle layer invasion. | *As there is no ''muscularis mucosae'', the [[cancer staging]] is different; pT1a is lamina propria invasion. pT1b is muscle layer invasion. | ||
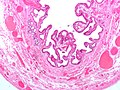
===Image=== | |||
<gallery> | |||
Image:Gallbladder_-_intermed_mag.jpg | Normal gallbladder - intermed. mag. (WC/Nephron) | |||
</gallery> | |||
=Overview= | =Overview= | ||
| Line 171: | Line 172: | ||
**The colour (yellow) is not strawberry-like. | **The colour (yellow) is not strawberry-like. | ||
Image | ====Image==== | ||
<gallery> | |||
Image:Cholesterolosis_of_the_Gallbladder.jpg | Gallbladder cholesterolosis. (WC/euthman) | |||
</gallery> | |||
===Microscopic=== | ===Microscopic=== | ||
Features: | Features: | ||
*Numerous foamy macrophages in the lamina propria. | *Numerous foamy macrophages in the lamina propria. | ||
Image | ====Image==== | ||
<gallery> | |||
Image:Gallbladder_cholesterolosis_intermed_mag_cropped.jpg | Cholesterolosis - intermed. mag. (WC) | |||
Image:Gallbladder_cholesterolosis_micro.jpg | Cholesterolosis. (WC) | |||
</gallery> | |||
===Sign out=== | ===Sign out=== | ||
<pre> | <pre> | ||
| Line 226: | Line 229: | ||
*Sometimes shinny. | *Sometimes shinny. | ||
Image | =====Image===== | ||
<gallery> | |||
Image:Gallensteine_2006_03_28.JPG | Yellow gallstones. (WC) | |||
</gallery> | |||
====Pigment stones==== | ====Pigment stones==== | ||
*Due to high [[RBC]] turnover, e.g. [[sickle cell disease]], thalassemia. | *Due to high [[RBC]] turnover, e.g. [[sickle cell disease]], thalassemia. | ||
Revision as of 03:06, 24 May 2013
The gallbladder, in pathology (and general surgery), is a growth industry... due to the worsening obesity epidemic.
Normal
Anatomy
- Body.
- Fundus.
- Neck.
Variations:
- Hartmann's pouch - invagination of the gallbladder wall at the origin of the cystic duct.
Image:
Histology
- No muscularis mucosae.
- Small amount of lymphocytes in the lamina propria.
Note:
- As there is no muscularis mucosae, the cancer staging is different; pT1a is lamina propria invasion. pT1b is muscle layer invasion.
Image
Overview
Most common:
- Cholelithiasis with cholecystitis.
Common:
- Antral-type metaplasia.
Uncommon:
- Intestinal metaplasia.
- Gallbladder dysplasia.
- Gallbladder carcinoma.
Common
Chronic cholecystitis
- Abbreviated CC.
General
Epidemiology
- Female, fat, fertile, family history, forty (though now getting younger... as people get fatter).
Etiology
- Cholelithiasis.
- Thick bile (acalculous cholecystitis).
Clinical (classic)
- Constant right upper quadrant pain after a fatty meal.
- Positive Murphy's sign (physical exam, with ultrasound).
Gross
- +/-Cholelithiasis - strongly associated pathology.
- +/-Strawberry-like appearance - common (due to gallbladder cholesterolosis).
- Small ridges (microvillus architecture) + yellow.
- Normal gallbladder mucosa = smooth, green.
- Small ridges (microvillus architecture) + yellow.
- +/-Congestion/erythema.
- +/-Wall thickening - typically ~ 6-7 mm.[2]
Note:
- Wall thickening (due to congestion/edema) is the important gross finding in acute cholecystitis.
- Wall thickenss greater than 10 mm should raise the suspicion of malignancy.[2]
Microscopic
Features:[3]
- Thickening of the gallbladder wall - due to fibrosis/muscular hypertrophy - key feature.
- Chronic inflammatory cells - usu. "minimal".
- Lymphocytes - most common.
- Rokitansky-Aschoff sinuses - common.[4]
- Entrapped epithelial crypts -- pockets of epithelium in the wall of the gallbladder.
- +/-Foamy macrophages in the lamina propria (cholesterolosis of the gallbladder).
DDx:
- Gallbladder adenocarcinoma.
- Gallbladder adenomyoma.
