Thyroid cytopathology
Thyroid cytopathology is a large part of cytopathology.
This article deals only with thyroid cytopathology. An introduction to cytopathology is in the cytopathology article. Head and neck cytopathology is dealt with in the Head and neck cytopathology article.
Normal thyroid
Radiology
Benign features - terms:[1]
- Spongiform configuration.
- Colloid clot - cyst.
- Giraffe pattern.
- Diffuse hyperechogenicity.
Follicular cells
- Uniform spacing of cells.
- "Cracks" (spaces) between cell - "crazy paving".[2]
Note:
- It is interesting that uniform spacing in the context of thyroid is benign... in breast suggests DCIS.
Microfollicles
Definition:[3]
- <15 follicular cells forming at least two thirds of a circle.
- Usually flat, i.e. not three dimensional.
Note:
- A small number of microfollicles is considered normal.
Images
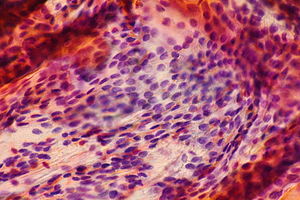
Colloid and endocrine atypia - high mag. (WC)
Colloid
Essentially - acellular crap with:
- Irregular/sharp borders.
- Cracks - key feature.
- Dark (uniform) staining with Romanowsky type stains.
- Green edge + red/orange centre with Pap stain.
- +/-Entraped red blood cells (RBCs).
Images
Hurthle cells
- May be spelled Hürthle cells.
Features:
- Large epithelioid cells with red granular material on Pap stain.
- Should not form 3-D balls.
Images
Normal parathyroid cytology
General
- May be confused with thyroid.
- No single feature can be use to reliably separate them, though several features may allow this.[4]
- FNAs are not useful for parathyroid lesions;[5] however, a parathyroid may be sampled inadvertently.
Cytology
Chief cells:[4]
- Small round-to-oval nucleus.
- Granular chromatin.
- Cytoplasm - often not distinct.
- Scattered naked nuclei.[6]
- +/-Nuclear moulding.
- +/-Nuclear overlap.
- +/-Papillary fragments - uncommon.[5]
Images:
DDx of naked nuclei:
- Granular cell tumour.
- Parathyroid.[5]
Adequacy criteria
- >=60 follicular cells. †
- No atypical cells.
Note 1:
- † Typically described as: at least 6 groups (with 10 or more follicular cells) on at least two smears.[8]
Note 2:
- The inadequate & suspicious rate with these criteria is 10-30%. In excision specimens, 75-80% are benign.[9]
- The above begs the question - should the criteria be changed?
Sign out
Thyroid Gland, Right Lobe, Fine Needle Aspiration: - Unsatisfactory; specimen processed and examined, but unsatisfactory due to insufficient material. Scant follicular cells, Hurthle cells and colloid present in a background of mixed inflammatory cells and abundant macrophages. Note: A repeat aspiration should be considered if clinically warranted.
Alternate
Thyroid Gland, Right Lobe, Fine Needle Aspiration: - Non-diagnostic. (Category I) Specimen processed and examined, but unsatisfactory due to scant cellularity. Some cellular degeneration noted, rare colloid and inflammatory cells present. Note: A repeat aspiration should be considered if clinically warranted.
Standard sign-out language
There is a standard way of describing thyroid cytopathology results.
