Difference between revisions of "Cholangiocarcinoma"
Jump to navigation
Jump to search
| Line 9: | Line 9: | ||
| LMDDx = [[metastatic carcinoma]] - esp. luminal GI tract, [[hepatocellular carcinoma]] | | LMDDx = [[metastatic carcinoma]] - esp. luminal GI tract, [[hepatocellular carcinoma]] | ||
| Stains = | | Stains = | ||
| IHC = CK7 +ve, [[CK20]] +ve/-ve, [[CK19]] +ve, HepPar-1 -ve, AFP -ve | | IHC = CK7 +ve, [[CK20]] +ve/-ve, [[CK19]] +ve, HepPar-1 -ve, AFP -ve, EMA +ve | ||
| EM = | | EM = | ||
| Molecular = | | Molecular = | ||
| Line 96: | Line 96: | ||
ICC vs. HCC:<ref name=pmid19173916>[Evaluation of immunohistochemical markers for differential diagnosis of hepatocellular carcinoma from intrahepatic cholangiocarcinoma] Dong H, Cong WL, Zhu ZZ, Wang B, Xian ZH, Yu H. Zhonghua Zhong Liu Za Zhi. 2008 Sep;30(9):702-5. Chinese. PMID 19173916.</ref> | ICC vs. HCC:<ref name=pmid19173916>[Evaluation of immunohistochemical markers for differential diagnosis of hepatocellular carcinoma from intrahepatic cholangiocarcinoma] Dong H, Cong WL, Zhu ZZ, Wang B, Xian ZH, Yu H. Zhonghua Zhong Liu Za Zhi. 2008 Sep;30(9):702-5. Chinese. PMID 19173916.</ref> | ||
*ICC: [[CK19]] (92.5%), MUC-1 (73.8%) +ve. | *ICC: [[CK19]] (92.5%), [[MUC-1]] (73.8%) +ve. | ||
*HCC: HepPar-1 (85.6%), CD34 (87.8%) +ve. | *HCC: HepPar-1 (85.6%), CD34 (87.8%) +ve. | ||
HCC vs. ICC:<ref name=pmid16627262>{{cite journal |author=Lei JY, Bourne PA, diSant'Agnese PA, Huang J |title=Cytoplasmic staining of TTF-1 in the differential diagnosis of hepatocellular carcinoma vs cholangiocarcinoma and metastatic carcinoma of the liver |journal=Am. J. Clin. Pathol. |volume=125 |issue=4 |pages=519–25 |year=2006 |month=April |pmid=16627262 |doi=10.1309/59TN-EFAL-UL5W-J94M |url=}}</ref> | HCC vs. ICC:<ref name=pmid16627262>{{cite journal |author=Lei JY, Bourne PA, diSant'Agnese PA, Huang J |title=Cytoplasmic staining of TTF-1 in the differential diagnosis of hepatocellular carcinoma vs cholangiocarcinoma and metastatic carcinoma of the liver |journal=Am. J. Clin. Pathol. |volume=125 |issue=4 |pages=519–25 |year=2006 |month=April |pmid=16627262 |doi=10.1309/59TN-EFAL-UL5W-J94M |url=}}</ref> | ||
*TTF-1: ~90-100% +ve (cytoplasmic) in HCC vs. ~10% in cholangiocarcinoma. | *TTF-1: ~90-100% +ve (cytoplasmic) in HCC vs. ~10% in cholangiocarcinoma. | ||
Note: | |||
*'''MUC-1''' is also known as ''[[EMA]]''. | |||
==Sign out== | ==Sign out== | ||
Revision as of 20:44, 18 September 2015
| Cholangiocarcinoma | |
|---|---|
| Diagnosis in short | |
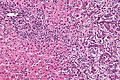
 Cholangiocarcinoma. H&E stain. | |
|
| |
| Synonyms | bile duct carcinoma |
|
| |
| LM | atypical cuboidal or columnar mucin producing cohesive cells (carcinoma) - usually gland forming (adenocarcinoma), classically with a dense fibrous (desmoplastic) stroma |
| LM DDx | metastatic carcinoma - esp. luminal GI tract, hepatocellular carcinoma |
| IHC | CK7 +ve, CK20 +ve/-ve, CK19 +ve, HepPar-1 -ve, AFP -ve, EMA +ve |
| Site | bile ducts (including pancreas, liver - see liver neoplasms) |
|
| |
| Associated Dx | liver flukes (Clonorchis sinensis, Opisthorchis viverrini), Caroli disease, primary sclerosing cholangitis - esp. in ulcerative colitis |
| Signs | +/-jaundice |
| Prevalence | uncommon |
| Blood work | +/-findings of cholestasis |
| Prognosis | poor |
| Clin. DDx | other liver tumours - hepatocellular carcinoma, metastases |
| Treatment | surgical resection if possible |
Cholangiocarcinoma is a malignant tumour that arise from the bile ducts and may been seen in the liver.
It is also known as bile duct carcinoma.[1]
General
- Malignancy of the biliary tree.
- May be intrahepatic, i.e. intrahepatic cholangiocarcinoma (abbreviated ICC), or extrahepatic.
Epidemiology
- Rare - approximately 1/5 the incidence of HCC.[2]
- More common among asians.
Risks:
- Infection - liver flukes (endemic to Southeast Asia):
- Caroli disease - rare congenital disease.[6]
- Primary sclerosing cholangitis - may be assoc. with inflammatory bowel disease (IBD), esp. ulcerative colitis (UC).
Gross
- Classically one large mass - outline described as cauliflower-like.[7]
- May have satellite nodules.