- Acute cholecystitis - more inflammation, lack Rokitansky-Aschoff sinuses, +/-mucosal erosions.
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS. - CHOLELITHIASIS.
Liver present
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS. - CHOLELITHIASIS. - SMALL AMOUNT OF LIVER WITHOUT APPARENT PATHOLOGY.
Micro
The sections show gallbladder wall with hemorrhage, and activated fibroblasts. The superficial mucosa has clusters of neutrophils.
Acute cholecystitis
General
- Less common than chronic cholecystitis.
- Usually due to gallstones.[5]
- Classically older individuals (50s and 60s) with a slight female predominance.[5]
Notes:
- Pathologic diagnosis very often discordant with clinical impression.[6]
Gross
Features:[5]
- Wall thickening - due to edema and hemorrhage.†
- Gallstone(s) - classically obstructing the gallbladder neck.
Note:
Microscopic
Features:[5]
- Edema.
- Hemorrhage.
- +/-Fibrin thrombi in small veins.
- +/-Mucosal erosions.
- +/-Neutrophils - useful
- +/-Reactive epithelial changes.[3]
Notes:
- May see activated fibroblasts.
DDx:
- Chronic cholecystitis - has less inflammation, fibrotic wall thickening/muscular hypertrophy, may have RK sinuses.
- Gallbladder adenocarcinoma.
Special types
Gangrenous cholecystitis
General:[9]
- Older.
- Clinically "sicker".
- Worse outcome than (acute) non-gangrenous cholecystitis.
Microscopic:
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - ACUTE CHOLECYSTITIS. - CHOLELITHIASIS.
GALLBLADDER, CHOLECYSTECTOMY: - ACUTE AND CHRONIC CHOLECYSTITIS WITH MULTIPLE MUCOSAL EROSIONS AND FOCAL NECROSIS OF THE GALLBLADDER WALL.
GALLBLADDER, CHOLECYSTECTOMY: - GANGRENOUS CHOLECYSTITIS. - CHOLELITHIASIS.
Gallbladder cholesterolosis
- AKA cholesterolosis.
- Informally known as strawberry gallbladder.
General
- Common in cholecystitis.
- Associated with yellow gallstones (cholesterol type gallstones).
Gross
Features:
- Mucosa has strawberry-like appearance.
- The similarity is in the surface texture.
- The colour (yellow) is not strawberry-like.
Image
Microscopic
Features:
- Numerous foamy macrophages in the lamina propria.
Image
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH CHOLESTEROLOSIS. - CHOLELITHIASIS.
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH FOCAL FOAMY MACROPHAGES IN LAMINA PROPRIA. - CHOLELITHIASIS.
Cholelithiasis
- AKA gallstones.
General
- Often accompanies cholecystitis/contributes and/or causes cholecystitis.
- Removed following biliary pancreatitis (gallstone pancreatitis) to reduce recurrence risk.[11][12]
The two types of gallstones:
- Cholesterol stones.
- Pigment stones.
Note:
- Most stones technically speaking are a mix, i.e. cholesterol and pigment. Many call yellow stones that are a mix "cholesterol stones".
Epidemiology
Classic risk factors for gallstones - 4 Fs:[13]
- Female.
- Fat.
- Forty.
- Fertile.
Additional:
- Family history.
Cholesterol stones
- More common than pigment stone.
Appearance:
- Clear or yellow.
- Opaque or translucent.
- Sometimes shinny.
Image
Pigment stones
- Due to high RBC turnover, e.g. sickle cell disease, thalassemia.
- Radio-opaque.[14]
Appearance:
- Black - key feature.
- Dull.
Sign out
GALLBLADDER CHOLECYSTECTOMY: - CHOLELITHIASIS. - MILD CHRONIC CHOLECYSTITIS.
Less common pathologic diagnoses
Adenomyoma of the gallbladder
General
- Glands in muscle.
- Analogous to what happens in the uterus.
- Significance - may mimic malignant tumours of the gallbladder.[15][16]
- Uncommon.
Gross
- Cystic spaces (Rokitansky-Aschoff sinuses) - may be seen on imaging.[17][18]
- Gallbladder wall thickening.
Microscopic
Features:[3]
- Glands in muscularis propria of the gallbladder wall - key feature.
- Significant muscular hypertrophy - key feature.
- No nuclear atypia.
DDx:
- Gallbladder carcinoma.