Bethesda (2009)
This is formally known as the "The Bethesda System for Reporting Thyroid Cytopathology"; it is based on the NCI classification of 2008:[10]
| Preferred | Plain language | Risk of malignancy | Usual management |
|---|---|---|---|
| Benign | Benign | ~ 0-3% | Follow-up, clinical |
| Follicular lesion of undetermined significance (FLUS) or atypia of undetermined significance |
Uncertain, favour benign | 5-15% | Repeat FNA |
| Follicular neoplasm or suspicious for follicular neoplasm; if oncocytic type it should be noted |
Uncertain, favour malignant | 15-30% | Hemithyroidectomy |
| Suspicious for malignancy | Probably malignant | 60-75% | Repeat vs. hemithyroidectomy |
| Malignant | Cancer | ~ 97-99% | Excise (total thyroidectomy) |
| Nondiagnostic or unsatisfactory | Lesion missed or inadequate | 1-4% | Repeat FNA |
NCI (2008)
A National Cancer Institute (NCI) consensus conference in 2008:[11]
| Preferred (NIC) | Alternate (NIC) | Plain language | Risk of malignancy | Usual management |
|---|---|---|---|---|
| Benign | - | Benign | ~ 1% | Follow/nothing |
| Follicular lesion of undetermined significance (FLUS) | 1. Atypia of undetermined significance 2. Rule-out neoplasm 3. Atypical follicular lesion 4. Cellular follicular lesion |
Uncertain, favour benign | 5-10% | Repeat FNA in 3 months |
| Follicular neoplasm | Suspicious for follicular neoplasm | Uncertain, favour malignant | 20-30% | Hemithyroidectomy |
| Hurthle cell neoplasm | Suspicious for Hurthle cell neoplasm | Uncertain, favour malignant | 20-30% | Hemithyroidectomy |
| Suspicious for malignancy | - | Probably malignant | 50-75% | Repeat vs. hemithyroidectomy |
| Malignant | - | Cancer | ~ 99% | Excise |
| Nondiagnostic | - | Lesion missed or inadequate | Unknown | Repeat FNA in 3 months |
Benign disease
Adenomatoid nodule
General
- Diagnosis benign thyroid tissue.
Cytology
Features:
- Benign follicular cells (abundant) with relatively little colloid.
DDx:
- Colloid nodule - has more colloid.
Sign out
Thyroid Gland, Left, Fine Needle Aspiration: - Benign. - Cellular aspirate. - Benign-appearing follicular cells with colloid, consistent with an adenomatous nodule.
Colloid nodule
General
- Diagnosis benign thyroid tissue.
Cytology
Features:
- Colloid - paucicellular material:
- "Thick" colloid = dense appearing blob, well-circumscribed +/- "cracking".
- "Watery" colloid = light, whispy/fluffy material.
- Macrofollicles:
- Ball of cells ~ 20 cells across.
Images
Graves disease
General
- Clinical diagnosis - based on serology.
Cytology
Features:
- +/-Flame cells on Romanowsky stain, e.g. Diff-Quik.[12]
- Red granular discolourization of the cytoplasm - thought to be endoplasmic reticulum.
Notes:
- Flame cells are indicative of cellular hyperactivity.
- Not pathognomonic for Graves disease, e.g. may be seen in early Hashimoto disease,
Images:
Lymphocytic thyroiditis
General
- Non-specific finding.
- May represent Hashimoto thyroiditis.
- Can be seen in Graves' disease.[13]
Cytology
Features:
- Lymphocytes not typical of circulating blood:
- Centrocytes.
- Small lymphocytes with a cleft.
- Centroblasts.
- Large lymphocytes with nucleolus and eccentric nucleus.
- Plasma cells.
- Cells with a "clockface nucleus".
- Centrocytes.
- Small mature lymphocytes in fragments of follicular cells - raise the suspicion of lymphocytic thyroiditis.[14]
- Small mature lymphocytes are not a reliable indicator of inflammation, as cells may layer during tissue preparation.[15]
Notes:
- Usually #1 and #2 are seen.
Hashimoto thyroiditis
General
- This is a clinical diagnosis.
- It should be reported by the pathologist as "lymphocytic thyroiditis".
- AMA +ve.
- Antithyroid antibody +ve.
- Antimicrosomal (antithyroid peroxidase).
- Antithyroglobulin.
- Increased risk of B-cell lymphoma.
Cytology
Features:[2]
- Polymorphous lymphoplasmacytic infiltrate with germinal centres.
- Tingible body macrophages.
- Found in germinal centres; have condensed chromatin fragments.[17]
- Lymphoid tangles.
- Found in almost 100% of cases.[16]
- Lymphoglandular bodies.
- Cytoplasmic fragment of a lymphoid cell.[18]
Note:
- Lymphocyte infiltration into fragments of oncocytic cells - strongly suggestive of Hashimoto disease. (???)