Image
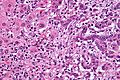
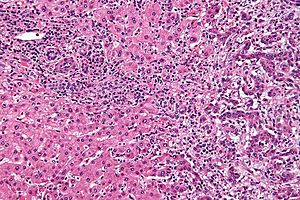
Microscopic
Features:[8]
- Usually an adenocarcinoma, i.e. gland forming with:
- Cuboidal or columnar mucin producing cells, and
- A dense fibrous (desmoplastic) stroma.
Notes:
- Biliary stents lead to reactive changes,[9] these can be confused for malignancy. One must always check whether a biliary stent was in situ at time of biopsy.[10]
- Usually abundant desmoplasia, ergo hard to get good, i.e. diagnositic, endoluminal brushing specimens.[11]
- May have hyaline inclusions.[12]
DDx:
- Metastatic adenocarcinoma.
- Fulminant hepatic necrosis.
- Bile ducts usu. left behind... look like well-differentiated adenocarcinoma.
- Bile duct adenoma.
- No necrosis, no mitotic activity, no significant nuclear pleomorphism.
Images
Cholangiocarcinoma - low mag. Shows the typical desmoplastic stroma. (WC/Nephron)
www:
- Cholangiocarcinoma & liver flukes - several images (upmc.edu).
- Cholangiocarcinoma - several images (upmc.edu).
IHC
Classic IHC pattern:[13]
- CK7 +ve.
- CK20 +ve/-ve.
- HepPar-1 -ve.
- AFP -ve.[11]
ICC vs. HCC:[14]
HCC vs. ICC:[15]
- TTF-1: ~90-100% +ve (cytoplasmic) in HCC vs. ~10% in cholangiocarcinoma.
Note:
- MUC-1 is also known as EMA.
Sign out
MASS, PANCREAS, CORE BIOPSY: - ADENOCARCINOMA, MODERATELY DIFFERENTIATED.
Note:
- On biopsy, it isn't possible to cleanly separate from pancreatic adenocarcinoma. Thus, it is better to stay vague.
Micro
The sections show an atypical gland-forming lesion (adenocarcinoma) in a fibrous background. This lesion is separate from the benign pancreatic glands that are present. The atypical glands are unequally spaced. Moderate-to-marked cytologic atypia is present. Mitotic activity is not readily apparent.
See also
References
- ↑ URL: http://www.cancer.org/cancer/bileductcancer/detailedguide/bile-duct-cancer-what-is-bile-duct-cancer. Access on: 23 May 2013.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 608. ISBN 978-0443066573.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 926. ISBN 0-7216-0187-1.
- ↑ Park, do H.; Son, HY. (Apr 2008). "Images in clinical medicine. Clonorchis sinensis.". N Engl J Med 358 (16): e18. doi:10.1056/NEJMicm054461. PMID 18420495.
- ↑ de Martel C, Plummer M, Franceschi S (March 2010). "Cholangiocarcinoma: Descriptive epidemiology and risk factors". Gastroenterol Clin Biol. doi:10.1016/j.gcb.2010.01.008. PMID 20202771.
- ↑ Ananthakrishnan AN, Saeian K (April 2007). "Caroli's disease: identification and treatment strategy". Curr Gastroenterol Rep 9 (2): 151–5. PMID 17418061.
- ↑ Nakanishi, Y.; Zen, Y.; Kawakami, H.; Kubota, K.; Itoh, T.; Hirano, S.; Tanaka, E.; Nakanuma, Y. et al. (Jul 2008). "Extrahepatic bile duct carcinoma with extensive intraepithelial spread: a clinicopathological study of 21 cases.". Mod Pathol 21 (7): 807-16. doi:10.1038/modpathol.2008.65. PMID 18425077.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 609. ISBN 978-0443066573.
- ↑ Carrasco, CH; Wallace, S; Charnsangavej, C; Richli, W; Wright, KC; Fanning, T; Gianturco, C (Dec 1985). "Expandable biliary endoprosthesis: an experimental study.". AJR Am J Roentgenol 145 (6): 1279-81. PMID 3877438.
- ↑ STC. 2 October 2009.
- ↑ 11.0 11.1 STC. 6 December 2010.
- ↑ Aishima, S.; Fujita, N.; Mano, Y.; Iguchi, T.; Taketomi, A.; Maehara, Y.; Oda, Y.; Tsuneyoshi, M. (Sep 2010). "p62+ Hyaline inclusions in intrahepatic cholangiocarcinoma associated with viral hepatitis or alcoholic liver disease.". Am J Clin Pathol 134 (3): 457-65. doi:10.1309/AJCP53YVVJCNDZIR. PMID 20716803.
- ↑ Iacobuzio-Donahue, Christine A.; Montgomery, Elizabeth A. (2005). Gastrointestinal and Liver Pathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 609. ISBN 978-0443066573.
- ↑ [Evaluation of immunohistochemical markers for differential diagnosis of hepatocellular carcinoma from intrahepatic cholangiocarcinoma] Dong H, Cong WL, Zhu ZZ, Wang B, Xian ZH, Yu H. Zhonghua Zhong Liu Za Zhi. 2008 Sep;30(9):702-5. Chinese. PMID 19173916.
- ↑ Lei JY, Bourne PA, diSant'Agnese PA, Huang J (April 2006). "Cytoplasmic staining of TTF-1 in the differential diagnosis of hepatocellular carcinoma vs cholangiocarcinoma and metastatic carcinoma of the liver". Am. J. Clin. Pathol. 125 (4): 519–25. doi:10.1309/59TN-EFAL-UL5W-J94M. PMID 16627262.