- Chronic cholecystitis - has less muscular hypertrophy; overlaps with this diagnosis.[3]
Image:
Gallbladder polyps
General
- Polyps are significant as they may be adenomatous, i.e. pre-cancerous.
- These are similar to polyps found elsewhere GI tract.
Microscopic
- See intestinal polyps.
Flat dysplasia:[19]
- Nuclear changes.
- Increased NC ratio.
- Hyperchromasia (essential).
- +/-Intestinal metaplasia --> goblet cells.
Gallbladder diverticulosis
General
- Uncommon.
- Thought to arise in the context of an outflow obstruction.[20]
Microscopic
Features:
- Mucosal pouch penetrating the muscularis propria of the gallbladder wall - key feature.
DDx:
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - CHRONIC CHOLECYSTITIS WITH DIVERTICULOSIS. - CHOLELITHIASIS.
Premalignant lesions
General
- Metaplasia associated with carcinoma.[21]
Hypothesis:[22]
- Antral type metaplasia --> intestinal metaplasia --> dysplasia --> carcinoma.
Intestinal metaplasia of the gallbladder
- AKA gallbladder intestinal metaplasia.
General
Significance:
- Increased risk of carcinoma.[21]
Microscopic
Features:[23]
- Goblet cells - key feature.
- +/-Paneth cells.[24]
Note:
- Often accompanied by antral type metplasia.
- Gastric antral-type epithelium - may form glands.
DDx:
Image:
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - INTESTINAL METAPLASIA OF THE GALLBLADDER, FOCAL. - CHRONIC CHOLECYSTITIS. - CHOLELITHIASIS. - NEGATIVE FOR DYSPLASIA.
Antral type metaplasia
General
Microscopic
Features:[24]
- Columnar cells with:
- Abundant, pale, apical mucin.
- Small basal nucleus.
- Cells often in nests -- below luminal surface.
- Cells vaguely resemble foveollar epithelium of the stomach.
Notes:
- May look similar to cells of the gallbladder neck[24] and common bile duct.[25]
- These glandular cells are not as columnar and have less well-defined cell borders.
- Cells with antral type metaplasia >2:1 (height:width), benign mucosal glands <2:1.
- These glandular cells are not as columnar and have less well-defined cell borders.
Images:
Gallbladder adenoma
- Gallbladder dysplasia redirects here.
General
- Premalignant lesion.
- May be associated with familial adenomatous polyposis or Peutz-Jeghers syndrome.[26]
Microscopic
Features:
- Gallbladder epithelium with:
- Nuclear atypia - key feature.
- Nuclear hyperchromasia.
- Nuclear crowding (pseudostratification) or round enlarged nuclei.
- +/-Goblet cells.
- Nuclear atypia - key feature.
Architectural subclassification:[27]
- Papillary ~ 45%.
- Tubulopapillary ~ 30%.
- Tubular ~ 25%.
Notes:
- All of the gallbladder should be submitted prior to sign out to exclude non-sampled adenocarcinoma.
DDx:
- Gallbladder adenocarcinoma.
- Reactive changes.
Image:
Sign out
GALLBLADDER, CHOLECYSTECTOMY: - BILIARY TYPE TUBULAR ADENOMA WITH HIGH GRADE DYSPLASIA. - MARGINS CLEAR OF ADENOMA (NEAREST MARGIN 1.0 CM).
Malignant
Gallbladder carcinoma
- AKA gallbladder adenocarcinoma.
General
- Uncommon.
Treatment:
- Cholecystectomy +/- lymph nodes +/- partial hepatectomy.[28]
Epidemiology
- Associated with gallstones.
- Increased risk in primary sclerosing cholangitis.
- Sex: female > male.
- Location: usually fundus, sometimes body.
Notes:
- Diffuse calcification of gallbladder wall, AKA "porcelain gallbladder" is not associated with carcinoma - based on a series of 10,741 cholecystectomies.[29]
- Focal mucosal calcification is associated with malignancy.[30]
- Cholangiocarcinoma is dealt with in the liver neoplasms article.
Gross
- Classic: mass projecting into the lumen.
- Marked gallbladder wall thickening.
- >10 mm should be considered with suspicion.[2]
Image:
Microscopic
Features:
- Usually adenocarcinoma.
- Mimics appearance of pancreatic ductal adenocarcinoma -- but less cellular mucin.[8]
Notes:
- May be very subtle, i.e. difficult to differentiate from normal glands.