Waffle category
Follicular lesion of undetermined significance
- Abbreviated FLUS.
- Also known as atypia of undetermined significance (abbreviated AUS).
General
- This is waffle diagnosis, i.e. something the pathologist diagnoses when they cannot decide whether it is benign or suspicious for malignant (follicular neoplasm or suspicious for malignancy).[19]
- Like all waffle diagnoses...
- Use should be minimized; < 7% is suggested, though it varies considerably between pathologists and institutions.[19]
- Like all waffle diagnoses...
Cytology
Features:
- Mild nuclear atypia - that by definition is insufficient for follicular neoplasm or suspicious for malignancy.
- Mild irregularities in the nuclear contour.
- Mild size variation or nuclear enlargement.
- Mild accentuation of nuclear staining.
Sign out
Atypia of undetermined significance (AUS).
Neoplastic and malignant
Papillary carcinoma
General
- Papillary thyroid carcinoma is basically the only entity (in cytopathology) that has near universally accepted criteria.
- This is why radiation oncologists say... "Basing stuff on pathology is like basing something on shifting sand."
Cytology
Criteria for papillary thyroid carcinoma:[20][21]
- Nuclear inclusion (really pseudoinclusions):[22]
- Edge of inclusion must be sharp (nuclear membrane-like).
- Size: at least 1/4 of the nucleus.
- Round, regular.
- Within epithelial cell.
- Additional criteria:[23] Inclusion center should match cytoplasm.
- Nucleoli (micro or macro).
- Nuclear grooves.
- No universal criteria; some believe grooves should go from edge-to-edge, i.e. across the nucleus.
- Nuclear enlargement.
- Changes in chromatin - patterns:
- Granular.
- Washed-out.
Additional features:
- Papillary architecture (not commonly seen).
- Clump of epithelial cells with attached fibrous tissue "tail" - that has a smooth edge.
- Cellular/nuclear membrane overlapping; cells do not respect one another (very common).
- +/-Psammoma bodies (uncommon - but helpful if seen).
Notes:
- Nuclear enlargement may be seen in Hashimoto's disease.[24]
- Nuclear grooves may be seen in Hashimoto's disease.[25]
- Papillary architecture may be seen in Graves disease.[26]
- Thick (dense) colloid common - described as "bubble gum". (???)
Images
Variants of PTC
- Tall cell variant.
- May mimic Hurthle cell neoplasm.
- Warthin-like variant.
- Superficially resembles Warthin tumour (presence of lymphocytes).
- Follicular variant of PTC; memory device ECT: Elongation, Clearing, Thick membranes.
- Nuclear elongation.
- Chromatin clearing.
- Thick nuclear membranes.
- Classic features of PTC (esp. pseudo-inclusions) are usually scarce in this variant.
Follicular neoplasm
General
- Can be thought of as a (neoplasm) garbage category for the thyroid gland - may represent:
Management:
- Hemithyroidectomy.
Cytology
Features:[11]
- Hypercellular lesion.
- 3-dimensional clusters of cells.
- Nuclear overlap/crowding.
- +/-Microfollicles, numerous.
- Microfollicles are defined as: <15 cells forming at least two thirds of a circle.
- +/-Atypia marked.
Diagnosis (follicular neoplasm) per MB:
- Either: 1-3 or 3-5.
Notes:
- A few microfollicles are normal.
- Atypia alone - "suspicious for malignancy" or "malignant".
- Nuclei are described as having the shape of an orange in follicular neoplasms... and potatoes in papillary thyroid carcinomas.
Oncocytic neoplasm
- AKA Hurthle cell neoplasm.
General
- Oncocytic perferred by WHO over Hurthle cell.
Cytology
Features:[11]
- Single cells or sheets of oncocytic cells.
- 3-D clusters.
- +/-Transgressing vessels - cluster of oncocytes surrounding vessels.
- Oncocytic cells:
- Well-defined cellular borders.
- Finely granular abundant cytoplasm.
- Nucleoli, may be prominent.
Notes:
- Benign (oncocytic) thyroid tissue may have:
- Significant nuclear pleomorphism.
- Multinucleation.
