Collagenous colitis
Collagenous colitis is a type of microscopic colitis. It has a characteristic clinical presentation and no apparent endoscopic changes.
General
Presentation:
- Chronic diarrhea, non-bloody.[1]
- Collagenous colitis may be related to lymphocytic colitis.
- It is hypothesized that these conditions may be the same pathology at different time points.[1]
Notes:
- Clinical DDx includes irritable bowel syndrome - which has no or subtle histopathologic changes.
Epidemiology
- Age: a disease of adults - usually 50s.
- Sex:
- Drugs are associated with LC and CC.
- NSAIDs - posulated association/weak association,
- SSRIs (used primarily for depression) - moderate association, dependent on specific drug.
- Associated with autoimmune disorders - celiac disease, diabetes mellitus, thyroid disorders and arthritis.[2]
- No increased risk of colorectal carcinoma.[2]
Treatment
- Sometimes just follow-up.
- Steroids - budesonide -- short-term treatment.[2]
Gross
- Endoscopic examination is normal.
- This is why it is called a microscopic colitis.
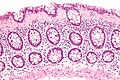
Microscopic
Features:
- Intraepithelial lymphocytes - important.
- Collagenous material in the lamina propria (pink on H&E) -- key feature.
- Can be demonstrated with a trichrome stain -- collagen = green on trichrome.
- Subepithelial collagen needs to be >= 10 micrometres thick for diagnosis.[2]
- Thickening is usually patchy.[4]
- Thickening "follows the crypts from the surface" - useful for differentiating from tangential sections of the basement membrane.[5]
- Collagen may envelope capillaries - useful to discern from basement membrane.[5]
Notes:
- CC is typically more prominent in the proximal colon - may reflect concentration gradient of offending causitive agents.[2]
- Significant negative findings:[6]
- No PMNs.
- No crypt distortion.
- Thickened collagen band uncommon in rectum.[4]
Images
Sign out
TRANSVERSE COLON, BIOPSY: - COLLAGENOUS COLITIS.
Micro
The sections show colonic mucosa with abundant intraepithelial lymphocytes (>20 lymphocytes/100 surface epithelial cells). A prominent collagen band is apparent below the epithelium (>10 micrometres thick). The glandular architecture is within normal limits.
There are no granulomas. No neutrophilic cryptitis is apparent. The epithelium matures appropriately to the surface.
See also
References
- ↑ 1.0 1.1 1.2 1.3 URL: http://emedicine.medscape.com/article/180664-overview. Accessed on: 31 May 2010.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Tysk C, Bohr J, Nyhlin N, Wickbom A, Eriksson S (December 2008). "Diagnosis and management of microscopic colitis". World J. Gastroenterol. 14 (48): 7280-8. PMID 19109861. http://www.wjgnet.com/1007-9327/14/7280.asp.
- ↑ Offner, FA.; Jao, RV.; Lewin, KJ.; Havelec, L.; Weinstein, WM. (Apr 1999). "Collagenous colitis: a study of the distribution of morphological abnormalities and their histological detection.". Hum Pathol 30 (4): 451-7. PMID 10208468.
- ↑ 4.0 4.1 Tanaka, M.; Mazzoleni, G.; Riddell, RH. (Jan 1992). "Distribution of collagenous colitis: utility of flexible sigmoidoscopy.". Gut 33 (1): 65-70. PMID 1740280.
- ↑ 5.0 5.1 Bell, D. 4 Mar 2009.
- ↑ http://hopkins-gi.nts.jhu.edu/pages/latin/templates/index.cfm?pg=disease1&disease=29&organ=6&lang_id=1