DDx:
See also
References
- ↑ URL: http://web.uni-plovdiv.bg/stu1104541018/docs/res/skandalakis'%20surgical%20anatomy%20-%202004/Chapter%2020_%20Extrahepatic%20Biliary%20Tract%20and%20Gallbladder.htm. Accessed on: 13 December 2012.
- ↑ 2.0 2.1 2.2 2.3 Kim, HJ.; Park, JH.; Park, DI.; Cho, YK.; Sohn, CI.; Jeon, WK.; Kim, BI.; Choi, SH. (Feb 2012). "Clinical usefulness of endoscopic ultrasonography in the differential diagnosis of gallbladder wall thickening.". Dig Dis Sci 57 (2): 508-15. doi:10.1007/s10620-011-1870-0. PMID 21879282.
- ↑ 3.0 3.1 3.2 3.3 Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 439. ISBN 978-0443066573.
- ↑ URL: http://www.whonamedit.com/synd.cfm/983.html. Accessed on: 29 October 2011.
- ↑ 5.0 5.1 5.2 5.3 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Reuter, Victor E; Stoler, Mark H (2009). Sternberg's Diagnostic Surgical Pathology (5th ed.). Lippincott Williams & Wilkins. pp. 1606. ISBN 978-0781779425.
Cite error: Invalid
<ref>tag; name "Ref_Sternberg5_1606" defined multiple times with different content Cite error: Invalid<ref>tag; name "Ref_Sternberg5_1606" defined multiple times with different content Cite error: Invalid<ref>tag; name "Ref_Sternberg5_1606" defined multiple times with different content - ↑ Fitzgibbons, RJ.; Tseng, A.; Wang, H.; Ryberg, A.; Nguyen, N.; Sims, KL. (Dec 1996). "Acute cholecystitis. Does the clinical diagnosis correlate with the pathological diagnosis?". Surg Endosc 10 (12): 1180-4. PMID 8939838.
- ↑ Tsung, JW.; Raio, CC.; Ramirez-Schrempp, D.; Blaivas, M. (Mar 2010). "Point-of-care ultrasound diagnosis of pediatric cholecystitis in the ED.". Am J Emerg Med 28 (3): 338-42. doi:10.1016/j.ajem.2008.12.003. PMID 20223393.
- ↑ 8.0 8.1 Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 174. ISBN 978-0470519035.
- ↑ Nikfarjam, M.; Niumsawatt, V.; Sethu, A.; Fink, MA.; Muralidharan, V.; Starkey, G.; Jones, RM.; Christophi, C. (Aug 2011). "Outcomes of contemporary management of gangrenous and non-gangrenous acute cholecystitis.". HPB (Oxford) 13 (8): 551-8. doi:10.1111/j.1477-2574.2011.00327.x. PMID 21762298.
- ↑ STC. 25 February 2009.
- ↑ Bouwense, SA.; Besselink, MG.; van Brunschot, S.; Bakker, OJ.; van Santvoort, HC.; Schepers, NJ.; Boermeester, MA.; Bollen, TL. et al. (2012). "Pancreatitis of biliary origin, optimal timing of cholecystectomy (PONCHO trial): study protocol for a randomized controlled trial.". Trials 13: 225. doi:10.1186/1745-6215-13-225. PMID 23181667.
- ↑ van Baal, MC.; Besselink, MG.; Bakker, OJ.; van Santvoort, HC.; Schaapherder, AF.; Nieuwenhuijs, VB.; Gooszen, HG.; van Ramshorst, B. et al. (May 2012). "Timing of cholecystectomy after mild biliary pancreatitis: a systematic review.". Ann Surg 255 (5): 860-6. doi:10.1097/SLA.0b013e3182507646. PMID 22470079.
- ↑ Szwed, Z.; Zyciński, P. (2007). "[4F's--still up to date risk factors of cholelithiasis].". Wiad Lek 60 (11-12): 570-3. PMID 18540184.
- ↑ URL: http://www.rxmed.com/b.main/b2.pharmaceutical/b2.1.monographs/CPS-%20Monographs/CPS-%20%28General%20Monographs-%20U%29/URSOFALK.html. Accessed on: 29 October 2011.