DDx:
Images
www:
Medullary thryoid carcinoma
General
- May be familial - associated with MEN II syndrome.
- Sometimes described as the melanoma of the thyroid - as it can look like almost anything.
Cytology
Features:[11]
- Single or loosely cohesive cells.
- Spindle cell morphology common.
- Abundant eosinophilc granular cytoplasm - key feature
- Salt and pepper chromatin - key feature; no nucleoli.
- Nucleus eccentric and round/oval - plasmacytoid appearance.
- Amyloid - acellular, amorphous material may be present; cotton candy-like.
- May be confused with fibrin...
- Fibrin = fluffy edge vs. amyloid = sharp border. (???)
- Fibrin - associated with PMNs/has PMNs within it.
- Amyloid cannot be definitively differentiated on morphologic grounds from colloid.
- Described by Halliday et al. as:[28]
- Romanowsky type staining: "amorphous, irregular, waxy basophilic to metachromatic clump".
- Pap staining: "cyanophilic-organophilic clumps of material + occasional prominent fissures".
- May be confused with fibrin...
Notes:
- May have pseudoinclusions - mimic papillary thyroid carcinoma.[29]
DDx:
Images:
IHC
- Calcitonin +ve - it arises from C cells (which produce calcitonin)
- CEA +ve (often better staining than calcitonin).[30]
- Congo-red +ve (if amyloid present) - mnemonic: CRAP -- congo red amyloid protein.
Anaplastic thyroid carcinoma
General
- Prognosis: very crappy.
- Classically rapid growth.
Note:
- Other fast growing lesion:
- Lymphoma (faster than anaplastic carcinoma).
- Blood accumulation.
Cytology
Features:
- Nuclear atypia - marked.
- Spindle cell morphology common.
- Nucleolus.
- Usually scant cellularity.[31]
- Necrosis very common.
DDx:
- Medullary thyroid carcinoma.
See also
References
- ↑ Bonavita, JA.; Mayo, J.; Babb, J.; Bennett, G.; Oweity, T.; Macari, M.; Yee, J. (Jul 2009). "Pattern recognition of benign nodules at ultrasound of the thyroid: which nodules can be left alone?". AJR Am J Roentgenol 193 (1): 207-13. doi:10.2214/AJR.08.1820. PMID 19542415.
- ↑ 2.0 2.1 2.2 Lefkowitch, Jay H. (2006). Anatomic Pathology Board Review (1st ed.). Saunders. pp. 672. ISBN 978-1416025887.
- ↑ Renshaw, AA.; Wang, E.; Wilbur, D.; Hughes, JH.; Haja, J.; Henry, MR. (Feb 2006). "Interobserver agreement on microfollicles in thyroid fine-needle aspirates.". Arch Pathol Lab Med 130 (2): 148-52. doi:10.1043/1543-2165(2006)130[148:IAOMIT]2.0.CO;2. PMID 16454552.
- ↑ 4.0 4.1 Absher, KJ.; Truong, LD.; Khurana, KK.; Ramzy, I. (Feb 2002). "Parathyroid cytology: avoiding diagnostic pitfalls.". Head Neck 24 (2): 157-64. PMID 11891946.
- ↑ 5.0 5.1 5.2 Agarwal, AM.; Bentz, JS.; Hungerford, R.; Abraham, D. (Jun 2009). "Parathyroid fine-needle aspiration cytology in the evaluation of parathyroid adenoma: cytologic findings from 53 patients.". Diagn Cytopathol 37 (6): 407-10. doi:10.1002/dc.21020. PMID 19283690.
- ↑ Heo, I.; Park, S.; Jung, CW.; Koh, JS.; Lee, SS.; Seol, H.; Choi, HS.; Cho, SY. (Oct 2013). "Fine needle aspiration cytology of parathyroid lesions.". Korean J Pathol 47 (5): 466-71. doi:10.4132/KoreanJPathol.2013.47.5.466. PMID 24255635.
- ↑ Johnson, SJ.; Sheffield, EA.; McNicol, AM. (Apr 2005). "Best practice no 183. Examination of parathyroid gland specimens.". J Clin Pathol 58 (4): 338-42. doi:10.1136/jcp.2002.002550. PMC 1770637. PMID 15790694. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770637/.