- ↑ Saul, WM.; Herrmann, PK. (1988). "[Adenomyoma of the gallbladder].". Dtsch Z Verdau Stoffwechselkr 48 (2): 112-6. PMID 3168899.
- ↑ Sasatomi, E.; Miyazaki, K.; Mori, M.; Satoh, T.; Nakano, S.; Tokunaga, O. (Oct 1997). "Polypoid adenomyoma of the gallbladder.". J Gastroenterol 32 (5): 704-7. PMID 9350002.
- ↑ Ching, BH.; Yeh, BM.; Westphalen, AC.; Joe, BN.; Qayyum, A.; Coakley, FV. (Jul 2007). "CT differentiation of adenomyomatosis and gallbladder cancer.". AJR Am J Roentgenol 189 (1): 62-6. doi:10.2214/AJR.06.0866. PMID 17579153.
- ↑ 18.0 18.1 Boscak, AR.; Al-Hawary, M.; Ramsburgh, SR.. "Best cases from the AFIP: Adenomyomatosis of the gallbladder.". Radiographics 26 (3): 941-6. doi:10.1148/rg.263055180. PMID 16702464.
- ↑ Tadrous, Paul.J. Diagnostic Criteria Handbook in Histopathology: A Surgical Pathology Vade Mecum (1st ed.). Wiley. pp. 172. ISBN 978-0470519035.
- ↑ Beilby, JO. (Aug 1967). "Diverticulosis of the gall bladder. The fundal adenoma.". Br J Exp Pathol 48 (4): 455-61. PMC 2093791. PMID 4963758. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2093791/.
- ↑ 21.0 21.1 Duarte I, Llanos O, Domke H, Harz C, Valdivieso V (September 1993). "Metaplasia and precursor lesions of gallbladder carcinoma. Frequency, distribution, and probability of detection in routine histologic samples". Cancer 72 (6): 1878–84. PMID 8364865.
- ↑ 22.0 22.1 22.2 Mukhopadhyay S, Landas SK (March 2005). "Putative precursors of gallbladder dysplasia: a review of 400 routinely resected specimens". Arch. Pathol. Lab. Med. 129 (3): 386–90. PMID 15737036. http://www.archivesofpathology.org/doi/pdf/10.1043/1543-2165%282005%29129%3C386%3APPOGDA%3E2.0.CO%3B2.
- ↑ Albores-Saavedra, J.; Nadji, M.; Henson, DE.; Ziegels-Weissman, J.; Mones, JM. (Jun 1986). "Intestinal metaplasia of the gallbladder: a morphologic and immunocytochemical study.". Hum Pathol 17 (6): 614-20. PMID 2872152.
- ↑ 24.0 24.1 24.2 24.3 Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 1789. ISBN 978-0781740517.
- ↑ Cutz, E. 3 March 2011.
- ↑ 26.0 26.1 Levy, AD.; Murakata, LA.; Abbott, RM.; Rohrmann, CA.. "From the archives of the AFIP. Benign tumors and tumorlike lesions of the gallbladder and extrahepatic bile ducts: radiologic-pathologic correlation. Armed Forces Institute of Pathology.". Radiographics 22 (2): 387-413. PMID 11896229. http://radiographics.rsna.org/content/22/2/387.full.
- ↑ Adsay, V.; Jang, KT.; Roa, JC.; Dursun, N.; Ohike, N.; Bagci, P.; Basturk, O.; Bandyopadhyay, S. et al. (Sep 2012). "Intracholecystic papillary-tubular neoplasms (ICPN) of the gallbladder (neoplastic polyps, adenomas, and papillary neoplasms that are ≥1.0 cm): clinicopathologic and immunohistochemical analysis of 123 cases.". Am J Surg Pathol 36 (9): 1279-301. doi:10.1097/PAS.0b013e318262787c. PMID 22895264.
- ↑ Biswas, PK. (Jul 2010). "Carcinoma gallbladder.". Mymensingh Med J 19 (3): 477-81. PMID 20639849.
- ↑ Towfigh S, McFadden DW, Cortina GR, et al (January 2001). "Porcelain gallbladder is not associated with gallbladder carcinoma". Am Surg 67 (1): 7?0. PMID 11206901.
- ↑ Stephen, AE.; Berger, DL. (Jun 2001). "Carcinoma in the porcelain gallbladder: a relationship revisited.". Surgery 129 (6): 699-703. doi:10.1067/msy.2001.113888. PMID 11391368.