- ↑ Carpi, A.; Sagripanti, A.; Nicolini, A.; Santini, S.; Ferrari, E.; Romani, R.; Di Coscio, G. (1998). "Large needle aspiration biopsy for reducing the rate of inadequate cytology on fine needle aspiration specimens from palpable thyroid nodules.". Biomed Pharmacother 52 (7-8): 303-7. PMID 9809173.
- ↑ Haugen, BR.; Woodmansee, WW.; McDermott, MT. (Mar 2002). "Towards improving the utility of fine-needle aspiration biopsy for the diagnosis of thyroid tumours.". Clin Endocrinol (Oxf) 56 (3): 281-90. PMID 11940037.
- ↑ Cibas ES, Ali SZ (November 2009). "The Bethesda System for Reporting Thyroid Cytopathology". Thyroid 19 (11): 1159–65. doi:10.1089/thy.2009.0274. PMID 19888858.
- ↑ 11.0 11.1 11.2 11.3 Baloch ZW, LiVolsi VA, Asa SL, et al. (June 2008). "Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference". Diagn. Cytopathol. 36 (6): 425-37. doi:10.1002/dc.20830. PMID 18478609.
- ↑ 12.0 12.1 URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-037-M.htm. Accessed on: 10 April 2012.
- ↑ Leövey, A.; Bakó, G.; Sztojka, I.; Bordán, L.; Szabó, T.; Kálmán, K.; Balázs, C. (1982). "The pathogenetic connection between Graves' disease and chronic lymphocytic thyroiditis. (The role and incidence of thyroid stimulating antibodies).". Acta Med Acad Sci Hung 39 (1-2): 1-6. PMID 6129766.
- ↑ GD. 2 February 2010.
- ↑ SB. ~29 January 2010.
- ↑ 16.0 16.1 Poropatich C, Marcus D, Oertel YC (1994). "Hashimoto's thyroiditis: fine-needle aspirations of 50 asymptomatic cases". Diagn. Cytopathol. 11 (2): 141-5. PMID 7813361. http://www3.interscience.wiley.com/journal/112701408/abstract?CRETRY=1&SRETRY=0.
- ↑ MacLennan I.C.M (1994). "Germinal Centers". Annual Review Immunology 12: 117-139. PMID 8011279.
- ↑ URL: http://www.definition-of.com/lymphoglandular+body. Accessed on: 27 January 2012.
- ↑ 19.0 19.1 Layfield LJ, Morton MJ, Cramer HM, Hirschowitz S (October 2009). "Implications of the proposed thyroid fine-needle aspiration category of "follicular lesion of undetermined significance": A five-year multi-institutional analysis". Diagn. Cytopathol. 37 (10): 710–4. doi:10.1002/dc.21093. PMID 19373907.
- ↑ SM. 12 January 2010.
- ↑ Kini SR. Guides to clinical aspiration biopsy: thryoid. 2nd Ed. 1996. P.134.
- ↑ Boerner SL, Asa SL. Biopsy Interpretation of the Thyroid. Lippincott Williams & Wilkins. ISBN 978-0-7817-7204-4. PP.112-3.
- ↑ SB. 8 January 2010.
- ↑ WG. 8 January 2010.
- ↑ WG. 8 January 2010.
- ↑ Biopsy Interpretation of the Thyroid. PP.97-98.
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/CytoLearn/CytoQuiz/CQ-021-040/CQ-039-M.htm. Accessed on: 10 April 2012.
- ↑ Halliday BE, Silverman JF, Finley JL (April 1998). "Fine-needle aspiration cytology of amyloid associated with nonneoplastic and malignant lesions". Diagn. Cytopathol. 18 (4): 270–5. PMID 9557261. http://www3.interscience.wiley.com/cgi-bin/fulltext/39158/PDFSTART.
- ↑ URL: http://www.papsociety.org/guidelines/Morphologic%20criteria.doc. Accessed on: 28 April 2010.
- ↑ SB. 7 January 2010.
- ↑ GS. March 2, 2010.